Abstract
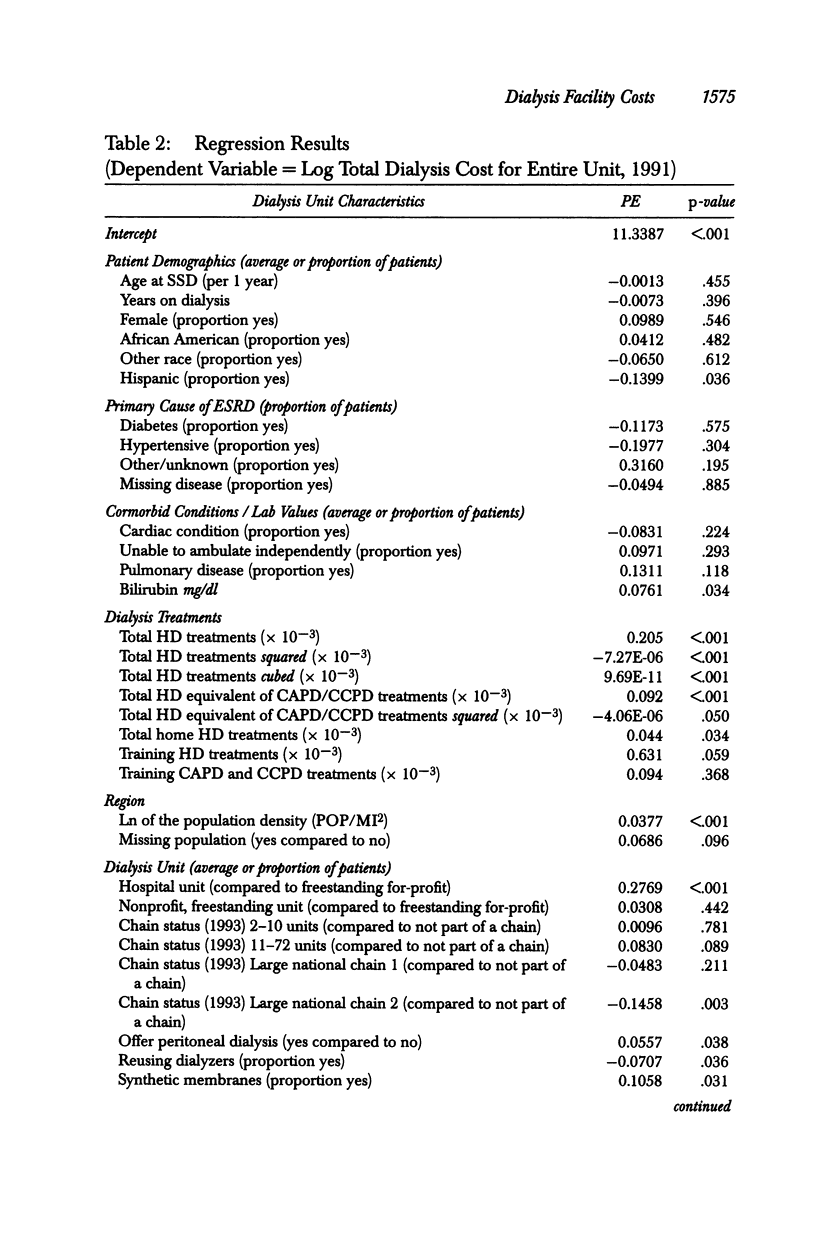
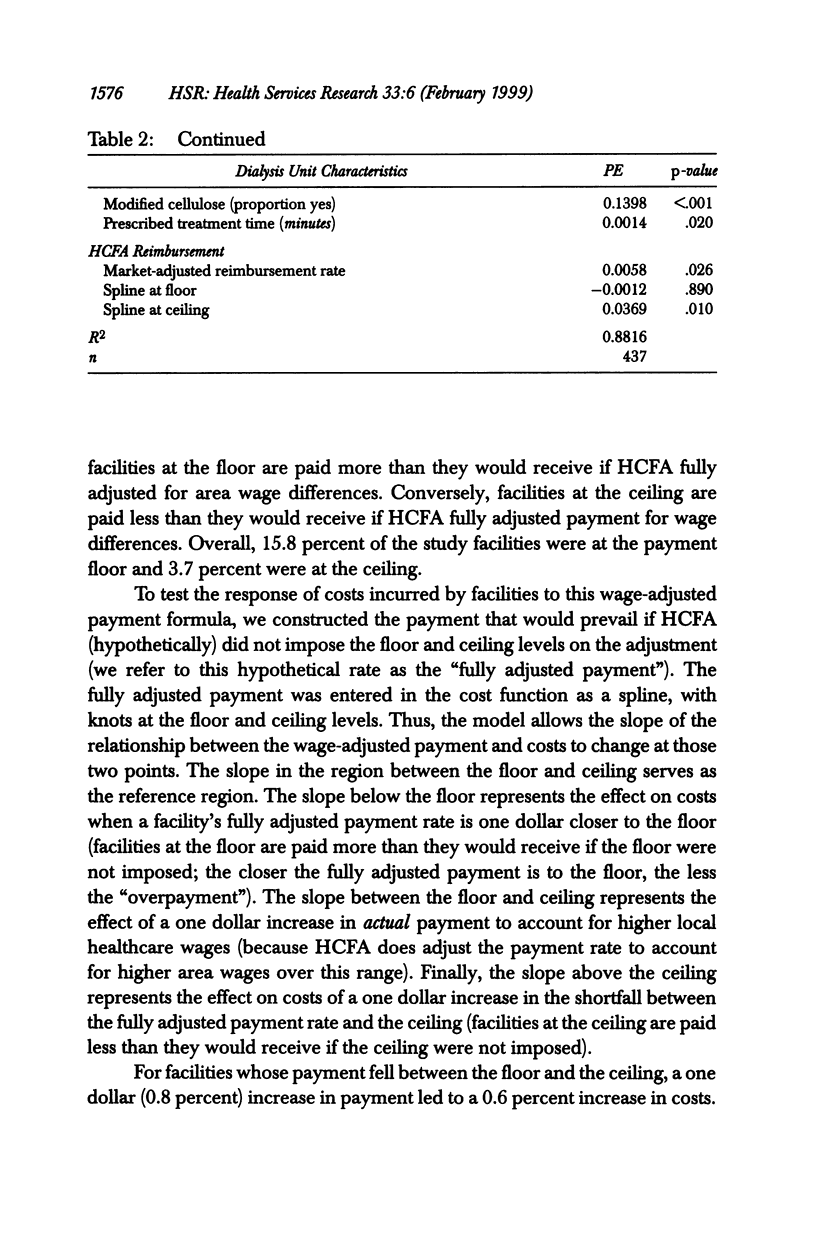
OBJECTIVE: To evaluate the effects of case mix, practice patterns, features of the payment system, and facility characteristics on the cost of dialysis. DATA SOURCES/STUDY SETTING: The nationally representative sample of dialysis units in the 1991 U.S. Renal Data System's Case Mix Adequacy (CMA) Study. The CMA data were merged with data from Medicare Cost Reports, HCFA facility surveys, and HCFA's end-stage renal disease patient registry. STUDY DESIGN: We estimated a statistical cost function to examine the determinants of costs at the dialysis unit level. PRINCIPAL FINDINGS: The relationship between case mix and costs was generally weak. However, dialysis practices (type of dialysis membrane, membrane reuse policy, and treatment duration) did have a significant effect on costs. Further, facilities whose payment was constrained by HCFA's ceiling on the adjustment for area wage rates incurred higher costs than unconstrained facilities. The costs of hospital-based units were considerably higher than those of freestanding units. Among chain units, only members of one of the largest national chains exhibited significant cost savings relative to independent facilities. CONCLUSIONS: Little evidence showed that adjusting dialysis payment to account for differences in case mix across facilities would be necessary to ensure access to care for high-cost patients or to reimburse facilities equitably for their costs. However, current efforts to increase dose of dialysis may require higher payments. Longer treatments appear to be the most economical method of increasing the dose of dialysis. Switching to more expensive types of dialysis membranes was a more costly means of increasing dose and hence must be justified by benefits beyond those of higher dose. Reusing membranes saved money, but the savings were insufficient to offset the costs associated with using more expensive membranes. Most, but not all, of the higher costs observed in hospital-based units appear to reflect overhead cost allocation rather than a difference in real resources devoted to treatment. The economies experienced by the largest chains may provide an explanation for their recent growth in market share. The heterogeneity of results by chain size implies that characterizing units using a simple chain status indicator variable is inadequate. Cost differences by facility type and the effects of the ongoing growth of large chains are worthy of continued monitoring to inform both payment policy and antitrust enforcement.