Abstract
Objective:
Both cognitive behavioral therapy for depression (CBT-D) combined with brief motivational interviewing (CBT-D + BMI) and alone are associated with symptom improvement among college students with co-occurring depression and heavy episodic drinking (HED). However, little is known about change processes underlying these different treatments.The current study uses a network approach to examine change process that may differentially underlie CBT-D + BMI relative to CBT alone.
Methods:
Participants included 94 college students with depression and HED who were randomized to either eight weeks of CBT-D + BMI or CBT alone. A network approach was adopted to examine how treatment condition influenced changes in the network structure of depression symptoms, heavy drinking, drinking motives, and consequences of alcohol. Network analyses were conducted using change scores representing the eight-week difference from pre-treatment to post-treatment assessments.
Results:
Relative to CBT-D alone, the combined CBT-D + BMI treatment influenced the symptom network structure by preferentially targeting reductions in drinking to cope motives and in the depression symptom ‘loss of interest’
Conclusion:
The current study revealed that combined CBT-D + BMI may confer therapeutic benefit through different network structure pathways than CBT-D alone. Specifically, augmenting CBT-D with BMI may influence change processes related to drinking motives, such as drinking to cope.
Keywords: Depression, Heavy episodic drinking, Network analyses, Alcohol, CBT, Motivational interviewing
1. Introduction
Major depressive disorder (MDD) exhibits high levels of comorbidity with heavy episodic drinking (HED, defined as 4 + /5 + drinks in a single sitting for women/men; Wechsler et al., 2001), especially among young adults and college student populations. Prior research has estimated that 81.7% of college students with depressive symptoms engage in alcohol consumption and approximately half of them partake in episodes of HED (Dawson et al., 2005). Moreover, the co-occurrence of depressive symptoms and heavy episodic drinking (HED) predisposes college students to have a higher risk for negative drinking consequences (Pedrelli et al., 2016), as they report a higher number of alcohol-related problems than students who do not endorse depressive symptoms but do drink heavily (Geisner et al., 2004 ; Geisner et al., 2018).
Because of the significant problems associated with co-occurring depression and alcohol misuse, significant efforts have been devoted to identifying effective interventions for these problems when they co-occur. Given the large body of evidence substantiating the efficacy of cognitive behavioral therapy for depression (CBT-D, Hofmann, Curtiss, Carpenter, and Kind, 2017) and motivational interviewing (MI) for alcohol use (Lundahl et al. 2010), interventions combining these two evidence-based treatments have been developed, and an earlier meta-analysis supported CBT augmented with MI relative to treatment as usual for individuals with comorbid MDD and alcohol use disorder (Riper et al., 2014). However, a recent randomized clinical trial examined the efficacy of combined CBT-D and brief motivational interviewing (BMI) relative to CBT-D alone for reducing depressive symptoms and HED in college students (Pedrelli et al, 2020), and results showed reduction of severity of HED and depression symptoms following both interventions but did not support an additive role of BMI (Pedrelli et al., 2020). Other studies have identified therapeutic benefit of MI as a supplement to usual outpatient care for the treatment of co-occurring depression and hazardous drinking (i.e., three or more drinks per occasion) (Satre et al., 2013). Notwithstanding the mixed evidence for the additive role of MI, combined treatment of MI and CBT may be associated with symptom improvement through different mechanisms than CBT-D alone.
Recent initiatives in mental health research have encouraged researchers to re-conceptualize mental disorders as complex systems, in which symptoms causally interact in such a manner that states of pathology emerge, rather than latent disease entities, which would require symptoms of a disorder to be fully explained by an unobservable disease mechanism (Hofmann, Curtiss, and McNally, 2016 ; Hofmann and Curtiss; 2018). By construing mental disorders in this complex systems framework, clinical trial research could reprioritize its focus on examining treatment processes underlying an intervention rather than determining whether or not an intervention is effective (Hayes et al., 2019 ; Hofmann, Curtiss, & Hayes, in press). In current clinical trial research, it is commonplace to examine the efficacy of an intervention by examining reductions in composite scores of symptoms (e.g., a global depression symptom index, etc.). Moreover, in clinical trials on co-occurring disorders, the effectiveness of treatment on different disorders (e.g. depression and HED) are examined separately without accounting for their underlying associations and for the fact that symptoms interact in a dynamic fashion. For example, reduction of depression may affect alcohol reduction and vice-versa (Bahorik et al., 2016). In accordance with attempts to better model the complexity of mental disorders, in particular co-occurring disorders, novel methodologies make it possible to examine how a treatment influences the relationships between the individual symptoms and features of a disorder over time rather than a composite score of disorder severity.
One such methodological approach uses network science to model mental disorders Borsboom and Cramer (2013). In brief, a network approach to mental disorders represents features or symptoms of a disorder as a node and associations between symptoms as edges. Within a network science framework, a mental disorder such as MDD would emerge as a result of mutually reinforcing connections between symptom nodes rather than as a result of an underlying latent disease mechanism that causes symptoms to covary. Several studies have embraced network science to examine the structural composition of disorders such as depression (Fried et al., 2016), anxiety (Heeren, Bernstein, and McNally, 2018), and comorbid presentations (Curtiss and Klemanski, 2016 ; Curtiss et al., 2018). Network science permits investigations into node centrality, which corresponds to how connected a node is to other nodes in the network. Node centrality may provide insight into how influential any given node is in the network. This information can be particularly critical when studying co-occurring disorders as it may reveal important connections among features of psychopathology.
Network approaches to mental disorders can be leveraged to identify change processes underlying treatments. Recent conceptualizations of mediation and mechanism research has underscored that change processes in psychotherapeutic interventions are not best represented by the simple linear mediation models commonly adopted in the field Hofmann, Hayes, and Curtiss (2020). Rather, methodology developed by network science and dynamical systems may be able to better capture the complex and mutually interacting processes that underlie effective treatments. Borsboom (2017) postulated that network science can be used to model not only symptoms, but also psychological processes and external features that may influence symptom behavior. By examining the influence that treatments exert on networks of psychopathology features and related constructs measuring potential mechanisms, greater insight may be provided on how treatments influence interactions between symptoms and mechanisms. Such approaches may afford more rigorous methodologies to study change processes in psychological interventions (Hofmann, Hayes, and Curtiss, 2020), and they have been adopted in prior studies. For instance, Kraft and colleagues (2019) examined the processes by which attention bias modification (ABM) ameliorates depression from a network science approach.
