Abstract
Purpose:
To investigate the reliability of a measure of fidelity of therapist delivery, quantify fidelity of delivery, and determine factors impacting fidelity in the Rehabilitation EArly for Congenital Hemiplegia (REACH) clinical trial.
Methods:
Ninety-five infants (aged 3–9 months) with unilateral cerebral palsy participated in REACH. The Therapist Fidelity Checklist (TFC) evaluated key intervention components. Video-recorded intervention sessions were scored using the TFC.
Results:
Inter- and intra-rater reliability were percentage agreement 77–100%. Fidelity of delivery was high for 88.9% of sessions and moderate for 11.1%. Sessions with moderate scores included infants receiving infant-friendly bimanual therapy and occurred at the intervention midpoint or later. No significant relationships were found for TFC scores and infant age, manual ability, or parent engagement.
Conclusions:
Fidelity of delivery was high for the REACH trial in most intervention sessions. Standardized therapist training with intervention manuals and monthly peer-to-peer support likely contributed to these results.
Introduction and Purpose
Cerebral palsy (CP) is the most prevalent cause of childhood motor impairment.1 Multiple factors, including distribution of motor impairments and age, impact the choice of intervention for children with CP.2 An estimated 28–59% of children with CP have unilateral CP (UCP).1,3,4 Upper extremity (UE) function is more commonly impacted compared with lower extremity function among children with UCP.5,6 Interventions to improve manual skills, such as reaching, grasping, and bimanual coordination, may positively impact participation in daily activities, problem solving, and cognition.7–9
International guidelines enable diagnosis of CP in infancy, allowing early referral to rehabilitation.10 Constraint-induced movement therapy (CIMT) and bimanual therapy (BIM) have known efficacy for improving UE function in school-aged children with UCP.2,5 These interventions incorporate repeated, task-specific, and child-initiated movement.2,5 Emerging evidence indicates that infant-friendly versions (Baby-CIMT and Baby-BIM) could optimize UE function for infants with UCP.11–13 The Rehabilitation Early for Congenital Hemiplegia (REACH, ACTRN12615000180516) trial is an international, multi-site, randomized comparative efficacy trial comparing equal doses of Baby-BIM and Baby-CIMT for improving UE function for infants with UCP.14 For REACH, intervention was delivered to infants in the home by parents or caregivers with bi-monthly coaching support from a physical or occupational therapist.
The REACH interventions were complex, with multiple components for the therapists to deliver, complex behaviors for parents to receive, and allowed for tailoring to the needs of individual infants with a range of manual abilities.15,16 Delivering complex interventions consistently can be challenging, making measurement of intervention fidelity vital.17,18 Intervention fidelity is the extent that intervention components occur as intended based on the intervention design. Accurate interpretation of clinical research is only possible when fidelity is measured because outcomes can be attributed to intervention components performed by participants rather than attributed only to the intervention design.15,18,19 For example, poor outcomes following CIMT may result from poor fidelity rather than an ineffective intervention. Intervention contamination occurs when components are unintentionally added or removed.20 For example, manually restraining the unimpaired hand to encourage use of the impaired hand for play would contaminate Baby-BIM because this unintentionally introduces an element of CIMT. Measuring fidelity in efficacy trials is important to ensure that intervention groups receive the planned dose of the intended intervention components with consistent quality and without contamination. In this way, intervention outcomes can be accurately compared.19
Intervention delivery occurs when intervention is passed from the therapist to a participant. Fidelity of delivery has been inadequately studied and reported for complex interventions.18 Simple criteria (e.g., present or absent) have commonly been used for measuring fidelity of delivery.21 This basic metric does not quantify the quality or extent to which therapists deliver complex, coaching-based interventions.21 Intervention-specific tools that define key intervention components have been recommended, developed, and implemented for complex interventions for infants with motor delays and/or high risk for CP.9,20,22–24 An intervention-specific measure of fidelity of delivery was developed for the REACH trial. The purposes of this study were to investigate the reliability of this intervention-specific measure, to determine fidelity of delivery for both intervention groups in the REACH trial, and to determine factors impacting fidelity of delivery. Factors hypothesized to have an impact on fidelity of delivery include intervention group allocation, infant age, baseline manual abilities, therapists’ prior experience, and parent engagement as an indicator of the therapist-parent partnering.
Methods
Study Design
The present sub-study was an analysis of the REACH randomized comparison trial (RCT).14 The study was approved by Children’s Health Queensland Hospital and Health Service (HREC/14/QRCH/375), The University of Queensland (2015000013), The Ohio State University (2018N0042), and Nationwide Children’s Hospital (MOD00005934) Institutional Review Boards. Eligibility criteria for the primary RCT were infants aged 3–9 months corrected age (CA) at study entry; asymmetric brain lesions identified by neuroimaging prior to 24 weeks post-term age; absent fidgety General Movements25 and/or low scores on the Hammersmith Infant Neurological Examination26,27 prior to 9 months CA; asymmetrical UE motor skills based on the Hand Assessment for Infants (HAI);28 and adequate visual skills to participate in intervention and evaluations.14 English was required to be spoken or translation for English available for home visitation. Infants were excluded if they had epilepsy uncontrolled by medication, visual impairment preventing participation in clinical assessments, or a ventriculo-peritoneal shunt.14 The study protocol has been published.14
Participants
Ninety-five (N=95) infants were enrolled in the primary RCT. Written informed consent was obtained from parents or legal caregivers for each enrolled infant. Infants were randomized using concealed random allocation to the Baby-BIM (49, 51.6%) or Baby-CIMT (46, 48.4%) group. Infants were enrolled across 5 intervention sites, including 4 Australian states: New South Wales (n=12, 12.6%), Queensland (n=34, 35.6%), Victoria (n=16, 16.8%), and Western Australia (n=20, 21.1%); and 1 site in the United States: Ohio (n=13, 13.7%).
Study therapist training
All study therapists (n=12) participated in standardized training for delivering both Baby-CIMT and Baby-BIM. Training included a 2-day certification course in the HAI, which was used to determine infants’ manual abilities and for incrementation of intervention activities.28 Two additional days of instruction were devoted to intervention rationale, intervention content according to group and level of manual ability, and family-centered care principles for delivering Baby-CIMT and Baby-BIM.14 Training included didactic and interactive components, and therapists were provided with standardized materials, including intervention group manuals and checklists for intervention delivery. Therapists participated in mandatory monthly meetings lasting 1 hour for peer-to-peer problem solving using case studies to avoid drift in delivery away from the interventions as designed.
