Abstract
Global warming has been changing the planet’s climate pattern, leading to increasing frequency, intensity and duration of extreme weather events and natural disasters. These climate-changing events affect various health outcomes adversely through complicated pathways. This paper reviews the main signs of climate change so far, e.g., suboptimal ambient temperature, sea-level rise and other conditions, and depicts the interactive pathways between different climate-changing events such as suboptimal temperature, wildfires, and floods with a broad range of health outcomes. Meanwhile, the modifying effect of socioeconomic, demographic and environmental factors on the pathways is summarised, such that the youth, elderly, females, poor and those living in coastal regions are particularly susceptible to climate change. Although Earth as a whole is expected to suffer from climate change, this review article discusses some potential benefits for certain regions, e.g., a more liveable environment and sufficient food supply. Finally, we summarise certain mitigation and adaptation strategies against climate change and how these strategies may benefit human health in other ways. This review article provides a comprehensive and concise introduction of the pathways between climate change and human health and possible solutions, which may map directions for future research.
Keywords: Climate change, Health, Pathways, Adaptation, Mitigation
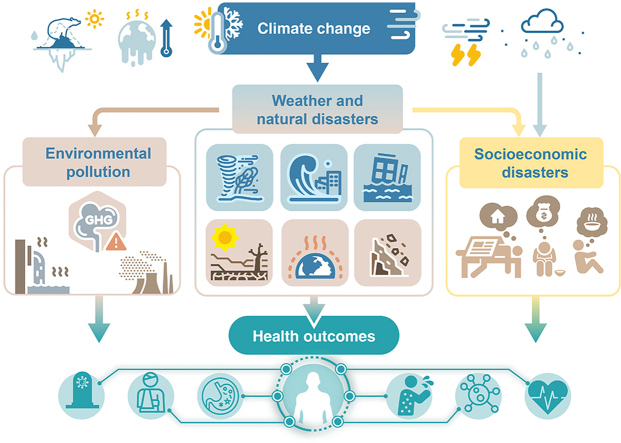
Graphical abstract
Highlights
-
•
Climate change affects health via natural disasters and socioeconomic pathways.
-
•
Benefits of climate change on health may exist in certain areas.
-
•
Socioeconomic and environmental factors may modify climate change-health pathways.
-
•
Certain mitigation and adaptation strategies are suggested against climate change.
1. Introduction
The atmospheric concentrations of carbon dioxide (CO2), methane (CH4), and nitrous oxide (N2O) have increased by 47%, 156% and 23% since the beginning of the Industrial Revolution [1]. The last 30 years, paralleling the unprecedented emission of greenhouse gases, were recorded as the hottest period since 1850 [2]. The warming atmosphere and ocean over time have affected Earth’s climate system and disrupted the balance of nature through complicated pathways, resulting in climate perturbation and natural disasters, e.g., more frequent extreme temperature events (ETEs), droughts and floods, over the past decades [3,4].
Climate change has been regarded as the single largest global health challenge in the 21st century by affecting the physical environment and ecosystem and their interactions with human beings [3,5,6]. The health outcomes range from premature deaths caused by natural disasters to communicable diseases due to deteriorated hygiene and over-proliferation of pathogens [3,7]. A multi-country study has suggested that climate change is responsible for 400,000 additional deaths each year and will contribute to 700,000 annual deaths by 2030 [8]. All populations living in low to high altitudes and in low- to high-income countries are under the threat of climate change regardless of their age and socioeconomic status.
Although the health impacts of climate change have been well documented, so far, the evidence has primarily focused on health outcomes associated with certain single climatic conditions [9,10]. For example, previous studies have revealed that heatwaves could raise the mortality rate of both cardiovascular and respiratory diseases [11]. However, few studies have described the interactions between different climatic variables or with other non-environmental factors and their co-effects on human health. Clarifying the pathways is crucial for understanding the impacts of climate change on human health and developing mitigation and adaptation strategies.
In this article, we reviewed the major pathways between environmental hazards mediated by climate change and human health. We mainly focused on five sections: major signs of climate change; adverse effects of climate change; regional benefits of climate change; modifying effects of socioeconomic, demographic, and other factors; and certain mitigation and adaption strategies. For each section, we summarised the main findings and mapped out the potential directions for future research.
2. Major signs of climate change
The global mean surface temperature in 2020 has increased by 0.94 °C above the 1951–1980 average [12]. In the context of global warming, the frequency, intensity and duration of ETEs and natural disasters have been increasing substantially. For example, the total records of severe heatwaves between 2015 and 2020 have been twice as high as the 1951–1980 average [13]. In addition, 46% of floods, 34% of storms, 31% of droughts and 32% of wildfires occurred in the last 15 years since 1900 [13]. The mean sea surface temperature has risen at a pace of 0.06 °C per decade since 1880 [14]. The warming atmosphere has been melting glaciers and ice sheets, which reduces the heat reflection, and in turn, accelerates global warming. The melt of ice sheets and glaciers along with the thermal expansion of seawater plays a pivotal role in rising sea levels. Between 1971 and 2010, the sea level rose by 1.7 mm per year, and the rate has doubled since 1993 [15].
Greenhouse gases are currently emitted at a pace exceeding the worst projection of the Intergovernmental Panel on Climate Change (IPCC) [1]. Consequently, the mean surface temperature in 2100 is projected to be 4 °C higher than the 1986–2005 average, far beyond the previous estimation (2 °C). Forceful strategies, e.g., cutting off 70% of anthropogenic emission by 2050 and achieving net negative emission by 2100, may confine the warming trend under the representative concentration pathway (RCP) 2.6 scenario, but the temperature will still increase by 1.0 °C by the end of the 21st century [1]. Even if anthropogenic emissions can be stopped immediately, the global mean surface temperature will continue to rise by 0.2–0.5 °C in the following decade [16].
Accompanied by the global warming trend, the patterns of a variety of meteorological and other events are also projected to change in the future. For example, the global monsoon summer precipitation is expected to increase by 1.71% ± 2.38% under the high climate change scenario in 2021–2040 [17]. Changes in temperature and precipitation are associated with various flooding patterns, whose frequency by 2100 will be 4–14 times higher than the 1971–2000 average [18]. The modelling study also suggested that the drought intensity would show a widespread increase. Due to global warming, the frequency, intensity, and duration of ETEs are projected to increase [19]. Holding the present emission pattern of greenhouse gases, the sea level by 2100 will be 75 cm higher than the 1986–2005 average [20]. Whether climate change would increase the frequency of hurricanes remains unclear. However, climate change may exacerbate the hazard of hurricanes [21].
3. Main pathways between climate change and human health
Global warming causes anomalies in climatic and natural conditions, and their interaction may lead to a higher risk of various health outcomes (Fig. 1).
Fig. 1.
Main pathways between climate change and health outcomes.
3.1. Extreme events
3.1.1. Suboptimal temperatures
Both low and high temperatures are associated with increased mortality risk, exhibiting a J-, U- or V-shape [22]. It was estimated that 5,083,173 deaths per year were attributable to suboptimal temperatures, accounting for 9.43% of total deaths worldwide from 2000 to 2019. On top of that, the temperature-related excess mortality is expected to further increase until the 2050s [10,23]. In addition to excess deaths, the temperature change may cause a range of disorders. For example, exposure to extremely high temperatures has been associated with a higher possibility of emergency department visits and hospital admissions due to diseases of the cardiovascular, respiratory and metabolic systems [11,[24], [25], [26], [27]]. The increased cases of depression, anxiety, and suicide during hot days suggest that extreme high temperature is likely to trigger behavioural and mental disorders [28,29]. Evidence also showed that extreme cold temperature is strongly associated with cardiorespiratory outcomes and amplifies the hazards of hypothermia and traffic accidents [30,31]. Findings from some studies indicated higher susceptibility at the onset of hot or cold seasons when the human body has not yet acclimatised to extreme meteorological conditions [32]. Populations living in cold areas may be more susceptible to high temperatures than those in hot areas due to a lack of long-term adaptation and less awareness of the effects of extreme heat.
3.1.2. Droughts
There have been 770 records of severe droughts since 1900, causing 38 million deaths [13]. Droughts are associated with extremely low precipitation, high evaporation and hot temperature, which may further increase the risk of dust storms, water insecurities, wildfires, food shortages and other health-related events. For example, dust storms may affect human health by carrying PMs, anthropogenic pollutants (e.g., dioxins, pesticides, and radioactive isotopes), and biomaterials [33]. The damage of dust storms may vary by geographic location. For example, researchers found that inhaling contaminated particles may contribute to valley fever in America, meningitis in West Africa, measles in Western China, and conjunctivitis in Asia [[34], [35], [36]].
Globally, four billion people experience severe water scarcity for at least one month each year [37]. Droughts may deteriorate water scarcity and water insecurity, increasing the risk of diarrhoea—the second leading cause of death, responsible for 525,000 global deaths each year in children under five [38]. In certain regions, every 10-mm decline in precipitation is associated with a 4% increase in diarrhoea incidence, while per 1 °C increase in temperature links to a 3%–11% increase in excess deaths from diarrhoea [39,40]. In 2050, there will be 320,000 deaths due to diarrhoea, of which 12% can be attributed to climate change, with 95% of cases occurring in Sub-Saharan Africa and South Asia [40]. Like other natural disasters, droughts may trigger conflicts and population migrations because of environmental deterioration and a shortage of essential resources [41,42].
3.1.3. Wildfires
In addition to drought, high temperature and low precipitation can increase the risk of wildfire, extending fire season and burning time in some areas. Other climatic conditions, such as El Niño-Southern Oscillation (ENSO) are also associated with frequent droughts and wildfires in some coastal regions [43]. Direct health impacts of wildfire events include burns, injuries, mental health effects, and premature deaths [44]. Choking on gas and dust due to wildfire causes 339,000 additional deaths annually, far beyond the number directly caused by wildfires [45]. Wildfire smoke also contains toxic components, such as particulate matters (PMs) and nitrogen oxides (NOx) [46]. Studies have suggested a consistent association between the level of fire-induced PMs and the risks of death and hospitalisation from all causes, including cardiovascular and respiratory causes [47,48]. Some components, such as free radicals and benzene, are multi-organically toxic, leading to lesions and even malignancy of the digestive, hemopoietic, and reproductive systems [46]. Increased greenhouse gas emissions from burning and decreased biodiversity from forest loss are likely to worsen climate change [49].