Given the high levels of co-occurrence between depression and HED among college students (Pedrelli et al., 2016), there has been longstanding interest in understanding potential mechanisms that explain this association. One prominent model of depression and HED has underscored the role of drinking as a maladaptive emotion regulation strategy to avoid distress associated with depression (Holahan et al., 2003). This ‘drinking to cope’ model of depression and HED posits that use of alcohol to escape unpleasant emotions predicts future increases in alcohol consumption and depression symptoms (Holahan et al., 2003). From a motivational perspective, reduction in negative affect as a result of alcohol consumption functions as a negative reinforcement motivation that prompts future episodes of HED Cooper (1994). Prior research has examined how drinking to cope predicts alcohol usage (Cooper et al., 2016); however, it has yet to be examined as a possible change process in treatment for depression and HED.
In the current study, a network approach is adopted to compare combined CBT-D and BMI (CBT-D + BMI) and CBT-D alone with respect to how they differentially influence the network structure of co-occurring depressive symptoms, HED severity, problematic consequences of drinking, and coping motives for drinking among college students. In both interventions, individuals received eight weeks of therapy. Each treatment might confer therapeutic benefit through different pathways and processes of change. The network approach embraced in the current study is better suited to identify how these interventions influence the relationships between individual features of pathology rather than changes in composite symptom severity. Specifically, nodes of the network analysis will comprise symptoms of depression and domains related to heavy alcohol use (i.e., coping motives for drinking, consequences of heavy drinking, and daily alcohol intake). A network approach permits a more rigorous examination of whether this treatment influences the role of motives for drinking in the network of co-occurring HED and depression, providing insight into theory-driven change processes related to the ‘drinking to cope’ model (Holahan et al., 2003). The node related to coping motives for drinking might represent a potential change process that is more uniquely associated with CBT-D + BMI, given its focus on highlighting the maladaptive role of alcohol use as a coping strategy and promoting the adoption of more adaptive emotion regulation strategies. The primary aim of the current study is to examine how CBT-D + BMI and CBT-D influence changes in network structure of co-occurring depression symptoms and HED among college students, as well as potential change processes related to drinking to cope motives.
2. Methods
2.1. Participants
The methodology underpinning data collection for this analysis has previously been described (Pedrelli et al., 2020). Briefly, we compared the effectiveness of an 8-week treatment combining CBT-D + BMI versus 8-week CBT-D for college students with HED and depressive symptoms. In both treatments, eight sessions of therapy were provided. A full description of the study flow can be reviewed in the original study publication (Pedrelli et al., 2020). In brief, a total of 140 individuals were assessed for eligibility, and after exclusion criteria were applied and uninterested participants decided to discontinue, a total of 94 individuals were randomized to either CBT-D + BMI (n = 46) or CBT-D (n = 48). Of these, 64 (68.08%) completed post-treatment assessments (n = 32 in each condition). The study sample included undergraduate students who were recruited from 2- or 4-year colleges in the Boston area. Participants were recruited through posters, advertisements online, and on public transportation. Inclusion criteria included current enrollment as an undergraduate student, 18–24 years old, presence of at least one HED episode in the past month, and the presence of mild to moderate depressive symptoms (scores between 10 and 30 on the Beck Depressive Inventory I (BDI-I; Beck, Steer, and Garbin, 1988). Exclusion criteria included meeting diagnostic criteria for bulimia, psychosis, bipolar disorder, or illicit substance abuse in the past six months, having received any psychosocial treatment for depression or substance dependence in the past month, having received CBT-D for depression and/or alcohol use in the previous six months, having discontinued or changed dosage of an antidepressant medication less than 1 month prior screening, and/or posing a serious suicide or homicide risk. All procedures were approved by the IRB and were in compliance with APA ethical standards.
2.2. Measures and materials
2.2.1. Diagnoses
Psychiatric disorders were assessed using the Structured Clinical Interview for DSM-IV Axis I disorders (SCID-IV; First et al., 1995). The SCID-IV is a semi-structured, clinician administered interview designed to assess current and lifetime diagnoses.
2.2.2. Depressive symptoms
The Beck Depression Inventory-I (BDI-I; Beck, 1961) was administered at the beginning of each therapy visit. The measure contains 21 self-report items that range from 0 to 3, where a higher score represents greater severity of symptoms. Items 1 (i.e., sadness), 12 (i.e., loss of interest), and 15 (i.e., loss of energy) were used for the current study, because they are representative of prominent depression features and were identified as being highly central depression nodes in prior network research (Fried et al., 2016).
2.2.3. Alcohol use
Frequency of alcohol use was measured using The Alcohol Timeline Followback (TLFB; Sobell and Sobell, 1979). Participants were asked to report the number of drinks they consumed over a one month time period. The TLFB was used to compute frequency of HED (4 standard drinks for women and 5 standard drinks for men) in the previous month.
2.2.4. Alcohol-related problems
The Brief Young Adult Alcohol Consequences Questionnaire (B-YAACQ; Kahler et al., 2005) contains 24 items and was used to assess different alcohol related problems in the past month. The total score of the B-YAACQ was used in the analyses to represent total drinking problems.
2.2.5. Motives for drinking
The Drinking Motives Questionnaire-Revised (DMQ-R; Cooper, 1994) was used to assess motives for drinking. This measure contains 20 items and is rated on a 5-point likert scale. Specifically, item 17 was used in the current study as it reflects general coping motives for alcohol use (drinking to ‘forget about your problems’). Other items reflecting coping motives for alcohol use were either too symptom specific (e.g., worry, nervous, depressed) or associated with improving self-confidence. Thus, the content of item 17 appeared to best reflect coping motives for alcohol use to address more general problems and distress. Furthermore, we did not have adequate power to investigate all items in the scale.
