Abstract
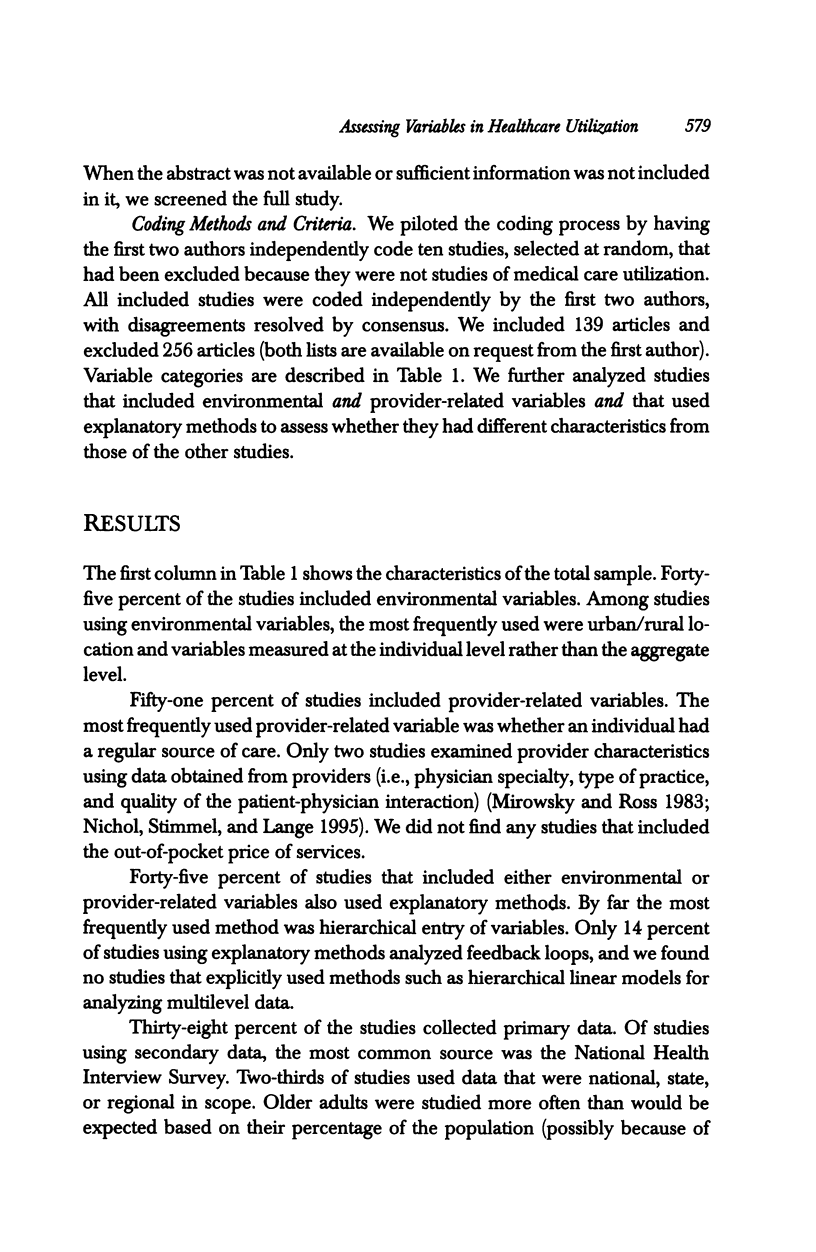
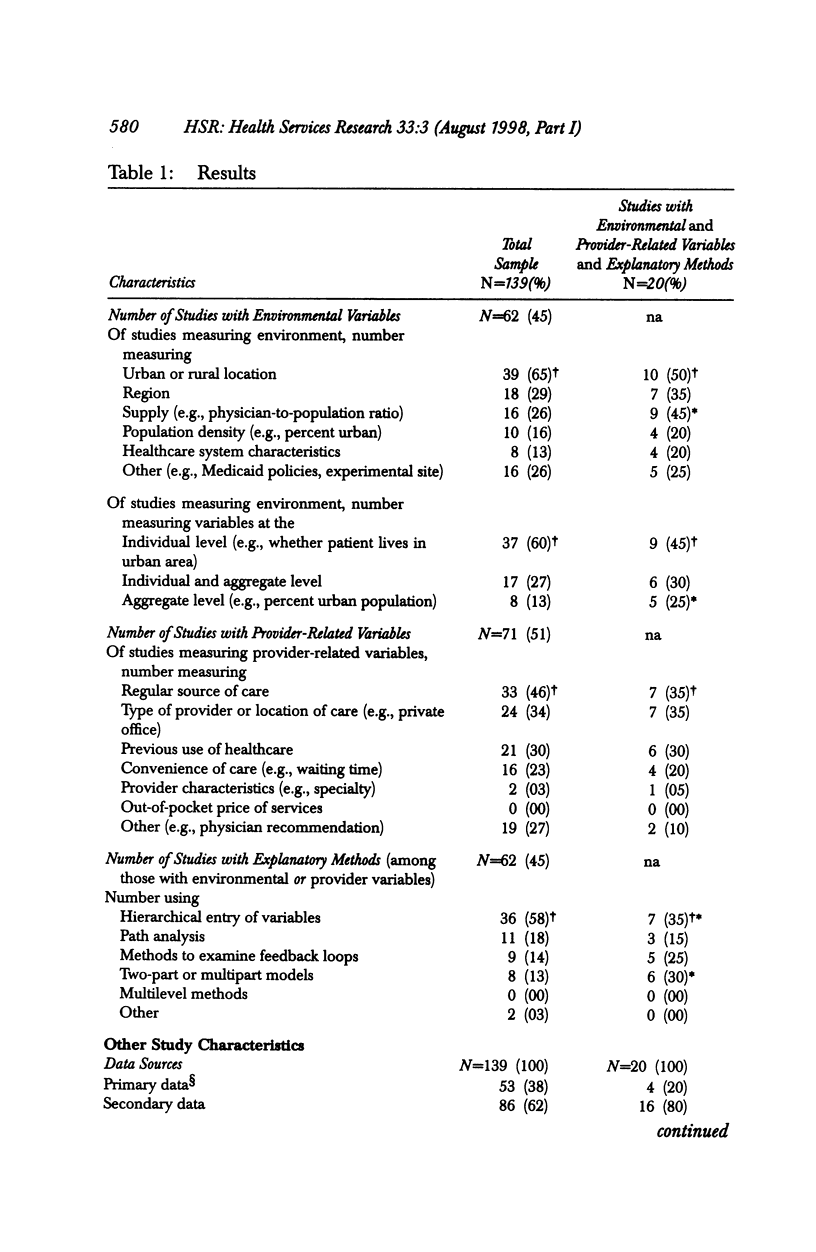
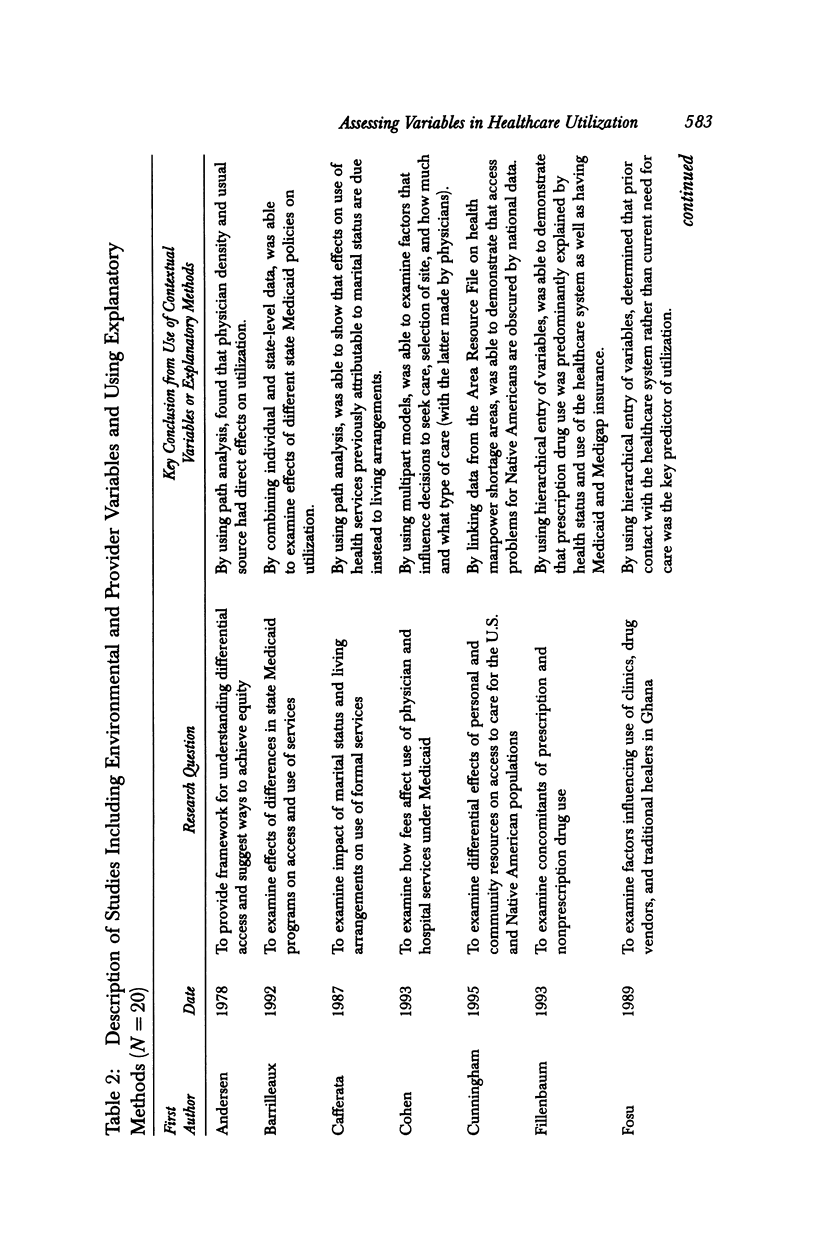
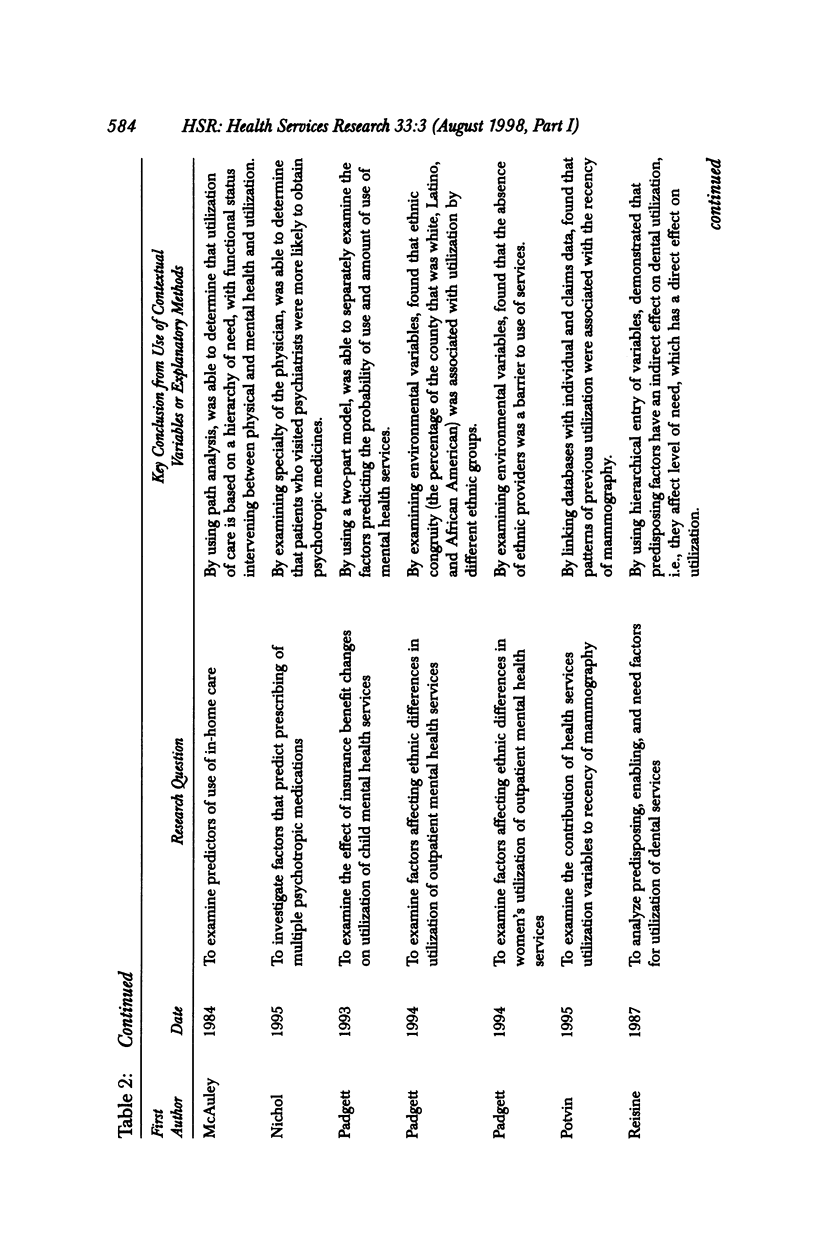
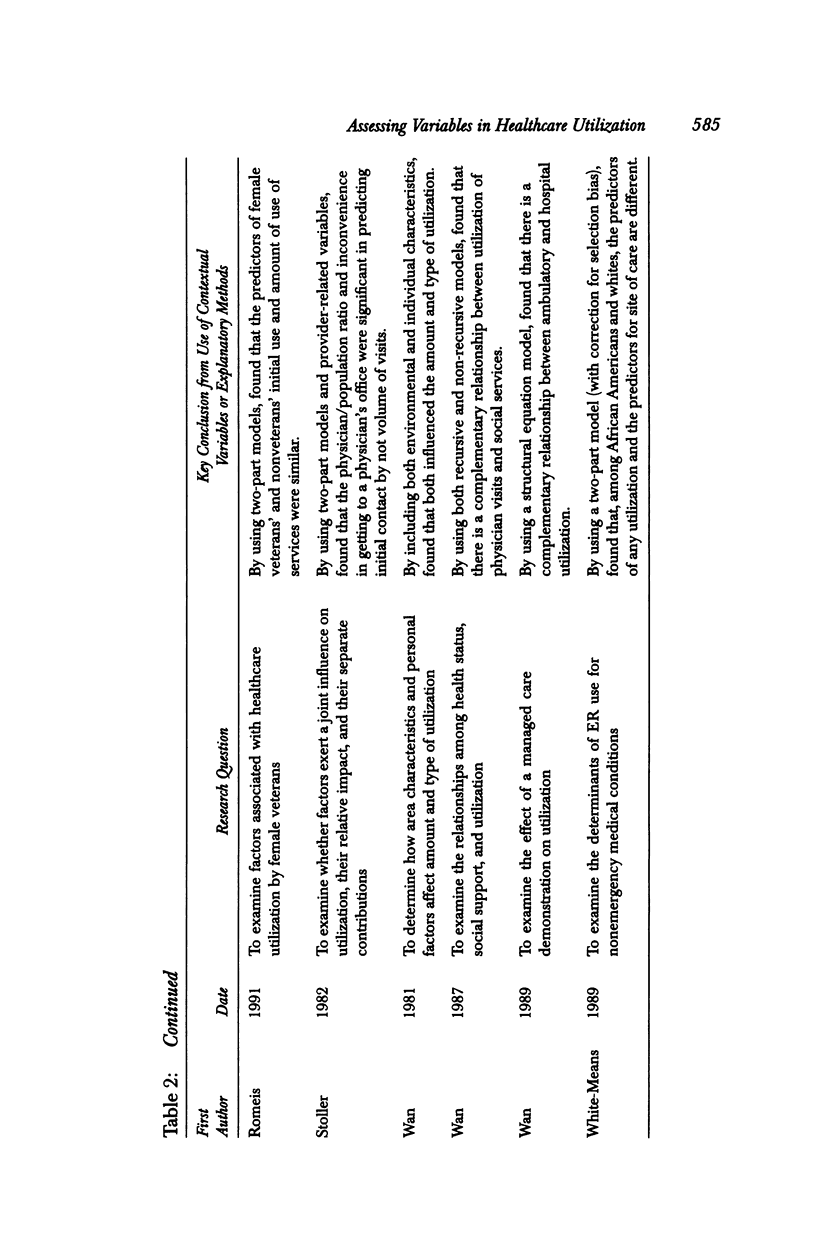
OBJECTIVE: The behavioral model of utilization, developed by Andersen, Aday, and others, is one of the most frequently used frameworks for analyzing the factors that are associated with patient utilization of healthcare services. However, the use of the model for examining the context within which utilization occurs-the role of the environment and provider-related factors-has been largely neglected. OBJECTIVE: To conduct a systematic review and analysis to determine if studies of medical care utilization that have used the behavioral model during the last 20 years have included environmental and provider-related variables and the methods used to analyze these variables. We discuss barriers to the use of these contextual variables and potential solutions. DATA SOURCES: The Social Science Citation Index and Science Citation Index. We included all articles from 1975-1995 that cited any of three key articles on the behavioral model, that included all articles that were empirical analyses and studies of formal medical care utilization, and articles that specifically stated their use of the behavioral model (n = 139). STUDY DESIGN: Design was a systematic literature review. DATA ANALYSIS: We used a structured review process to code articles on whether they included contextual variables: (1) environmental variables (characteristics of the healthcare delivery