Abstract
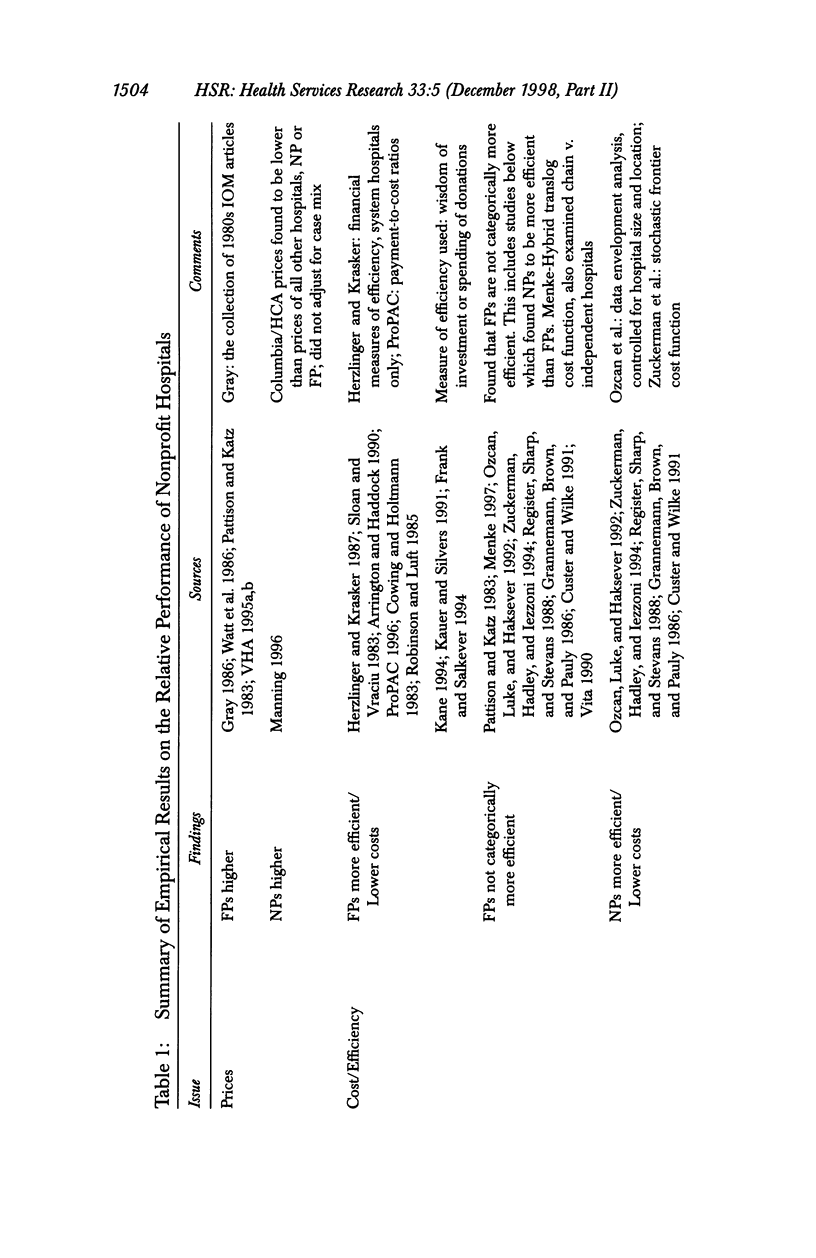
OBJECTIVE: To describe the contributions of nonprofit hospitals and health plans to healthcare markets and to analyze state policy options with regard to the conversion of nonprofits to for-profit status. DATA SOURCES/STUDY SETTING: Secondary national and state data from a variety of sources, 1980-present. STUDY DESIGN: Policy analysis. DATA COLLECTION/EXTRACTION METHODS: Development of a conceptual economic framework; analysis of empirical, legal, and theoretical literature; and review of statutes, rules, and court decisions. PRINCIPAL FINDINGS: Three main rationales support special status for nonprofits, especially hospitals: charity care, other community benefits, and consumer protection. The main social rationale for for-profits is their incentives for better efficiency. There are reasons to expect that nonprofit and for-profit goals differ; however, measured differences in community hospital cost, prices, and quality between nonprofit and for-profit hospitals are undetectable or inconclusive. Nonprofit hospitals do provide more uncompensated care than for-profit hospitals. Similarities between nonprofit and for-profit hospitals may exist because nonprofits may set norms that for-profits follow to some degree. States have substantial power and discretion in overseeing nonprofit conversions. Some have regularized oversight through new legislation that constrains, but does not eliminate, state officials' discretion. These statutes may be deferential to converting entities and their buyers or may be very restrictive of them. CONCLUSIONS: Overseeing the appropriate disposition of nonprofit assets in individual conversions is extremely important. States should also monitor local market conditions through community benefits assessments and other data collection, however, to accurately assess (and possibly redress) what is lost or gained from conversion. Local market conditions are likely more important in determining hospital behavior than ownership form. Potentially, a mix of for-profit and nonprofit hospitals in a given market may improve market performance due to constraints the two ownership types may exercise over one another. If nonprofits disappear, the states may need to maintain quality and access norms through regulation.
