Abstract
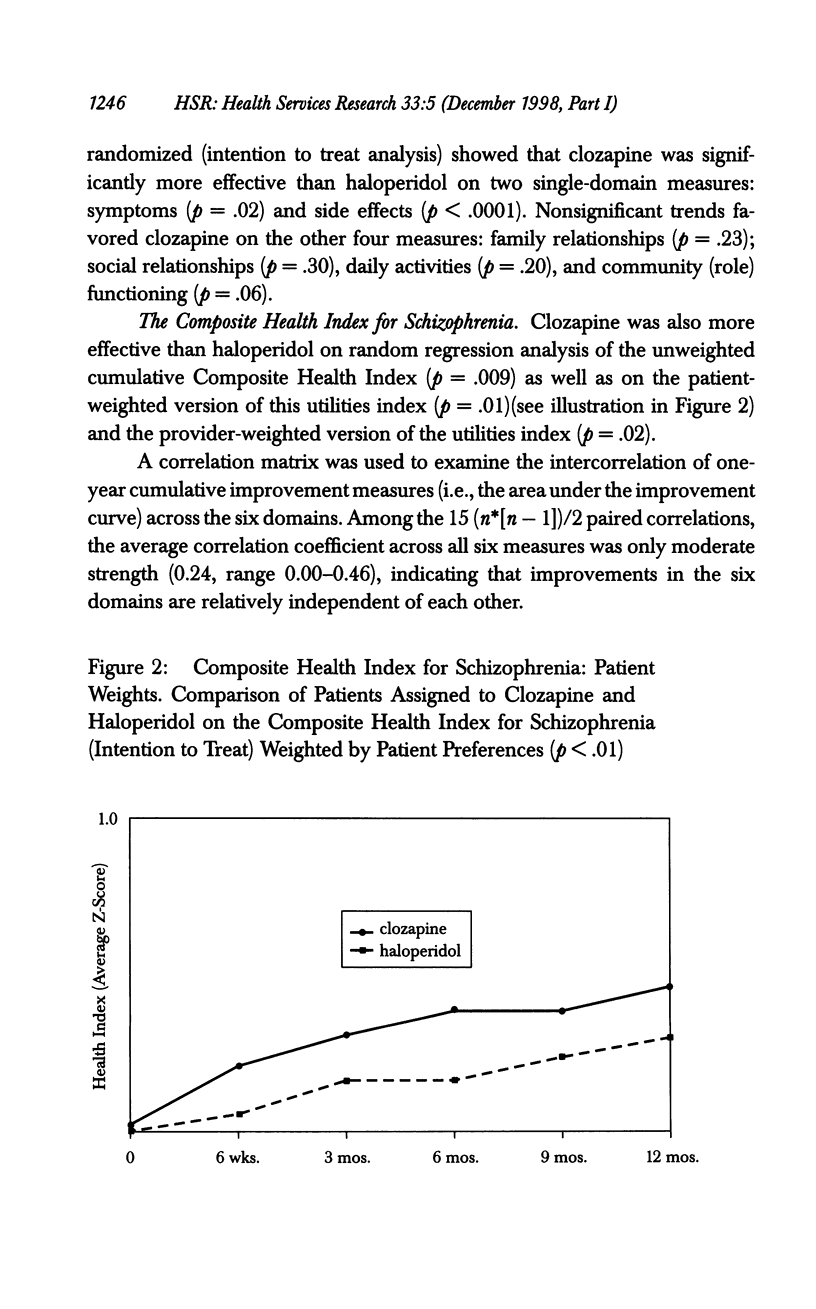
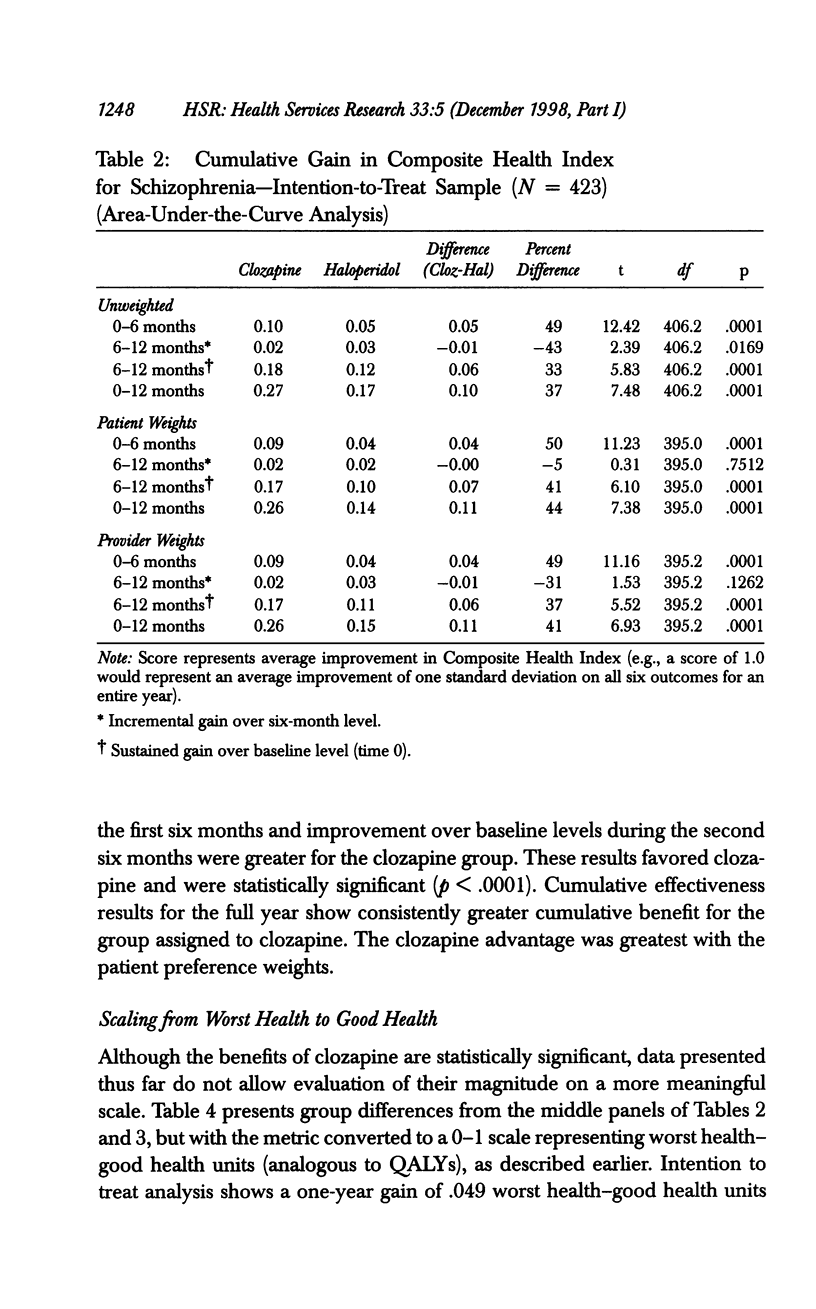
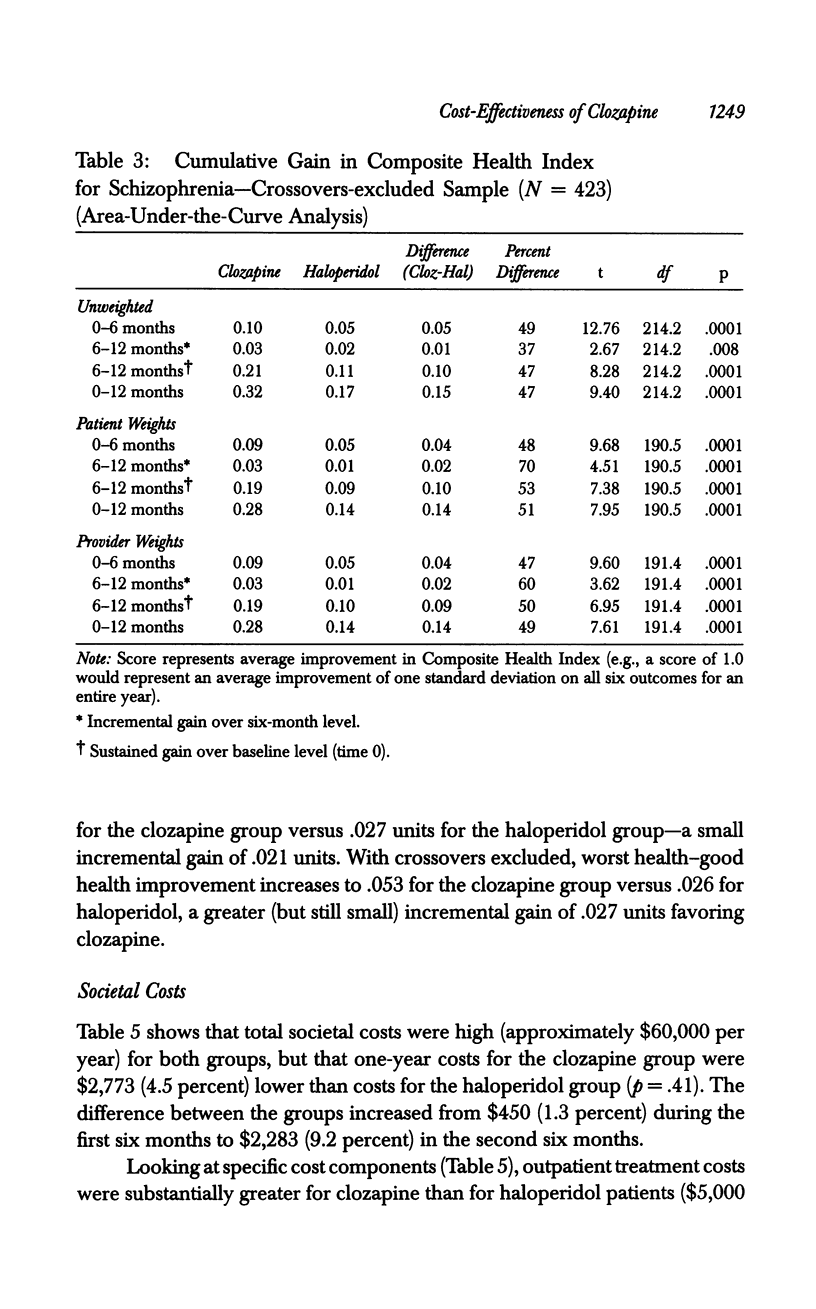
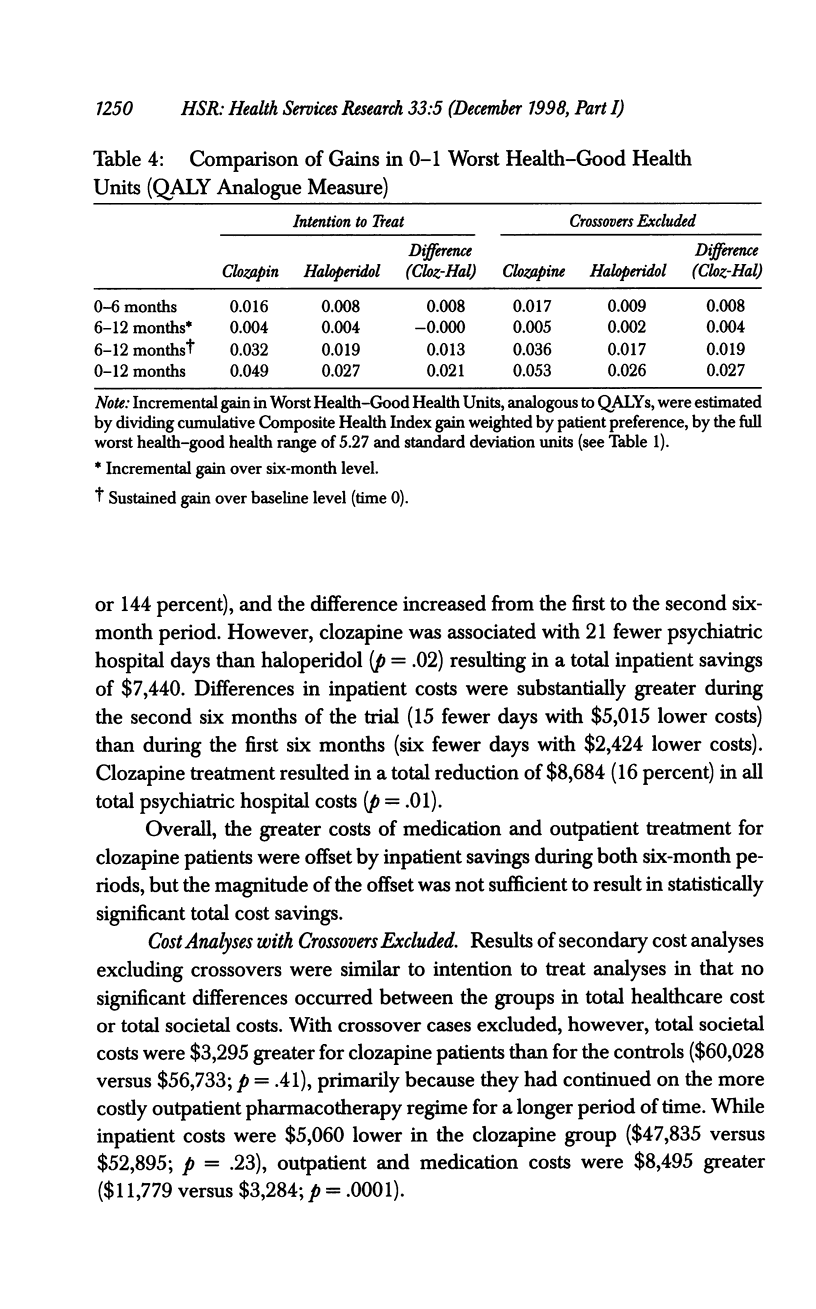
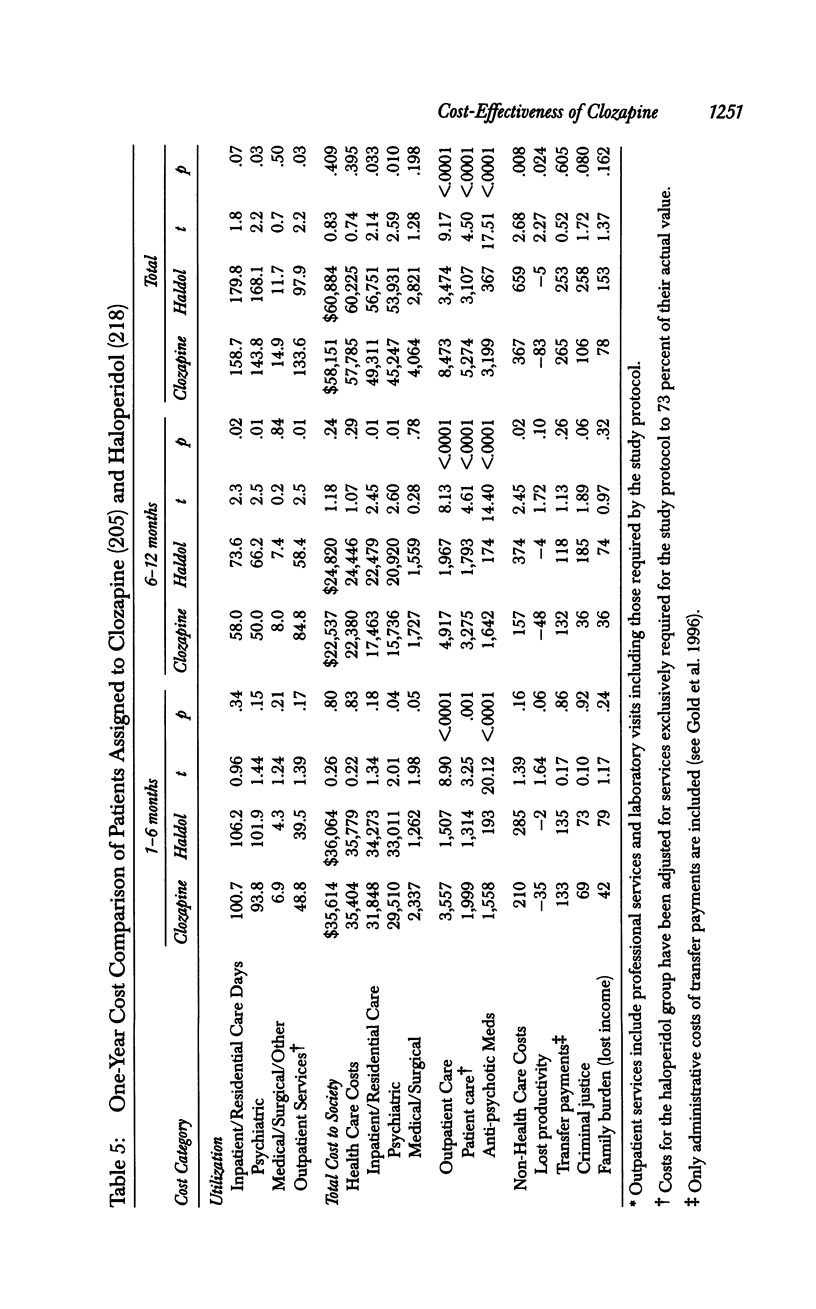
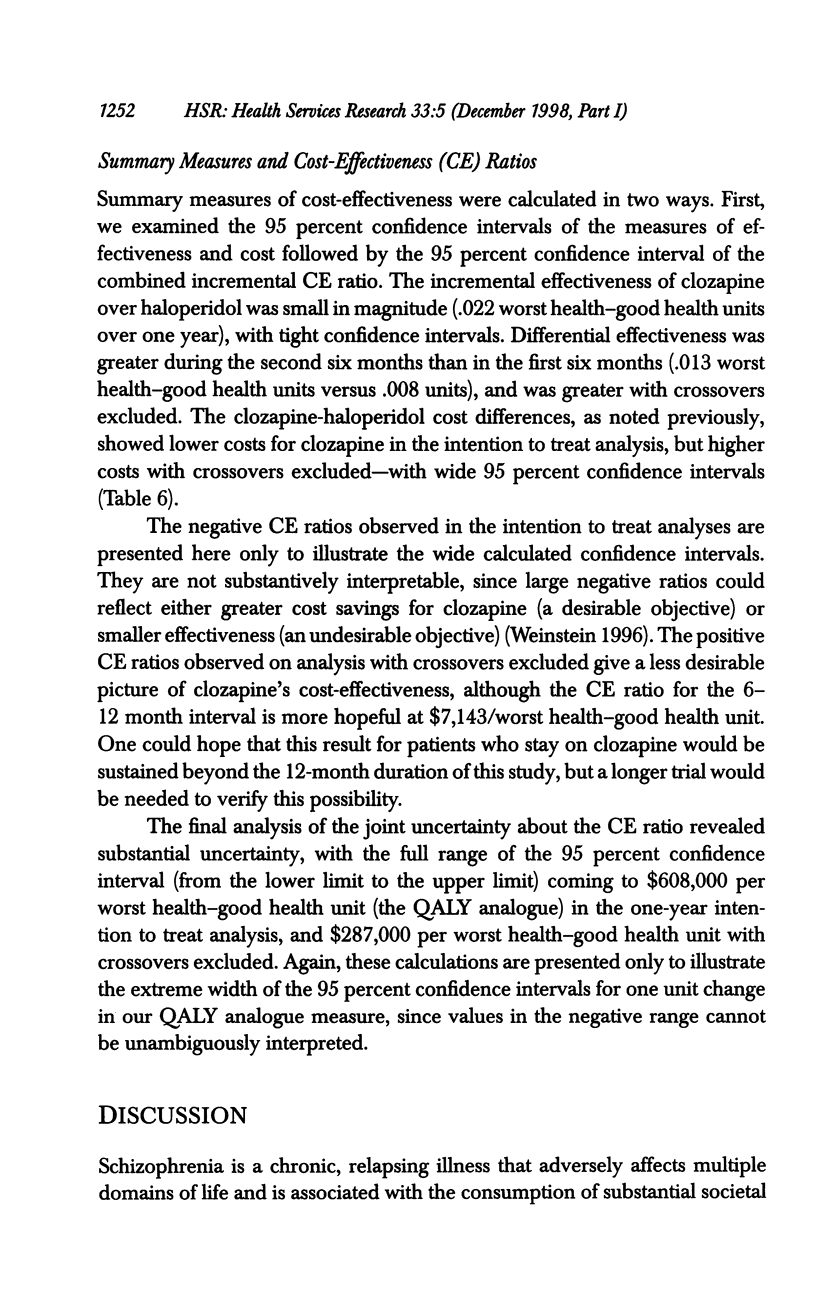
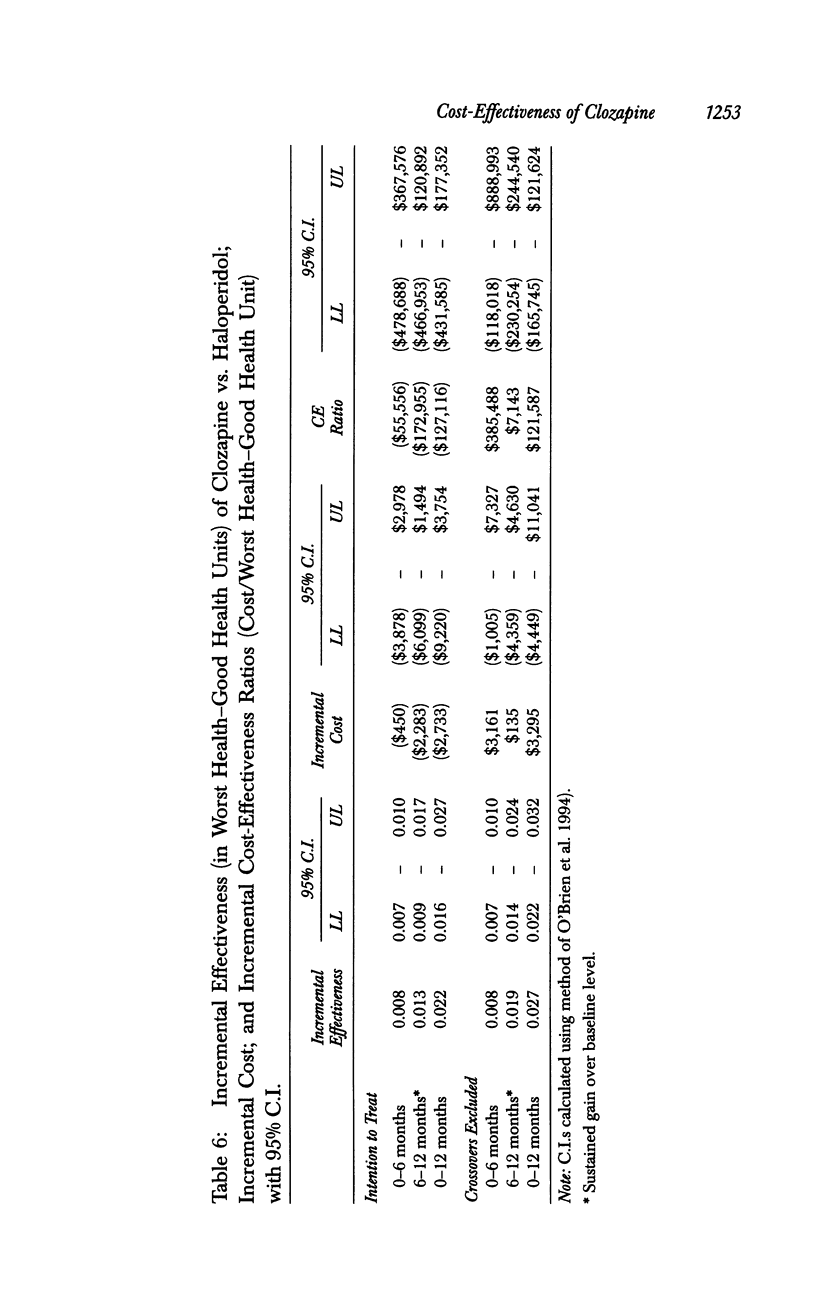
OBJECTIVE: To develop new methods for combining results from multiple outcome domains and to demonstrate their application in a study of the cost-effectiveness of clozapine in treating hospitalized patients with refractory schizophrenia. DATA SOURCES/STUDY SETTING: Interview assessments, and administrative utilization and cost data, concerning 423 patients with refractory schizophrenia who had been hospitalized for 30-364 days during the year before study entry, at 15 VA medical centers. STUDY DESIGN: A 12-month double-blind trial compared clozapine (n = 205) and