Abstract
Background:
Underrepresentation of women in plastic surgery remains a concern. This study investigates gender-related differences in self-confidence and surgical ability among plastic surgery trainees in an effort to work toward gender parity.
Methods:
Residents and fellows were recorded performing up to three cleft lip repairs on a high-fidelity simulator. Demographic information was collected, and two questionnaires were completed to assess self-confidence after each simulation. Videos were rated blindly using the objective structured assessment of technical skills and unilateral cleft lip repair competency assessment tool. Differences between participants were estimated using generalized estimating equations modeling, and correlation between overall self-confidence and performance was examined using Pearson correlation (r).
Results:
Twenty-six participants (six self-identified women and 20 self-identified men) completed 73 simulated procedures. There was no gender-related difference in training level, volume of prior experience, speed with which participants completed each simulated procedure, or objective performance. However, a significant difference was found in overall procedural self-confidence, with women rating their confidence lower (mean = 16.9, SD = 4.3) than men (mean = 19.4, SD = 3.8); P = 0.021. Further analysis revealed that confidence scores correlated more strongly with objective performance for women (r = 0.83) than for men (r = 0.45).
Conclusions:
Women plastic surgery trainees overall reported lower self-confidence than their male counterparts, despite demonstrating at least as much skill. Confidence and skill were more closely related for women, suggesting that mentorship focused on concrete skill building may help close the confidence gap.
Takeaways
Question: Can simulation help illuminate gender-related differences in trainee self-confidence and its relationship with surgical skill?
Findings: In a group of plastic surgery trainees taking part in cleft lip simulation, women reported lower self-confidence than their male counterparts, despite demonstrating at least as much skill. However, confidence and skill were more closely related for women.
Meaning: Gender-related disparities in self-confidence persist despite similar surgical skill. Because others’ perception of an individual’s competence is related to their confidence, addressing this gap is a necessary step toward gender parity.
INTRODUCTION
Similar to other surgical specialties, the gap in female representation within plastic surgery has been steadily narrowing in recent decades. Despite this, concern persists about disparities in opportunity, ranging from female representation within plastic surgery leadership, to retention and promotion in academic surgical departments, salary, and even in how residents are recruited and trained.1,2 Along with this, research has emerged that women residents in plastic surgery and other surgical specialties report lower levels of confidence than their male colleagues3–5 and that compared with evaluations of their performance by attending surgeons, women underrate their performance, whereas men overrate their performance.6 Self-confidence has self-fulfilling effects, bringing more opportunities to those who simply seem more confident.7 Thus, this gap in confidence between female and male residents has implications for how attending surgeons and others in positions of authority perceive their competence,8–10 which has potential ramifications for the effectiveness of education provided during training and access to future career opportunities.
Over the past several years, we have accumulated experience with how plastic surgery residents and fellows assess themselves in the setting of cleft lip simulation. Observations made during these sessions, and the lack of literature on gender variation in plastic surgery trainee confidence, prompted us to further inspect gender-specific differences. The purpose of this investigation was to determine if a difference in self-confidence exists in the low-stress setting of simulation and whether confidence correlates with surgical ability. We hypothesized that female residents report lower self-confidence despite having similar surgical skill. This is a relationship we can uniquely measure in the context of simulation in a way that is difficult to do in real life for two reasons. First, because the procedures in this study were conducted from start to finish without guidance, influence (and possible biases) of a supervising surgeon on forward progress of the procedure is reduced. Second, simulation allows for gender-blind evaluation of competence which cannot happen in a live operative setting, mitigating potential for implicit bias on the part of the rater.