3.1.4. Floods and storms
Floods are usually caused by heavy rainfalls, storms and sea-level rise. Floods and storms are the most common and destructive natural disasters worldwide [50,51]. Between 1900 and 2015, there were more than 4500 records of floods, causing almost 90 million homelessness and 7 million deaths [52]. Besides injuries and drownings, threats continue after flooding. Studies have shown an increased short- and long-term risk of mortality and aggravation of non-communicable diseases in flood-stricken populations in the first year [53,54]. Pollutants deposited in the environment, such as river sediment and sewage, may be flushed out due to the flood. The overflow of sewers may contaminate drinking water and agricultural soil and water with chemicals, pharmaceutical ingredients and pathogens. Floods worsened the hygiene condition by destroying public facilities, increasing the risk of water- and vector-borne diseases. Heavy rainfalls and receding floodwater provided breeding sites for disease vectors, facilitating the transmission of malaria, dengue fever, yellow fever, and West Nile fever [55]. There were also reports regarding infections associated with ears, eyes, nose, skin, and respiratory and gastrointestinal tracts after flooding [56]. Moreover, the relationship between flood and mental disorders was also well documented, e.g., post-traumatic stress disorders (PTSD), depression, anxiety, and stress. Some studies estimated that the incidence of mental disorders might vary between 8.6% and 53% in the first two years after flooding [57]. Mental and physical disorders derived from floods may also affect maternal and offspring health, such as preterm birth, low birth weight, and impaired social functioning in their children [58,59].
Storms, such as hurricanes and tropical storms, could also significantly affect the environment and human health. It has been estimated that tropical cyclones have caused about 1.33 million deaths since the beginning of the 20th century, with more than 629 million people affected [60]. Similar to floods, in addition to the instant injuries directly caused by storms [61], studies have demonstrated an increased short-term risk of hospitalisations due to respiratory, infectious, and parasitic diseases and preterm birth [51,62]. Higher risks of mental disorders, such as acute stress, sleep disorder, and PTSD, have also been reported in storm-stricken populations by recent studies [59,63].
3.2. Ground-level air pollution
The effects of both short- and long-term air pollution exposures on cardiovascular mortality and morbidity have been ascertained according to previous controlled human exposure and epidemiological and animal toxicological studies [64]. The respiratory effects of air pollution exposure have been well investigated by large cohort studies, indicating that air pollution exposure causes decrements in lung function growth in children, lung function decline in adults, asthma, chronic obstructive pulmonary disease, lung cancer and respiratory death [[65], [66], [67], [68], [69], [70], [71], [72]]. Furthermore, accumulating evidence demonstrated that high exposure to air pollution could increase the mortality and the risk of endocrine diseases, metabolic diseases, nervous system diseases, reproductive diseases and cancer [69,[72], [73], [74]].
Climatic factors may be involved in the pathway from air pollution to human health [75,76]. High temperature promotes the chemical transformations of some air pollutants (e.g., the photochemical synthesis of ozone); air-stagnation episodes inhibit the dilution and dispersion of air pollutants, while rainfalls accelerate the deposition of air pollutants. On the other hand, climatic factors can influence an individual’s behaviour, which determines the way of exposure to air pollution. For example, in high latitude areas, a higher annual temperature may result in more days with an optimal temperature, on which outdoor activity will be encouraged, and individuals may be exposed to air pollution for a longer period. On the contrary, frequent rainfalls will result in a longer indoor time, which limits the exposure to outdoor air pollution but may amplify the effects of indoor air pollution. Some studies indicated that the adverse health effects of PM10, sulphur dioxide and nitrogen dioxide are more severe during cold days, while other studies had opposite findings [77]. It should be noted that air pollution can also significantly affect regional climate through aerosol direct effects (e.g., scattering or absorbing radiation) and aerosol indirect effects (e.g., participating in cloud formation), in addition to its role in global warming [78].
3.3. Temperature rise
3.3.1. Vector-borne diseases
The survival and proliferation of pathogens and vectors may increase in a warming world, resulting in more epidemics of vector-borne diseases, mainly transmitted by arthropod vectors [79]. An extended warm season prolongs the epidemic period and enlarges the geographic distribution. Warmer temperature promotes oviposition and shortens egg incubation of vectors, and increases the risk behaviour of human beings, such as less dressing. Humidity is also associated with disease transmission by affecting the lifespan of vectors [80]. For example, female mosquitos may have a reduced size and wingspan in a warm environment with high humidity and require more frequent biting to survive [81]. Recent studies have projected that epidemics of vector-borne diseases are likely to rise in the following decades [82], in 2050, climate change will bring 33,000 additional deaths, with 97% occurring in East Sub-Saharan Africa and South Asia. It has been estimated that over 6.1 billion people will be at risk of mosquito-borne dengue fever in 2080, accounting for 60% of the world’s population [83].
3.3.2. Allergens
The earlier onset of warm days in spring and delayed arrival of cold days extend the flowering period. In North America, elevated temperature and carbon dioxide concentration have resulted in a 20-day-earlier, 8-day-longer season of allergenic pollen, accompanied by a 21% increase in the level of annual pollen concentration between 1990 and 2018 [84]. A higher pollen concentration may be related to allergic rhinitis, asthma, hay fever and other allergic symptoms [85,86]. Oceanfront houses with rising sea levels and water-intruded houses after heavy rainfalls, storms and floods become damp and moist, increasing the growth of fungi and moulds indoors during warm days and thus leading to health problems such as respiratory allergies, asthma and rhinitis [87,88].
3.3.3. El Niño, La Niña & Oceanic Oscillation pattern
Abnormal sea temperature and monsoon induced by global warming and other natural disasters may distract ocean currents and trigger certain events, such as El Niño, La Niña and Oceanic Oscillation patterns [89,90]. El Niño and La Niña contribute to the anomalies of temperature, precipitation and air pressure, which further cause natural or artificial disasters, e.g., droughts, floods, wildfires, storms and displacements. ENSO may also be associated with diarrhoeal diseases, especially cholera [91,92]. A previous study has also found that ENSO was likely to contribute to the outbreaks of dengue fever and malaria in some regions [93,94]. For example, a 1 °C change in sea surface temperature, i.e., a weak ENSO, was linked to a 20% increase in malaria in Colombia [94]. Similarly, La Niña has also been reported to be associated with an increased risk of epidemics such as malaria and infection of shigellosis and leptospirosis [91,95,96].
3.4. Food insecurity
3.4.1. Crops
Climate change is projected to negatively affect food production and security in all aspects of the food system (availability, access, utilisation and stability) and their interactions. Extreme weather-related disasters, including droughts, heavy rainfalls, windstorms, floods and hails, are increasing, thus reducing the yields of major crops [97]. Besides, high moisture and temperature may proliferate pests and weeds, threatening food production and causing famine in some regions. Similarly, high indoor humidity results in food contamination via aflatoxin and other toxins of fungi and mould [98]. It has been estimated that 720–811 million individuals faced hunger in 2020 [99]. Consequently, human health is under threat due to the lack of sufficient nutrients to maintain life or being more susceptible to infectious diseases. By 2050, climate change will reduce 3.2% of global food availability per person, causing 529,000 additional deaths worldwide due to changes in dietary and weight-related factors [100]. Moreover, reduced food yield increases the use of fertilisers, herbicides and pesticides, further contaminating soil and water. Crops growing from contaminated soil and irrigation water can result in a broad range of food-borne diseases [101]. Last but not least, the global food system generates greenhouse gas emissions from multiple sources, with an average of 16 billion tonnes of CO2 equivalents per year from 2012 to 2017 [102].
3.4.2. Fishery and aquaculture
Fish products provide 17% of animal protein intake and 7% of all proteins for the global population [103]. Climate change may affect the production ecology and biodiversity of aquatic systems, resulting in reduced production and yield, as well as changes in species composition in catches and geographic distribution. These changes are also affecting the socioeconomic status of the fisheries and aquaculture sector in many parts of the world [104]. Previous studies have estimated that the fishery yield may increase in some mid- and high-latitude regions but decrease in tropical areas because of global warming [105,106]. High sea surface temperature is a crucial environmental variable for the distribution, proliferation, toxicity and duration of harmful algal blooms (HABs) along certain coastlines [107]. The paralytic shellfish toxins (PSTs) excreted by HABs can cause deadly muscle paralysis and vomiting [108,109]. Besides, high sea surface temperature is likely to accelerate the proliferation of waterborne pathogens alongside coastlines, such as Vibrio cholera, vulnificus and parahaemolyticus. Consuming contaminated seafood can result in infections, including diarrhoea, septicaemia and even death. In addition to marine fishery, climate change may also shift the ecosystems of inland lakes and therefore affect the freshwater fishery. For example, a previous study investigated the long-term thermal change in 139 lakes across six continents, showing a 6.3% non-overlap between thermal habitats in baseline (1978–1995) and recent (1996–2013) periods [110]. Another study has estimated that 4%, 9% and 36% of freshwater fish species will have over half of their present-day geographic range exposed to climatic extremes in the future world with a 1.5 °C, 2 °C and 3.2 °C warmer global mean temperature, respectively [111].
4. Possible benefits of climate change on human health
Despite climate change being associated with a range of adverse health outcomes, certain climatic conditions may have some benefits [112]. For example, although rainfalls and floods may trigger vector-borne diseases in tropical and subtropical regions, heavy events may reduce disease outbreaks by destroying the habitats of vectors and their eggs. Similarly, some dry and low-latitude regions are projected to experience less precipitation due to climate change, which may reduce the density of insects, and hence, the prevalence of vector-borne diseases.
