Despite advancements in lung cancer diagnosis and treatments leading to improved outcomes over the last decade, lung cancer remains the leading cause of cancer mortality in the United States. In 2021, there will be an estimated 235,760 new cases of lung cancer diagnosed and 131,880 estimated deaths [1]. Although lung cancer affects people of all races and ethnicities, it does not affect them all equally. Black individuals have increased lung cancer mortality compared with White, non-Hispanic individuals. Despite the decreasing incidence in lung cancer among Latino and Hispanic people, lung cancer remains the leading cause of cancer related death among Latino individuals [1–3]. This is in part due to the stage at the time of diagnosis, as only 17% of Latino and Hispanic individuals are diagnosed with localized disease and the 5-year survival rate for distant stage disease is 6% [3].
Primary risk reduction is a critical strategy to improve lung cancer outcomes. Smoking is the leading cause of preventable mortality in the United States, accounting for more than 480,00 deaths every year [4]. Smoking is an important public health issue in the Latino community; smoking-related cancer and cardiovascular disease, including heart disease and stroke, are among the top five leading causes of death among Latino people. The majority of Latino current smokers report wanting to quit, with 56.2% reporting a quit attempt in the past year, but access to smoking cessation resources lag in the Latino community [4]. In addition, lower rates health insurance coverage among Latino individuals makes it less likely that they will have opportunities to be identified as a smoker, receive smoking cessation counseling, or be advised to undergo lung cancer screening (LCS). We anticipate these smoking-related disparities will continue to be a leading cause of preventable mortality in this community without targeted interventions.
Secondary risk reduction, including LCS, can serve as a pillar to bridge disparities in lung cancer outcomes through early detection among Latino communities. However, despite the proven benefits of LCS in reducing lung cancer mortality, only 10% to 20% of the eligible population has been screened and, specifically, the proportion of eligible Latino people participating in LCS is likely to be lower [5]. The barriers to LCS uptake are complex and multifactorial, from difficulty understanding eligibility criteria, readability level of available health information for shared decision making, cost concerns, safety concern in routine care due to the ongoing COVID-19 pandemic, among others [6]. These factors are magnified among Latino individuals who face multilevel systemic barriers to care likely resulting in lower LCS rates. Without culturally tailored outreach and multilevel interventions for Latino communities, lung cancer disparities are likely to widen with the introduction of new LCS criteria. The recently updated LCS eligibility guidelines recommended by the US Preventive Services Task Force (USPSTF) provides an opportune window to redesign outreach efforts and improve LCS participation among latino communities [7]. The USPSTF is committed to addressing systemic racism through clinical recommendations, and the expansion in LCS guidelines represents a foundational step [7]. A recently published article established the USPSTF commitment to bridging health disparities that are a result of structural societal barriers [8]. They provide a framework to proactively address these issues that include promotion of racial and ethnic diversity in evidence-based data and fostering transparency in identifying and addressing these gaps in health care. The updated USPSTF guidelines for LCS eligibility provide a concrete first step in addressing disparities in lung cancer care through early detection [7]. Underrepresented minorities tend to be exposed to other lung cancer risk factors that result in being diagnosed at an earlier age with a lower pack-year smoking history [3]. The new USPSTF guidelines lower the starting age to 50 (from 55) and the smoking history to 20 (from 30) pack-years, thus increasing the likelihood of Latino people to be eligible for LCS. To achieve maximum benefit and increase LCS uptake, outreach efforts need to be tailored to fit the needs of the Latino community to ensure participation in this lifesaving screening examination. Cancer screening rates, particularly for racial and ethnic minority groups, have been lowered because of the COVID-19 pandemic. The COVID-19 pandemic has exacerbated health disparities related to social determinants of health among racial and ethnic minorities, and this effect is impacting LCS in the return to care phase [9]. Racial and ethnic minorities, including Latino individuals, have experienced increased morbidity and mortality due to COVID-19 disease secondary to a combination of socioeconomic and medical factors that increase their exposure and result in higher likelihood of experiencing delays in seeking care and lack of access to virtual care [10]. The ongoing pandemic has resulted in diversion of medical resources to address immediate needs and postponing nonurgent, routine medical care including LCS. Without targeted outreach, this postponement of LCS can potentially result in widening the existing disparities in LCS among minority communities. The National Institute on Minority Health and Health Disparities offers a multidimensional research framework that can be adapted to facilitate assessment of emerging disparities, identify opportunities, and measure progress in LCS [11]. It is paramount that our return to cancer screening is tailored for those who are most vulnerable.
Outreach programs are most effective when community-based participatory research principles are leveraged in the process [12,13] and integrated in all aspects of intervention design, from conceptualization to implementation and evaluation. Community-based participatory research engages the community to partner with the health care system in defining the community’s identified health needs and barriers to care including the research question, intervention design, and ultimately intervention implementation. It is the underpinning of patient-centered outcomes research and patient-centered care delivery. Engaging diverse community stakeholders will provide direct knowledge to detect and understand barriers and facilitators to LCS across Latino communities. This approach also serves to promote bridges of trust with community members, who will be active participants in the implementation process. Building trust is a key component to foster long-term relationships and the longitudinal engagement necessary to improve health disparities among Latino communities. Without the development of targeted interventions that incorporate these elements, the existing health care disparities gap will continue to widen, affecting Latino communities who are most vulnerable.