Measures
Therapist Fidelity Checklist (TFC):
This intervention-specific checklist was developed for the REACH trial. The purpose of the TFC was to measure key components of intervention delivered by therapists to parents, differentiation of the Baby-CIMT and Baby-BIM interventions, and therapist competence in delivering the interventions. Steps for checklist development followed recommendations for developing quality fidelity measures.29 Chief investigators and content experts for the REACH trial defined key intervention components based on theoretical underpinnings for Baby-CIMT and Baby-BIM. Intervention components were then defined as observable behaviors for coding. An initial version of the checklist included 21 items. A coding manual described behaviors for each item indicating full adherence to the intervention design (scored as 2), partial adherence (scored as 1), absent adherence (scored as 0), or proscribed behaviors (unintended behaviors added to when intervention was delivered, scored as P). A TFC total score was derived as the sum of all item scores.
Therapist survey:
A self-report survey was completed by all study therapists during the standardized training. Demographic items included years of pediatric practice and experience treating children with UCP.
Pediatric Rehabilitation Intervention Measure of Engagement – General (PRIME-G)30:
This 12-item parent-report questionnaire measures parent engagement with an intervention. The PRIME-G takes about 5 minutes to complete. Each item has a positive pole and a negative pole. A 7-point Likert-type scale has a range of 1 (strongly agree with the negative pole) to 7 (strongly agree with the positive pole). The total score is derived from the sum of item scores and ranges from 12 to 84. Parents completed the PRIME-G at the commencement, the midpoint, and completion of the intervention period when the infant was 12–15 months CA. The PRIME-G Total Score for the corresponding time of the recorded home intervention session was used in the present study.
Hand Assessment for Infants (HAI)28:
The HAI is a criterion- and norm-referenced assessment with strong validity and reliability.31,32 The purpose of the HAI is to evaluate the quality and frequency of spontaneous use of the more impaired UE for children with asymmetrical UE motor skills. The HAI takes about 10–15 minutes to administer and is a video-recorded observation-based play session using a standard set of toys. There are 17 items on the HAI, including 12 unimanual items and 5 items assessing bimanual skills. Scores for each item range from 0 to 2. For unimanual items, each hand is scored individually, with a raw score ranging from 0 to 24. For this study, the total raw score of the for impaired hand from the pre-intervention (‘baseline’) HAI assessment was used.
Procedures
Monthly home-based intervention sessions with the study therapist, parent(s), and infant were video-recorded and used for scoring the TFC. Two trained raters scored a sample of 30 randomly selected home intervention sessions to test inter-rater reliability. For intra-rater reliability, a single rater scored the 30 selected home visits twice. For fidelity of delivery, a total of 72 home visit session recordings were selected for scoring. The first delivery of Baby-BIM and Baby-CIMT was scored for each therapist (n=22 sessions). Additionally, approximately 10% of home visits for each therapist (n=50 sessions) were randomly selected for scoring.14 Scoring was completed by raters with established inter-rater reliability (JZ, LS, KS, JH). Raters did not score sessions in which they were the therapist providing intervention to avoid bias. The a-priori TFC cutoff score for high fidelity of delivery was established as >80% (score ≥13 out of 16), moderate was ≥50%–80% (8–12 out of 16), and low was <50 (<8 out of 16).33,34 To monitor fidelity for the REACH trial, in cases when fidelity was scored low, supplemental training and additional supervision from local site coordinators were provided to therapists.
Statistical Analysis
Demographic characteristics of infants in scored sessions were compared to all REACH trial participants using Chi-squared tests for categorical variables and t tests for continuous variables. A Chi-squared test was used to determine differences in proportions of infants treated by study therapists in scored sessions compared with the REACH trial overall. Percentage agreement was calculated between raters (inter-rater) and for sessions scored twice by the same rater (intra-rater) for reliability testing. Descriptive statistics were calculated for TFC scores. Scores were non-normally distributed (Figure 1), so medians and interquartile ranges (IQRs) versus unadjusted means were calculated for total scores. Given the small number of sessions (n=8, 11.1%) that scored <80% cutoff for high fidelity on the TFC, regression analysis was not conducted to explore factors impacting scores. Spearman’s rho was used to determine the correlation between TFC total scores and infant age, baseline HAI Impaired Hand Raw Score, and parent-reported PRIME-G scores. Categorical variables violated assumption of independence of observations for Mann-Whitney U and Kruskal Wallis tests. Graphical representations and descriptions of TFC scores across categorical variables were used to explore potential patterns. All analyses were performed using IBM SPSS Statistics for Windows, Version 27.0 (IBM Corp., Armonk).
Figure 1.