system, external environment, and community-level enabling factors); and (2) provider-related variables (patient factors that may be influenced by providers and provider characteristics that interact with patient characteristics to influence utilization). We also examined the methods used in studies that included contextual variables. PRINCIPAL FINDINGS: Forty-five percent of the studies included environmental variables and 51 percent included provider-related variables. Few studies examined specific measures of the healthcare system or provider characteristics or used methods other than simple regression analysis with hierarchical entry of variables. Only 14 percent of studies analyzed the context of healthcare by including both environmental and provider-related variables as well as using relevant methods. CONCLUSIONS: By assessing whether and how contextual variables are used, we are able to highlight the contributions made by studies using these approaches, to identify variables and methods that have been relatively underused, and to suggest solutions to barriers in using contextual variables.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aday L. A., Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974 Fall;9(3):208–220. [PMC free article] [PubMed] [Google Scholar]
- Andersen R., Aday L. A. Access to medical care in the U.S.: realized and potential. Med Care. 1978 Jul;16(7):533–546. doi: 10.1097/00005650-197807000-00001. [DOI] [PubMed] [Google Scholar]
- Andersen R., Newman J. F. Societal and individual determinants of medical care utilization in the United States. Milbank Mem Fund Q Health Soc. 1973 Winter;51(1):95–124. [PubMed] [Google Scholar]
