Advances in microvascular surgical techniques have expanded the scope of free flap (FF) reconstruction. Tools predicting wound1 and overall2 outcomes now enhance operative planning, which can also be facilitated by 3D reconstructions. Perforator mapping and postanastomotic FF perfusion can be guided by Doppler ultrasound, thermographic, and hyperspectral imaging, with implantable probes also expediting postoperative FF compromise detection, allowing prompt operative/nonoperative flap salvage procedures,3 for example, venous supercharging.
Despite this, complication rates in head and neck reconstruction remain higher (7.7%) than in other regions, for example, breast (5.11%) and extremities (1.32%).4 Furthermore, complications in this region are potentially catastrophic, exposing major vessels and potentially precipitating anastomotic leaks or salivary fistulae.
Routine dual venous anastomosis (DVA)5 diminishes venous compromise and subsequent thrombosis, especially when anastomosing onto different venous systems, for example, the internal jugular and external jugular veins. However, DVA necessitates further dissection and longer operating time. Separately, indocyanine green fluorescence angiography (ICGFA) improves outcomes in autologous breast reconstruction. Here, we seek to demonstrate and quantify improved perfusion with DVA via metrics applied and validated in other surgical specialties.
Within a trial (ClinicalTrials.gov Identifier: NCT04220242), operative ICGFA was performed on an anterolateral thigh (ALT) flap deployed to reconstruct an 8 × 10 cm defect following total laryngectomy and bilateral selective neck dissection for invasive squamous cell carcinoma (T3N0) in a 66-year-old man. The ALT flap was raised using a subfascial technique through the intermuscular septum and a standard pedicle, including a single artery and two veins, was harvested. The lateral circumflex femoral artery was anastomosed (end-to-end, 9-0 nylon) to the facial artery and both venae comitantes to the external jugular and internal jugular tributaries, respectively, using 2.5-mm couplers (Synovis). ICGFA (0.1 mg/kg ICG) was performed and visually interpreted following single-vein anastomosis and repeated following DVA using EleVision IR (Medtronic, Ireland). The flap healed, and the patient was discharged without any flap complications. Using bespoke software (IBM Research Europe, Ireland), a fluorescence-time series from every pixel was captured from the 5-minute-long videos recorded 30 minutes apart, following each anastomosis.
From these curves, the maximum intensity (Fmax), rate of inflow (upslope), and rate of outflow (downslope) were determined, statistically interrogated, and computed into heat maps.
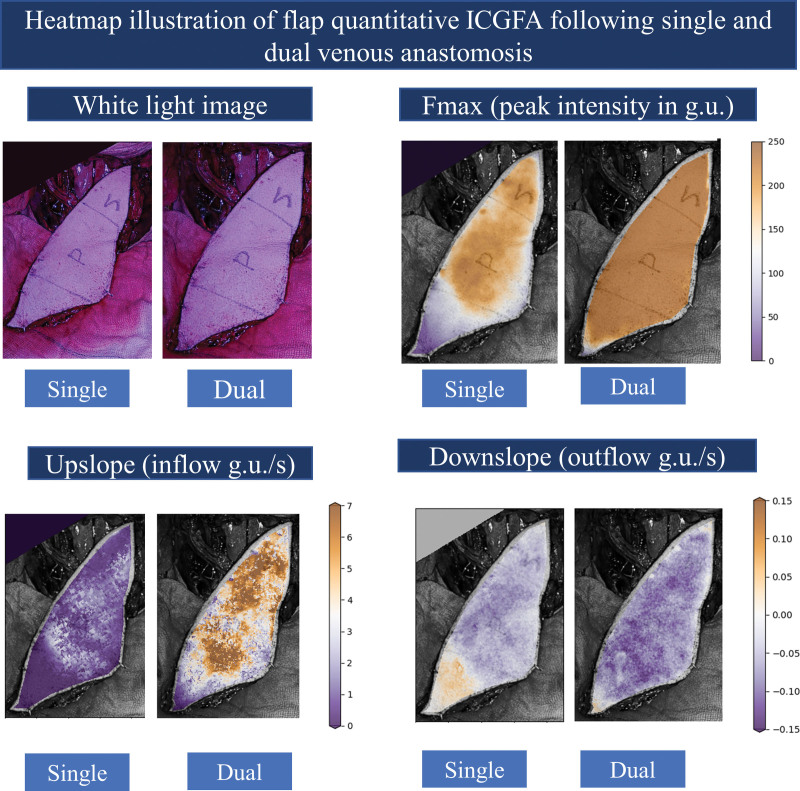
Visual ICGFA assessment showed brisker and broader distribution following DVA versus single-vein anastomosis (Fig. 1). [See Video (online), which displays fluorescence angiography following 0.1 mg/kg of ICG using the EleVision IR (Medtronic, Ireland) near-infrared open camera system following single venous anastomosis (left) and DVA (right) on an anterolateral thigh microvascular FF.]
Fig. 1.