Potential solutions address three general promoters of LCS: awareness, opportunities, and participation (Fig. 1). Successful implementation of interventions to promote LCS should incorporate each key stakeholder’s locus of control. At the patient level, intervention components include increasing accessibility of multilingual health information, appropriate reading level, and image-rich content that accounts for numeracy. Stressing the importance of providing an accurate smoking history and routinely soliciting this information as well as routinely querying interest in a shared decision-making encounter for LCS can be additionally directed toward the patient. For providers, LCS guideline dissemination, consistent documentation, and update of smoking history and increasing LCS enrollment for newly eligible patients are within their scope of influence. Ultimately, system intervention components may include tailoring culturally aware LCS education for the Latino population, using electronic medical record identification of patient eligibility, and incorporating LCS in population health and quality metrics dashboards.
Fig. 1.
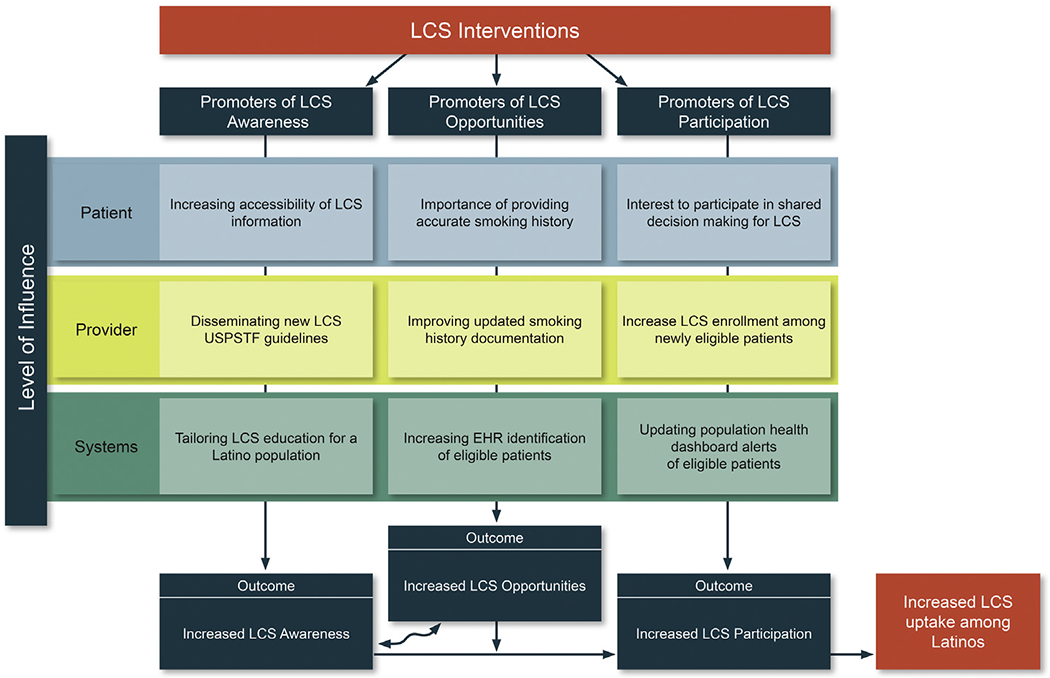
Adapted conceptual model lung cancer screening intervention model to reduce health disparities. Adapted from Ford et al [16] and incorporating elements from National Institute of Minority Health and Health Disparities [11], this model structures barriers and promoters to increase awareness, opportunities, and participation in clinical trials to reduce disparities in clinical care and LCS by locus of control. Within this framework, we provide examples of intervention components. LCS = lung cancer screening; USPSTF = US Preventative Services Task Force.
Culturally aware interventions need to account for communication mechanisms prevalent in the Latino community. The proliferation of telehealth services, smartphone message delivery, and patient portal expansion emphasizes the need for digitization of outreach to scale implementation. However, as with all innovations, we run the risk of widening the disparities gap, particularly the digital divide. “Techquity,” or equitable access to technology such as stable broadband access or smartphone penetration and willingness to use mobile data for health encounters, provides opportunities for health systems to engage the Latino community members to provide their unique perspective through preparatory community-based participatory research [14]. Intervention components at the patient level need sufficient flexibility to be delivered by telephone, as text only, or through a smartphone application or patient portal as determined by the patients’ needs, preferences, and resources. All these mechanisms of communication need to be explicitly tested and adapted with equity in mind.
The effect of care quality and access has been estimated to modify only 20% of the variation in outcomes while social determinants of health and the physical environment has cumulatively affect up to 50% of variation [15]. These latter two elements can be inferred by ZIP code. Hearing directly from the community adds further nuance to the development and implementation of effective strategies to improve LCS and narrow disparities in morbidity and mortality from lung cancer in the Latino community. We encourage all radiologists to identify potential opportunities within their sphere of influence to understand the unique needs of their patient population to better serve their community, wherever they are. Although we discuss specific barriers in the Latino community, these principles are applicable to all communities and practices. We must meet patients where they are regarding knowledge, willingness, and access to LCS to be able to deliver the right information and right care to the right patient at the right time. This update in USPSTF recommended guidelines for LCS serves as a catalyst for us to regroup and improve LCS participation among Latino communities, but this requires a collaborative effort, in which radiologists are critical, to decrease the growing disparities in LCS screening.