Climate change is also likely to reduce the prevalence of diseases and mortality associated with cold temperatures in certain countries and regions [113]. For example, with rising temperatures, labour productivity in countries with low baseline temperatures may increase, thus reducing cold-related labour loss [114]. In addition, certain countries may have less excess deaths associated with extreme cold ambient temperature in this warming world [113]. However, it remains inconsistent whether the decline in cold-related deaths can offset the increase in heat-related mortality in certain areas. Moreover, the positive effects of climate change vary substantially by geographical locations and tend to be short-term, which may be quickly outweighed by negative effects [115].
Warming temperature accelerates the melt of glaciers, thus providing more drinking and agricultural water for populations living in glacial-fed water catchments [112]. Longer warm days provide an extended period for plant growth, while a higher atmospheric concentration of CO2 increases photosynthesis by providing extra carbon sources. Over the last 35 years, 25%–50% of the vegetated land in the world has shown a greening trend largely due to the CO2 fertilisation effect [116]. The greening trend is more profound in high northern latitudes and northern temperate regions [117]. Increasing greening may also benefit human health as higher surrounding greenness is associated with a lower risk of many ageing-related diseases [118]. It should be noted that plants’ capacity to absorb nitrogen and minerals, such as zinc and iron, is expected to decline in some regions because of acid rain, leading to unbalanced food production, which may offset the benefit of climate change. Besides, extended precipitation may lead to delays in production processes [119]. For the marine fisheries and aquaculture sector, climate change may cause geographic shifts in fishery resources, with some regions in high latitudes experiencing an increase in productivity [120].
5. The impacts of socioeconomic, demographic and environmental factors on the pathways
The modifying effects of non-climatic factors on the climate change-health pathways should not be overlooked. Table 1 summarises some major modifiers, including age, sex, economic level, social status, education, land use, location, public health policy and public attitude.
Table 1.
The main influence of major socioeconomic, demographic and environmental factors on the pathways between climate change and human health.
| Aspects | Variables | Impacts |
|---|---|---|
| Demographic | Age |
Children and the elderly
|
| Sex |
Women
|
|
| Socioeconomic | Socioeconomic and educational level |
The poverty
|
| Public health policy |
Inactive policy
|
|
| Public attitude towards climate change |
Negative attitude Response to climate change: passive attitude – less effective mitigation and adaptation. |
|
| Environmental | Land use |
Unbalanced ecosystem
|
| Topographic character |
Certain regions
|
Specific populations are particularly vulnerable to climate change, partly due to socioeconomic inequalities, cultural norms, or intrinsic physiological factors. For example, aged populations and children are especially vulnerable to suboptimal temperatures due to impaired or immature thermoregulatory capacities [121]. New-borns and children have lower resistance to extreme disasters, pathogens, toxins and undernutrition and higher exposure per unit of weight to risk factors. Lower socioeconomic status often puts poor people at higher risk and reduces access to sufficient food and fresh water, high-quality medical services, and safe shelters against ETEs, floods and other natural disasters associated with climate change [112,122,123]. Health impacts of climate change also exhibit sex differences. Education levels, biological differences, social roles and activity patterns make women more vulnerable to environmental hazards [124]. The sex gap tends to be larger in countries where gender inequalities are particularly significant. Specific occupations may be particularly susceptible to climate change, such that farmers and construction workers have higher exposure to ETEs than others [125,126]. Certain places, such as cities, coastlines, plains and basins, may experience increased risks of heatwaves, floods, storms and droughts [127,128], which threaten human health through air pollution, infectious disease, food insecurity and undernutrition. Humans are experiencing an explosion in population size so that the global population by 2050 will be 29% larger than the 2011 level [129,130]. Agricultural production is one of the main sources of greenhouse gases. A larger population also means higher food demand and more anthropogenic activities, which irreversibly affect the climate, and eventually, show their joint impacts on human health. Therefore, non-climatic conditions can interact with each other and modify climate-health pathways.
6. Possible solutions
6.1. Mitigation
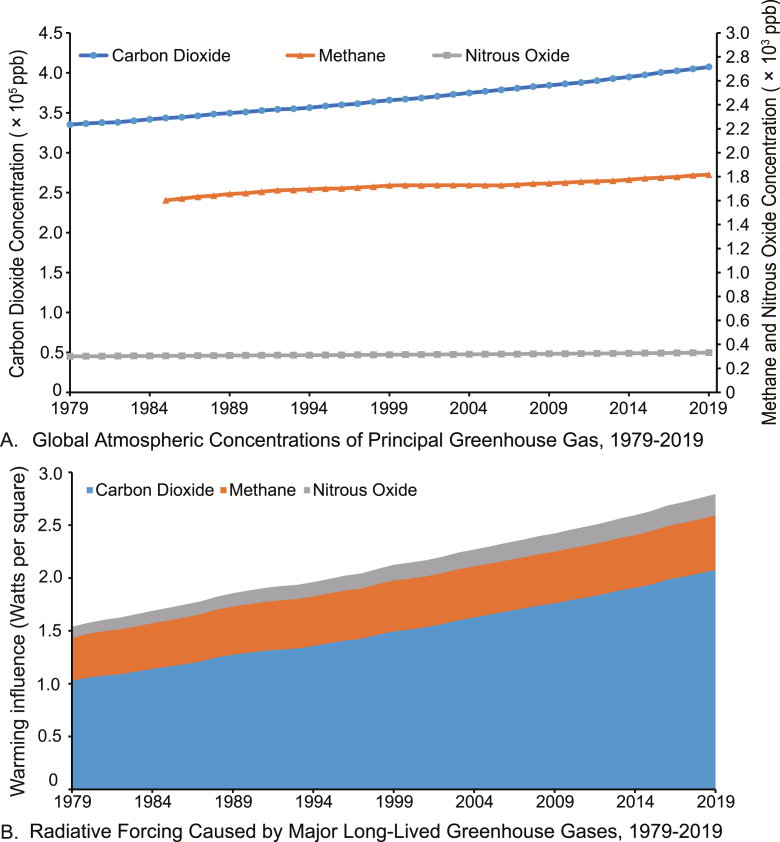
Global greenhouse gas emissions continued to grow to a record high of 52.4 gigatons of CO2 equivalent (GtCO2e; 59.1 GtCO2e, including land-use change) in 2019, with fossil CO2 reaching a record of 38.0 GtCO2e (72.5%), mainly originating from the main activity sectors (including power industry, combustion for industrial manufacturing and fuel production, transport, buildings and other sectors) [131]. Atmospheric concentrations of major greenhouse gases (CO2, CH4 and N2O) have increased dramatically over the last decades, with the emission of CO2 over 200 times and 1200 times higher than that of CH4 and N2O, respectively in 2019 (Fig. 2A). The degradation of CH4 and N2O may take decades, whereas CO2 exists in the atmosphere steadily [132]. The radiative forcing of the three gases was 2.8 in 2019, 48.5% higher than it was in 1990 (Fig. 2B). CO2 accounted for 74.3% of radiative forcing, with the rest shared by CH4 (18.5%) and N2O (7.2%).
Fig. 2.
Global anthropogenic greenhouse gas emissions and radiative forcing in 1979–2019. Data are collected from the United States Environmental Protection Agency [133,134].
Mitigation strategies are highly associated with atmospheric concentrations, lifetime and global warming influence of greenhouse gases, and their anthropogenic sources. Current estimates in Asia reported that air pollution reduction brought by mitigation actions under the 2 °C goal could decrease premature deaths by 0.79 million by 2050, with the mitigation co-benefits decidedly more than the cost [135].
6.1.1. Reducing human emission
Although global CO2 emission has been projected to decrease in 2020 compared with 2019 emission levels because of COVID-19 [136,137], countries should strengthen their mitigation commitments in order to achieve the Paris Agreement’s long-term target of limiting global mean temperature increase to well below 2 °C [137]. Fossil fuel burning contributes the most to air pollution, which, in total, kills over 6 million people every year [9]. Globally, a phase-out of fossil fuel use can prevent an excess mortality rate of 3.61 million annually from outdoor air pollution [138]. Coal, oil and gas, the three most widely used fossil fuels, account for 85% of anthropogenic CO2 emissions. These fossil fuels are mainly consumed by electricity generation, heating, transportation and industrial production. From an energy supply aspect, transferring to clean and renewable energies such as solar, wind, geothermal and wave energy can effectively mitigate the emission burden. Strategies from an energy end-use aspect can contribute to the target of cutting down emissions, e.g., promoting and increasing investments in clean energy and adding health tax to energy prices. Transportation is responsible for 24% of the CO2 emissions from fuel combustion. To this end, effective actions should be taken, such as phasing out the internal combustion engine, reducing private car usage, encouraging walking, cycling and public transport, as well as creating people-centred cities with convenient public transport and high walkability to blue and green spaces. Since coal mining and gas and oil consumption produce one-third of atmospheric CH4, reducing the use of fossil fuels also mitigates the CH4 emission challenge. Given agriculture is another major source of CH4, changing cultivating strategy and food structure (e.g., improving livestock management, decreasing food waste and loss and adopting healthy and predominantly plant-based diets) can be more significant for cutting down CH4 emissions. Improving techniques for waste processing is another way to decrease CH4 concentration. Mitigation strategies of CH4 also effectively reduce N2O emissions because the two greenhouse gases share certain sources.
6.1.2. Sinking or artificially removing atmospheric greenhouse gas
It is estimated that 61% of anthropogenic emissions of CO2 during 2010–2019 were removed via natural sink (35% by land and 26% by oceans, respectively) [139]. Forests and other green spaces are the main force for the land sink of CO2. Therefore, reforestation may reduce the atmospheric concentration of CO2 by increasing carbon sink, and so do algal blooms. Developing new technology to directly filter CO2 out from the atmosphere is also a practical way.