Flap perfusion metrics calculated from the fluorescence video data (following single venous anastomosis and DVA) were illustrated as an augmented view over the camera displayed a white light image (top left) of the ALT flap. These metrics for every pixel of the flap were enumerated as a heat map with a color scale increasing upward from purple to yellow. Fmax (peak intensity, top right) in grayscale units (g.u.), inflow (upslope, bottom left), and outflow (downslope, more negative denotes faster outflow) gradients (g.u./s: second). The letters denote the target donor site of the flap tissue with P denoting the pharynx and S denoting the skin.
Video 1. displays fluorescence angiography following 0.1 mg/kg of ICG using the EleVision� IR, Medtronic, Ireland near-infrared open camera system following single (left) and dual (right) venous anastomosis on an anterolateral thigh microvascular free flap.
ICGFA metrics significantly favored improved perfusion following the DVA (Wilcoxon signed-rank P < 0.001, Table 1). The flap fluoresced brighter (Fmax 222.15 ± 15.57 versus 157.22 ± 51.42 g.u.: grayscale units) with steeper upslope (inflow 4.36 ± 1.98 versus 0.81 ± 0.72 g.u./s) and downslope (outflow −0.08 ± 0.03 versus −0.04 ± 0.03 g.u./s) gradients.
Table 1.
Data Analysis for Full Flap Quantitative ICGFA following Single-vein Anastomosis and DVA: Including the Number of Pixels (n) at Which the Fluorescence Intensity Change over Time Was Converted into a Time Series, Mean ± SD for the Maximum Fluorescence (Fmax in g.u.: Grayscale Units) Inflow (Upslope) and Outflow (Downslope) Gradients (g.u./s: Second)
| Full Flap (per Pixel) Quantitative ICGFA Data following Single and Dual Venous Anastomosis | |||
|---|---|---|---|
| Single Anastomosis, Mean ± SD | Dual Anastomosis, Mean ± SD | P | |
| Time fluorescence curves sampled per flap (n) | 80,395 | 106,758 | |
| Fmax (g.u.) | 157.22 ± 51.42 | 222.15 ± 15.57 | <0.001* |
| Upslope (inflow) gradient (g.u./s) | 0.81 ± 0.72 | 4.36 ± 1.98 | <0.001* |
| Downslope (outflow) gradient (g.u./s) | −0.04 ± 0.03 | −0.08 ± 0.03 | <0.001* |
P values denote statistical significance for Wilcoxon signed-rank test (following Shapiro-Wilk test for normality, SPSS version 27; IBM).
P < 0.05
These proposed methodologies might quantitatively support decision-making, removing interpretation variability. Furthermore, the selected camera compensates for interassessment distance-related fluorescence variations. Despite a brief interassessment period, flap flow is known to improve with time, even before choke vessel opening. Confounding variables require assessment using control cases in an investigative case series.
This case report augments evidence supporting routine DVA in head and neck surgery when technically possible by objectively demonstrating improved perfusion via full flap computational ICGFA assessment.
DISCLOSURES
Dr. Cahill is named on a patent filed in relation to processes for visual determination of tissue biology, receives speaker fees from Stryker Corp, Ethicon/J&J, and Olympus, research funding from Intuitive Corp, consultancy fees from Arthrex, Diagnostic Green, Distalmotion, and Medtronic (Touch Surgery), and holds research funding from the Irish Government (DTIF) in collaboration with IBM Research Europe in Ireland, from EU Horizon 2020 in collaboration with Palliare and Steripak, from Horizon Europe in collaboration with Arctur, and from Intuitive and Medtonic for specific research and development awards. Jeffrey Dalli was employed as a researcher in the DTIF and is a recipient of the TESS scholarship (MALTA). Dr. Epperlein is a full-time employee of IBM Research Europe, a division of IBM, which provides technical products and services worldwide to government, healthcare, and life-sciences companies. The other authors have no financial interest to declare.
ACKNOWLEDGMENT
This research includes a consenting adult patient and was approved by the Mater Misericordiae University Hospital (Dublin, Ireland) institutional review board (Reference 1/378/2092, ClinicalTrials.gov Identifier: NCT04220242).
Footnotes
Published online 7 December 2023.
Disclosure statements are at the end of this article, following the correspondence information.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Guarro G, Cozzani F, Rossini M, et al. The modified TIME-H scoring system, a versatile tool in wound management practice: a preliminary report. Acta Biomed. 2021;92:e2021226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Winter E, Glauser G, Caplan IF, et al. The LACE+ index as a predictor of 30-day patient outcomes in a plastic surgery population: a coarsened exact match study. Plast Reconstr Surg. 2020;146:296e–305e. [DOI] [PubMed] [Google Scholar]
- 3.Boissiere F, Gandolfi S, Riot S, et al. Flap venous congestion and salvage techniques: a systematic literature review. Plast Reconstr Surg Global Open. 2021;9:e3327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kwok AC, Agarwal JP. An analysis of free flap failure using the ACS NSQIP database does flap site and flap type matter? Microsurgery. 2017;37:531–538. [DOI] [PubMed] [Google Scholar]
- 5.Christianto S, Li KY, Lau A, et al. Single versus double venous anastomoses in head and neck reconstruction: systematic review and cumulative meta analysis. Int J Oral Maxillofac Surg. 2017;46:119. [DOI] [PubMed] [Google Scholar]