Full text
PDF




































Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arrington B., Haddock C. C. Who really profits from not-for-profits? Health Serv Res. 1990 Jun;25(2):291–304. [PMC free article] [PubMed] [Google Scholar]
- Bauerschmidt A. D., Jacobs P. Pricing objectives in nonprofit hospitals. Health Serv Res. 1985 Jun;20(2):153–162. [PMC free article] [PubMed] [Google Scholar]
- Becker E. R., Sloan F. A. Hospital ownership and performance. Econ Inq. 1985 Jan;23(1):21–36. doi: 10.1111/j.1465-7295.1985.tb01750.x. [DOI] [PubMed] [Google Scholar]
- Bovbjerg R. R., Griffin C. C., Carroll C. E. U.S. health care coverage and costs: historical development and choices for the 1990s. J Law Med Ethics. 1993 Summer;21(2):141–162. doi: 10.1111/j.1748-720x.1993.tb01239.x. [DOI] [PubMed] [Google Scholar]
- Claxton G., Feder J., Shactman D., Altman S. Public policy issues in nonprofit conversions: an overview. Health Aff (Millwood) 1997 Mar-Apr;16(2):9–28. doi: 10.1377/hlthaff.16.2.9. [DOI] [PubMed] [Google Scholar]
- Clement J. P., Smith D. G., Wheeler J. R. What do we want and what do we get from not-for-profit hospitals? Hosp Health Serv Adm. 1994 Summer;39(2):159–178. [PubMed] [Google Scholar]
- Fox D. M., Isenberg P. Anticipating the magic moment: the public interest in health plan conversions in California. Health Aff (Millwood) 1996 Spring;15(1):202–209. doi: 10.1377/hlthaff.15.1.202. [DOI] [PubMed] [Google Scholar]
- Grannemann T. W., Brown R. S., Pauly M. V. Estimating hospital costs. A multiple-output analysis. J Health Econ. 1986 Jun;5(2):107–127. doi: 10.1016/0167-6296(86)90001-9. [DOI] [PubMed] [Google Scholar]
- Hartz A. J., Krakauer H., Kuhn E. M., Young M., Jacobsen S. J., Gay G., Muenz L., Katzoff M., Bailey R. C., Rimm A. A. Hospital characteristics and mortality rates. N Engl J Med. 1989 Dec 21;321(25):1720–1725. doi: 10.1056/NEJM198912213212506. [DOI] [PubMed] [Google Scholar]
- Herzlinger R. E., Krasker W. S. Who profits from nonprofits? Harv Bus Rev. 1987 Jan-Feb;65(1):93–106. [PubMed] [Google Scholar]
- Kertesz L. Not your father's Blue Cross/Blue Shield. Mod Healthc. 1996 Oct 14;26(42):62-4, 66, 68-70. [PubMed] [Google Scholar]
- Kopit W. G., McCann R. W. Toward a definitive antitrust standard for nonprofit hospital mergers. J Health Polit Policy Law. 1988 Winter;13(4):635–662. doi: 10.1215/03616878-13-4-635. [DOI] [PubMed] [Google Scholar]
- Kuttner R. Columbia/HCA and the resurgence of the for-profit hospital business. (1) N Engl J Med. 1996 Aug 1;335(5):362–367. doi: 10.1056/NEJM199608013350524. [DOI] [PubMed] [Google Scholar]
- LeBlanc A. J., Hurley R. E. Adoption of HIV-related services among urban US hospitals: 1988 and 1991. Med Care. 1995 Sep;33(9):881–891. doi: 10.1097/00005650-199509000-00001. [DOI] [PubMed] [Google Scholar]
- Lewin L. S., Eckels T. J., Miller L. B. Setting the record straight. The provision of uncompensated care by not-for-profit hospitals. N Engl J Med. 1988 May 5;318(18):1212–1215. doi: 10.1056/NEJM198805053181829. [DOI] [PubMed] [Google Scholar]
- Mann J., Melnick G., Bamezai A., Zwanziger J. Uncompensated care: hospitals' responses to fiscal pressures. Health Aff (Millwood) 1995 Spring;14(1):263–270. doi: 10.1377/hlthaff.14.1.263. [DOI] [PubMed] [Google Scholar]
- McCue M. J., Clement J. P., Hoerger T. J. The association of ownership and system affiliation with the financial performance of inpatient psychiatric hospitals. Inquiry. 1993 Fall;30(3):306–317. [PubMed] [Google Scholar]
- Melnick G. A., Zwanziger J., Bamezai A., Pattison R. The effects of market structure and bargaining position on hospital prices. J Health Econ. 1992 Oct;11(3):217–233. doi: 10.1016/0167-6296(92)90001-h. [DOI] [PubMed] [Google Scholar]
- Menke T. J. The effect of chain membership on hospital costs. Health Serv Res. 1997 Jun;32(2):177–196. [PMC free article] [PubMed] [Google Scholar]