2.3. Procedure
After providing consent, and upon completion of baseline assessments, participants were then randomized to receive eight in-person sessions of CBT-D or CBT-D + BMI. Specific treatment manuals were created for the two interventions, with adaptations for college-related pressures. Therapy sessions lasted for 50–60 min. The post-treatment assessment occurred upon completion of the eight therapy sessions, or approximately two months following the baseline visit.
With respect to intervention content, the CBT-D + BMI treatment comprised both traditional cognitive behavioral therapy strategies for the treatment of depression combined with brief motivational interviewing. Specifically, after the first session, which provided psychoeducation about depression symptoms and the CBT model, sessions two and three reviewed a Personalized Feedback Form (PFF) that included information about the participant’s alcohol use and a comparison of their use with normative consumption. The participant’s reactions to this information provided a basis for exploring their goals and motives using motivational interviewing. The following sessions (three to eight) focused on cognitive restructuring, behavior activation for low mood, relaxation strategies, and relapse prevention strategies. The CBT-D intervention consisted of the same treatment content, except review of the PFF and subsequent motivational interviewing was excluded. Alcohol use was discussed only if brought up by the participants and conversation was limited to providing education. Elicitation of change talk was not undertaken during the CBT-D sessions.
2.4. Network analysis
This study used a network structure including representative items from depression and drinking behaviors to investigate the relationship between depressive symptoms, heavy episodic drinking, and treatment outcomes. The networks were estimated using a graphical Gaussian model (GGM), and the R package qgraph (Epskamp, Cramer, Waldorp, Schmittmann, and Borsboom, 2012). The graphical LASSO, a least absolute shrinkage and selection operator, was used to mitigate the likelihood of false edges in the model (Epskamp and Fried, 2018 ; Friedman, Hastie, & Tibshirani, 2008). For these graphical regularization procedures, a model with the lowest extended Bayesian Information Criterion (EBIC) value is determined by specifying a value known as the hyperparameter gamma (γ). The value of gamma is often specified between 0 and 0.5 (Epskamp et al., 2018). Larger values of gamma yield more conservative network models with fewer edges, whereas smaller values facilitate more exploratory aims by increasing sensitivity and favoring models with more edges. Consistent with the more exploratory aims of the current study, gamma was fixed to 0 to enhance sensitivity. Within the network, nodes represent symptoms of depression, HED, and related constructs. The following nodes were chosen as they are most representative of these constructs: the TLFB indicates the past month number of HED episodes; DMQ-R item 17 (i.e., drinking to cope and forget about problems) is theoretically linked to the ‘drinking to cope’ model (Holahan et al., 2003); the B-YAACQ total score represents problematic consequences of drinking; depression features of sadness, loss of interest, and loss of energy (i.e., BDI-I item 1, BDI-I item 12, BDI-I item 15) were chosen because they are representative of depression and were found highly central in past network studies (Fried et al., 2016); and treatment condition. Edges represent the partial correlations between nodes, while controlling for the effects of other nodes.
Both pre-treatment and post-treatment cross-sectional networks were estimated. Because of sample size limitations, a permutation-based network comparison test, which requires complete cases, would not be appropriately powered to reveal treatment related differences. Instead, ‘change score’ network models were estimated such that nodes reflected changes in pre-treatment and post-treatment outcomes of depression and alcohol measures. Additionally, a treatment node was included to examine the differential effect of the two treatments (CBT-D + BMI and CBT-D) on other nodes in the network. This strategy affords greater power to detect treatment changes because treatment can be added to the network as an additional node in the change score network, which limits the number of parameters that needs to be estimated and obviates the need to conduct permutation network comparison tests across multiple networks. Positive change scores of nodes indicate improvement in symptom and pathology related constructs, and negative scores of nodes indicate worsening.
The primary centrality parameter examined in this network is strength, which is a reliable centrality metric that has been shown to have greater stability compared to other centrality parameters (Epskamp, Borsboom, and Fried, 2016). The strength parameter signifies the sum of the weights of the edges attached to each node. The strength of all nodes were analyzed.
3. Results
3.1. Descriptive characteristics
At baseline, the majority of the 94 participants were women (68.1%), identified as White (54.3%) and non-Hispanic/Latino (82.1%), and were between 18 and 23 years old (M = 19.9 ± 1.4). On average, participants reported moderate depressive symptoms (BDI = 19.5 ± 6.8) at their screen visit, and engaged in HED more than once per week (4.9 ± 3.5 past month). Across treatment conditions, there were no significant differences in mean age (CBT-D + BMI = 19.7 vs. CBT-D = 20.1), gender distribution (CBT-D + BMI = 28.3% female vs. CBT-D = 35.4% female), ethnicity (CBT-D + BMI = 87% non-Hispanic/Latino vs. CBT-D = 81.3% non-Hispanic/Latino), and race CBT-D + BMI = 60.9% White vs. CBT-D = 47.9% White) (p ’s > 0.05). At baseline, there were no between-group treatment differences across clinical variable means, including BDI-1 (CBT-D + BMI = 2.17 ± 0.75 vs. CBT-D = 2.04 ± 0.63), BDI-12 (CBT-D + BMI = 2.19 ± 0.70 vs. CBT-D = 2.07 ± 0.77), BDI-15 (CBT-D + BMI = 2.33 ± 0.72 vs. CBT-D = 2.22 ± 0.76), B-YAACQ (CBT-D + BMI = 5.14 ± 3.81 vs. CBT-D = 6.05 ± 4.67), HED (CBT-D + BMI = 5.17 ± 3.61 vs. CBT-D = 4.70 ± 3.48), and DMQ-R-17 (CBT-D + BMI = 3.41 ± 1.39 vs. CBT-D = 3.75 ± 1.24)) (p ’s > 0.05). Full baseline demographic characteristics can be located in the original publication detailing the trial (Pedrelli et al., 2020).