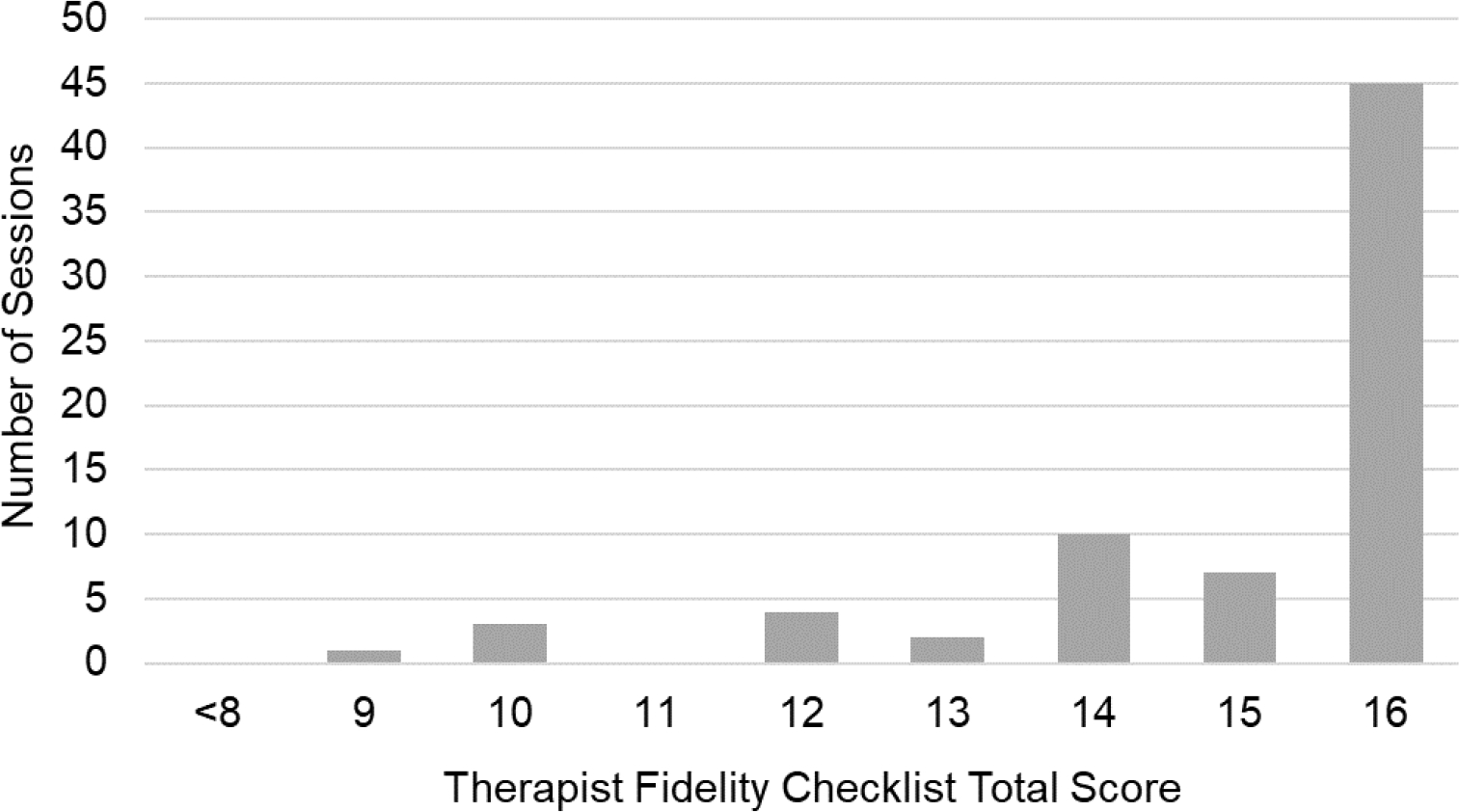
Frequency of Therapist Fidelity Checklist Total Scores for all scored sessions.
Results
Infant characteristics
Characteristics of infants in scored sessions and all infants in the REACH trial are in Table 1. There were no significant differences in characteristics for infants in the present fidelity sub-study compared with all infants in the REACH trial.
Table 1.
Infant Characteristics from Sessions Scored for Fidelity of Delivery versus All Participants in the REACH Trial
| Scored Sessions (n=53) | REACH Trial (n=95) | P Value | |
|---|---|---|---|
|
| |||
| Sexa | |||
| Male | 26 (49.1%) | 50 (52.6%) | .605 |
| Female | 27 (50.9%) | 45 (47.4%) | |
|
| |||
| GA at Birth (w) | |||
| Mean (SD) | 35.58 (5.26) | 35.27 (5.27) | .608 |
|
| |||
| Age at Baseline (m) | |||
| Mean (SD) | 6.47 (1.63) | 6.51 (1.62) | .869 |
|
| |||
| Intervention Sitea | |||
| New South Wales | 8 (15.1%) | 12 (12.6%) | |
| Queensland | 14 (26.4%) | 34 (35.8%) | |
| Victoria | 10 (18.9%) | 16 (16.8%) | .723 |
| Western Australia | 13 (24.5%) | 20 (21.1%) | |
| Ohio | 8 (15.1%) | 13 (13.7%) | |
|
| |||
| Intervention Groupa | |||
| Baby-CIMT | 27 (50.9%) | 46 (48.4%) | .713 |
| Baby-BIM | 26 (49.1%) | 49 (51.6%) | |
|
| |||
| Hemiplegic Sidea | |||
| Right | 28 (52.8%) | 51 (53.7%) | .901 |
| Left | 25 (47.2%) | 44 (46.3%) | |
|
| |||
| HAI Imp Raw Score | |||
| Mean (SD) | 10.53 (6.41) | 10.09 (5.87) | .677 |
Abbreviations: REACH, Rehabilitation EArly for Congenital Hemiplegia; GA, gestational age; w, weeks; SD, standard deviation; m, months; CIMT, constraint-induced movement therapy; BIM, bimanual therapy; HAI Imp Raw Score, Hand Assessment for Infants Impaired Hand Raw Score
P values were the result of Chi-squared tests for categorical variables and t tests for continuous variables.
Frequency (proportion)
Therapist characteristics
Years of clinical practice experience for therapists who delivered REACH interventions are in Table 2. Therapists varied in the number of infants treated during the REACH trial. The proportion of infants treated in sessions scored for the present study did not differ significantly from the proportions treated for the REACH trial overall.
Table 2.
Study Therapist Practice Experience and Proportion of Infants Treated in Sessions Scored for Fidelity of Delivery versus the REACH Trial Overall
| Years of Professional Experience |
|||||
|---|---|---|---|---|---|
| Therapist | Pediatrics | Children with UCP | Scored Sessions (N=72 sessions)a | REACH Trial (N=95 infants)b | P Value |
|
| |||||
| 1 | 5–10 | 8+ | 14 (19.4%) | 15 (15.8%) | .476 |
| 2 | 10–15 | 8+ | 11 (15.3%) | 10 (10.5%) | |
| 3 | 10–15 | 6–8 | 3 (4.2%) | 4 (4.2%) | |
| 4 | 20+ | 8+ | 4 (5.6%) | 6 (6.3%) | |
| 5 | 5–10 | 8+ | 3 (4.2%) | 4 (4.2%) | |
| 6 | 15–20 | 8+ | 9 (12.5%) | 7 (7.4%) | |
| 7 | 20+ | 8+ | 1 (1.4%) | 1 (1.1%) | |
| 8 | 10–15 | 6–8 | 7 (9.7%) | 8 (8.4%) | |
| 9 | 15–20 | 8+ | 10 (13.9%) | 26 (27.4%) | |
| 10 | 20+ | 8+ | 0 (0%) | 1 (1.1%) | |
| 11 | 5–10 | 4–6 | 5 (6.9%) | 6 (6.3%) | |
| 12 | 5–10 | 0–2 | 5 (6.9%) | 7 (7.4%) | |
Abbreviations: REACH, Rehabilitation EArly for Congenital Hemiplegia; CP, cerebral palsy; UCP, unilateral cerebral palsy.