- Barrilleaux C. J., Miller M. E. Decisions without consequences: cost control and access in state Medicaid programs. J Health Polit Policy Law. 1992 Spring;17(1):97–118. doi: 10.1215/03616878-17-1-97. [DOI] [PubMed] [Google Scholar]
- Broyles R. W., Rosko M. D. The demand for health insurance and health care: a review of the empirical literature. Med Care Rev. 1988 Fall;45(2):291–338. doi: 10.1177/107755878804500205. [DOI] [PubMed] [Google Scholar]
- Cafferata G. L. Marital status, living arrangements, and the use of health services by elderly persons. J Gerontol. 1987 Nov;42(6):613–618. doi: 10.1093/geronj/42.6.613. [DOI] [PubMed] [Google Scholar]
- Cohen J. W. Medicaid physician fees and use of physician and hospital services. Inquiry. 1993 Fall;30(3):281–292. [PubMed] [Google Scholar]
- Cunningham P. J., Cornelius L. J. Access to ambulatory care for American Indians and Alaska Natives; the relative importance of personal and community resources. Soc Sci Med. 1995 Feb;40(3):393–407. doi: 10.1016/0277-9536(94)e0072-z. [DOI] [PubMed] [Google Scholar]
- Duncan C., Jones K., Moon G. Health-related behaviour in context: a multilevel modelling approach. Soc Sci Med. 1996 Mar;42(6):817–830. doi: 10.1016/0277-9536(95)00181-6. [DOI] [PubMed] [Google Scholar]
- Fillenbaum G. G., Hanlon J. T., Corder E. H., Ziqubu-Page T., Wall W. E., Jr, Brock D. Prescription and nonprescription drug use among black and white community-residing elderly. Am J Public Health. 1993 Nov;83(11):1577–1582. doi: 10.2105/ajph.83.11.1577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fosu G. B. Access to health care in urban areas of developing societies. J Health Soc Behav. 1989 Dec;30(4):398–411. [PubMed] [Google Scholar]