METHODS
The current work is a secondary analysis of cleft lip simulation data prospectively collected for a previous institutional review board–exempt (IRB-P00035608) educational study.11 In that investigation, plastic surgery trainees from rotating residency programs and from the craniofacial/pediatric plastic surgery fellowship at our hospital were videotaped while performing up to three unilateral cleft lip repairs (UCLRs) on a high-fidelity simulator without instruction or guidance during the operation (Fig. 1). The initial repair was followed by structured debriefing and an immediate second repair to apply lessons learned. The third simulation occurred approximately three months later to test for knowledge retention (Fig. 2). Demographic information was collected at the beginning of the study, including gender, postgraduate year, training track (independent resident, integrated resident, and craniofacial/pediatric plastic surgery fellow), and self-reported number of cleft lip procedures previously participated in. Additional experience with cleft lip repair gained between the first two and the third simulation was extracted from hospital case logs.
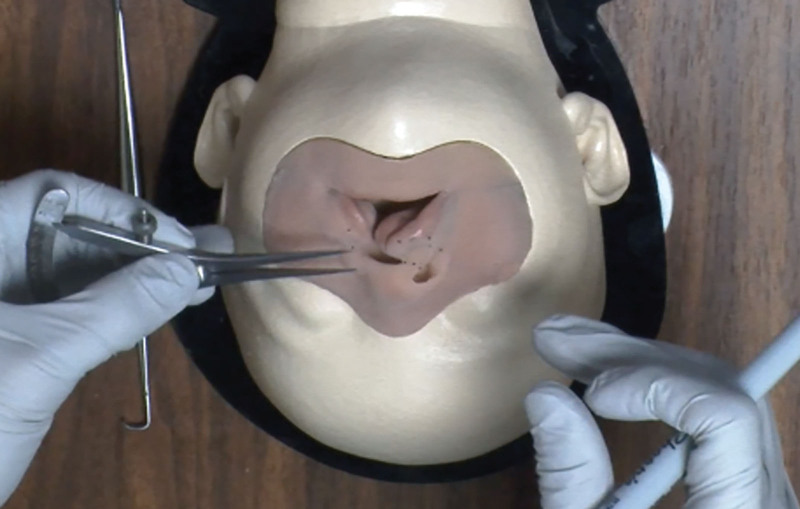
Fig. 1.
Overhead video view used for rating simulated procedures.
Fig. 2.
Simulation workflow. Three simulation (sim) sessions were conducted. After each simulation, participants completed two confidence questionnaires (survey) and then underwent a structured feedback session (debrief).
After finishing each simulation, trainees completed two questionnaires about their confidence with the procedure. The first pertained to their general self-confidence and feelings during the procedure (eg, “were you worried during the procedure?”), whereas the second assessed their confidence performing specific elements of the operation being simulated (eg, “I can independently mark a UCLR”). The first survey was a validated procedural self-confidence survey consisting of six questions rated on a five-point Likert-style scale (score range 6–30). (See appendix, Supplemental Digital Content 1, which displays overall procedural self-confidence scale, http://links.lww.com/PRSGO/C942.) The second survey was a cleft lip repair–specific assessment of knowledge/skill consisting of six questions rated on a four-point Likert-scale (score range 6–24) designed for a previous study.12 (See appendix, Supplemental Digital Content 2, which displays the confidence with cleft lip specific knowledge/skill scale, http://links.lww.com/PRSGO/C943.)
Participants’ videos were blindly rated posthoc by a single cleft surgeon using the modified objective structured assessment of technical skills (OSATS, score range 4–20; See appendix, Supplemental Digital Content 3, which displays the modified OSATS scale, http://links.lww.com/PRSGO/C944), a global surgical skill score, and a procedure-specific 18-item UCLR competency assessment tool (score range 18–54; See appendix, Supplemental Digital Content 4, which displays the unilateral cleft lip repair competency assessment tool, http://links.lww.com/PRSGO/C945)13 that is both totaled and also subdivided into “marking,” “performing,” and “results” scores.