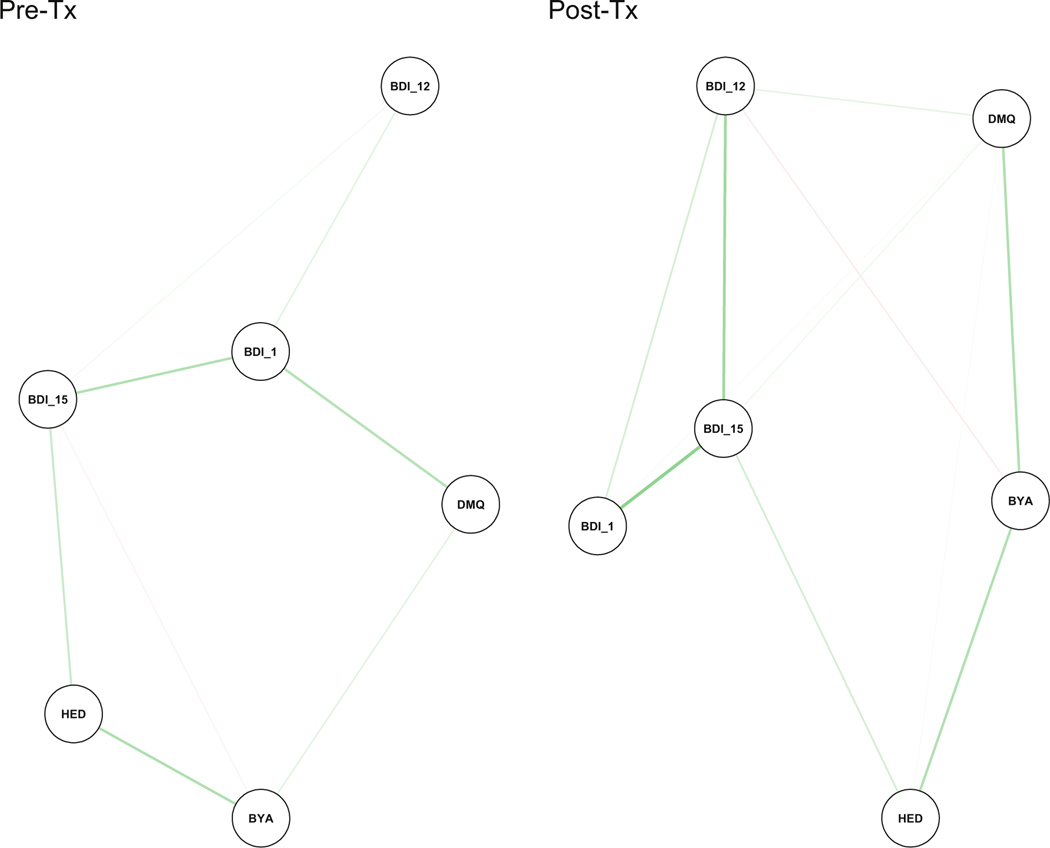
3.2. Pre-treatment and post-treatment networks
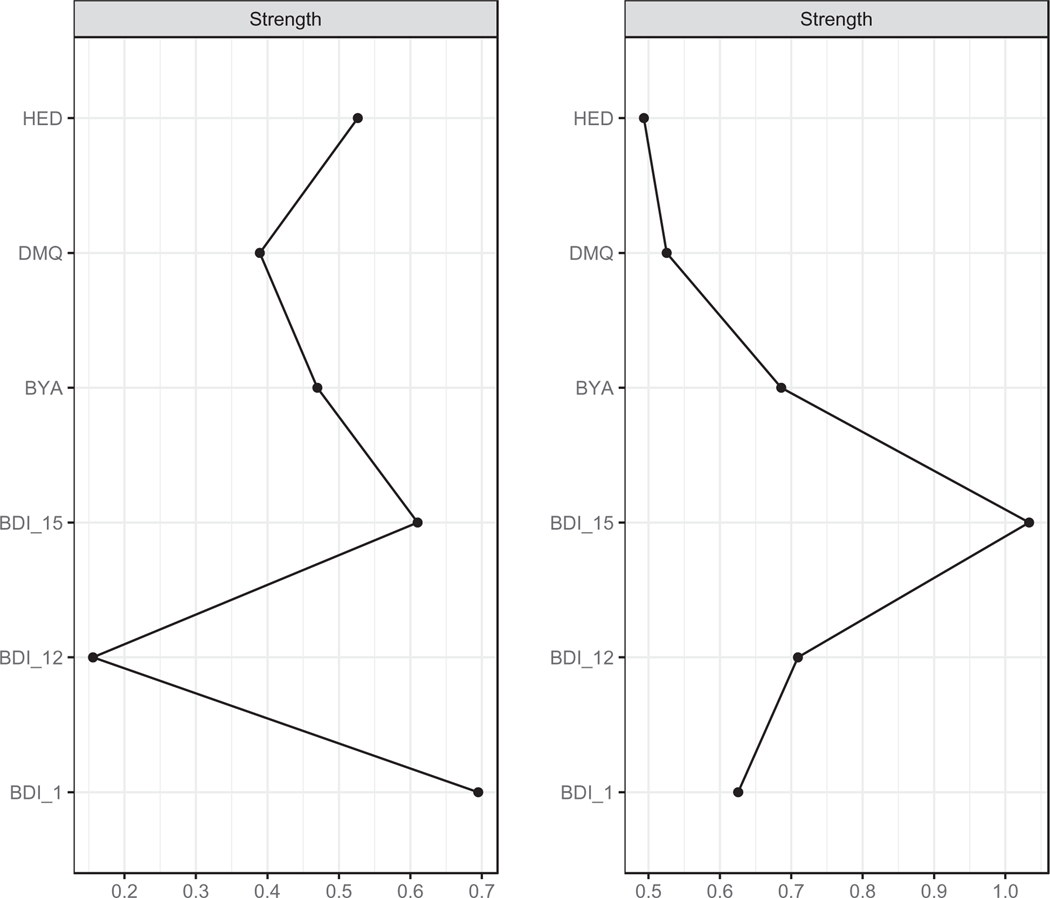
The pre-treatment and post-treatment networks are presented in Fig. 1. In the interest of statistical power, these networks were collapsed across each treatment condition. In the pre-treatment network, the nodes representing sadness, loss of energy, and frequency of HED evidenced the highest centrality with strength values of 0.69, 0.61, and 0.53, respectively (Fig. 2). As can be observed in Fig. 1, the node with the greatest level of connectivity (i.e., sadness) exhibited strong connections with loss of energy and motives for drinking and a weaker connection with loss of interest. The second most central node (i.e., loss of energy) was strongly related to sadness and frequency of HED.