haloperidol (n = 218) in the treatment of refractory schizophrenia. DATA COLLECTION/EXTRACTION METHODS: Data from standard assessment instruments, gathered at baseline and at 6 weeks, and at 3, 6, 9, and 12 months, were used to develop a Composite Health Index for Schizophrenia, a measure that addresses outcome in six domains, weighted by patient or provider preferences. Cumulative improvement was estimated by computing the area under the improvement curve. This measure was then combined with cost data, reflecting consumption of societal resources to estimate incremental cost-effectiveness ratios. PRINCIPAL FINDINGS: Clozapine was significantly more effective than haloperidol on measures of symptoms (p = .02) and side effects (p < .0001), with nonsignificant trends in the positive direction on community role functioning (p = .06), family relationships (p = .23), social relationships (p = .30), and daily activities (p = .20). Clozapine was also more effective than haloperidol on the one-year cumulative Composite Health Index for Schizophrenia (p < .0001 for all weighting schemes). After converting this measure to a 0-1 Worst Health-Good Health Scale analogous to Quality Adjusted Life Years, clozapine was found to yield a small improvement of .049 Worst Health-Good Health Units as compared to an improvement of only .027 Units for haloperidol (p < .0001). Average annual costs were $2,733 lower for clozapine (95% C.I. = -$9,220 to $3,754). Although clozapine was significantly more effective than haloperidol, the summary cost-effectiveness ratio had a wide 95 percent confidence interval ranging from -$431,585 to $177,352. CONCLUSIONS: Methods demonstrate an approach to using conventional disease-specific