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Dor A., Farley D. E. Payment source and the cost of hospital care: evidence from a multiproduct cost function with multiple payers. J Health Econ. 1996 Feb;15(1):1–21. doi: 10.1016/0167-6296(95)00029-1. [DOI] [PubMed] [Google Scholar]
- Dor A., Held P. J., Pauly M. V. The Medicare cost of renal dialysis. Evidence from a statistical cost function. Med Care. 1992 Oct;30(10):879–891. doi: 10.1097/00005650-199210000-00001. [DOI] [PubMed] [Google Scholar]
- Farley D. O. Competition under fixed prices: effects on patient selection and service strategies by hemodialysis providers. Med Care Res Rev. 1996 Sep;53(3):330–349. doi: 10.1177/107755879605300307. [DOI] [PubMed] [Google Scholar]
- Feldman H. I., Kinosian M., Bilker W. B., Simmons C., Holmes J. H., Pauly M. V., Escarce J. J. Effect of dialyzer reuse on survival of patients treated with hemodialysis. JAMA. 1996 Aug 28;276(8):620–625. [PubMed] [Google Scholar]
- Frank R. G., McGuire T. G., Newhouse J. P. Risk contracts in managed mental health care. Health Aff (Millwood) 1995 Fall;14(3):50–64. doi: 10.1377/hlthaff.14.3.50. [DOI] [PubMed] [Google Scholar]
- Fries B. E., Schneider D. P., Foley W. J., Gavazzi M., Burke R., Cornelius E. Refining a case-mix measure for nursing homes: Resource Utilization Groups (RUG-III). Med Care. 1994 Jul;32(7):668–685. doi: 10.1097/00005650-199407000-00002. [DOI] [PubMed] [Google Scholar]
- Gardner J. Dialysis outcomes in works. HCFA may set quality, practice guidelines for ESRD program. Mod Healthc. 1997 Feb 3;27(5):64–65. [PubMed] [Google Scholar]
- Gold M. R., Hurley R., Lake T., Ensor T., Berenson R. A national survey of the arrangements managed-care plans make with physicians. N Engl J Med. 1995 Dec 21;333(25):1678–1683. doi: 10.1056/NEJM199512213332505. [DOI] [PubMed] [Google Scholar]