Fig. 1.
Pre-Treatment and Post-Treatment Networks
Note. Network analyses for pre and post treatment. Associations between nodes are reflected by edge thickness, with thicker edges representing stronger associations. Positive associations are indicated by green edges, whereas negative associations are indicated by red edges. BDI_1 = sadness; BDI_12 = loss of interest in people; BDI_15 = loss of energy; DMQ = drink to forget about your problems; BYA = negative alcohol consequences; HED = heavy episodic drinking.
Fig. 2.
Pre-Treatment and Post-Treatment Strength Indices
Note : The plot on the left depicts strength for the pre-treatment network, whereas the one on the right depicts strength for the post-treatment network. In both cases, raw scores are presented for strength indices. BDI_1 = sadness; BDI_12 = loss of interest in people; BDI_15 = loss of energy; DMQ = drink to forget about your problems; BYA = negative alcohol consequences; HED = heavy episodic drinking.
In the post-treatment network, the node representing sadness and HED were among the least central nodes with strength values of 0.63 and 0.49, respectively. In contrast, loss of energy and loss of interest were the most central nodes with strength values of 1.03 and 0.71, respectively.
3.3. Symptom change networks
To interrogate how treatment condition influences the network structure over time, two change-score networks (i.e., ‘delta’ networks) were estimated, one of which included treatment as a node and the other did not (Fig. 3). The treatment node represents a dummy-coded variable such that the value 0 refers to CBT-D and the value 1 refers to the combined CBT-D + BMI intervention. The change score nodes reflect changes from pre-treatment scores to post-treatment nodes (i.e., positive values of symptom scores denote improvement across time).
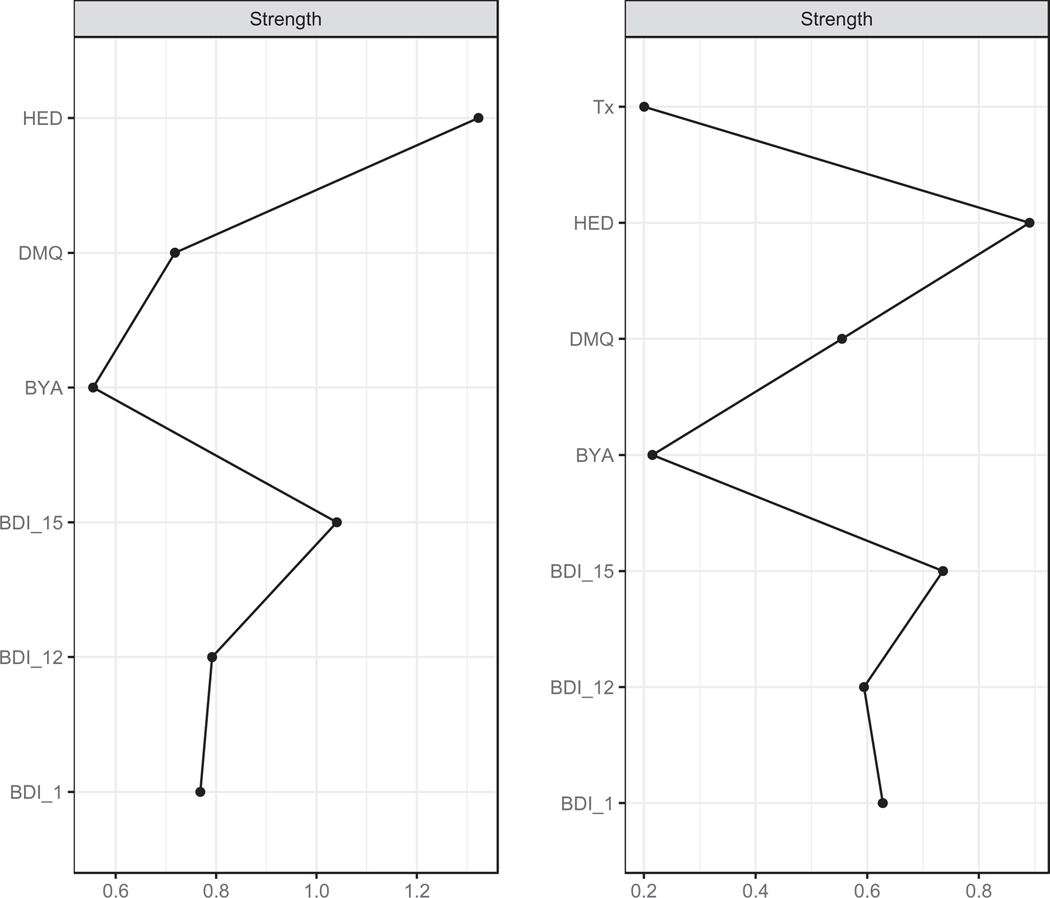
Fig. 3.
Change Score Networks
Note. With the exception of the treatment node, all other nodes represent change scores. Associations between nodes are reflected by edge thickness, with thicker edges representing stronger associations. Positive associations are indicated by green edges, whereas negative associations are indicated by red edges. BDI_1 = sadness; BDI_12 = loss of interest in people; BDI_15 = loss of energy; DMQ = drink to forget about your problems; BYA = negative alcohol consequences; HED = heavy episodic drinking.
In the change-score network without treatment as a node, frequency of HED and loss of energy exhibited the highest strength centrality measures (1.32 and 1.04, respectively) (Fig. 4). That is, across time points reductions in HED was strongly associated with changes in other domains, including improvements in loss of energy and sadness, as well as reductions in adverse consequences of alcohol (B-YAACQ). Interestingly, changes in HED were inversely associated with changes in loss of interest and coping motives for drinking (Fig. 3).
Fig. 4.
Change Score Network Strength Indices
Note : The plot on the left depicts strength for the change score network without treatment included as a node, whereas the one on the right depicts strength for the change score network including treatment as a node. In both cases, raw scores are presented for strength indices. BDI_1 = sadness; BDI_12 = loss of interest in people; BDI_15 = loss of energy; DMQ = drink to forget about your problems; BYA = negative alcohol consequences; HED = heavy episodic drinking.