6.1.3. Co-benefits of mitigation actions
The health co-benefits of mitigation actions can be obtained via various pathways. For example, facilitating cycling or walking is beneficial to human health by increasing physical activity and improving air quality via reducing fossil fuel combustion. Such efforts can achieve a reduction in adverse health outcomes (e.g., morbidity and mortality) related to air pollution (e.g., asthma), physical inactivity (e.g., obesity) and traffic noise (e.g., anxiety) [112,140,141]. Similarly, the promotion of residential greenness not only facilitates climate mitigation but also provides health co-benefits, such as increasing physical activities, improving mental health and reducing all-cause mortality [142]. Besides, energy prices, considering healthcare costs, may reduce the emission of greenhouse gases by over 20% and cut down deaths associated with outdoor air pollution by approximately 33% [143]. Given livestock farming consumes a large proportion of cereals, reducing meat consumption or increasing cultured meat may help ease food shortage. Last but not least, changing the current emission pathway to the RCP4.5 scenario will save around 500,000 lives per year by 2030 [52].
6.2. Adaptation
6.2.1. General response
The adaptation strategies usually include four aspects: 1) to regularly assess health vulnerabilities and adaptation capacities, 2) to develop and implement an evidence-based adaptation plan for health, 3) to strengthen the climate resilience and environmental sustainability of healthcare systems and facilities,4) to protect health and advance climate justice by implementing health-promoting interventions in other sectors. More modules should be integrated into the early warning system, e.g., early forecasting extreme weather, predicting climate-related diseases, estimating possible health risks, evaluating damage levels, proposing preventative strategies, providing medical and rescue plans and establishing a program for post-disaster reconstruction [144].
6.2.2. Specific actions
Specific actions can be taken at different levels to adapt to the impacts of climate change [145,146]. At the social level, public health systems and policies are critical, e.g., providing financial support and disaster-coping education for vulnerable populations. At the behavioural level, enhanced living conditions may reduce the impacts of extreme weather events. For example, a large number of deaths occurred in the elderly population during the 2003 European heatwave event, which could have been lessened if nursing homes and communities had been equipped with air conditioning [147]. At the physical level, increasing the coverage of green plants can promote the absorption of heat in cities. Greenspace may also reduce the morbidity of numerous disorders by blocking traffic noise, refreshing air quality, and providing sporting areas [148]. In addition, the urban areas are mainly made up of buildings, which contribute to the urban heat island. Some studies have provided certain primary evidence that urban adaptations, e.g., green roofs, cool walls and cool pavement, can effectively control urban climate, which may further cushion the adverse effect of extreme temperature events [149,150]. For example, a study in Sydney found that the peak indoor temperatures for buildings with or without green roofs and green walls were 27.7 °C and 34.6 °C, respectively [151]. Another study in China reported that the 2-m surface temperature in summer reduced up to 0.74 K and 1.19 K for green roofs and cool roofs, respectively [152]. Dams and reservoirs can protect people from floods and coastal storms, benefit commercial fishery and defend against droughts. Therefore, some physical-level adaptations not only reduce the impact of certain climatic conditions but also comprehensively enhance human health by maintaining a more comfortable environment and ecosystem.
7. Conclusions
To date, the signs of climate change are increasingly obvious, including ETEs, floods, storms and other climatic or natural disasters. These events affect human health from non-communicable diseases, infections, injuries to mental disorders, food insecurity and other issues through a variety of pathways. Certain socioeconomic, demographic and environmental factors may modify the pathways between climate change and health. Although climate change plays an adverse role at the global level, it can also benefit certain regions by improving local liveable ecosystems. For reducing the health threat due to climate change, mitigation and adaptation actions should be adopted at various levels, which may bring some co-benefits.
Declaration of competing interests
The authors have declared no conflicts of interest.
Acknowledgements
This study was supported by the Australian Research Council (DP210102076), Australian National Health and Medical Research Council (APP2000581), Asian Development Bank, the Natural Science Foundation of Shandong Province China (ZR2021QH318), and the Shandong Excellent Young Scientists Fund Program (Overseas) (2022HWYQ-055). YG was supported by a Career Development Fellowship of the Australian National Health and Medical Research Council (APP1163693). SL was supported by an Early Career Fellowship of the Australian National Health and Medical Research Council (APP1109193). QZ was supported by the Program of Qilu Young Scholars of Shandong University, China. PY, WH, YG, BW, YW and TY were supported by China Scholarship Council funds (No. 201906210065 for PY, 202006380055 for WH, 202008110182 for YG, 202006010043 for BW, and 202006010044 for YW, and 201906320051 for TY).
Contributor Information
Shanshan Li, Email: shanshan.li@monash.edu.
Yuming Guo, Email: yuming.guo@monash.edu.
References
- 1.Allan R.P., Arias P.A., Berger S., Canadell J.G., Cassou C., Chen D.L., Cherchi A., Connors S.L., Coppola E., Cruz F.A., et al. Cambridge University Press; 2021. Summary for Policymakers. Climate Change 2021: The Physical Science Basis: Working Group I Contribution to the Sixth Assessment Report of IPCC. [Google Scholar]
- 2.Allen M., Antwi-Agyei P., Aragon-Durand F., et al. Intergovernmental Panel on Climate Change; 2019. Technical Summary: Global Warming of 1.5° C. An IPCC Special Report on the Impacts of Global Warming of 1.5° C Above Pre-Industrial Levels and Related Global Greenhouse Gas Emission Pathways, in The Context of Strengthening the Global Response to the Threat of Climate Change, Sustainable Development, and Efforts to Eradicate Poverty. [Google Scholar]
- 3.Romanello M., McGushin A., Napoli C.D., Drummond P., Hughes N., Jamart L., Kennard H., Lampard P., Rodriguez B.S., Arnell N., et al. The 2021 report of the Lancet Countdown on health and climate change: code red for a healthy future. Lancet. 2021;398:1619–1662. doi: 10.1016/S0140-6736(21)01787-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pörtner H.-O., Roberts D.C., Poloczanska E.S., Mintenbeck K., Tignor M., Alegría A., Craig M., Langsdorf S., Löschke S., Möller V., et al. Cambridge University Press/UNEP; 2022. Summary for Policymakers. Climate Change 2022-Impacts, Adaptation and Vulnerability: Working Group II Contribution to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change. [Google Scholar]
- 5.Vicedo-Cabrera A.M., Scovronick N., Sera F., Royé D., Schneider R., Tobias A., Astrom C., Guo Y., Honda Y., Hondula D.M., et al. The burden of heat-related mortality attributable to recent human-induced climate change. Nat. Clim. Change. 2021;11:492–500. doi: 10.1038/s41558-021-01058-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Perera A.T.D., Nik V.M., Chen D., Scartezzini J.L., Hong T. Quantifying the impacts of climate change and extreme climate events on energy systems. Nat. Energy. 2020;5:150–159. doi: 10.1038/s41560-020-0558-0. [DOI] [Google Scholar]
- 7.Lemery J., Knowlton K., Sorensen C. John Wiley & Sons; 2021. Global Climate Change and Human Health: From Science to Practice. [Google Scholar]
- 8.McKinnon M. Estudios Gráfcos Europeos, SA; Spain: 2012. Climate Vulnerability Monitor: A Guide to the Cold Calculus of a Hot Planet; p. 331. [Google Scholar]
- 9.Murray C.J.L., Aravkin A.Y., Zheng P., Abbafati C., Abbas K.M., Abbasi-Kangevari M., Abd-Allah F., Abdelalim A., Abdollahi M., Abdollahpour I., et al. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1223–1249. doi: 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhao Q., Guo Y., Ye T., Gasparrini A., Tong S., Overcenco A., Urban A., Schneider A., Entezari A., Vicedo-Cabrera A.M., et al. Global, regional, and national burden of mortality associated with non-optimal ambient temperatures from 2000 to 2019: a three-stage modelling study. Lancet Planet. Health. 2021;5:e415–e425. doi: 10.1016/S2542-5196(21)00081-4. [DOI] [PubMed] [Google Scholar]
- 11.Zhao Q., Li S., Coelho M.S.Z.S., Saldiva P.H.N., Hu K., Huxley R.R., Abramson M.J., Guo Y. The association between heatwaves and risk of hospitalization in Brazil: a nationwide time series study between 2000 and 2015. PLoS Med. 2019;16 doi: 10.1371/journal.pmed.1002753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berkeley Earth Global temperature report. http://berkeleyearth.org/global-temperature-report-for-2020/