Continuous data are expressed as mean and SD. Fisher exact test was implemented to compare categorical data on participants in the training level by gender. To elucidate differences in experience, duration needed to complete the operation, self-reported questionnaire score, and objective video rating measures between men and women participants, P values were calculated using generalized estimating equations modeling to account for multiple simulations per subject and control for the training level. The relationship between overall procedural self-confidence and objectively rated performance was examined separately for men and women using Pearson correlation (r) and corresponding P values. All statistical analyses were performed using Statistical Package for the Social Sciences (SPSS, version 24; IBM, Armonk, N.Y.) and Stata software (version 16.1; StataCorp LLC, College Station, Tex.). A two-tailed P value less than 0.050 was considered statistically significant.
RESULTS
Twenty-six participants ranging from postgraduate year 3 through fellow (Table 1) completed a total of 73 simulated cleft lip repairs. All participants completed two simulations and 21 returned for the third session. Six participants were women; they performed a total of 17 simulated procedures. Twenty participants were men; they performed a total of 56 simulated procedures. There was no difference in the training level between women and men (P = 0.951). One male participant did not complete the initial procedural confidence and cleft lip self-assessment surveys.
Table 1.
Participant Training Levels
| Postgraduate Year | Female | Male |
|---|---|---|
| Integrated 3 | 1 | 3 |
| Integrated 4/independent 6 | 1 | 3 |
| Integrated 5/independent 7 | 1 | 7 |
| Integrated 6/independent 8 | 1 | 4 |
| Craniofacial/pediatric plastic surgery fellow | 2 | 3 |
| Total | 6 | 20 |
Integrated postgraduate year 4/independent postgraduate year 6, integrated postgraduate year 5/independent postgraduate year 7, and integrated postgraduate year 6/independent postgraduate year 8 residents were grouped together based on their analogous position in the rotation schedule.
When controlling for both training level and repeat simulations, there was no difference between men and women in volume of prior experience with cleft lip repair or in the speed with which they completed each simulated procedure. There was also no difference between men and women in objective performance both on the OSATS global surgical skill scale or on the total score for the cleft lip–specific UCLR scale. There was a difference in UCLR result subscore (women 10.5 versus men 9.4, P = 0.039), but no difference in UCLR marking or performing subscores.
Pertaining to subjective questionnaires, there was no significant difference in confidence performing specific cleft lip surgical skills in women (mean = 14.9, SD = 3.6) versus men (mean = 16.4, SD = 3.7; P = 0.051). A significant difference was found between men and women in overall procedural self-confidence, meaning how participants felt about the procedure and their level of comfort and anxiety, with women trainees rating their confidence lower (mean = 16.9, SD = 4.3) than men trainees (mean = 19.4, SD = 3.8; P = 0.021) (Table 2).
Table 2.
Comparison by Gender
| Variable | Female (n = 17) |
Male (n = 56) |
P Value |
|---|---|---|---|
| Total prior experience (n) | 13.8 (11.8) | 9.9 (11.6) | 0.527 |
| Duration of procedure (min) | 72.7 (26.1) | 85.4 (31.6) | 0.196 |
| Self-assessed knowledge/skill | 14.9 (3.6) | 16.4 (3.7) | 0.051 |
| Self-confidence | 16.9 (4.3) | 19.4 (3.8) | 0.021* |
| OSATS | 17.0 (2.3) | 16.6 (2.5) | 0.485 |
| UCLR total | 48.0 (3.9) | 45.1 (6.9) | 0.130 |
| UCLR marking | 11.0 (0.9) | 10.3 (1.6) | 0.150 |
| UCLR performing | 26.5 (2.7) | 25.4 (4) | 0.359 |
| UCLR result | 10.5 (1.2) | 9.4 (2.1) | 0.039* |
Data are presented as mean (SD).
P values were calculated using generalized estimating equations modeling to account for multiple simulations per subject and adjust for the postgraduate year level.
Statistically significant.