Years of professional experience based on therapist self-report on the therapist survey.
Proportions calculated based on a total number of 72 session randomly selected for assessing fidelity of delivery for this study.
Proportions calculated based on a total number of 95 infants who received intervention for the REACH trial.
P value was from the result of a Chi-squared test to assess the proportion of intervention sessions scored for fidelity of delivery compared with the proportion of infants treated in the REACH trial for each therapist.
Therapist Fidelity Checklist Reliability
Average percentage agreement between raters was 84.3% (range 37% – 100%). For intra-rater reliability, percentage agreement for individual items between ratings was 95% (range 77% – 100%), indicating excellent agreement.35 Based on reliability results, 13 items were removed from the original TFC for the following reasons: poor inter- or intra-rater agreement, frequently not observed during sessions, not considered essential to the interventions, having multiple or poorly defined components, or redundancy with other items (Supplemental Digital Content 1). The revised TFC had 8 items (Supplemental Digital Content 2) and was used in the present sub-study. Items were scored as 2 (full adherence), 1 (partial adherence), 0 (absent), or P (proscribed). The maximum score of the checklist was 16.
Therapist Fidelity Checklist Total Scores
Frequencies of TFC total scores across all scored sessions are graphed in Figure 1. Total scores ranged from 9–16, with a median (IQR) of 16 (14, 16). Most sessions (n=64, 88.9%) were scored as high fidelity of delivery (score ≥13 out of 16). The remaining 8 sessions (11.1%) were scored as moderate fidelity (TFC scores 8–12 out of 16).
Therapist Fidelity Checklist Item Scores
No items were scored as P (proscribed) for any intervention session, meaning that therapists were not observed adding intervention components that were not described in the manual during scored sessions. The proportion of sessions for which individual TFC items were scored as 2, 1, and 0 are graphed for sessions scored as high versus moderate fidelity in Figure 2. The items “Working with Infant,” “Infant Position,” “Intervention Accuracy,” and “Constraint Use” were never scored 0 and were scored 2 in most (75–98.4%) sessions regardless of Total Score. The items “Family Comprehension,” “Therapist Intervention-Specific Skills,” “Play Sequences,” and “Intervention-Specific Strategies” were scored 2 in most (84.4–98.4%) sessions with high fidelity of delivery. In contrast, for sessions with moderate fidelity, these same items were scored as 2 for 0–37.5% of the sessions and as 0 for 12.5–62.5% (Figure 2).
Figure 2.

100% stacked columns represent the proportion of the total number of sessions scored as high fidelity of delivery (Therapist Fidelity Checklist Total Score ≥13 out of 16, n=64) or moderate fidelity of delivery (Therapist Fidelity Checklist Total Score of 8–12 out of 16, n=8). Shading indicates the score for each individual checklist item.
Infant characteristics, parent engagement, and fidelity of delivery
No significant relationships were found between TFC Total Scores and infant age (p=.054), HAI Impaired Hand Raw Score (p=.205), or PRIME-G Total Score (p=.377).
Fidelity of delivery, intervention group, and prior therapist experience
TFC total scores by intervention group, timing of home visit, and prior therapist experience are in Figure 3. All infants treated in the 8 sessions with moderate fidelity were randomized to the Baby-BIM group (Figure 3a). Six of the 8 sessions (75.0%) with moderate fidelity occurred in the second half (home visit 4 or later) of the intervention period (Figure 3b). Therapists had a range of prior professional experience in pediatrics and with children with UCP (Table 2). TFC Total Scores are similar across years of pediatric experience (Figure 3c) and experience with children with UCP (Figure 3d).
Figure 3.
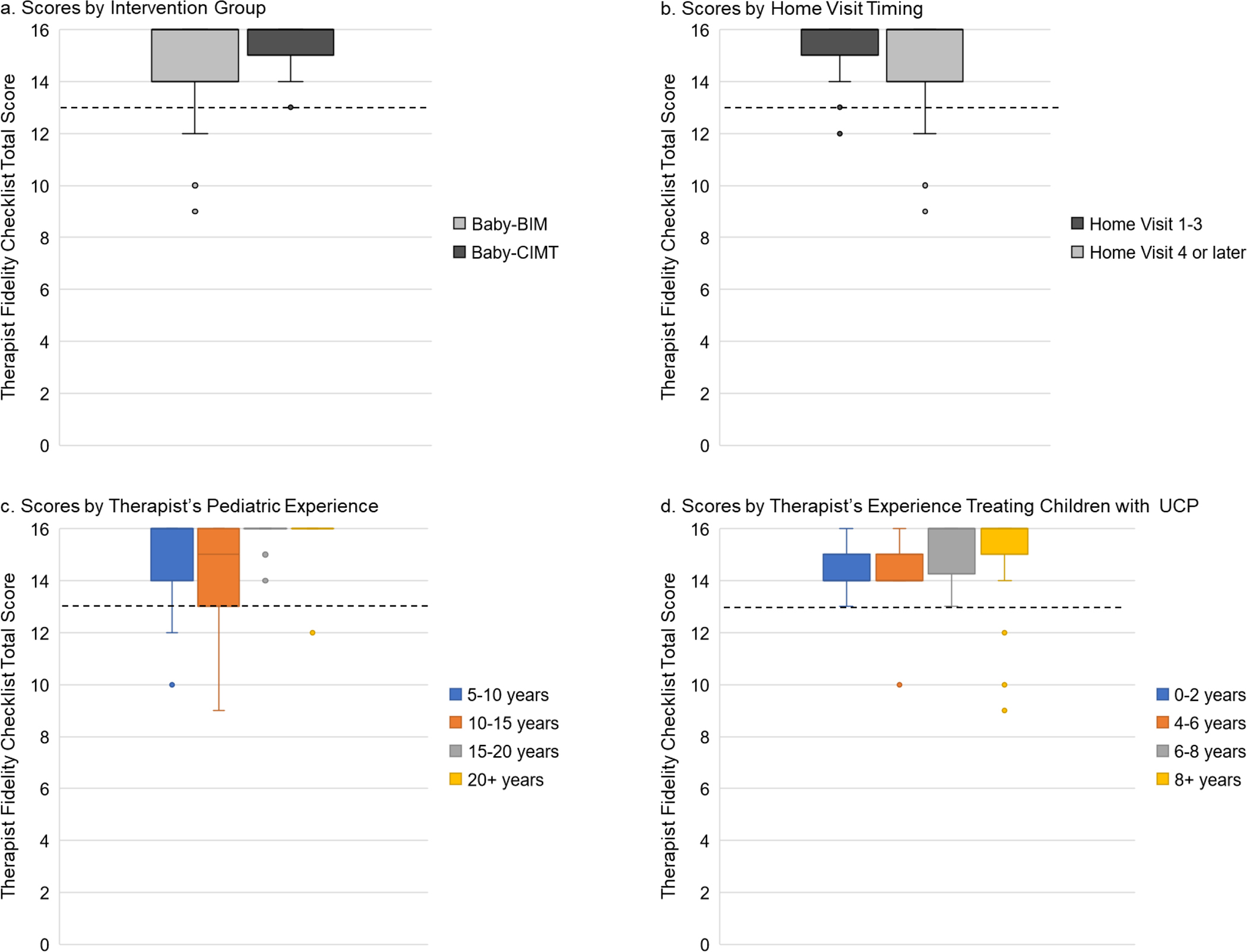
Abbreviations: UCP, unilateral cerebral palsy; Baby-BIM, infant-friendly bimanual therapy; Baby-CIMT, infant-friendly constraint-induced movement therapy.