- 13.Centre for Research on the Epidemiology of Disasters EM-DAT: The CRED/OFDA international disaster database. https://public.emdat.be/
- 14.National Oceanic and Atmospheric Administration Climate at a glance: Time series. http://www.ncdc.noaa.gov
- 15.Merrifield M.A., Leuliette E., Thompson P., et al. 2016. Sea Level Variability and Change. [in "State of the Climate in 2015"] [Google Scholar]
- 16.Matthews H.D., Zickfeld K. Climate response to zeroed emissions of greenhouse gases and aerosols. Nat. Clim. Change. 2012;2:338–341. doi: 10.1038/nclimate1424. [DOI] [Google Scholar]
- 17.Chen Z., Zhou T., Zhang L., Chen X., Zhang W., Jiang J. Global land monsoon precipitation changes in CMIP6 projections. Geophys. Res. Lett. 2020;47 doi: 10.1029/2019GL086902. [DOI] [Google Scholar]
- 18.Hirabayashi Y., Mahendran R., Koirala S., Konoshima L., Yamazaki D., Watanabe S., Kim H., Kanae S. Global flood risk under climate change. Nat. Clim. Change. 2013;3:816–821. doi: 10.1038/nclimate1911/. [DOI] [Google Scholar]
- 19.Hartmann Amgkt Dennis L., Rusticucci Matilde, Alexander Lisa V., Brönnimann Stefan, Charabi Yassine Abdul-Rahman, Dentener Frank J., Dlugokencky Edward J., Easterling David R., Kaplan Alexey, Soden Brian J., et al. In: Climate Change 2013: The Physical Science Basis Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Stocker T.F., Qin D., Plattner G.-K., et al., editors. Cambridge University Press; Cambridge, UK and New York, NY, USA: 2013. Observations: atmosphere and surface; pp. 159–254. [Google Scholar]
- 20.Matthew Collins R.K., Arblaster Julie, Dufresne Jean-Louis, Fichefet Thierry, Friedlingstein Pierre, Gao Xuejie, Gutowski William J., Jr., Johns Tim. In: Climate Change 2013: The Physical Science Basis Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Stocker T.F., Qin D., Plattner G.-K., et al., editors. Cambridge University Press; Cambridge, UK and New York, NY, USA: 2013. Long-term climate change: projections, commitments and irreversibility; pp. 1029–1136. [Google Scholar]
- 21.Marsooli R., Lin N., Emanuel K., Feng K. Climate change exacerbates hurricane flood hazards along US Atlantic and Gulf Coasts in spatially varying patterns. Nat. Commun. 2019;10:3785. doi: 10.1038/s41467-019-11755-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guo Y., Gasparrini A., Armstrong B., Li S., Tawatsupa B., Tobias A., Lavigne E., de Sousa Zanotti Stagliorio Coelho M., Leone M., Pan X., et al. Global variation in the effects of ambient temperature on mortality: a systematic evaluation. Epidemiology. 2014;25:781–789. doi: 10.1097/EDE.0000000000000165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sun Z., Wang Q., Chen C., Yang Y., Yan M., Du H., Chen K., Ji J.S., Li T. Projection of temperature-related excess mortality by integrating population adaptability under changing climate—China, 2050s and 2080s. China CDC Weekly. 2021;3:697–701. doi: 10.46234/ccdcw2021.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ebi K.L., Capon A., Berry P., Broderick C., de Dear R., Havenith G., Honda Y., Kovats R.S., Ma W., Malik A., et al. Hot weather and heat extremes: health risks. Lancet. 2021;398:698–708. doi: 10.1016/S0140-6736(21)01208-3. [DOI] [PubMed] [Google Scholar]
- 25.Tian Y., Liu H., Si Y., Cao Y., Song J., Li M., Wu Y., Wang X., Xiang X., Juan J., et al. Association between temperature variability and daily hospital admissions for cause-specific cardiovascular disease in urban China: a national time-series study. PLoS Med. 2019;16 doi: 10.1371/journal.pmed.1002738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lu P., Xia G., Zhao Q., Xu R., Li S., Guo Y. Temporal trends of the association between ambient temperature and hospitalisations for cardiovascular diseases in Queensland, Australia from 1995 to 2016: a time-stratified case-crossover study. PLoS Med. 2020;17 doi: 10.1371/journal.pmed.1003176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wu Y., Xu R., Wen B., Coelho M., Saldiva P.H., Li S., Guo Y. Temperature variability and asthma hospitalisation in Brazil, 2000-2015: a nationwide case-crossover study. Thorax. 2021;76:962–969. doi: 10.1136/thoraxjnl-2020-216549. [DOI] [PubMed] [Google Scholar]
- 28.Kim Y., Kim H., Gasparrini A., Armstrong B., Honda Y., Chung Y., Ng C.F.S., Tobias A., Íñiguez C., Lavigne E., et al. Suicide and ambient temperature: a multi-country multi-city study. Environ. Health Perspect. 2019;127:117007. doi: 10.1289/EHP4898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Khan A.M., Finlay J.M., Clarke P., Sol K., Melendez R., Judd S., Gronlund C.J. Association between temperature exposure and cognition: a cross-sectional analysis of 20, 687 aging adults in the United States. BMC Publ. Health. 2021;21:1484. doi: 10.1186/s12889-021-11533-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang P., Wiens K., Wang R., Luong L., Ansara D., Gower S., Bassil K., Hwang S.W. Cold weather conditions and risk of hypothermia among people experiencing homelessness: implications for prevention strategies. Int. J. Environ. Res. Publ. Health. 2019;16:3259. doi: 10.3390/ijerph16183259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee H., Myung W., Kim H., Lee E.M., Kim H. Association between ambient temperature and injury by intentions and mechanisms: a case-crossover design with a distributed lag nonlinear model. Sci. Total Environ. 2020;746:141261. doi: 10.1016/j.scitotenv.2020.141261. [DOI] [PubMed] [Google Scholar]
- 32.Zhao Q., Li S., Coelho M.S.Z.S., Saldiva P.H.N., Hu K., Abramson M.J., Huxley R.R., Guo Y. Assessment of intraseasonal variation in hospitalization associated with heat exposure in Brazil. JAMA Netw. Open. 2019;2 doi: 10.1001/jamanetworkopen.2018.7901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fussell J.C., Kelly F.J. Mechanisms underlying the health effects of desert sand dust. Environ. Int. 2021;157:106790. doi: 10.1016/j.envint.2021.106790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tong D.Q., Wang J.X.L., Gill T.E., Lei H., Wang B. Intensified dust storm activity and Valley fever infection in the southwestern United States, Geophys. Res. Lett. 2017;44:4304–4312. doi: 10.1002/2017GL073524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ma Y., Zhou J., Yang S., Zhao Y., Zheng X. Assessment for the impact of dust events on measles incidence in Western China. Atmos. Environ. 2017;157:1–9. doi: 10.1016/j.atmosenv.2017.03.010. [DOI] [Google Scholar]
- 36.Ko R., Hayashi M., Hayashi H., Hayashi K., Kato H., Kurata Y., Fuchino Y., Nakamichi T., Migita H., Yano H., et al. Correlation between acute conjunctivitis and Asian dust on ocular surfaces. J. Toxicol. Environ. Health. 2016;79:367–375. doi: 10.1080/15287394.2016.1162248. [DOI] [PubMed] [Google Scholar]
- 37.UNICEF Water Scarcity: Key Facts. https://www.unicef.org/wash/water-scarcity 2020 2021.
- 38.WHO Fact Sheet . 2017. WHO: Diarrhoeal Disease.https://www.who.int/news-room/fact-sheets/detail/diarrhoeal-disease 02.05.2017 2017. [Google Scholar]
- 39.Lloyd S.J., Kovats R.S., Armstrong B.G. Global diarrhoea morbidity, weather and climate. Clim. Res. 2007;34:119–127. doi: 10.3354/cr034119. [DOI] [Google Scholar]
- 40.Sari Kovats S.L. World Health Organization; 2014. Diarrhoeal Disease [in “Quantitative Risk Assessment of the Effects of Climate Change on Selected Causes of Death, 2030s and 2050s”] pp. 37–50. [Google Scholar]
- 41.Hermans K., Garbe L. Droughts, livelihoods, and human migration in northern Ethiopia. Reg. Environ. Change. 2019;19:1101–1111. doi: 10.1007/s10113-019-01473-z. [DOI] [Google Scholar]
- 42.Adaawen S., Rademacher-Schulz C., Schraven B., Segadlo N. In: Drought Challenges. Mapedza E., Tsegai D., Bruntrup M., McLeman R., editors. Elsevier; Amsterdam: 2019. Drought, migration, and conflict in sub-Saharan Africa: what are the links and policy options? pp. 15–31. [DOI] [Google Scholar]
- 43.Cardil A., Rodrigues M., Ramirez J., De-Miguel S., Silva C.A., Mariani M., Ascoli D. Coupled effects of climate teleconnections on drought, Santa Ana winds and wildfires in southern California. Sci. Total Environ. 2021;765:142788. doi: 10.1016/j.scitotenv.2020.142788. [DOI] [PubMed] [Google Scholar]
- 44.Xu R., Yu P., Abramson M.J., Johnston F.H., Samet J.M., Bell M.L., Haines A., Ebi K.L., Li S., Guo Y. Wildfires, global climate change, and human health. N. Engl. J. Med. 2020;383:2173–2181. doi: 10.1056/NEJMsr2028985. [DOI] [PubMed] [Google Scholar]
- 45.Johnston F.H., Henderson S.B., Chen Y., Randerson J.T., Marlier M., Defries R.S., Kinney P., Bowman D.M.J.S., Brauer M. Estimated global mortality attributable to smoke from landscape fires. Environ. Health Perspect. 2012;120:695–701. doi: 10.1289/ehp.1104422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Reisen F., Duran S.M., Flannigan M., Elliott C., Rideout K. Wildfire smoke and public health risk. Int. J. Wildland Fire. 2015;24:1029. doi: 10.1071/wf15034. [DOI] [Google Scholar]
- 47.Chen G., Guo Y., Yue X., Tong S., Gasparrini A., Bell M.L., Armstrong B., Schwartz J., Jaakkola J.J.K., Zanobetti A., et al. Mortality risk attributable to wildfire-related PM 2·5 pollution: a global time series study in 749 locations. Lancet Planet. Health. 2021;5:e579–e587. doi: 10.1016/S2542-5196(21)00200-X. [DOI] [PubMed] [Google Scholar]