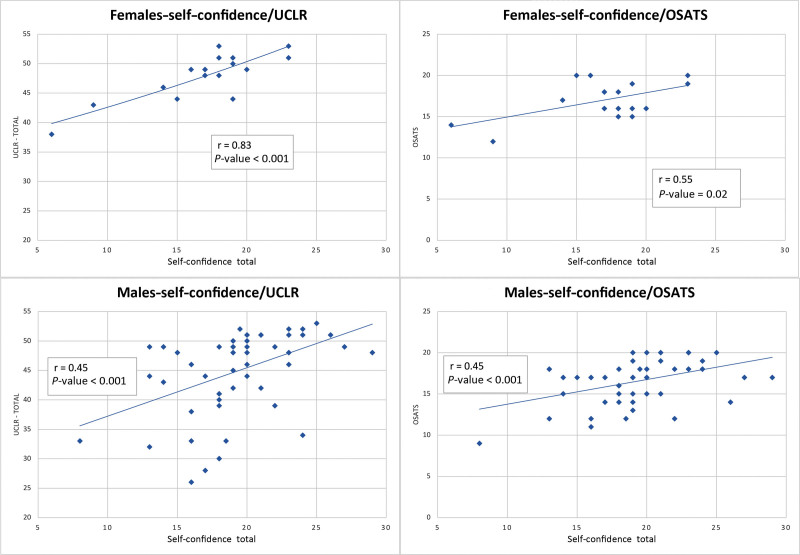
Delving further into overall procedural self-confidence, although scores significantly correlated with cleft lip repair performance (“UCLR–total”) for both men and women, confidence correlated more strongly with objective performance for women (r = 0.83, P < 0.001) than for men (r = 0.45, P < 0.001) (Fig. 3). A similar pattern was seen for global surgical skill (OSATS), but for women trainees the correlation was less compared with the procedure-specific scale (r = 0.55, P = 0.021), so the difference from their male colleagues was not as striking (r = 0.45, P < 0.001). In addition, individual questions of the procedural self-confidence questionnaire were granularly analyzed to determine if there were specific domains that could better point us to areas for disparity improvement. We found women scored significantly lower on the questions, “what was your surgical skill level during the procedure? (P = 0.036),” “were you anxious during the procedure?” (P = 0.008), and “based on your performance today, would you have liked to avoid this procedure altogether?” (P < 0.001) (Table 3).
Fig. 3.
Correlation between objective cleft lip specific performance and confidence.
Table 3.
Comparison of Individual Self-confidence Domains by Gender
| Question | Female (n = 17) |
Male (n = 56) |
P Value |
|---|---|---|---|
| How confident were you overall during the procedure? | 2.47 (0.80) | 2.62 (0.87) | 0.502 |
| What was your surgical skill level during the procedure? | 2.65 (0.61) | 2.96 (0.67) | 0.036* |
| Were you worried during the procedure? | 2.88 (0.86) | 3.02 (0.78) | 0.434 |
| Were you anxious during the procedure? | 2.59 (1.00) | 3.29 (0.81) | 0.008* |
| Based on your performance today, would you have liked to avoid this procedure altogether? | 3.53 (1.37) | 4.49 (0.74) | <0.001* |
| How comfortable are you with the independent planning and performing of the procedure? | 2.82 (0.81) | 3.00 (0.77) | 0.289 |
Data are presented as mean (SD).
P values were calculated using generalized estimating equations modeling to account for multiple simulations per subject and adjust for the postgraduate year level.
Statistically significant.