Box and whisker plots of the distribution of Therapist Fidelity Checklist Total Scores for (3a) Baby-BIM versus Baby-CIMT intervention groups (Baby-BIM, n=39; Baby-CIMT, n=33); (3b) Home visits 1–3 by the study therapist (n=45) versus home visits 4 or later (n=27); (3c) Prior pediatric experience (5–10 years, n=27; 10–15 years, n=21; 15–20 years, n=19; 20+ years, n=5); and Years of experience treating children with UCP (0–2 years, n=5; 4–6 years, n=5; 6–8 years, n=10; 8+ years, n=52). The dotted line indicates a Therapist Fidelity Checklist Total Score of 13 out of 16 (>80%), corresponding to high fidelity of delivery.
Discussion
When complex interventions are delivered to infants with UCP by parents using a coaching model, fidelity of therapist delivery must be measured and reported to understand intervention effectiveness.18,36 For the REACH trial, Baby-BIM and Baby-CIMT involved multiple components tailored to the individual needs of infant’s based on their manual abilities. Intervention occurred across multiple, international sites. Parents were supported by trained therapists with a range of prior clinical experience to provide intervention to their infants at home. The results of the present study indicate high fidelity of delivery for the REACH trial in most home intervention sessions. Standardized training, comprehensive intervention manuals, monthly therapist-to-therapist support, and a fidelity monitoring plan contributed to these findings. In cases of moderate fidelity, results indicate that ongoing monitoring is important to ensure consistency in delivery throughout an intervention period. Baby-BIM may have become more challenging from the intervention midpoint in a small number of cases as infants became more lateralized in their manual abilities.
No standard measures of fidelity of delivery currently exist for early interventions for infants with UCP.18 There are fidelity of delivery measures for more general use. For example, the Pediatric Rehabilitation Observational measure of Fidelity (PROF) may be useful when monitoring generic behaviors, such as therapist-family rapport.37 Intervention-specific measures, rather than generic checklists, are important to use when investigating intervention effectiveness, such as in the REACH trial, because key intervention components can be defined within the measure.23 Researchers investigating intervention for children with CP or other neurodevelopmental disorders have developed intervention-specific measures of fidelity of delivery.23,38,39 The Children with Hemiparesis Arm and Movement Project (CHAMP) used a checklist to score randomly selected video-recorded intervention sessions between therapists and children for a therapist-directed intervention.38,40 The START-Play intervention occurred during collaborative sessions among a therapist, parent, and infant.9 One intervention session was scored using a checklist in cases when parents and therapist consented to video-recording in the START-Play trial.23 Similar to our results, START-Play therapists achieved the a-priori threshold for fidelity of delivery for most intervention behaviors after standardized training.23 Importantly, all intervention sessions for the REACH trial were video-recorded as part of the study protocol. This allowed random selection of a sample of intervention sessions across the intervention period for evaluating fidelity of delivery. Our selected sessions included a representative sample of families, intervention sites, therapists, intervention groups, and infants. The demands of tool development present a potential barrier for researchers who plan to measure fidelity of delivery. Currently, there is no way to directly compare fidelity of delivery across these studies using different intervention-specific measures. Development of a template for defining key intervention-specific components used to measure fidelity of delivery could promote more widespread measurement and reporting of fidelity and enable comparison of fidelity across intervention trials.
Consistent with recommendations for monitoring and enhancing intervention fidelity, we established an a-priori threshold for fidelity of delivery for REACH.19,33 Our threshold for high (>80%) and moderate (50–80%) has been used by others investigating fidelity.33,34,41 Importantly, the impact of different levels of fidelity of delivery on intervention outcomes is unknown.41,42 There is some evidence that greater fidelity of delivery yields better outcomes.36 There are, however, examples of perfect fidelity of delivery (100%) and poor intervention outcomes in adult populations.43 This may be due to a potentially ineffective intervention, or it may be that the intervention was not fully engaged with or enacted by participating families in the context of their daily lives.18,29,44 Further investigation is needed to understand the implications for high, moderate, and poor fidelity of delivery and the relationship to parent enactment of intervention with their child.