- 48.Ye T., Guo Y., Chen G., Yue X., Xu R., Coêlho M., Saldiva P., Zhao Q., Li S. Risk and burden of hospital admissions associated with wildfire-related PM 2·5 in Brazil, 2000-15: a nationwide time-series study, Lancet Planet. Health. 2021;5:e599–e607. doi: 10.1016/S2542-5196(21)00173-X. [DOI] [PubMed] [Google Scholar]
- 49.Bowman D.M.J.S., Kolden C.A., Abatzoglou J.T., Johnston F.H., van der Werf G.R., Flannigan M. Vegetation fires in the anthropocene. Nat. Rev. Earth Environ. 2020;1:500–515. doi: 10.1038/s43017-020-0085-3. [DOI] [Google Scholar]
- 50.Rentschler J., Salhab M. The World Bank; 2020. People in Harm's Way: Flood Exposure and Poverty in 189 Countries. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Parks R.M., Anderson G.B., Nethery R.C., Navas-Acien A., Dominici F., Kioumourtzoglou M.A. Tropical cyclone exposure is associated with increased hospitalization rates in older adults. Nat. Commun. 2021;12:1545. doi: 10.1038/s41467-021-21777-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sari Kovats S.H., Lloyd Simon. World Health Organization; 2014. Introduction and Key Findings [in “Quantitative Risk Assessment of the Effects of Climate Change on Selected Causes of Death, 2030s and 2050s”] pp. 3–16. [Google Scholar]
- 53.Paterson D.L., Wright H., Harris P.N.A. Health risks of flood disasters. Clin. Infect. Dis. 2018;67:1450–1454. doi: 10.1093/cid/ciy227. [DOI] [PubMed] [Google Scholar]
- 54.Yan M., Wilson A., Peel J.L., Magzamen S., Sun Q., Li T., Anderson G.B. Community-wide mortality rates in Beijing, China, during the July 2012 flood compared with unexposed periods. Epidemiology. 2020;31:319–326. doi: 10.1097/EDE.0000000000001182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tiu L.A., Wahid W.E., Andriani W.Y., Mirnawati, Tosepu R. Literature review: impact of temperature and rainfall on incident malaria. IOP Conf. Ser. Earth Environ. Sci. 2021;755 doi: 10.1088/1755-1315/755/1/012084. [DOI] [Google Scholar]
- 56.Musacchio A., Andrade L., O'Neill E., Re V., O'Dwyer J., Hynds P.D. Planning for the health impacts of climate change: flooding, private groundwater contamination and waterborne infection - a cross-sectional study of risk perception, experience and behaviours in the Republic of Ireland. Environ. Res. 2021;194:110707. doi: 10.1016/j.envres.2021.110707. [DOI] [PubMed] [Google Scholar]
- 57.Alderman K., Turner L.R., Tong S. Floods and human health: a systematic review. Environ. Int. 2012;47:37–47. doi: 10.1016/j.envint.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 58.Hetherington E., Adhikari K., Tomfohr-Madsen L., Patten S., Metcalfe A. Birth outcomes, pregnancy complications, and postpartum mental health after the 2013 Calgary flood: a difference in difference analysis. PLoS One. 2021;16 doi: 10.1371/journal.pone.0246670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Haq I.U., Mehmood Z., Afzal T., Khan N., Ahmed B., Nawsherwan, Ali L., Khan A., Muhammad J., Khan E.A., et al. Prevalence and determinants of stunting among preschool and school-going children in the flood-affected areas of Pakistan. Braz. J. Biol. 2021;82 doi: 10.1590/1519-6984.249971. [DOI] [PubMed] [Google Scholar]
- 60.Doocy S., Daniels A., Murray S., Kirsch T.D. The human impact of floods: a historical review of events 1980-2009 and systematic literature review. PLoS Curr. 2013;5 doi: 10.1371/currents.dis.f4deb457904936b07c09daa98ee8171a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Konkel L. Tropical cyclone exposures and health: a new data set to assess associations over time. Environ. Health Perspect. 2020;128:124001. doi: 10.1289/EHP8653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sun S., Weinberger K.R., Yan M., Brooke Anderson G., Wellenius G.A. Tropical cyclones and risk of preterm birth: a retrospective analysis of 20 million births across 378 US counties. Environ. Int. 2020;140:105825. doi: 10.1016/j.envint.2020.105825. [DOI] [PubMed] [Google Scholar]
- 63.Tasdik Hasan M., Adhikary G., Mahmood S., Papri N., Shihab H.M., Kasujja R., Ahmed H.U., Azad A.K., Nasreen M. Exploring mental health needs and services among affected population in a cyclone affected area in costal Bangladesh: a qualitative case study. Int. J. Ment. Health Syst. 2020;14:12. doi: 10.1186/s13033-020-00351-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.EPA US . U.S. Environmental Protection Agency; 2019. Integrated Science Assessment (ISA) for Particulate Matter (Final Report, Dec 2019) [PubMed] [Google Scholar]
- 65.Gauderman W.J., Urman R., Avol E., Berhane K., McConnell R., Rappaport E., Chang R., Lurmann F., Gilliland F. Association of improved air quality with lung development in children. N. Engl. J. Med. 2015;372:905–913. doi: 10.1056/NEJMoa1414123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gauderman W.J., Avol E., Gilliland F., Vora H., Thomas D., Berhane K., McConnell R., Kuenzli N., Lurmann F., Rappaport E., et al. The effect of air pollution on lung development from 10 to 18 years of age. N. Engl. J. Med. 2004;351:1057–1067. doi: 10.1056/nejmoa040610. [DOI] [PubMed] [Google Scholar]
- 67.Chen J., Hoek G. Long-term exposure to PM and all-cause and cause-specific mortality: a systematic review and meta-analysis. Environ. Int. 2020;143:105974. doi: 10.1016/j.envint.2020.105974. [DOI] [PubMed] [Google Scholar]
- 68.Wang M., Aaron C.P., Madrigano J., Hoffman E.A., Angelini E., Yang J., Laine A., Vetterli T.M., Kinney P.L., Sampson P.D., et al. Association between long-term exposure to ambient air pollution and change in quantitatively assessed emphysema and lung function. JAMA. 2019;322:546–556. doi: 10.1001/jama.2019.10255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bettiol A., Gelain E., Milanesio E., Asta F., Rusconi F. The first 1000 days of life: traffic-related air pollution and development of wheezing and asthma in childhood. A systematic review of birth cohort studies. Environ. Health. 2021;20:46. doi: 10.1186/s12940-021-00728-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Liu S., Jørgensen J.T., Ljungman P., Pershagen G., Bellander T., Leander K., Magnusson P.K.E., Rizzuto D., Hvidtfeldt U.A., Raaschou-Nielsen O., et al. Long-term exposure to low-level air pollution and incidence of asthma: the ELAPSE project. Eur. Respir. J. 2021;57:2003099. doi: 10.1183/13993003.03099-2020. [DOI] [PubMed] [Google Scholar]
- 71.Park J., Kim H.J., Lee C.H., Lee C.H., Lee H.W. Impact of long-term exposure to ambient air pollution on the incidence of chronic obstructive pulmonary disease: a systematic review and meta-analysis. Environ. Res. 2021;194:110703. doi: 10.1016/j.envres.2020.110703. [DOI] [PubMed] [Google Scholar]
- 72.Yu P., Guo S., Xu R., Ye T., Li S., Sim M.R., Abramson M.J., Guo Y. Cohort studies of long-term exposure to outdoor particulate matter and risks of cancer: a systematic review and meta-analysis. Innovation (N Y) 2021;2:100143. doi: 10.1016/j.xinn.2021.100143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wu L., Jin L., Shi T., Zhang B., Zhou Y., Zhou T., Bao W., Xiang H., Zuo Y., Li G., et al. Association between ambient particulate matter exposure and semen quality in Wuhan, China. Environ. Int. 2017;98:219–228. doi: 10.1016/j.envint.2016.11.013. [DOI] [PubMed] [Google Scholar]
- 74.Chen H., Kwong J.C., Copes R., Hystad P., van Donkelaar A., Tu K., Brook J.R., Goldberg M.S., Martin R.V., Murray B.J., et al. Exposure to ambient air pollution and the incidence of dementia: a population-based cohort study. Environ. Int. 2017;108:271–277. doi: 10.1016/j.envint.2017.08.020. [DOI] [PubMed] [Google Scholar]
- 75.Fann N.L., Nolte C.G., Sarofim M.C., Martinich J., Nassikas N.J. Associations between simulated future changes in climate, air quality, and human health. JAMA Netw. Open. 2021;4 doi: 10.1001/jamanetworkopen.2020.32064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Hong C., Zhang Q., Zhang Y., Davis S.J., Tong D., Zheng Y., Liu Z., Guan D., He K., Schellnhuber H.J. Impacts of climate change on future air quality and human health in China. Proc. Natl. Acad. Sci. U.S.A. 2019;116:17193–17200. doi: 10.1073/pnas.1812881116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Areal A.T., Zhao Q., Wigmann C., Schneider A., Schikowski T. The effect of air pollution when modified by temperature on respiratory health outcomes: a systematic review and meta-analysis. Sci. Total Environ. 2022;811:152336. doi: 10.1016/j.scitotenv.2021.152336. [DOI] [PubMed] [Google Scholar]
- 78.Hong C., Zhang Q., Zhang Y., Davis S.J., Zhang X., Tong D., Guan D., Liu Z., He K. Weakening aerosol direct radiative effects mitigate climate penalty on Chinese air quality. Nat. Clim. Change. 2020;10:845–850. doi: 10.1038/s41558-020-0840-y/. [DOI] [Google Scholar]
- 79.Rocklöv J., Dubrow R. Climate change: an enduring challenge for vector-borne disease prevention and control. Nat. Immunol. 2020;21:479–483. doi: 10.1038/s41590-020-0648-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Craig M.H., Snow R.W., le Sueur D. A climate-based distribution model of malaria transmission in sub-Saharan Africa, Parasitol. Today Off. 1999;15:105–111. doi: 10.1016/s0169-4758(99)01396-4. [DOI] [PubMed] [Google Scholar]