DISCUSSION
In the United States, the gender gap in female representation among plastic surgery residents has steadily narrowed over several decades.14 In 1998, only 13% of medical school graduates who pursued plastic surgery training were women, but by 2022 this proportion had risen to nearly 46%.14,15 Despite this progress, growth in female representation among practicing plastic surgeons has not yet caught up. According to the American Society of Plastic Surgeons, women currently constitute only 17% of board-certified plastic surgeons.16 In the academic plastic surgery setting, despite growth of female residents at a rate of 1% per year over the last 10 years to reach a current proportion of 40%, growth in female faculty has occurred more slowly, with women constituting only 22% of faculty, 12% of program directors, and less than 9% of department heads.17 Similarly, a recent analysis by Yin et al found that only 17% of plastic surgery leadership positions are held by women.18 Although data presented in these studies indicates that progress continues to be made, the “leaky pipeline” effect remains a concern. Moreover, recent literature has documented differences in pay between male and female surgeons that are not associated with time in practice.2 Thus, recognizing that gender parity remains incompletely rectified is a critical step in better addressing the problem.19
As awareness of gender-related disparities has grown and the gap in women working in surgical specialties has narrowed, interest in underlying causes of persistent inequity between men and women has arisen. Studies exploring gender-specific differences among surgical residents3–5 commonly focus on disparity in self-confidence. The available evidence indicates that there are disparities in the perception of confidence20 and perception of competence21 among male and female medical students and scientists by those observing them. The relationship between confidence and perceived competence has best been explored in the discipline of psychology. In their 1982 study, Schlenker and Leary8 found that when individuals seem more confident in their ability, they are perceived to be more competent. Another 2019 study by Ronay et al10 found that confidence increases others’ perception of an individual’s leadership potential, regardless of the individual’s actual competence. Synthesizing research on the relationship between confidence and perception of competence, business psychologist Nasher pointed out,9 “perceptions of competence are just as important for success as actual competence,” and “if you project confidence, others will tend to believe you know what you’re talking about, and they will then filter ambiguous information…to fit their initial impression.” This work raises concern that low self-confidence in the surgical training setting might be misinterpreted as a shortage of competence. Moreover, the amalgamation of these studies indicates that confident people could have more opportunities offered to them because they may be perceived as being more competent and better leaders. Conversely, lower confidence may limit career-advancing opportunities.
Theories exist to explain the gender difference in confidence including the influence of social constructs and disparity in educational opportunity.22 Regardless of the reason, to improve the experience of all plastic surgery trainees and ultimately obtain true gender equality within our profession, we must better understand the interplay between gender, confidence, and competence. Understanding these differences can help optimize educational quality and provide a learning environment in which both women and men trainees thrive.
Simulation provides a unique opportunity to assess self-perception and to measure global and procedure-specific skill in a blinded manner. Our results show that women report having less general confidence than men do, despite having at least as much surgical ability. This is a phenomenon objectively documented in other science, technology, engineering, and mathematics disciplines, for example, in computing, where women score similarly to men in objective accuracy but have lower self-reported confidence.23 Such disparity has also been reported in research from other surgical specialties.5,24 These findings also correlate with studies from the psychology literature, documenting greater levels of anxiety and negative emotions in women versus men, as they respond to perceived threats or punishment.25,26 What our results unearthed as a layer of complexity within the larger question of perceived versus intrinsic confidence and competence is that within the cohort of women trainees, confidence and ability had a stronger relationship than for the male cohort.
The ramifications of these results need further study but would suggest that confidence is more closely tied to actual surgical skill in female trainees, and that confidence and skill may not be as closely correlated in male trainees. Faculty members and clinical staff must be aware that on a group level, lower levels of confidence in women do not mean lower levels of competence. In fact, women performed equally to men on most objective measures and scored higher on the UCLR Results score. Rather, men as a whole view themselves more confidently with less of a relationship to their skill. Although having lower self-confidence on average does not seem to hinder women’s performance, it may be detrimental to how colleagues and supervisors perceive them and has been shown to be associated with a more reserved approach toward career-advancing opportunities.27 Awareness of these general differences between gender groups may facilitate a more nuanced understanding of and approach to trainees expressing varied levels of confidence.