There were circumstances in which therapists had greater difficulty employing their intervention skills. In all cases of moderate fidelity of delivery, Baby-BIM was being delivered, mostly at or after the intervention midpoint. During that time of the intervention period, infants were 7–12 months CA. Skills required for implementing the Baby-BIM intervention may be more challenging in some circumstances as the intervention period progressed. For example, as infants’ bimanual skills became more lateralized, it may have been more challenging to deliver the essential components of the Baby-BIM intervention. Neurodevelopment may contribute to these findings. For infants with UCP, reorganization of bilateral corticospinal modulation can be disrupted to a variable extent by perinatal brain damage and result in primarily contralateral UE activation, bilateral activation patterns, or primarily ipsilateral activation.45 These patterns of re-organization may impact UE function, with children demonstrating poorer dexterity and bimanual skills when their more impaired hand is controlled primarily by ipsilateral corticospinal projections.45 It may be that as infants in the present study experienced greater difficulty performing advanced fine motor skills with their more impaired hand, they developed stronger lateralization where they used their less impaired hand to a greater extent for these tasks. This may have presented a unique challenge when delivering Baby-BIM versus Baby-CIMT because infants may have demonstrated less persistence at bimanual actions in the absence of a restraint.
Monitoring fidelity over time can reduce drift away from delivering the intervention as designed. Home intervention sessions were video recorded for the REACH trial to enable scoring of the TFC at different time points during the intervention period. Monitoring fidelity while intervention is being delivered affords the opportunity to implement additional supports to enhance fidelity for specific therapists in real time rather than waiting until a trial is complete to discover drift in fidelity.42 For REACH, ongoing training and monthly peer-to-peer support were provided to individual therapists using case studies to avoid inadequate fidelity of delivery.
Previous clinical experience was explored as a potential factor impacting therapist delivery for the REACH trial. Some researchers have found that length of provider experience does not relate to fidelity of delivery.23,46 Others have found that fidelity was poorer among inexperienced providers.46,47 Inconsistent findings may relate to different strategies used to measure fidelity of delivery. Professional experience has been found to significantly relate to some aspects of fidelity of delivery (quality of intervention delivery), but not related to other aspects (adherence to intervention behaviors).46 Type of previous clinical experience is important as self-efficacy and skills develop from domain-specific experience more than overall years of experience.48 For example, a pediatric therapist might have experience implementing CIMT in a clinic setting, but they may have limited experience with a parent coaching or home-based intervention. Our results are consistent with others who have suggested that standard training of providers may overcome variability of prior professional experience to optimize fidelity of delivery.23
Conclusion
Fidelity of delivery was high for both interventions in the REACH trial (Baby-CIMT and Baby-BIM) for most home intervention sessions. Standardized training, manualization of intervention components, regular therapist peer-to-peer support, and a fidelity monitoring plan may have contributed to these findings. In cases of moderate fidelity, results indicate that some interventions (i.e., Baby-BIM) may be more challenging to deliver as designed over time. Ongoing monitoring and additional training as needed are important to ensure consistency in delivery throughout an intervention period.
Limitations
The TFC was developed specifically for use within the REACH trial. This limits the generalizable use of this measure of fidelity of delivery. Percent agreement was calculated for inter- and intra-rater reliability of the TFC, which does not account for agreement between ratings by chance. It may be that scoring a larger proportion of home visit sessions (>10% selected for the present study) may have yielded different results, yet this limitation was minimized by using a randomly selected sample of intervention sessions. Our results indicate that the selection strategy was effective in obtaining a representative sample based on characteristics of the overall REACH trial. Finally, differential weighting of items on the TFC could have revealed greater variability in fidelity of delivery and may have impacted our results.
Supplementary Material
WHAT THIS ADDS TO THE EVIDENCE:
Standardized therapist training, manualization of intervention principles and components, and regular peer-to-peer support throughout an intervention period can result in high fidelity of delivery for complex interventions, such as infant-friendly constraint-induced movement therapy (Baby-CIMT) and bimanual therapy (Baby-BIM). Ongoing monitoring and additional training are needed to ensure consistency in delivery over time. The impact of high fidelity of delivery on the extent that parents enact intervention activities with their child in the home requires further investigation.
Acknowledgements
We would like to thank the families who participated in the REACH study. The work done by these families made this research possible. Thank you to Mollie Moore and Thalia Prakash, 4th year Occupational Therapy honors students in the School of Health and Rehabilitation Sciences at The University of Queensland for your contributions. We would also like to acknowledge the REACH study therapists who provided intervention for this trial.
Grant Support:
The REACH trial is funded by the Australian National Health and Medical Research Council (NHMRC) Project Grant for REACH 1059332; LS was supported by a NHMRC Career Development Fellowship (1160694); NHMRC Research Fellowship (RB) 1105038. KS was funded in part by a mentored award through the APTA Academy of Pediatric Physical Therapy and by the National Center for Advancing Translational Sciences (TL1TR002735). JCH was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (5P2CHD101912-03).
Footnotes
Conflict of Interest Statement: The authors declare no conflicts of interest.