In the change-score network including treatment as a node, again frequency of HED and loss of energy demonstrated the highest strength centrality measures (0.89 and 0.73, respectively). The treatment node exhibited positive associations with the drinking to cope motives node and the loss of interest node, with regularized partial correlation coefficients of 0.13 and 0.07, respectively (Fig. 3). On average, individuals in the combined intervention condition (CBT-D + MI) exhibited greater reductions in drinking to cope motives and improvement in loss of interest relative to those who received CBT-D as a stand-alone treatment. Furthermore, when the treatment node was included, adverse consequences of alcohol consumption was less densely connected to other nodes in the change network (e.g., no connection with drinking to cope motives and loss of energy).
3.4. Network stability
To appraise the stability and accuracy of the networks, case-dropping bootstrapping procedures were employed. Figures S1-S4 in the Supplementary Materials depict each of the bootstrapping analyses. Results indicate that even when dropping 50% of the cases, the correlation between the original centrality indices and those obtained from the subset is still moderate to large.
4. Discussion
Recent attention has been devoted to the treatment of co-occurring depression and HED, especially given the fact that the onset of this combined presentation often emerges among young adults (Dawson et al., 2005). Recent treatment strategies have considered integrating the most promising components of different evidence-based interventions such as CBT-D and BMI for depression and HED (Pedrelli et al., 2020). Although prior research has examined which treatments confer therapeutic benefit on levels of overall disorder severity, relatively little research has been conducted on how evidence-based practices influence networks of co-occurring depressive symptoms and HED. Adopting a network approach permits a more nuanced examination of how the relationships between co-occurring symptoms change over time in the context of treatment (Kraft et al., 2019 ; Hofmann and Curtiss, 2018). Differential change processes may underlie each treatment strategy.
In the current study, the network structure of co-occurring depressive symptoms and HED among college students exhibited differences across pre-treatment and post-treatment time points collapsed across treatment condition. The most notable difference was related to the centrality of the individual node ‘sadness’. For the pre-treatment network, this node exhibited the most connections to other symptoms of depression and drinking behaviors. This may be unsurprising, as prior research examining the comorbidity between low mood and alcohol use disorders suggest that this cardinal depression symptom may contribute to motivations for heavy alcohol use as a way to cope with distressing levels of negative affect (Anker et al., 2017). Nonetheless, it is of interest that the centrality of sadness was reduced in the overall post-treatment network collapsed across treatment conditions, exhibiting connections only with other depression symptoms (i.e., loss of interest and loss of energy) and no longer with motives for drinking.
Change-score networks were examined to ascertain the influence of CBT-D and CBT-D + BMI on the symptom networks. In the change-score network without considering treatment, improvements in frequency of HED and in reduced energy were the nodes with the greatest connectivity. Although the cross-sectional nature of the current network approach does not accommodate causal conclusions or speculations about directionality, the current results are consistent with the idea that changes in heavy alcohol consumption and energy level may influence improvements in other symptoms. This may underscore their role as transdiagnostic features connecting symptom networks from disparate disorders. Indeed, prior research examining mechanisms of comorbidity has converged on the notion that increased substance use (e.g., alcohol) exhibits temporal precedence in predicting higher levels of depressive symptomatology and further substance use (Fergusson, Boden, and Horwood, 2011) in particular in young adults.
The change-score network including treatment as a node revealed positive associations between treatment condition and nodes representing drinking to cope motives and loss of interest (i.e., anhedonia). Substantive interpretations of this result indicate that the combined CBTD + BMI was associated with greater reductions in coping motivations for drinking and improvements in anhedonia relative to CBT-D alone. These results are sensible in light of the content of each therapeutic condition. The combined intervention included a BMI component focused on raising ambivalence about heavy alcohol use by highlighting how drinking may be associated with negative consequences while offering alternative strategies to cope with aversive mood (e.g., behavioral activation and cognitive restructuring). Consistent with the ‘drinking to cope’ model of co-occuring depression and HED (Holahan et al., 2003), results suggest that drinking to cope might represent a change process more uniquely targeted by the combined CBT-D + BMI intervention. An explanation for the beneficial influence of the combined intervention on anhedonia might be revealed by considering decision-making research on anhedonia as deficit in effort-based motivational processes (Treadway, Bossaller, Shelton, and Zald, 2012). Treadway and Zald (2011) have posited that anhedonia not only corresponds to a deficit in hedonic response to rewards, but also to diminished motivation to pursue adaptive rewarding activities. Conceptualizing anhedonia as primarily a deficit in motivation, Treadway and Zald (2011) proposed that interventions targeting motivational systems and eliciting change behaviors to engage in more adaptive rewarding activities would be profitable. Given that motivational interviewing is designed to elicit motivation for behavioral change, perhaps interventions featuring BMI may accrue benefit to anhedonic symptomatology.
Although the original clinical trial did not reveal significant differences between the treatment conditions on average levels of composite symptom measures (Pedrelli et al., 2020), results of the current study underscore how considering the complexity of co-occurring disorder presentations using network analyses can reveal different pathways through which each treatment may ameliorate symptom severity. Rather than leading to different levels of improvement of overall symptom severity, these treatments may result in differences in the direct connections between individual symptom features and problematic drinking behaviors. Although composite scores comprise individual items, they can obfuscate how individual features are targeted by treatment. Thus, a substantive conclusion from the current study may be that augmenting standard CBT-D with BMI influences the extent to which nodes such as drinking to cope and loss of interest are connected to other symptom nodes in the network. Hence, augmenting CBT-D treatment with BMI might target change processes related to drinking to cope more so than CBT-D alone.