- Gatsonis C., Normand S. L., Liu C., Morris C. Geographic variation of procedure utilization. A hierarchical model approach. Med Care. 1993 May;31(5 Suppl):YS54–YS59. doi: 10.1097/00005650-199305001-00008. [DOI] [PubMed] [Google Scholar]
- Geller S. E., Burns L. R., Brailer D. J. The impact of nonclinical factors on practice variations: the case of hysterectomies. Health Serv Res. 1996 Feb;30(6):729–750. [PMC free article] [PubMed] [Google Scholar]
- Kronenfeld J. J. Provider variables and the utilization of ambulatory care services. J Health Soc Behav. 1978 Mar;19(1):68–76. [PubMed] [Google Scholar]
- Mechanic D. Correlates of physician utilization: why do major multivariate studies of physician utilization find trivial psychosocial and organizational effects? J Health Soc Behav. 1979 Dec;20(4):387–396. [PubMed] [Google Scholar]
- Miller R. H., Luft H. S. Managed care plan performance since 1980. A literature analysis. JAMA. 1994 May 18;271(19):1512–1519. [PubMed] [Google Scholar]
- Mirowsky J., Ross C. E. Patient satisfaction and visiting the doctor: a self-regulating system. Soc Sci Med. 1983;17(18):1353–1361. doi: 10.1016/0277-9536(83)90195-8. [DOI] [PubMed] [Google Scholar]
- Nichol M. B., Stimmel G. L., Lange S. C. Factors predicting the use of multiple psychotropic medications. J Clin Psychiatry. 1995 Feb;56(2):60–66. [PubMed] [Google Scholar]
