Abstract
Background
Eye movement desensitization and reprocessing (EMDR) therapy has been reported to be very efficacious for treating post-traumatic stress disorder (PTSD) and other anxiety-related conditions. However, a review of the literature reveals the sparse use of this therapy in the field of pediatric dentistry. This study aimed to evaluate anxiety trends in pediatric dental patients during local anesthesia and extraction with and without EMDR therapy.
Methods
Children in the age range of 8–12 years who required dental extractions were assigned randomly into two groups: an EMDR group (group 1) and a routine behavior management therapy group (group 2; receiving more traditional interventions such as tender love and care behavioral modeling, and distraction). Anxiety scores were recorded at four levels using the visual facial anxiety scale (VFAS) preoperatively, after therapy, after the administration of local anesthesia (LA), and after extraction.
Results
Reduced anxiety was observed after the delivery of EMDR therapy, after LA administration, and post-extraction in the EMDR group compared to pre-operative anxiety scores of anxiety (P < 0.001; unpaired Student’s t and Mann-Whitney U tests). In the control group, mild reductions in anxiety after routine behavior management therapy were observed, accompanied by spikes in anxiety levels after LA and extractions.
Conclusion
EMDR therapy was found to be valuable for reducing anxiety among pediatric dental patients during tooth extraction procedures.
Keywords: Anxiety, Children, Extraction, Eye Movement Desensitization Reprocessing, Local Anesthesia
INTRODUCTION
Anxiety is a normal emotional reaction that can be triggered even in the absence of known causes and stimuli. When it is associated with even the thought of visiting a dental care professional for any preventive or therapeutic dental procedure, it is referred to as “dental anxiety” [1]. Dental anxiety ultimately leads to poor oral health status, often manifesting as decayed, missed, and filled tooth surfaces and the further deterioration of oral health—particularly for matters requiring urgent care and attention [2]. Thus, there is both a current and long-term need to alleviate dental anxiety in order to promote preventive and therapeutic oral health care.
Anxiolysis is defined as the reduction of anxiety, achieved either via pharmacological or non-pharmacological techniques [3]. Non-pharmacological techniques include effective communication, audiovisual distraction, reinforcement, “tell-show-do”, behavioral modeling, physical restraints, cognitive behavioral management, and others [1,4]. Guided imagery, systematic desensitization, hypnosis, and progressive muscle relaxation are other psychotherapeutic interventions that can be used for the management of dental anxiety [1].
Eye movement desensitization and reprocessing (EMDR) is a novel psychotherapeutic technique invented by Francine Shapiro in 1989 that primarily aims to treat memories of traumatic origin and the stress symptoms associated with them, mainly in patients with post-traumatic stress disorder (PTSD) [5]. EMDR therapy can also be used to address neurotic problems such as phobias, anxiety-related disorders, and depression [6]. However, in current practice, EMDR therapy has been successfully used to reduce anxiety among children prior to new stressful situations, such as prior to the administration of local anesthesia (LA) or invasive medical procedures [7,8]. However, the role of this therapy in the pediatric dental field has not been studied extensively. Hence, in this trial, we evaluated the effect of EMDR therapy for anxiolysis among children who either had unpleasant memories of past dental experiences, or those who had no dental experience but had anticipatory anxiety issues due to having received threatening information regarding dental procedures. In order to showcase the principles of EMDR, children who had had positive prior dental experiences or showed no anxiety were not included in this study.
The therapy consists of a standard protocol in which eight phases are considered to involve bilateral stimulation (most commonly horizontal saccadic eye movements) to desensitize the level of discomfort caused by traumatic memories. The therapy also targets reprocessing traumatic memories and integrating them into the patient's standard biographical memories [6,9].
The method is based on the concept of the adaptive information processing (AIP) model [10]. EMDR has been extensively studied, and is even recognized by the National Institute for Health and Clinical Excellence and the World Health Organization as a treatment of choice for PTSD [6,11]. It has also been reported in the literature that the use of alternating bilateral stimulation of the eyes in patients with dental phobias due to prior histories of traumatic dental experiences was found to be effective in cases of mild-to-moderate phobias [12]. Alternating bilateral stimulation of the eyes can be easily guided by clinicians and is simple to execute on patients with phobias during treatment procedures in the dental operating room [11,12].
The purpose of this study was to evaluate anxiety trends in pediatric dental patients during the administration of LA and dental extraction procedures, with and without EMDR therapy.
METHODS
1. Study design
This study was conducted on 8–12-year-old children who presented to the Outpatient Department of Pedodontics & Preventive Dentistry (OPD) at the University College of Medical Sciences and Guru Teg Bahadur Hospital (Delhi, India). This age range was selected because children of these ages can be easily guided to follow instructions and perform eye movements, while children in lower age ranges are not able to properly roll their eyes as needed to complete the therapy—as was shown in an earlier study by Tirupathi et al. [7]. The majority of the children who reported to the dental OPD needing dental extractions also fell into this age range. Dietary counseling and oral hygiene instructions were given to all of the patients.