The results of the current study should be interpreted in light of certain limitations. Although networks were estimated at multiple time-points (i.e., pre-treatment and post-treatment), the networks were still cross-sectional in design, which forbids strong causal conclusions. Thus, care should be exercised for speculations about whether central nodes should be identified as treatment targets. A highly central node in a cross-sectional network may either be a proximal or terminal cause of other nodes, which may limit conclusions about what specific node an intervention should target (Fried and Cramer, 2017 ; Hofmann and Curtiss, 2018). That notwithstanding, the treatment node in the change-score network represents an experimental manipulation using randomization, which can facilitate conclusions about how treatment condition conveys its effect on individual nodes in the network. A second limitation was the sample size. Although the sample size was adequately powered for the purposes of the original randomized controlled trial, the current sample of 94 participants did not afford enough power to allow formal network comparison tests between the pre-treatment and post-treatment networks. Therefore, strong conclusions about whether certain nodes (e.g., sadness) exhibited statistically significant differences in centrality at a given time-point cannot be corroborated. Third, the current study only investigated network changes from pre-treatment to post-treatment. Thus, it would be beneficial for future research to consider more intensive long-term assessment, measuring symptomatology multiple times throughout the course of treatment and including further follow-up time points. Such a trial design would be better poised to elucidate treatment processes and mechanisms. Finally, the experimental conditions compared two treatment strategies head-to-head. The absence of a waitlist condition, in which participants do not receive treatment, makes it difficult to rule out the possibility that changes in the networks were related to the mere passage of time rather than to treatment. It could be the case that such changes as were identified in the current study are the result of other explanations, such as regression to the mean or psychotherapy common factors.
These limitations notwithstanding, this represents the first study to examine treatment of co-occurring depression and HED among college students using a network approach. By construing mental disorders, and in particular co-occurring disorders, as complex systems from a network perspective, clinical trials are better poised to examine treatment processes rather than the overall efficacy of treatment protocols (Hayes et al., 2019 ; Hofmann, Curtiss, & Hayes, in press). By examining how combined therapy versus monotherapy exerts an effect on nodes in a network of symptom changes, further insight can be derived into the treatment processes underlying combined CBT-D + BMI. The current research is in accord with the recent introduction of network intervention analysis as a procedure to identify how treatment components can sequentially influence specific symptoms over time (Blanken et al., 2019). Future research directions could include using network intervention analysis procedures in conjunction with more frequent assessment periods to identify how different treatment stages of MI contribute to changes in specific associations between symptoms over time. This could promote better identification of treatment processes, techniques, and mechanisms helpful for recovery, as they unfold over time (Blanken et al., 2019).
Although Pedrelli et al. (2020) found comparable benefits between these treatment strategies, results of the network analyses might reveal different change processes associated with each treatment. Conclusions from the current study underscore that BMI might target change processes related to drinking to cope. It would be profitable for future research to further our knowledge of how treatments target mental disorders from a complex systems perspective by emphasizing intensive time-series data to better delineate symptom dynamics and idiographic disorder processes.
Supplementary Material
Acknowledgements
There are no relevant acknowledgements for the current manuscript.
Role of Funding
The funding source was the National Institute on Alcohol Abuse and Alcoholism (# 5K23AA020064). The role of the sponsor was to provide funding for the study trial and participant collection. The funding source did not have any role in determining the data analyses, preparation of the manuscript, or decisions about journal submission.
Data transparency statement
The data reported in this manuscript have been previously published in the original clinical trial paper. The original clinical trial emphasized results regarding the differential efficacy of the two treatment options (i.e., CBT + MI vs. CBT alone). The current paper uses a vastly different methodological technique (i.e., network analyses) to examine different change processes underlying each treatment.
Footnotes
Supplementary materials
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jadr.2020.100040.
Declaration of Competing Interest
None of the authors have disclosures of interest that bear on the current manuscript or research study.
References
- Anker JJ, Forbes MK, Almquist ZW, Menk JS, Thuras P, Unruh AS, Kushner MG, 2017. A network approach to modeling comorbid internalizing and alcohol use disorders. J. Abnorm. Psychol 126, 325–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bahorik AL, Leibowitz A, Sterling SA, Travis A, Weisner C, Satre DD, 2016. The role of hazardous drinking reductions in predicting depression and anxiety symptom improvement among psychiatry patients: a longitudinal study. J. Affect. Disord 206, 169–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J, 1961. An inventory for measuring depression. Arch. Gen. Psychiatry 4, 53–61. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Garbin MG, 1988. Psychometric properties of the beck depression inventory twenty-five years of evaluation. Clin. Psych. Rev 8, 77–100. [Google Scholar]
- Blanken TF, Van Der Zweerde T, Van Straten A, Van Someren EJ, Borsboom D, Lancee J, 2019. Introducing network intervention analysis to investigate sequential, symptom-specific treatment effects: a demonstration in co-occurring insomnia and depression. Psychother. Psychosom 88, 52–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D, 2017. A network theory of mental disorders. World Psychiatry 16, 5–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D, Cramer AO, 2013. Network analysis: an integrative approach to the structure of psychopathology. Ann. Rev. Clin. Psychol 9, 91–121. [DOI] [PubMed] [Google Scholar]
- Cooper LM, 1994. Motivations for alcohol use among adolescents: development and validation of a four-factor model. Psychol. Assess 6, 117–128. [Google Scholar]
- Cooper ML, Kuntsche E, Levitt A, Barber L, Wolf S, 2016. A motivational perspective on substance use: review of theory and research. In: Sher KJ (Ed.), Oxford Handbook of Substance Use Disorders. Oxford University Press, New York, NY, pp. 375–421. [Google Scholar]