measures to evaluate the cumulative effectiveness of novel treatments for psychotic disorders and for expressing their economic effect as cost-effectiveness ratios. Among high hospital users with refractory schizophrenia, clozapine is more cost-effective than standard treatment, although the magnitude of its effect is small and there is considerable uncertainty about the cost estimates.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alvir J. M., Lieberman J. A., Safferman A. Z., Schwimmer J. L., Schaaf J. A. Clozapine-induced agranulocytosis. Incidence and risk factors in the United States. N Engl J Med. 1993 Jul 15;329(3):162–167. doi: 10.1056/NEJM199307153290303. [DOI] [PubMed] [Google Scholar]
- Carpenter W. T., Jr, Conley R. R., Buchanan R. W., Breier A., Tamminga C. A. Patient response and resource management: another view of clozapine treatment of schizophrenia. Am J Psychiatry. 1995 Jun;152(6):827–832. doi: 10.1176/ajp.152.6.827. [DOI] [PubMed] [Google Scholar]
- Essock S. M., Hargreaves W. A., Covell N. H., Goethe J. Clozapine's effectiveness for patients in state hospitals: results from a randomized trial. Psychopharmacol Bull. 1996;32(4):683–697. [PubMed] [Google Scholar]
- Gibbons R. D., Hedeker D., Elkin I., Waternaux C., Kraemer H. C., Greenhouse J. B., Shea M. T., Imber S. D., Sotsky S. M., Watkins J. T. Some conceptual and statistical issues in analysis of longitudinal psychiatric data. Application to the NIMH treatment of Depression Collaborative Research Program dataset. Arch Gen Psychiatry. 1993 Sep;50(9):739–750. doi: 10.1001/archpsyc.1993.01820210073009. [DOI] [PubMed] [Google Scholar]