Keane et al proposed ways to decrease the confidence gap between male and female plastic surgery residents. These strategies include dedicated curricula focused on leadership, communication skills, self-advocacy, and highlighting women’s accomplishments.1 Our pilot analysis adds to this conversation by raising an additional strategy for confidence building. Because our results show that performance and confidence are more closely linked on an individual level in women, an educational strategy to mitigate the gender gap in confidence could be to focus on interventions that directly build skill. Because the projection of confidence influences others’ perception of an individual’s competence, we need to deliberately focus on cultivating skill and confidence in female residents. The perception of residents held by those in supervisory positions has implications for opportunities those trainees are offered in the future. This may be particularly true when those senior individuals have not had a chance to directly observe the trainees’s performance (eg, society leaders, fellowship directors, or chairpersons recruiting a new hire) because this is the situation in which the projection of confidence is most influential on perception of competence.8 Because improving resident ability is a modifiable way to influence self-confidence, this pilot study raises a new avenue for future research and educational interventions focusing on objective, concrete skill building as a component of closing the confidence gap and working toward gender equity.
LIMITATIONS
This study has several limitations, the primary one being its small sample size, especially of the female cohort. This was an inherent limitation imposed by the small proportion of female residents rotating through our institution in the 2-year period during which the study was conducted. Thus, findings may not be generalizable to all residents or plastic surgery training programs. It is also prudent to acknowledge the fact that this data set pertains to one specific operation, cleft lip repair, and set of measurement tools. It is possible that other results could be found if other types of simulation or real life clinical experiences are explored. However, the fact that the disparity in self-confidence found parallels results of other previous studies adds credibility to our data.
CONCLUSIONS
This study highlights the persistent gender gap in confidence among plastic surgery residents, despite similar objective performance between men and women. As confidence and skill were more closely related for women, we propose targeted skill-building interventions to help close the gender confidence gap. Future research is needed to determine the long-term impact of these interventions on the professional development and career trajectories of female plastic surgery residents, and investigate additional factors that may contribute to the sex gap in confidence.
DISCLOSURES
The simulator used in this article is proprietary technology developed by Boston Children’s Hospital Immersive Design Systems. Drs. Rogers-Vizena and Saldanha were involved in the development process; the other authors were not involved in the development process and no authors have current financial interest to declare. This work was supported by a National Endowment for Plastic Surgery grant from the Plastic Surgery Foundation.
Supplementary Material
Footnotes
Published online 7 December 2023.
Presented at the New England Society for Plastic and Reconstructive Surgeons Annual Meeting, June 10, 2023, Mystic, Connecticut; and at Plastic Surgery The Meeting 2023, October, 27, 2023, Austin, Texas.
Disclosure statements are at the end of this article, following the correspondence information.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Keane AM, Larson EL, Santosa KB, et al. Women in leadership and their influence on the gender diversity of academic plastic surgery programs. Plast Reconstr Surg. 2021;147:516–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Raborn LN, Gokun Y, Molina BJ, et al. Another day, another 82 cents: a national survey assessing gender-based wage differences in board-certified plastic surgeons. Plast Reconstr Surg Glob Open. 2023;11:e5196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luc JGY, Moon MR, Antonoff MB. Impact of sex on confidence and perception of training in cardiothoracic surgery. Am Surg. 2020;86:e119–e121. [PubMed] [Google Scholar]
- 4.Van Boerum MS, Jarman AF, Veith J, et al. The confidence gap: findings for women in plastic surgery. Am J Surg. 2020;220:1351–1357. [DOI] [PubMed] [Google Scholar]
- 5.Flyckt RL, White EE, Goodman LR, et al. The use of laparoscopy simulation to explore gender differences in resident surgical confidence. Obstet Gynecol Int. 2017;2017:1945801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cooney CM, Aravind P, Lifchez SD, et al. Differences in operative self-assessment between male and female plastic surgery residents: a survey of 8,149 cases. Am J Surg. 2021;221:799–803. [DOI] [PubMed] [Google Scholar]
- 7.Chamorro-Premuzic T. Why Do so Many Incompetent Men Become Leaders?: (and How to Fix It). Boston, Mass.: Harvard Business Review Press; 2019. [Google Scholar]
- 8.Schlenker B, Leary MR. Audiences’ reactions to self-enhancing, self-denigrating, and accurate self-presentations. J Experimental Soc Psychol. 1982;18:89–104. [Google Scholar]
- 9.Nasher J. To seem more competent, be more confident. 2019. Available at https://hbr.org/2019/03/to-seem-more-competent-be-more-confident.