- Padgett D. K., Patrick C., Burns B. J., Schlesinger H. J., Cohen J. The effect of insurance benefit changes on use of child and adolescent outpatient mental health services. Med Care. 1993 Feb;31(2):96–110. doi: 10.1097/00005650-199302000-00002. [DOI] [PubMed] [Google Scholar]
- Padgett D. K., Patrick C., Burns B. J., Schlesinger H. J. Ethnicity and the use of outpatient mental health services in a national insured population. Am J Public Health. 1994 Feb;84(2):222–226. doi: 10.2105/ajph.84.2.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips K. A., Kerlikowske K., Baker L. C., Chang S. W., Brown M. L. Factors associated with women's adherence to mammography screening guidelines. Health Serv Res. 1998 Apr;33(1):29–53. [PMC free article] [PubMed] [Google Scholar]
- Pottick K., Hansell S., Gutterman E., White H. R. Factors associated with inpatient and outpatient treatment for children and adolescents with serious mental illness. J Am Acad Child Adolesc Psychiatry. 1995 Apr;34(4):425–433. [PubMed] [Google Scholar]
- Potvin L., Camirand J., Béland F. Patterns of health services utilization and mammography use among women aged 50 to 59 years in the Québec Medicare system. Med Care. 1995 May;33(5):515–530. doi: 10.1097/00005650-199505000-00006. [DOI] [PubMed] [Google Scholar]
- Reisine S. A path analysis of the utilization of dental services. Community Dent Oral Epidemiol. 1987 Jun;15(3):119–124. doi: 10.1111/j.1600-0528.1987.tb00497.x. [DOI] [PubMed] [Google Scholar]
