Abstract
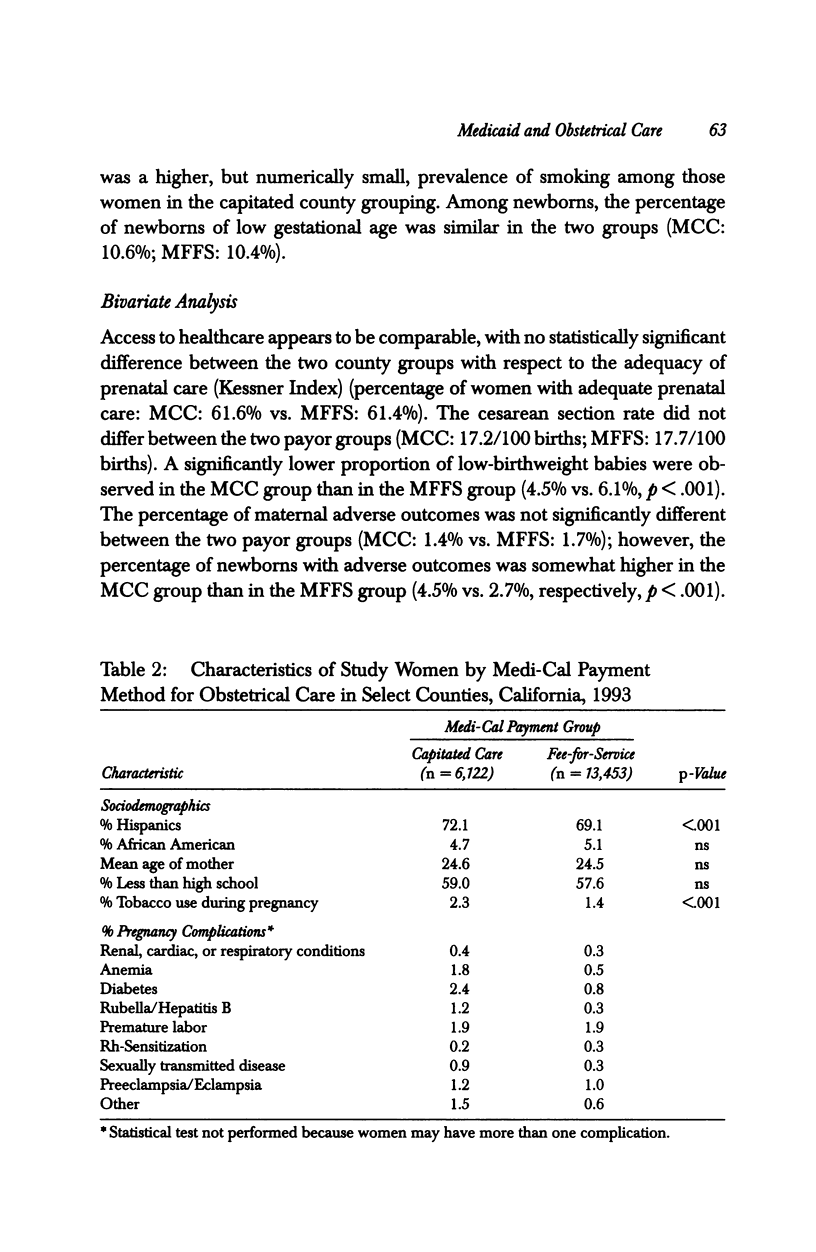
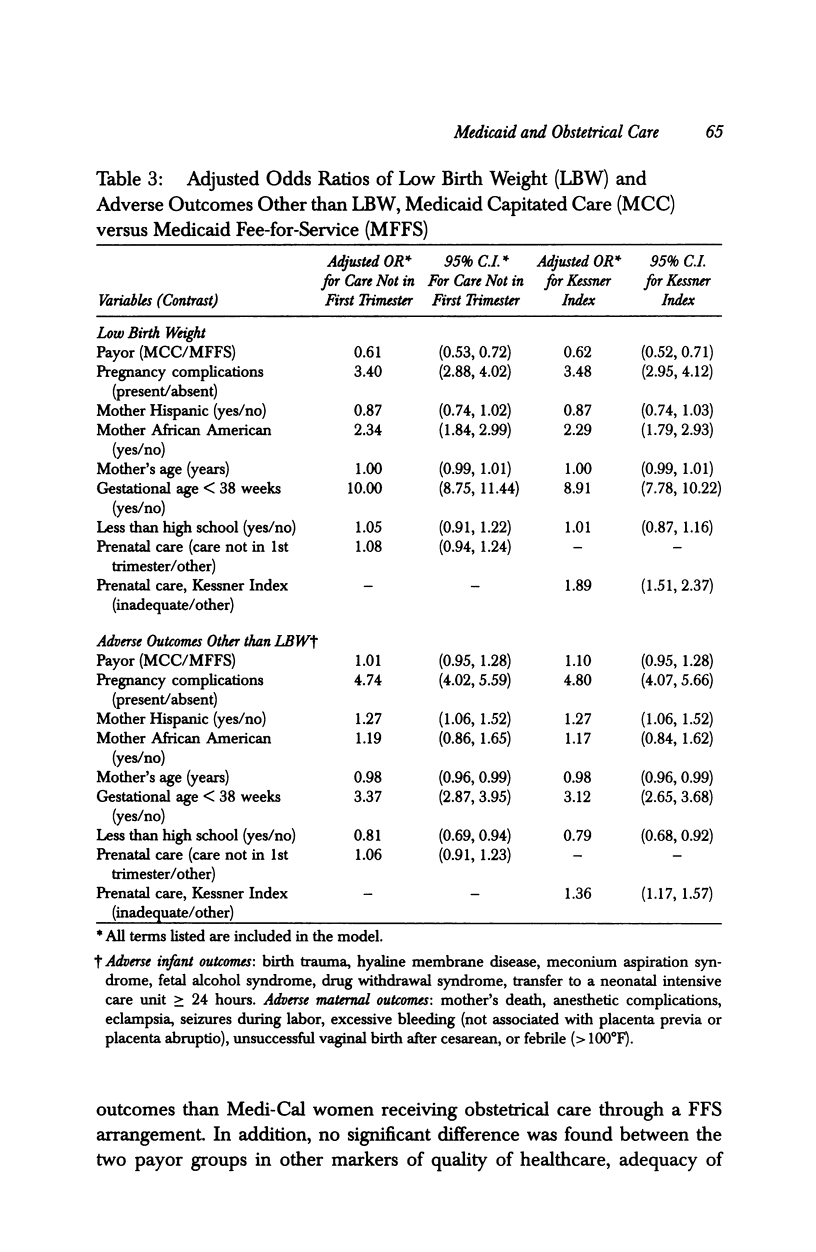
OBJECTIVE: To determine if the payment method influenced the likelihood of selected obstetrical process measures and pregnancy outcome indicators among Medicaid women. DATA SOURCE/STUDY SETTING: Data from the live birth certificates computer file for 1993 from the State of California. The computer files contain information about the demographic characteristics of the mother, her medical conditions prior to delivery, medical problems during labor and delivery, delivery method, newborn and maternal outcomes, and expected principal source of payment for prenatal care and for hospital delivery. STUDY DESIGN: The study sample consisted of singleton live births to women in the California Medi-Cal program residing in one of two counties in which a mixed-model managed care plan was the method of reimbursement or in one of three counties in which fee-for-service was the payment method. The study and control counties were matched in terms of geographic proximity and sociodemographics. PRINCIPAL FINDINGS: Among Medi-Cal women, the likelihood of low birth weight (LBW) was lower in the capitated payment group than in the fee-for-service payment group even when controlling for maternal and newborn characteristics and adequacy of prenatal care. There was no difference in either the adequacy of prenatal care, the cesarean birth rate, or the likelihood of adverse pregnancy outcomes other than LBW between the two payer groups. CONCLUSIONS: Results of this "natural experiment" suggest that enrollment of pregnant Medi-Cal beneficiaries in capitated healthcare services through a primary care case management system in a county-organized health system/health insuring organization can have a beneficial effect on low birth weight and provide care comparable to a fee-for-service system.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Carey T. S., Weis K., Homer C. Prepaid versus traditional Medicaid plans: lack of effect on pregnancy outcomes and prenatal care. Health Serv Res. 1991 Jun;26(2):165–181. [PMC free article] [PubMed] [Google Scholar]