- 81.Li T., Yang Z., Wang M. Temperature, relative humidity and sunshine may be the effective predictors for occurrence of malaria in Guangzhou, Southern China, 2006-2012, Parasit. Vectors. 2013;6:155. doi: 10.1186/1756-3305-6-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Andreas Béguin J.R., Åström Christofer, Sauerborn Rainer, Louis Valerie, Hales Simon. World Health Organization; 2014. Malaria [in “Quantitative Risk Assessment of the Effects of Climate Change on Selected Causes of Death, 2030s and 2050s”] pp. 51–60. [Google Scholar]
- 83.Messina J.P., Brady O.J., Golding N., Kraemer M.U.G., Wint G.R.W., Ray S.E., Pigott D.M., Shearer F.M., Johnson K., Earl L., et al. The Current and future global distribution and population at risk of dengue. Nat. Microbiol. 2019;4:1508–1515. doi: 10.1038/s41564-019-0476-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Anderegg W.R.L., Abatzoglou J.T., Anderegg L.D.L., Bielory L., Kinney P.L., Ziska L. Anthropogenic climate change is worsening North American pollen seasons. Proc. Natl. Acad. Sci. U.S.A. 2021;118 doi: 10.1073/pnas.2013284118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Osborne N.J., Alcock I., Wheeler B.W., Hajat S., Sarran C., Clewlow Y., McInnes R.N., Hemming D., White M., Vardoulakis S., et al. Pollen exposure and hospitalization due to asthma exacerbations: daily time series in a European City. Int. J. Biometeorol. 2017;61:1837–1848. doi: 10.1007/s00484-017-1369-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Marselle M.R., Stadler J., Korn H., Irvine K.N., Bonn A. Springer; Cham: 2019. Biodiversity and Health in the Face of Climate Change[M] [DOI] [Google Scholar]
- 87.Kekeh M., Akpinar-Elci M., Allen M.J. Springer International Publishing; Cham: 2019. Sea Level Rise and Coastal Communities. Extreme Weather Events and Human Health; pp. 171–184. [DOI] [Google Scholar]
- 88.Caillaud D., Leynaert B., Keirsbulck M., Nadif R., Mould ANSES working group Indoor mould exposure, asthma and rhinitis: findings from systematic reviews and recent longitudinal studies. Eur. Respir. Rev. 2018;27:170137. doi: 10.1183/16000617.0137-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Yang Y., Wu L., Guo Y., Gan B., Cai W., Huang G., Li X., Geng T., Jing Z., Li S., et al. Greenhouse warming intensifies north tropical Atlantic climate variability. Sci. Adv. 2021;7 doi: 10.1126/SCIADV.ABG9690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Cai W., Wang G., Dewitte B., Wu L., Santoso A., Takahashi K., Yang Y., Carréric A., McPhaden M.J. Increased variability of eastern Pacific El Niño under greenhouse warming. Nature. 2018;564:201–206. doi: 10.1038/s41586-018-0776-9. [DOI] [PubMed] [Google Scholar]
- 91.Kim J.H., Sung J., Kwon H.J., Cheong H.K. Effects of El Nino/La Nina on the number of imported shigellosis cases in the Republic of Korea, 2004–2017. Int. J. Environ. Res. Publ. Health. 2020;18:211. doi: 10.3390/ijerph18010211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Heaney A.K., Shaman J., Alexander K.A. El niño-southern oscillation and under-5 diarrhea in Botswana. Nat. Commun. 2019;10:5798. doi: 10.1038/s41467-019-13584-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Pramanik M., Singh P., Kumar G., Ojha V.P., Dhiman R.C. El Niño Southern Oscillation as an early warning tool for dengue outbreak in India. BMC Publ. Health. 2020;20:1498. doi: 10.1186/s12889-020-09609-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Mantilla G., Oliveros H., Barnston A.G. The role of ENSO in understanding changes in Colombia's annual malaria burden by region, 1960-2006. Malar. J. 2009;8:6. doi: 10.1186/1475-2875-8-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Colston J., Paredes Olortegui M., Zaitchik B., Peñataro Yori P., Kang G., Ahmed T., Bessong P., Mduma E., Bhutta Z., Sunder Shrestha P., et al. Pathogen-specific impacts of the 2011-2012 La niña-associated floods on enteric infections in the MAL-ED Peru cohort: a comparative interrupted time series analysis. Int. J. Environ. Res. Publ. Health. 2020;17:487. doi: 10.3390/ijerph17020487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Arias-Monsalve C., Builes-Jaramillo A. Impact of El Niño-Southern oscillation on human leptospirosis in Colombia at different spatial scales. J. Infect. Dev. Ctries. 2019;13:1108–1116. doi: 10.3855/jidc.11702. [DOI] [PubMed] [Google Scholar]
- 97.Wang J., Vanga S., Saxena R., Orsat V., Raghavan V. Effect of climate change on the yield of cereal crops: a review. Climate. 2018;6:41. doi: 10.3390/cli6020041. [DOI] [Google Scholar]
- 98.Obi C.M., Enweani-Nwokelo I.B., Oshim I.O., Okeke M.U. 2021. Assessment of Fungal Concentrations Associated with Relative Humidity and Temperature Variations in the Indoor Environment. [DOI] [Google Scholar]
- 99.UNICEF . Rome, FAO: FAO, IFAD, UNICEF, WFP and WHO; 2021. The State of Food Security and Nutrition in the World 2021. Transforming Food Systems for Food Security, Improved Nutrition and Affordable Healthy Diets for All. https://doi.org/104060/cb4474en. [Google Scholar]
- 100.Springmann M., Mason-D'croz D., Robinson S., Garnett T., Godfray H.C.J., Gollin D., Rayner M., Ballon P., Scarborough P. Global and regional health effects of future food production under climate change: a modelling study. Lancet. 2016;387:1937–1946. doi: 10.1016/S0140-6736(15)01156-3. [DOI] [PubMed] [Google Scholar]
- 101.Kuriachen P., Aiswarya S., Aditya K.S. Springer Singapore; Singapore: 2021. Climate Change and Food Security: Two Parallel Concerns. Climate Change and Resilient Food Systems; pp. 399–414. [DOI] [Google Scholar]
- 102.Clark M.A., Domingo N.G.G., Colgan K., Thakrar S.K., Tilman D., Lynch J., Azevedo I.L., Hill J.D. Global food system emissions could preclude achieving the 1.5° and 2°C climate change targets. Science. 2020;370:705–708. doi: 10.1126/science.aba7357. [DOI] [PubMed] [Google Scholar]
- 103.Nations FaAOotU . 2020. The State of World Fisheries and Aquaculture 2020 - Sustainability in Action. Rome. [Google Scholar]
- 104.Nations FaAOotU . 2020. FAO's Work on Climate Change: Fisheries and Aquaculture 2020. [Google Scholar]
- 105.Muringai R.T., Mafongoya P.L., Lottering R. Climate change and variability impacts on sub-Saharan African fisheries: a review. Rev. Fish. Sci. Aquac. 2021;29:706–720. doi: 10.1080/23308249.2020.1867057. [DOI] [Google Scholar]
- 106.Franco B.C., Defeo O., Piola A.R., Barreiro M., Yang H., Ortega L., Gianelli I., Castello J.P., Vera C., Buratti C., et al. Climate change impacts on the atmospheric circulation, ocean, and fisheries in the southwest South Atlantic Ocean: a review. Clim. Change. 2020;162:2359–2377. doi: 10.1007/s10584-020-02783-6. [DOI] [Google Scholar]
- 107.Xiao X., Agustí S., Pan Y., Yu Y., Li K., Wu J., Duarte C.M. Warming amplifies the frequency of harmful algal blooms with eutrophication in Chinese coastal waters. Environ. Sci. Technol. 2019;53:13031–13041. doi: 10.1021/acs.est.9b03726. [DOI] [PubMed] [Google Scholar]
- 108.Quayle D.B. Fisheries Research Board of Canada; 1969. Paralytic Shellfish Poisoning in British Columbia. [Google Scholar]
- 109.Kao C. 1993. Paralytic Shellfish Poisoning. [Google Scholar]
- 110.Kraemer B.M., Pilla R.M., Woolway R.I., Anneville O., Ban S., Colom-Montero W., Devlin S.P., Dokulil M.T., Gaiser E.E., Hambright K.D., et al. Climate change drives widespread shifts in lake thermal habitat. Nat. Clim. Change. 2021;11(6):522–541. [Google Scholar]
- 111.Kraemer B.M., Pilla R.M., Woolway R.I., Anneville O., Ban S., Colom-Montero W., Devlin S.P., Dokulil M.T., Gaiser E.E., Hambright K.D., et al. Climate change drives widespread shifts in lake thermal habitat. Nat. Clim. Change. 2021;11:521–529. doi: 10.1038/s41558-021-01060-3. [DOI] [Google Scholar]
- 112.Barbarossa V., Bosmans J., Wanders N., King H., Bierkens M.F.P., Huijbregts M.A.J., Schipper A.M. Threats of global warming to the world's freshwater fishes. Nat. Commun. 2021;12:1701. doi: 10.1038/s41467-021-21655-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Gasparrini A., Guo Y., Sera F., Vicedo-Cabrera A.M., Huber V., Tong S., de Sousa Zanotti Stagliorio Coelho M., Saldiva P.H.N., Lavigne E., Correa P.M., et al. Projections of temperature-related excess mortality under climate change scenarios. Lancet Planet. Health. 2017;1:e360–e367. doi: 10.1016/S2542-5196(17)30156-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Day E., Fankhauser S., Kingsmill N., Costa H., Mavrogianni A. Upholding labour productivity under climate change: an assessment of adaptation options. Clim. Pol. 2019;19:367–385. doi: 10.1080/14693062.2018.1517640. [DOI] [Google Scholar]
- 115.Watts N., Amann M., Arnell N., Ayeb-Karlsson S., Belesova K., Boykoff M., Byass P., Cai W., Campbell-Lendrum D., Capstick S., et al. The 2019 report of the Lancet Countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate. Lancet. 2019;394:1836–1878. doi: 10.1016/S0140-6736(19)32596-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Zhu Z., Piao S., Myneni R.B., Huang M., Zeng Z., Canadell J.G., Ciais P., Sitch S., Friedlingstein P., Arneth A., et al. Greening of the earth and its drivers. Nat. Clim. Change. 2016;6:791–795. doi: 10.1038/nclimate3004. [DOI] [Google Scholar]