- Curtiss J, Ito M, Takebayashi Y, Hofmann SG, 2018. Longitudinal network stability of the functional impairment of anxiety and depression. Clini. Psychol. Sci 6 (3), 325–334. [Google Scholar]
- Curtiss J, Klemanski DH, 2016. Taxonicity and network structure of generalized anxiety disorder and major depressive disorder: an admixture analysis and complex network analysis. J. Affect. Disord 199, 99–105. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grat BF, Stinson FG, Chou PS, 2005. Psychopathology associated with drinking and alcohol use disorders in the college and general adult populations. Drug Alcohol Depend. 77, 139–150. [DOI] [PubMed] [Google Scholar]
- Epskamp S, Borsboom D, & Fried EI (2016). Estimating psychological networks and their stability: a tutorial paper. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S, Cramer AOJ, Waldorp LJ, Schmittmann VD, Borsboom D, 2012. qgraph: Network visualizations of relationships in psychometric data. J. Stat. Software 48, 18. [Google Scholar]
- Epskamp S, Fried EI, 2018. A tutorial on regularized partial correlation networks. Psychol. Methods 23, 617–634. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Boden JM, Horwood LJ, 2011. Structural models of the comorbidity of internalizing disorders and substance use disorders in a longitudinal birth cohort. Soc. Psychiatry Psychiatr. Epidemiol 46, 933–942. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Williams JBW, Gibbon M, 1995. Structured Clinical Interview for DSM-IV. American Psychiatric Press, Washington, DC. [Google Scholar]
- Fried EI, Cramer AOJ, 2017. Moving forward: challenges and directions for psychopathological network theory and methodology. Perspect. Psychol. Sci 12, 999–1020. [DOI] [PubMed] [Google Scholar]
- Fried EI, Epskamp S, Nesse RM, Tuerlinckx F, Borsboom D, 2016. What are’good’depression symptoms? Comparing the centrality of DSM and non-DSM symptoms of depression in a network analysis. J. Affect. Disord 189, 314–320. [DOI] [PubMed] [Google Scholar]
- Friedman J, Hastie T, Tibshirani R, 2008. Sparse inverse covariance estimation with the graphical lasso. Biostat. 9 (3), 432–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geisner IM, Larimer ME, Neighbors C, 2004. The relationship among alcohol use, related problems, and symptoms of psychological distress: Gender as a moderator in a college sample. Addict. Behav 29, 843–848. [DOI] [PubMed] [Google Scholar]
- Geisner IM, Mallett K, Varvil-Weld L, Ackerman S, Trager BM, Turrisi R, 2018. An examination of heavy drinking, depressed mood, drinking related constructs, and consequences among high-risk college students using a person-centered approach. Addict. Behav 78, 22–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes SC, Hofmann SG, Stanton CE, Carpenter JK, Sanford BT, Curtiss JE, Ciarrochi J, 2019. The role of the individual in the coming era of process-based therapy. Behav. Res. Ther 117, 40–53. [DOI] [PubMed] [Google Scholar]
- Heeren A, Bernstein EE, McNally RJ, 2018. Deconstructing trait anxiety: a network perspective. Anxiety, Stress, & Coping 31 (3), 262–276. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Curtiss J, Carpenter JK, Kind S, 2017. Effect of treatments for depression on quality of life: a meta-analysis. Cogn. Behav. Ther 46 (4), 265–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Curtiss J, 2018. A complex network approach to clinical science. Eur. J. Clin. Invest 48 (8), e12986. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Curtiss J, McNally RJ, 2016. A complex network perspective on clinical science. Perspect. Psychol. Sci 11 (5), 597–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Curtiss JE, Hayes SC, 2020. Beyond linear mediation: toward a dynamic network approach to study treatment processes. Clin. Psychol. Rev 76, 101824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holahan CJ, Moos RH, Holahan CK, Cronkite RC, Randall PK, 2003. Drinking to cope and alcohol use and abuse in unipolar depression: a 10-year model. J. Abnorm. Psychol 112, 159–165. [PubMed] [Google Scholar]
- Kahler CW, Strong DR, Read JP, 2005. Toward efficient and comprehensive measurement of the alcohol problems continuum in college students: the brief young adult alcohol consequences questionnaire. Alcohol Clin. Exp. Res 29 (7), 1180–1189. [DOI] [PubMed] [Google Scholar]
- Kraft B, Jonassen R, Heeren A, Harmer C, Stiles T, Landrø NI, 2019. Attention bias modification in remitted depression is associated with increased interest and leads to reduced adverse impact of anxiety symptoms and negative cognition. Clin. Psychol. Sci 7, 530–544. [Google Scholar]
- Lundahl BW, Kunz C, Brownell C, Tollefson D, Burke BL, 2010. A meta-analysis of motivational interviewing: twenty-five years of empirical studies. Res. Soc. Work Practice 20, 137–160. [Google Scholar]
- Pedrelli P, Borsari B, Lipson SK, Heinze JE, Eisenberg D, 2016. Gender differences in the relationships among major depressive disorder, heavy alcohol use, and mental health treatment engagement among college students. J. Stud. Alcohol and Drugs 77, 620–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedrelli P, Borsari B, Merrill JE, Fisher LB, Nyer M, Shapero BG, Farabaugh A, Hayden ER, Merrill JE, Levine MT, Fava M, Weiss RD, 2020. Evaluating the combination of a brief motivational intervention plus cognitive behavioral therapy for depression and heavy episodic drinking in college students. Psychol. Addict. Behav 34 (2), 308–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riper H, Andersson G, Hunter SB, de Wit J, Berking M, Cuijpers P, 2014. Treatment of comorbid alcohol use disorders and depression with cognitive-behavioural therapy and motivational interviewing: a meta-analysis. Addiction 109 (3), 394–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satre DD, Delucchi K, Lichtmacher J, Sterling SA, Weisner C, 2013. Motivational interviewing to reduce hazardous drinking and drug use among depression patients. J. Subst. Abuse Treat 44, 323–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Maisto SA, Sobell MB, Cooper AM, 1979. Reliability of alcohol abusers’ self reports of drinking behavior. Behav. Res. Therapy 17, 157–160. [DOI] [PubMed] [Google Scholar]
- Treadway M, Bossaller N, Shelton R, Zald D, 2012. Effort-based decision-making in major depressive disorder: a translational model of motivational anhedonia. J. Abnorm. Psychol 121, 553–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treadway MT, Zald DH, 2011. Reconsidering anhedonia in depression: lessons from translational neuroscience. Neurosci. Biobehav. Rev 35, 537–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler H, Nelson TF, 2001. Binge drinking and the american college student: what’s five drinks? Psychol. Addict. Behav 15, 287–291. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data reported in this manuscript have been previously published in the original clinical trial paper. The original clinical trial emphasized results regarding the differential efficacy of the two treatment options (i.e., CBT + MI vs. CBT alone). The current paper uses a vastly different methodological technique (i.e., network analyses) to examine different change processes underlying each treatment.