- Morey R. C., Fine D. J., Loree S. W., Retzlaff-Roberts D. L., Tsubakitani S. The trade-off between hospital cost and quality of care. An exploratory empirical analysis. Med Care. 1992 Aug;30(8):677–698. doi: 10.1097/00005650-199208000-00002. [DOI] [PubMed] [Google Scholar]
- Morrisey M. A., Wedig G. J., Hassan M. Do nonprofit hospitals pay their way? Health Aff (Millwood) 1996 Winter;15(4):132–144. doi: 10.1377/hlthaff.15.4.132. [DOI] [PubMed] [Google Scholar]
- Needleman J., Chollet D. J., Lamphere J. Hospital conversion trends. Health Aff (Millwood) 1997 Mar-Apr;16(2):187–195. doi: 10.1377/hlthaff.16.2.187. [DOI] [PubMed] [Google Scholar]
- Norton E. C., Staiger D. O. How hospital ownership affects access to care for the uninsured. Rand J Econ. 1994 Spring;25(1):171–185. [PubMed] [Google Scholar]
- Ozcan Y. A., Luke R. D., Haksever C. Ownership and organizational performance. A comparison of technical efficiency across hospital types. Med Care. 1992 Sep;30(9):781–794. [PubMed] [Google Scholar]
- Pattison R. V., Katz H. M. Investor-owned and not-for-profit hospitals. A comparison based on California data. N Engl J Med. 1983 Aug 11;309(6):347–353. doi: 10.1056/NEJM198308113090606. [DOI] [PubMed] [Google Scholar]
- Potter M. A., Longest B. B., Jr The divergence of federal and state policies on the charitable tax exemption of nonprofit hospitals. J Health Polit Policy Law. 1994 Summer;19(2):393–422. doi: 10.1215/03616878-19-2-393. [DOI] [PubMed] [Google Scholar]
- Relman A. S. Are voluntary hospitals caring for the poor? N Engl J Med. 1988 May 5;318(18):1198–1200. doi: 10.1056/NEJM198805053181811. [DOI] [PubMed] [Google Scholar]
- Robinson J. C., Luft H. S. The impact of hospital market structure on patient volume, average length of stay, and the cost of care. J Health Econ. 1985 Dec;4(4):333–356. doi: 10.1016/0167-6296(85)90012-8. [DOI] [PubMed] [Google Scholar]
- Sanders S. M. The "common sense" of the nonprofit hospital tax exemption: a policy analysis. J Policy Anal Manage. 1995 Summer;14(3):446–466. [PubMed] [Google Scholar]
- Schlesinger M., Marmor T. R., Smithey R. Nonprofit and for-profit medical care: shifting roles and implications for health policy. J Health Polit Policy Law. 1987 Fall;12(3):427–457. doi: 10.1215/03616878-12-3-427. [DOI] [PubMed] [Google Scholar]
- Shook T. L., Sun G. W., Burstein S., Eisenhauer A. C., Matthews R. V. Comparison of percutaneous transluminal coronary angioplasty outcome and hospital costs for low-volume and high-volume operators. Am J Cardiol. 1996 Feb 15;77(5):331–336. doi: 10.1016/s0002-9149(97)89359-9. [DOI] [PubMed] [Google Scholar]
- Shriber D. State experience in regulating a changing health care system. Health Aff (Millwood) 1997 Mar-Apr;16(2):48–68. doi: 10.1377/hlthaff.16.2.48. [DOI] [PubMed] [Google Scholar]
- Vita M. G. Exploring hospital production relationships with flexible functional forms. J Health Econ. 1990 Jun;9(1):1–21. doi: 10.1016/0167-6296(90)90038-5. [DOI] [PubMed] [Google Scholar]
- Watt J. M., Derzon R. A., Renn S. C., Schramm C. J., Hahn J. S., Pillari G. D. The comparative economic performance of investor-owned chain and not-for-profit hospitals. N Engl J Med. 1986 Jan 9;314(2):89–96. doi: 10.1056/NEJM198601093140206. [DOI] [PubMed] [Google Scholar]
- Weissman J. Uncompensated hospital care. Will it be there if we need it? JAMA. 1996 Sep 11;276(10):823–828. doi: 10.1001/jama.276.10.823. [DOI] [PubMed] [Google Scholar]
- Wolfson J., Hopes S. L. What makes tax-exempt hospitals special? Healthc Financ Manage. 1994 Jul;48(7):56–60. [PubMed] [Google Scholar]
- Young G. J., Desai K. R., Van Deusen Lukas C. Does the sale of nonprofit hospitals threaten health care for the poor? Health Aff (Millwood) 1997 Jan-Feb;16(1):137–141. doi: 10.1377/hlthaff.16.1.137. [DOI] [PubMed] [Google Scholar]
- Zuckerman S., Hadley J., Iezzoni L. Measuring hospital efficiency with frontier cost functions. J Health Econ. 1994 Oct;13(3):255–340. doi: 10.1016/0167-6296(94)90027-2. [DOI] [PubMed] [Google Scholar]