References
- 1.ACPR Register Group. Australian Cerebral Palsy Register Report. Cerebral Palsy Alliance Research Institute; 2018. [Google Scholar]
- 2.Novak I, Morgan C, Fahey M, et al. State of the Evidence Traffic Lights 2019: Systematic Review of Interventions for Preventing and Treating Children with Cerebral Palsy. Curr Neurol Neurosci Rep. 2020;20(2):3. doi: 10.1007/s11910-020-1022-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sellier E, McIntyre S, Smithers-Sheedy H, Platt MJ, SCPE and ACPR Groups. European and Australian Cerebral Palsy Surveillance Networks Working Together for Collaborative Research. Neuropediatrics. 2020;51(2):105–112. doi: 10.1055/s-0039-3402003 [DOI] [PubMed] [Google Scholar]
- 4.LaForme Fiss A, McCoy SW, Bartlett D, Avery L, Hanna SE, On Track Study Team. Developmental Trajectories for the Early Clinical Assessment of Balance by Gross Motor Function Classification System Level for Children With Cerebral Palsy. Phys Ther. 2019;99(2):217–228. doi: 10.1093/ptj/pzy132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sakzewski L, Ziviani J, Boyd RN. Efficacy of upper limb therapies for unilateral cerebral palsy: a meta-analysis. Pediatrics. 2014;133(1):e175–204. doi: 10.1542/peds.2013-0675 [DOI] [PubMed] [Google Scholar]
- 6.Wiklund LM, Uvebrant P. Hemiplegic cerebral palsy: correlation between CT morphology and clinical findings. Dev Med Child Neurol. 1991;33(6):512–523. [DOI] [PubMed] [Google Scholar]
- 7.Imms C, Reilly S, Carlin J, Dodd KJ. Characteristics influencing participation of Australian children with cerebral palsy. Disabil Rehabil. 2009;31(26):2204–2215. doi: 10.3109/09638280902971406 [DOI] [PubMed] [Google Scholar]
- 8.Eliasson AC, Forssberg H, Hung YC, Gordon AM. Development of hand function and precision grip control in individuals with cerebral palsy: a 13-year follow-up study. Pediatrics. 2006;118(4):e1226–1236. doi: 10.1542/peds.2005-2768 [DOI] [PubMed] [Google Scholar]
- 9.Harbourne RT, Dusing SC, Lobo MA, et al. START-Play Physical Therapy Intervention Impacts Motor and Cognitive Outcomes in Infants With Neuromotor Disorders: A Multisite Randomized Clinical Trial. Phys Ther. 2021;101(2):pzaa232. doi: 10.1093/ptj/pzaa232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Novak I, Morgan C, Adde L, et al. Early, Accurate Diagnosis and Early Intervention in Cerebral Palsy: Advances in Diagnosis and Treatment. JAMA Pediatr. 2017;171(9):897–907. doi: 10.1001/jamapediatrics.2017.1689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eliasson AC, Nordstrand L, Ek L, et al. The effectiveness of Baby-CIMT in infants younger than 12 months with clinical signs of unilateral-cerebral palsy; an explorative study with randomized design. Res Dev Disabil. 2018;72:191–201. doi: 10.1016/j.ridd.2017.11.006 [DOI] [PubMed] [Google Scholar]
- 12.Chamudot R, Parush S, Rigbi A, Horovitz R, Gross-Tsur V. Effectiveness of Modified Constraint-Induced Movement Therapy Compared With Bimanual Therapy Home Programs for Infants With Hemiplegia: A Randomized Controlled Trial. Am J Occup Ther. 2018;72(6):7206205010p1–7206205010p9. doi: 10.5014/ajot.2018.025981 [DOI] [PubMed] [Google Scholar]
- 13.Maitre NL, Jeanvoine A, Yoder PJ, et al. Kinematic and Somatosensory Gains in Infants with Cerebral Palsy After a Multi-Component Upper-Extremity Intervention: A Randomized Controlled Trial. Brain Topogr. 2020;33(6):751–766. doi: 10.1007/s10548-020-00790-5 [DOI] [PubMed] [Google Scholar]
- 14.Boyd RN, Ziviani J, Sakzewski L, et al. REACH: study protocol of a randomised trial of rehabilitation very early in congenital hemiplegia. BMJ Open. 2017;7(9):e017204. doi: 10.1136/bmjopen-2017-017204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337:a1655. doi: 10.1136/bmj.a1655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Skivington K, Matthews L, Simpson SA, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ. 2021;374:n2061. doi: 10.1136/bmj.n2061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rixon L, Baron J, McGale N, Lorencatto F, Francis J, Davies A. Methods used to address fidelity of receipt in health intervention research: a citation analysis and systematic review. BMC Health Serv Res. 2016;16(1):663. doi: 10.1186/s12913-016-1904-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Walton H, Spector A, Tombor I, Michie S. Measures of fidelity of delivery of, and engagement with, complex, face-to-face health behaviour change interventions: A systematic review of measure quality. Br J Health Psychol. 2017;22(4):872–903. doi: 10.1111/bjhp.12260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bellg AJ, Borrelli B, Resnick B, et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium. Health Psychol. 2004;23(5):443–451. doi: 10.1037/0278-6133.23.5.443 [DOI] [PubMed] [Google Scholar]
- 20.An M, Dusing SC, Harbourne RT, Sheridan SM, START-Play Consortium. What Really Works in Intervention? Using Fidelity Measures to Support Optimal Outcomes. Phys Ther. Published online January 16, 2020. doi: 10.1093/ptj/pzaa006 [DOI] [PubMed] [Google Scholar]
- 21.Keogh A, Matthews J, Hurley DA. An assessment of physiotherapist’s delivery of behaviour change techniques within the SOLAS feasibility trial. Br J Health Psychol. 2018;23(4):908–932. doi: 10.1111/bjhp.12323 [DOI] [PubMed] [Google Scholar]
- 22.Dusing SC, Harbourne RT, Hsu LY, et al. The SIT-PT Trial Protocol: A Dose-Matched Randomized Clinical Trial Comparing 2 Physical Therapist Interventions for Infants and Toddlers With Cerebral Palsy. Phys Ther. 2022;102(7):pzac039. doi: 10.1093/ptj/pzac039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.An M, Nord J, Koziol NA, et al. Developing a fidelity measure of early intervention programs for children with neuromotor disorders. Dev Med Child Neurol. 2021;63(1):97–103. doi: 10.1111/dmcn.14702 [DOI] [PubMed] [Google Scholar]
- 24.Dusing SC, Burnsed JC, Brown SE, et al. Efficacy of Supporting Play Exploration and Early Development Intervention in the First Months of Life for Infants Born Very Preterm: 3-Arm Randomized Clinical Trial Protocol. Phys Ther. 2020;100(8):1343–1352. doi: 10.1093/ptj/pzaa077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Einspieler C, Prechtl H, Bos A, Ferrari F, Cioni G. Prechtl’s Method on the Qualitative Assessment of General Movements in Preterm, Term and Young Infants. Mac Keith Press; 2004. [DOI] [PubMed] [Google Scholar]