- 10.Ronay RO J, Lehmann-Willenbrock N, Mayoral S, et al. Playing the trump card: Why we select overconfident leaders and why it matters. Leadersh Q. 2019;30:101316. [Google Scholar]
- 11.Rogers-Vizena CR, Saldanha FYL, Sideridis GD, et al. High-fidelity cleft simulation maintains improvements in performance and confidence: a prospective study. J Surg Educ. 2023. [online ahead of print September 9, 2023]. [DOI] [PubMed] [Google Scholar]
- 12.Geoffrion R, Lee T, Singer J. Validating a self-confidence scale for surgical trainees. J Obstet Gynaecol Can. 2013;35:355–361. [DOI] [PubMed] [Google Scholar]
- 13.Rogers-Vizena CR, Sideridis GD, Patel KG, et al. A competency assessment tool for unilateral cleft lip repair. Plast Reconstr Surg Glob Open. 2020;8:e2954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Colleges AoAM. Report on residents—number of active residents, by type of medical school, GME specialty, and sex. Available at https://www.aamc.org/data-reports/students-residents/interactive-data/report-residents/2022/table-b3-number-active-residents-type-medical-school-gme-specialty-and-gender. Published 2022. Accessed November 28, 2022.
- 15.Karamanos E, Julian BQ, Wampler M, et al. Gender bias in the integrated plastic surgery residency: a snapshot of current trends. Plast Reconstr Surg Glob Open. 2020;8:e2581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ross A; American Society of Plastic Surgery. Women underrepresented in plastic surgery. Available at https://www.plasticsurgery.org/news/press-releases/women-underrepresented-in-plastic-surgery. Accessed December 1, 2022.
- 17.Chen W, Baron M, Bourne DA, et al. A report on the representation of women in academic plastic surgery leadership. Plast Reconstr Surg. 2020;145:844–852. [DOI] [PubMed] [Google Scholar]
- 18.Yin C, McAuliffe PB, Liao CD, et al. Has the increase of women in surgical training programs led to a concomitant increase in female leadership positions? A 10-year analysis. Ann Plast Surg. 2023;90:376–379. [DOI] [PubMed] [Google Scholar]
- 19.Phillips NA, Tannan SC, Kalliainen LK. Understanding and overcoming implicit gender bias in plastic surgery. Plast Reconstr Surg. 2016;138:1111–1116. [DOI] [PubMed] [Google Scholar]
- 20.Blanch DC, Hall JA, Roter DL, et al. Medical student gender and issues of confidence. Patient Educ Couns. 2008;72:374–381. [DOI] [PubMed] [Google Scholar]
- 21.Moss-Racusin CA, Dovidio JF, Brescoll VL, et al. Science faculty’s subtle gender biases favor male students. Proc Natl Acad Sci U S A. 2012;109:16474–16479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eagly AH, Carli LL. The female leadership advantage: an evaluation of the evidence. Leadersh Q. 2003;14:807–834. [Google Scholar]
- 23.Liberatore MJ, Wagner WP. Gender, performance, and self-efficacy: a quasi-experimental field study. J Comput Inf Syst. 2022;62:109–117. [Google Scholar]
- 24.Lind DS, Rekkas S, Bui V, et al. Competency-based student self-assessment on a surgery rotation. J Surg Res. 2002;105:31–34. [DOI] [PubMed] [Google Scholar]
- 25.Feingold A. Gender differences in personality: a meta-analysis. Psychol Bull. 1994;116:429–456. [DOI] [PubMed] [Google Scholar]
- 26.Weisberg YJ, Deyoung CG, Hirsh JB. Gender differences in personality across the ten aspects of the big five. Front Psychol. 2011;2:178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ehrlinger J, Dunning D. How chronic self-views influence (and potentially mislead) estimates of performance. J Pers Soc Psychol. 2003;84:5–17. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.