Acknowledgments
Dr Flores reports grants from National Cancer Institute Research Diversity Supplement, grants from American College of Radiology Innovation Fund. Dr Carlos is Editor-in-Chief of the JACR and reports other support from JACR, during the conduct of the study. The other authors state that they have no conflict of interest related to the material discussed in this article. All authors are employees of academic institutions.
Contributor Information
Efrén J. Flores, Harvard Medical School, Boston, Massachusetts; Department of Radiology, Massachusetts General Hospital, Boston, Massachusetts; The Mongan Institute, Boston, Massachusetts.
Kelly E. Irwin, Harvard Medical School, Boston, Massachusetts; Director, Collaborative Care and Community Engagement Program, Massachusetts General Hospital Cancer Center; Department of Psychiatry, Massachusetts General Hospital, Boston, Massachusetts; and The Mongan Institute, Boston, Massachusetts.
Elyse R. Park, Harvard Medical School, Boston, Massachusetts; Director of the Health Promotion and Resiliency Intervention Research Program, Massachusetts General Hospital, Associate Director of Survivorship Research & Psychosocial Services, Department of Psychiatry, Massachusetts General Hospital, Boston, Massachusetts; and The Mongan Institute, Boston, Massachusetts.
Ruth C. Carlos, Assistant Chair for Clinical Research, Department of Radiology, University of Michigan Medical Center, Ann Arbor Michigan; and University of Michigan, School of Medicine, Ann Arbor, Michigan.
REFERENCES
- 1.American Cancer Society. Cancer facts & figures 2019. Published 2019. Available at: https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2019.html. Accessed February 28, 2021.
- 2.American Cancer Society. Cancer facts & figures for Hispanics/Latinos 2018-2020. Published 2018. Available at: https://www.Cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-facts-and-figures-for-hispanics-and-latinos/cancer-facts-and-figures-for-hispanics-and-latinos-2018-2020.pdf. Accessed March 1, 2021.
- 3.Jemal A, Fedewa SA. Lung cancer screening with low-dose computed tomography in the United States-2010 to 2015. JAMA Oncol 2017;3:1278–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Smoking and tobacco use. Fast facts. Available at: https://www.cdc.gov/tobacco/data_statistics/fact_sheets/fast_facts/index.htm. Accessed March 9, 2021.
- 5.Narayan AK, Gupta Y, Little BP, Shepard JO, Flores EJ. Lung cancer screening eligibility and use with low-dose computed tomography: results from the 2018 Behavioral Risk Factor Surveillance System cross-sectional survey. Cancer 2021;127:748–56. [DOI] [PubMed] [Google Scholar]
- 6.Wang GX, Neil JM, Fintelmann FJ, Little BP, Narayan AK, Flores EJ. Guideline-discordant lung cancer screening: emerging demand and provided indications. J Am Coll Radiol 2021;18:395–405. [DOI] [PubMed] [Google Scholar]
- 7.US Preventive Services Task Force. Final recommendation statement: lung cancer: screening. Available at. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/lung-cancer-screening. Accessed March 9, 2021.
- 8.Doubeni CA, Simon M, Krist AH. Addressing systemic racism through clinical preventive service recommendations from the US Preventive Services Task Force. JAMA 2021;325:627–8. [DOI] [PubMed] [Google Scholar]
- 9.Dorn AV, Cooney RE, Sabin ML. COVID-19 exacerbating inequalities in the US. Lancet. April 2020;395(10232):1243–4. 10.1016/S0140-6736(20)30893-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rocklöv J, Sjödin H. High population densities catalyse the spread of COVID-19. J Travel Med 2020;27(3). 10.1093/jtm/taaa038. taaa038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.NCI. National Institute on Minority Health and Health Disparities Research Framework. Available at: https://www.nimhd.nih.gov/docs/research_framework/research-framework-slide.pdf. Accessed February 8, 2021.
- 12.Committee CCEKF. Principals of Community Engagement. Second Edition 2011. [Google Scholar]
- 13.Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med 2003;139:907–15. [DOI] [PubMed] [Google Scholar]
- 14.Velasquez D, Mehrotra A. Ensuring the growth of telehealth during COVID-19 does not exacerbate disparities in care. Health Affairs 2020. 10.1377/hblog20200505.591306. [DOI] [Google Scholar]
- 15.Hood CM, Gennuso KP, Swain GR, Catlin BB. County health rankings: relationships between determinant factors and health outcomes. Am J Prev Med 2016;50:129–35. [DOI] [PubMed] [Google Scholar]
- 16.Ford JG, Howerton MW, Lai GY, et al. Barriers to recruiting underrepresented populations to cancer clinical trials: a systematic review. Cancer 2008;112:228–42. [DOI] [PubMed] [Google Scholar]