- Heinrichs D. W., Hanlon T. E., Carpenter W. T., Jr The Quality of Life Scale: an instrument for rating the schizophrenic deficit syndrome. Schizophr Bull. 1984;10(3):388–398. doi: 10.1093/schbul/10.3.388. [DOI] [PubMed] [Google Scholar]
- Kane J. M., Marder S. R. Psychopharmacologic treatment of schizophrenia. Schizophr Bull. 1993;19(2):287–302. doi: 10.1093/schbul/19.2.287. [DOI] [PubMed] [Google Scholar]
- Kane J., Honigfeld G., Singer J., Meltzer H. Clozapine for the treatment-resistant schizophrenic. A double-blind comparison with chlorpromazine. Arch Gen Psychiatry. 1988 Sep;45(9):789–796. doi: 10.1001/archpsyc.1988.01800330013001. [DOI] [PubMed] [Google Scholar]
- Kay S. R., Fiszbein A., Opler L. A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- Meltzer H. Y., Cola P., Way L., Thompson P. A., Bastani B., Davies M. A., Snitz B. Cost effectiveness of clozapine in neuroleptic-resistant schizophrenia. Am J Psychiatry. 1993 Nov;150(11):1630–1638. doi: 10.1176/ajp.150.11.1630. [DOI] [PubMed] [Google Scholar]