- Griffiths R. I., Powe N. R., Gaskin D. J., Anderson G. F., de Lissovoy G. V., Whelton P. K. The production of dialysis by for-profit versus not-for-profit freestanding renal dialysis facilities. Health Serv Res. 1994 Oct;29(4):473–487. [PMC free article] [PubMed] [Google Scholar]
- Hakim R. M., Held P. J., Stannard D. C., Wolfe R. A., Port F. K., Daugirdas J. T., Agodoa L. Effect of the dialysis membrane on mortality of chronic hemodialysis patients. Kidney Int. 1996 Aug;50(2):566–570. doi: 10.1038/ki.1996.350. [DOI] [PubMed] [Google Scholar]
- Held P. J., García J. R., Pauly M. V., Cahn M. A. Price of dialysis, unit staffing, and length of dialysis treatments. Am J Kidney Dis. 1990 May;15(5):441–450. doi: 10.1016/s0272-6386(12)70362-1. [DOI] [PubMed] [Google Scholar]
- Held P. J., Levin N. W., Bovbjerg R. R., Pauly M. V., Diamond L. H. Mortality and duration of hemodialysis treatment. JAMA. 1991 Feb 20;265(7):871–875. [PubMed] [Google Scholar]
- Held P. J., Pauly M. V. Competition and efficiency in the end stage renal disease program. J Health Econ. 1983 Aug;2(2):95–118. doi: 10.1016/0167-6296(83)90001-2. [DOI] [PubMed] [Google Scholar]
- Held P. J., Port F. K., Wolfe R. A., Stannard D. C., Carroll C. E., Daugirdas J. T., Bloembergen W. E., Greer J. W., Hakim R. M. The dose of hemodialysis and patient mortality. Kidney Int. 1996 Aug;50(2):550–556. doi: 10.1038/ki.1996.348. [DOI] [PubMed] [Google Scholar]
- Held P. J., Wolfe R. A., Gaylin D. S., Port F. K., Levin N. W., Turenne M. N. Analysis of the association of dialyzer reuse practices and patient outcomes. Am J Kidney Dis. 1994 May;23(5):692–708. doi: 10.1016/s0272-6386(12)70280-9. [DOI] [PubMed] [Google Scholar]
- Hirth R. A., Held P. J. Some of the small print on managed care proposals for end-stage renal disease. Adv Ren Replace Ther. 1997 Oct;4(4):314–324. doi: 10.1016/s1073-4449(97)70020-7. [DOI] [PubMed] [Google Scholar]
- Owen W. F., Jr, Lew N. L., Liu Y., Lowrie E. G., Lazarus J. M. The urea reduction ratio and serum albumin concentration as predictors of mortality in patients undergoing hemodialysis. N Engl J Med. 1993 Sep 30;329(14):1001–1006. doi: 10.1056/NEJM199309303291404. [DOI] [PubMed] [Google Scholar]
- Vladeck B. C. From the Health Care Financing Administration. JAMA. 1995 Jun 28;273(24):1896–1896. doi: 10.1001/jama.273.24.1896. [DOI] [PubMed] [Google Scholar]