- Fiscella K. Does prenatal care improve birth outcomes? A critical review. Obstet Gynecol. 1995 Mar;85(3):468–479. doi: 10.1016/0029-7844(94)00408-6. [DOI] [PubMed] [Google Scholar]
- Freund D. A., Hurley R. E., Paul J., Grubb C., Rossiter L. F., Adamache K. W. Interim findings from the Medicaid competition demonstrations. Adv Health Econ Health Serv Res. 1989;10:153–181. [PubMed] [Google Scholar]
- Goldfarb N. I., Hillman A. L., Eisenberg J. M., Kelley M. A., Cohen A. V., Dellheim M. Impact of a mandatory Medicaid case management program on prenatal care and birth outcomes. A retrospective analysis. Med Care. 1991 Jan;29(1):64–71. doi: 10.1097/00005650-199101000-00006. [DOI] [PubMed] [Google Scholar]
- Jesilow P., Geis G., Pontell H. Fraud by physicians against Medicaid. JAMA. 1991 Dec 18;266(23):3318–3322. [PubMed] [Google Scholar]
- Krieger J. W., Connell F. A., LoGerfo J. P. Medicaid prenatal care: a comparison of use and outcomes in fee-for-service and managed care. Am J Public Health. 1992 Feb;82(2):185–190. doi: 10.2105/ajph.82.2.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray J. L., Bernfield M. The differential effect of prenatal care on the incidence of low birth weight among blacks and whites in a prepaid health care plan. N Engl J Med. 1988 Nov 24;319(21):1385–1391. doi: 10.1056/NEJM198811243192105. [DOI] [PubMed] [Google Scholar]
- Petitti D. B., Hiatt R. A., Chin V., Croughan-Minihane M. An outcome evaluation of the content and quality of prenatal care. Birth. 1991 Mar;18(1):21–25. doi: 10.1111/j.1523-536x.1991.tb00049.x. [DOI] [PubMed] [Google Scholar]
- Quick J. D., Greenlick M. R., Roghmann K. J. Prenatal care and pregnancy outcome in an HMO and general population: a multivariate cohort analysis. Am J Public Health. 1981 Apr;71(4):381–390. doi: 10.2105/ajph.71.4.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley G. F., Potosky A. L., Lubitz J. D., Brown M. L. Stage of cancer at diagnosis for Medicare HMO and fee-for-service enrollees. Am J Public Health. 1994 Oct;84(10):1598–1604. doi: 10.2105/ajph.84.10.1598. [DOI] [PMC free article] [PubMed] [Google Scholar]