Ethical clearance was granted by the institutional ethics committee IECHR-2022-53-10-R2 dated 28-04-2022 and the study was registered as a clinical trial under the identifier CTRI/2023/05/052370. The nature and aim of our study were explained to both the parents and the children. Before proceeding with any interventions, written consent was obtained from the parents, and assent was indicated by all of the children.
The sample size required for this study was calculated at a 95% confidence interval (α = 0.05) and 80% statistical power as:
(β = 0.20) where Zα & Zβ are constant (Zα = 1.96 and Zβ = 0.84) with an expected effect size (ES) of 0.69 and a δ of 3.007. The estimated sample size was 19.
Children who were experiencing any specific medical illnesses or physiological impairments, those who were intellectually deficient, and those with any known allergies to local anesthetics were excluded from the study. We included children aged 8–12 years who require dental extractions due to sequelae resulting from grossly decayed teeth, unrestorable teeth with only root stumps remaining, pathologic resorption, furcation involvement, and who were showing mild to moderate levels of anxiety preoperatively as per the indicators in the novel visual facial anxiety scale (VFAS) [13].
When the inclusion criteria were met the patients were assigned a number based on a sequence generated via the block randomization method (www.randomization.com). The sequence allocated was concealed from all of the participating investigators using sequentially numbered opaque sealed envelopes (SNOSEs). Two groups were generated:
Group I: EMDR therapy.
Group II: Routine behavior management therapy (including traditional methods such as tender love and care [TLC], behavioral modeling, distraction, and others).
EMDR therapy was used in the test group for behavior management. Levels of anxiety were recorded using the VFAS at four different time intervals: baseline anxiety/pre-operative, after the delivery of behavior management therapy, after administering the local anesthetic injection, and after the extraction procedure was completed. The investigator was well-trained in recording medical, history including mental state examinations, as well as identifying anxiety-related symptoms and the correct way to conduct EMDR therapy. EMDR was conducted under the guidance of a certified professor of psychiatry as well. The investigator had also been trained and certified in EMDR via an accredited course from the International Academy of Therapists (IAOTH). EMDR therapy was performed by the investigator, and the measurement of anxiety levels was done by a post-graduate student from the Department of Pedodontics and Preventive Dentistry. LA administration and dental extraction were done by the investigator under the supervision of a professor from the Department of Pedodontics and Preventive Dentistry. The step-wise summary of the study methodology is illustrated in Fig. 1.
Fig. 1. Stepwise illustration of the study methodology. EMDR, eye movement desensitization and reprocessing; n, number; UCMS & GTBH, University College of Medical Sciences and Guru Teg Bahadur Hospital.
The adaptive form of EMDR therapy for the children was included. During the detailed history-taking phase the children were asked about situations that caused them anxiety. They were guided to think about a safe place before starting the procedure, asked to perform the eye movements required by the therapy (Fig. 2), and the therapy was delivered in eight phases as per the standard EMDR therapy protocol detailed by Francine Shapiro [9]. The therapy was given just prior to the administration of local anesthesia (Table 1).
Fig. 2. Performing eye movement desensitization and reprocessing therapy on a child in the dental operating suite.
Table 1. Phases of EMDR therapy (simplified steps for children).
| S. no. | Phases | Description |
|---|---|---|
| Phase 1 | History taking | Questioning to identify past events or current triggers that is causing anxiety to the child. |
| Phase 2 | Preparation | Metaphors and techniques were used to nurture stabilization and a state of self-restraint like to imagine about a place that is giving a sense of tranquility. |
| Phase 3 | Assessment | Elicitation of emotion creating anxiety and any desired constructive view was introduced to the child. |
| Phase 4 | Desensitization | Eye movements were instilled that allowed the spontaneous disclosure of past or currently held emotions or beliefs and any physical sensations. |
| Phase 5 | Installation | Soundness of desired constructive belief was enhanced by repeatedly incorporating eye movements. |
| Phase 6 | Body scan | Child was asked to concentrate on any residual physical sensation like to notice taught abdomen, crossed legs, perspiration on palm or anything in the body anywhere. |
| Phase 7 | Closure | Metaphors and self control techniques were used if needed to reassure the child. |
| Phase 8 | Reevaluation | The treatment effects were evaluated. |
EMDR, eye movement desensitization and reprocessing.
Behavior management was done in the control group using routine behavior management techniques such as TLC, distraction, behavioral modeling, tell-show-do, and others.
1. Surgical procedure
Before injecting the LA, a topical numbing gel (lignocaine hydrochloride 2%) was applied to the injection site. After a delay of 3–5 minutes for it to infiltrate the tissues, the LA agent (lignocaine 2%, 1:200,000 adrenaline) was injected using a 26 G (12 mm) needle. All LA injections were given by one operator only. The rate of LA administration was slow, maintaining an average duration of approximately 1 mL/minute to cause less discomfort to the patient.