- 117.Piao S., Wang X., Park T., Chen C., Lian X., He Y., Bjerke J.W., Chen A., Ciais P., Tømmervik H., et al. Characteristics, drivers and feedbacks of global greening. Nat. Rev. Earth Environ. 2020;1:14–27. doi: 10.1038/s43017-019-0001-x. [DOI] [Google Scholar]
- 118.Xu R., Li S., Li S., Wong E.M., Southey M.C., Hopper J.L., Abramson M.J., Guo Y. Surrounding greenness and biological aging based on DNA methylation: a twin and family study in Australia. Environ. Health Perspect. 2021;129:87007. doi: 10.1289/EHP8793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Leisner C.P. Review: climate change impacts on food security- focus on perennial cropping systems and nutritional value. Plant Sci. 2020;293:110412. doi: 10.1016/j.plantsci.2020.110412. [DOI] [PubMed] [Google Scholar]
- 120.Cheung W.W.L., Lam V.W.Y., Sarmiento J.L., Kearney K., Watson R., Pauly D. Projecting global marine biodiversity impacts under climate change scenarios. Fish Fish. 2009;10:235–251. doi: 10.1111/j.1467-2979.2008.00315.x. [DOI] [Google Scholar]
- 121.Son J.Y., Liu J.C., Bell M.L. Temperature-related mortality: a systematic review and investigation of effect modifiers. Environ. Res. Lett. 2019;14:073004. doi: 10.1088/1748-9326/ab1cdb. [DOI] [Google Scholar]
- 122.Xu R., Zhao Q., Coelho M.S.Z.S., Saldiva P.H.N., Abramson M.J., Li S., Guo Y. Socioeconomic level and associations between heat exposure and all-cause and cause-specific hospitalization in 1, 814 Brazilian Cities: a nationwide case-crossover study. PLoS Med. 2020;17 doi: 10.1371/journal.pmed.1003369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Han C., Xu R., Gao C.X., Yu W., Zhang Y., Han K., Yu P., Guo Y., Li S. Socioeconomic disparity in the association between long-term exposure to PM2.5 and mortality in 2640 Chinese Counties. Environ. Int. 2021;146:106241. doi: 10.1016/j.envint.2020.106241. [DOI] [PubMed] [Google Scholar]
- 124.Xia T., Fang F., Montgomery S., Fang B., Wang C., Cao Y. Sex differences in associations of fine particulate matter with non-accidental deaths: an ecological time-series study. Air Qual. Atmos. Health. 2021;14:863–872. doi: 10.1007/s11869-021-00985-0. [DOI] [Google Scholar]
- 125.Varghese B.M., Barnett A.G., Hansen A.L., Bi P., Hanson-Easey S., Heyworth J.S., Sim M.R., Pisaniello D.L. The effects of ambient temperatures on the risk of work-related injuries and illnesses: evidence from Adelaide, Australia 2003-2013. Environ. Res. 2019;170:101–109. doi: 10.1016/j.envres.2018.12.024. [DOI] [PubMed] [Google Scholar]
- 126.Martínez-Solanas È., López-Ruiz M., Wellenius G.A., Gasparrini A., Sunyer J., Benavides F.G., Basagaña X. Evaluation of the impact of ambient temperatures on occupational injuries in Spain. Environ. Health Perspect. 2018;126:067002. doi: 10.1289/EHP2590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Hieronymus M., Kalén O. Sea-level rise projections for Sweden based on the new IPCC special report: the ocean and cryosphere in a changing climate. Ambio. 2020;49:1587–1600. doi: 10.1007/s13280-019-01313-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Mintenbeck K. Key findings of the IPCC special report on ocean and cryosphere in a changing climate–challenges, opportunities and future scenarios. Ocean Sci. Meet. 2020;2020 Agu; 2020. [Google Scholar]
- 129.Georgescu M. Challenges associated with adaptation to future urban expansion. J. Clim. 2015;28:2544–2563. doi: 10.1175/jcli-d-14-00290.1. [DOI] [Google Scholar]
- 130.Sander M., Oxlund B., Jespersen A., Krasnik A., Mortensen E.L., Westendorp R.G., Rasmussen L.J. The challenges of human population ageing. Age Ageing. 2015;44:185–187. doi: 10.1093/ageing/afu189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Pryce J., Richardson M., Lengeler C. Insecticide-treated nets for preventing malaria. Cochrane Database Syst. Rev. 2018;11:CD000363. doi: 10.1002/14651858.CD000363.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Cicerone R.J., Oremland R.S. Biogeochemical aspects of atmospheric methane. Glob. Biogeochem. Cycles. 1988;2:299–327. doi: 10.1029/GB002i004p00299. [DOI] [Google Scholar]
- 133.United States Environmental Protection Agency Climate change indicators: Atmospheric concentrations of greenhouse gases. https://www.epa.gov/climate-indicators/climate-change-indicators-atmospheric-concentrations-greenhouse-gases
- 134.United States Environmental Protection Agency Climate change indicators: Climate forcing. https://www.epa.gov/climate-indicators/climate-change-indicators-climate-forcing
- 135.Xie Y., Dai H., Xu X., Fujimori S., Hasegawa T., Yi K., Masui T., Kurata G. Co-benefits of climate mitigation on air quality and human health in Asian countries. Environ. Int. 2018;119:309–318. doi: 10.1016/j.envint.2018.07.008. [DOI] [PubMed] [Google Scholar]
- 136.Le Quéré C., Jackson R.B., Jones M.W., Smith A.J.P., Abernethy S., Andrew R.M., De-Gol A.J., Willis D.R., Shan Y., Canadell J.G., et al. Temporary reduction in daily global CO2 emissions during the COVID-19 forced confinement. Nat. Clim. Change. 2020;10:647–653. doi: 10.1038/s41558-020-0797-x. [DOI] [Google Scholar]
- 137.Bhatia K.T., Vecchi G.A., Knutson T.R., Murakami H., Kossin J., Dixon K.W., Whitlock C.E. Recent increases in tropical cyclone intensification rates. Nat. Commun. 2019;10:635. doi: 10.1038/s41467-019-08471-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Lelieveld J., Klingmüller K., Pozzer A., Burnett R.T., Haines A., Ramanathan V. Effects of fossil fuel and total anthropogenic emission removal on public health and climate. Proc. Natl. Acad. Sci. U.S.A. 2019;116:7192–7197. doi: 10.1073/pnas.1819989116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.IBGE (Brazilian Institute of Geography and Statistics) 2017. National Survey of Health 2013. [Google Scholar]
- 140.Schraufnagel D.E., Balmes J.R., De Matteis S., Hoffman B., Kim W.J., Perez-Padilla R., Rice M., Sood A., Vanker A., Wuebbles D.J. Health benefits of air pollution reduction. Ann. Am. Thorac. Soc. 2019;16:1478–1487. doi: 10.1513/AnnalsATS.201907-538CME. [DOI] [PubMed] [Google Scholar]
- 141.Dedoussi I.C., Eastham S.D., Monier E., Barrett S.R.H. Premature mortality related to United States cross-state air pollution. Nature. 2020;578:261–265. doi: 10.1038/s41586-020-1983-8. [DOI] [PubMed] [Google Scholar]
- 142.Kua K.P., Lee S. The influence of residential greenness on mortality in the Asia-Pacific region: a systematic review and meta-analysis. Perspect. Publ. Health. 2021;141:342–353. doi: 10.1177/17579139211011496. [DOI] [PubMed] [Google Scholar]
- 143.Coady D., Parry I., Sears L., Shang B.P. How large are global energy subsidies? Int. Monetar. Fund. 2015 doi: 10.5089/9781513532196.001. [DOI] [Google Scholar]
- 144.Lowe R., Coelho C.A., Barcellos C., Carvalho M.S., Catão R., Coelho G.E., Ramalho W.M., Bailey T.C., Stephenson D.B., Rodó X. Evaluating probabilistic dengue risk forecasts from a prototype early warning system for Brazil. Elife. 2016;5 doi: 10.7554/eLife.11285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Clar C., Steurer R. Climate change adaptation at different levels of government: characteristics and conditions of policy change. Nat. Resour. Forum. 2019;43:121–131. doi: 10.1111/1477-8947.12168. [DOI] [Google Scholar]
- 146.Phuong L.T.H., Biesbroek G.R., Wals A.E.J. Barriers and enablers to climate change adaptation in hierarchical governance systems: the case of Vietnam. J. Environ. Pol. Plann. 2018;20:518–532. doi: 10.1080/1523908X.2018.1447366. [DOI] [Google Scholar]
- 147.Kovats R.S., Hajat S. Heat stress and public health: a critical review. Annu. Rev. Publ. Health. 2008;29:41–55. doi: 10.1146/annurev.publhealth.29.020907.090843. [DOI] [PubMed] [Google Scholar]
- 148.Dzhambov A.M., Browning M.H.E.M., Markevych I., Hartig T., Lercher P. Analytical approaches to testing pathways linking greenspace to health: a scoping review of the empirical literature. Environ. Res. 2020;186:109613. doi: 10.1016/j.envres.2020.109613. [DOI] [PubMed] [Google Scholar]
- 149.Krayenhoff E.S., Moustaoui M., Broadbent A.M., Gupta V., Georgescu M. Diurnal interaction between urban expansion, climate change and adaptation in US cities. Nat. Clim. Change. 2018;8:1097–1103. doi: 10.1038/s41558-018-0320-9. [DOI] [Google Scholar]
- 150.Georgescu M., Morefield P.E., Bierwagen B.G., Weaver C.P. Urban adaptation can roll back warming of emerging megapolitan regions. Proc. Natl. Acad. Sci. U.S.A. 2014;111:2909–2914. doi: 10.1073/pnas.1322280111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Castiglia Feitosa R., Wilkinson S.J. Small-scale experiments of seasonal heat stress attenuation through a combination of green roof and green walls. J. Clean. Prod. 2020;250:119443. doi: 10.1016/j.jclepro.2019.119443. [DOI] [Google Scholar]
- 152.He C., Zhao J., Zhang Y., He L., Yao Y., Ma W., Kinney P.L. Cool roof and green roof adoption in a metropolitan area: climate impacts during summer and winter. Environ. Sci. Technol. 2020;54:10831–10839. doi: 10.1021/acs.est.0c03536. [DOI] [PubMed] [Google Scholar]