- Romeis J. C., Gillespie K. N., Virgo K. S., Thorman K. E. Female veterans' and nonveterans' use of health care services. Med Care. 1991 Sep;29(9):932–936. doi: 10.1097/00005650-199109000-00013. [DOI] [PubMed] [Google Scholar]
- Shortell S. M., Richardson W. C., LoGerfo L. P., Diehr P., Weaver B., Green K. E. The relationships among dimensions of health services in two provider systems: a causal model approach. J Health Soc Behav. 1977 Jun;18(2):139–159. [PubMed] [Google Scholar]
- Stoller E. P. Patterns of physician utilization by the elderly: a multivariate analysis. Med Care. 1982 Nov;20(11):1080–1089. doi: 10.1097/00005650-198211000-00003. [DOI] [PubMed] [Google Scholar]
- Stump T. E., Johnson R. J., Wolinsky F. D. Changes in physician utilization over time among older adults. J Gerontol B Psychol Sci Soc Sci. 1995 Jan;50(1):S45–S58. doi: 10.1093/geronb/50b.1.s45. [DOI] [PubMed] [Google Scholar]
- Wan T. T., Broida J. H. Factors affecting variations in health services utilization in Quebec, Canada. Socioecon Plann Sci. 1981;15(5):231–242. doi: 10.1016/0038-0121(81)90043-4. [DOI] [PubMed] [Google Scholar]
- Wennberg J. E., Barnes B. A., Zubkoff M. Professional uncertainty and the problem of supplier-induced demand. Soc Sci Med. 1982;16(7):811–824. doi: 10.1016/0277-9536(82)90234-9. [DOI] [PubMed] [Google Scholar]
- Wennberg J. E. Future directions for small area variations. Med Care. 1993 May;31(5 Suppl):YS75–YS80. doi: 10.1097/00005650-199305001-00012. [DOI] [PubMed] [Google Scholar]
- White-Means S. I., Thornton M. C. Nonemergency visits to hospital emergency rooms: a comparison of blacks and whites. Milbank Q. 1989;67(1):35–57. [PubMed] [Google Scholar]