- Meltzer H. Y. Treatment of the neuroleptic-nonresponsive schizophrenic patient. Schizophr Bull. 1992;18(3):515–542. doi: 10.1093/schbul/18.3.515. [DOI] [PubMed] [Google Scholar]
- O'Brien B. J., Drummond M. F., Labelle R. J., Willan A. In search of power and significance: issues in the design and analysis of stochastic cost-effectiveness studies in health care. Med Care. 1994 Feb;32(2):150–163. doi: 10.1097/00005650-199402000-00006. [DOI] [PubMed] [Google Scholar]
- Reid W. H., Mason M., Toprac M. Savings in hospital bed-days related to treatment with clozapine. Hosp Community Psychiatry. 1994 Mar;45(3):261–264. doi: 10.1176/ps.45.3.261. [DOI] [PubMed] [Google Scholar]
- Revicki D. A., Shakespeare A., Kind P. Preferences for schizophrenia-related health states: a comparison of patients, caregivers and psychiatrists. Int Clin Psychopharmacol. 1996 Jun;11(2):101–108. [PubMed] [Google Scholar]
- Rosenheck R., Cramer J., Xu W., Thomas J., Henderson W., Frisman L., Fye C., Charney D. A comparison of clozapine and haloperidol in hospitalized patients with refractory schizophrenia. Department of Veterans Affairs Cooperative Study Group on Clozapine in Refractory Schizophrenia. N Engl J Med. 1997 Sep 18;337(12):809–815. doi: 10.1056/NEJM199709183371202. [DOI] [PubMed] [Google Scholar]
- Rupp A., Keith S. J. The costs of schizophrenia. Assessing the burden. Psychiatr Clin North Am. 1993 Jun;16(2):413–423. [PubMed] [Google Scholar]
- Simpson G. M., Angus J. W. A rating scale for extrapyramidal side effects. Acta Psychiatr Scand Suppl. 1970;212:11–19. doi: 10.1111/j.1600-0447.1970.tb02066.x. [DOI] [PubMed] [Google Scholar]