- 26.Romeo DM, Ricci D, Brogna C, Mercuri E. Use of the Hammersmith Infant Neurological Examination in infants with cerebral palsy: a critical review of the literature. Dev Med Child Neurol. 2016;58(3):240–245. doi: 10.1111/dmcn.12876 [DOI] [PubMed] [Google Scholar]
- 27.Romeo DMM, Cioni M, Palermo F, Cilauro S, Romeo MG. Neurological assessment in infants discharged from a neonatal intensive care unit. Eur J Paediatr Neurol. 2013;17(2):192–198. doi: 10.1016/j.ejpn.2012.09.006 [DOI] [PubMed] [Google Scholar]
- 28.Krumlinde-Sundholm L, Ek L, Sicola E, et al. Development of the Hand Assessment for Infants: evidence of internal scale validity. Dev Med Child Neurol. 2017;59(12):1276–1283. doi: 10.1111/dmcn.13585 [DOI] [PubMed] [Google Scholar]
- 29.Walton H, Spector A, Williamson M, Tombor I, Michie S. Developing quality fidelity and engagement measures for complex health interventions. Br J Health Psychol. 2020;25(1):39–60. doi: 10.1111/bjhp.12394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.PRIME Research Team. Project Summary. PRIME: The Pediatric Rehabilitation Intervention Measure of Engagement (PRIME) Team. Published 2021. Accessed November 2, 2021. http://primeresearchteam.com/project-summary/ [Google Scholar]
- 31.Ek L, Eliasson AC, Sicola E, et al. Hand Assessment for Infants: normative reference values. Dev Med Child Neurol. 2019;61(9):1087–1092. doi: 10.1111/dmcn.14163 [DOI] [PubMed] [Google Scholar]
- 32.Ullenhag A, Ek L, Eliasson AC, Krumlinde-Sundholm L. Interrater and test-retest reliability of the Hand Assessment for Infants. Dev Med Child Neurol. Published online July 5, 2021. doi: 10.1111/dmcn.14967 [DOI] [PubMed] [Google Scholar]
- 33.Borrelli B. The Assessment, Monitoring, and Enhancement of Treatment Fidelity In Public Health Clinical Trials. J Public Health Dent. 2011;71(s1):S52–S63. doi: 10.1111/j.1752-7325.2011.00233.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Boutron I, Altman DG, Moher D, Schulz KF, Ravaud P, CONSORT NPT Group. CONSORT Statement for Randomized Trials of Nonpharmacologic Treatments: A 2017 Update and a CONSORT Extension for Nonpharmacologic Trial Abstracts. Ann Intern Med. 2017;167(1):40–47. doi: 10.7326/M17-0046 [DOI] [PubMed] [Google Scholar]
- 35.Terwee CB, Mokkink LB, Knol DL, Ostelo RWJG, Bouter LM, de Vet HCW. Rating the methodological quality in systematic reviews of studies on measurement properties: a scoring system for the COSMIN checklist. Qual Life Res. 2012;21(4):651–657. doi: 10.1007/s11136-011-9960-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Durlak JA, DuPre EP. Implementation matters: a review of research on the influence of implementation on program outcomes and the factors affecting implementation. Am J Community Psychol. 2008;41(3–4):327–350. doi: 10.1007/s10464-008-9165-0 [DOI] [PubMed] [Google Scholar]
- 37.Di Rezze B, Law M, Eva K, Pollock N, Gorter JW. Development of a generic fidelity measure for rehabilitation intervention research for children with physical disabilities. Dev Med Child Neurol. 2013;55(8):737–744. doi: 10.1111/dmcn.12114 [DOI] [PubMed] [Google Scholar]
- 38.Ramey SL, DeLuca S, Stevenson RD, Case-Smith J, Darragh A, Conaway M. Children with Hemiparesis Arm and Movement Project (CHAMP): protocol for a multisite comparative efficacy trial of paediatric constraint-induced movement therapy (CIMT) testing effects of dosage and type of constraint for children with hemiparetic cerebral palsy. BMJ Open. 2019;9(1):e023285. doi: 10.1136/bmjopen-2018-023285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Beckers L, Smeets R, de Mooij M, et al. Process Evaluation of Home-based Bimanual Training in Children with Unilateral Cerebral Palsy (The COAD-study): A Mixed Methods Study. Dev Neurorehabil. Published online December 26, 2021:1–17. doi: 10.1080/17518423.2021.2011459 [DOI] [PubMed] [Google Scholar]
- 40.Ramey SL, DeLuca SC, Stevenson RD, et al. Constraint-Induced Movement Therapy for Cerebral Palsy: A Randomized Trial. Pediatrics. 2021;148(5):e2020033878. doi: 10.1542/peds.2020-033878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.French SD, Green SE, Francis JJ, et al. Evaluation of the fidelity of an interactive face-to-face educational intervention to improve general practitioner management of back pain. BMJ Open. 2015;5(7):e007886. doi: 10.1136/bmjopen-2015-007886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Breitenstein SM, Gross D, Garvey CA, Hill C, Fogg L, Resnick B. Implementation fidelity in community-based interventions. Res Nurs Health. 2010;33(2):164–173. doi: 10.1002/nur.20373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Barber JP, Gallop R, Crits-Christoph P, et al. The role of therapist adherence, therapist competence, and alliance in predicting outcome of individual drug counseling: Results from the National Institute Drug Abuse Collaborative Cocaine Treatment Study. Psychotherapy Research. 2006;16(2):229–240. doi: 10.1080/10503300500288951 [DOI] [Google Scholar]
- 44.King G, Chiarello LA, McLarnon MJW, et al. A measure of parent engagement: plan appropriateness, partnering, and positive outcome expectancy in pediatric rehabilitation sessions. Disabil Rehabil. Published online January 4, 2021:1–10. doi: 10.1080/09638288.2020.1864036 [DOI] [PubMed] [Google Scholar]
- 45.Simon-Martinez C, Jaspers E, Mailleux L, et al. Corticospinal Tract Wiring and Brain Lesion Characteristics in Unilateral Cerebral Palsy: Determinants of Upper Limb Motor and Sensory Function. Neural Plast. 2018;2018:2671613. doi: 10.1155/2018/2671613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Knoche LL, Sheridan SM, Edwards CP, Osborn AQ. Implementation of a Relationship-Based School Readiness Intervention: A Multidimensional Approach to Fidelity Measurement for Early Childhood. Early Child Res Q. 2010;25(3):299–313. doi: 10.1016/j.ecresq.2009.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dane AV, Schneider BH. Program integrity in primary and early secondary prevention: are implementation effects out of control? Clin Psychol Rev. 1998;18(1):23–45. doi: 10.1016/s0272-7358(97)00043-3 [DOI] [PubMed] [Google Scholar]
- 48.Eccles JS. Expectancies, values and academic behaviors. In: Achievement and Achievement Motives. Freeman; 1983:75–146. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