After confirming the adequacy of the LA, each patient was positioned appropriately in the dental chair and the teeth were separated gently and firmly from their soft tissue attachments using a #9 Molt’s Periosteal elevator by applying the concave aspect of the instrument facing the cervical aspect of the tooth. The straight elevator was used to luxate the tooth, which was then removed using appropriately sized forceps. Postoperative instructions were given in accordance with the American Academy of Pediatric Dentistry (AAPD) guidelines, and a moist gauze piece was packed at the surgical site under firm pressure to control any bleeding [14].
2. Statistical analysis
Data was retrieved and compiled onto a Microsoft Excel worksheet and statistically analyzed using Statistical Packages for Social Sciences (SPSS) version 21 software. Numbers and percentages for categorical data, and means and standard deviations for continuous data, were calculated for each group. The unpaired Student’s t-test was used for inter-group comparisons of continuous data, and the Mann-Whitney U test was used for comparisons between the groups.
RESULTS
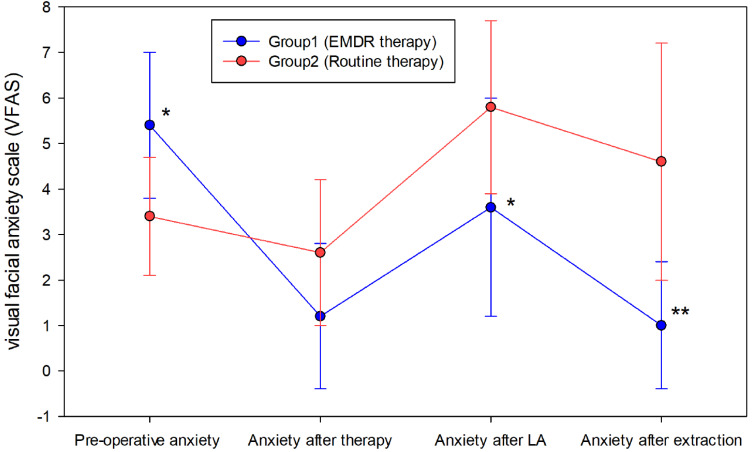
A total of 20 children (10 male and 10 female) were included in this randomized controlled pilot study. All fell within the 8–12-year-old age range, with a mean age of 9.6 ± 1.5 (Table 2). The evaluation of anxiety was done using VFAS at four different time intervals. When the anxiety measurements following the delivery of behavior management therapy were compared between the two groups, it was found that the difference in the means was –1.40, which was not statistically significant (P > 0.05; Table 3, Fig. 3). However, when anxiety measurements immediately after the administration of LA were compared, it was found that the difference in mean was –2.20—which was statistically significant (P < 0.05). Similarly, the difference in means immediately after extraction was –3.60, which was also statistically significant (P < 0.05; Table 3). Thus, children in the EMDR group experienced less anxiety after the administration of LA and following the extraction procedure, compared to those who only received routine behavior management therapy.
Table 2. Demographic details depicting the gender wise and mean age distribution of study participants.
| Frequency | Percent | P value | ||
|---|---|---|---|---|
| Gender | Male | 10 | 50.0% | 1.00 |
| Female | 10 | 50.0% | ||
| Total | 20 | 100.0% | ||
| Age | N | Minimum age (years) | Maximum age (years) | Mean ± SD |
| 20 | 8.0 | 12.0 | 9.6 ± 1.5 | |
N, number; SD, standard deviation.
Table 3. Intergroup comparison of anxiety among children at different time intervals in both groups.
| Intervals at which anxiety is recorded | Group 1 (EMDR therapy) Mean ± SD | Group 2 (routine behavior management therapy) Mean ± SD | P value |
|---|---|---|---|
| Pre-operative anxiety (A1) | 5.4 ± 1.6 | 3.4 ± 1.3 | 0.008 |
| Anxiety after therapy (A2) | 1.2 ± 1.6 | 2.6 ± 1.6 | 0.077 |
| Anxiety after LA (A3) | 3.6 ± 2.4 | 5.8 ± 1.9 | 0.041* |
| Anxiety after extraction (A4) | 1 ± 1.4 | 4.6 ± 2.6 | < 0.001** |
Statistical test: Unpaired Student’s t-test - intergroup comparison, Mann Whitney U test - intergroup comparison between the groups, *statistically significant if P value < 0.05, **statistically highly significant if P value < 0.001. EMDR, eye movement desensitization and reprocessing; LA, local anesthesia.
Fig. 3. Comparison of anxiety parameters at different time intervals. Statistical test: Unpaired Student’s t-test - intergroup comparison, Mann Whitney U test - intergroup comparison between the groups, *statistically significant if P value < 0.05, **statistically highly significant if P value < 0.001. EMDR, eye movement desensitization and reprocessing.
DISCUSSION
We studied the effect of EMDR therapy among 8–12-year-old dental patients experiencing anxiety while undergoing extraction procedures. As the administration of LA and dental extractions are anxiety-provoking and can cause emotional trauma in children, management of this anxiety can help practitioners better conduct the procedures, as well as instill positive attitudes in the child for future dental appointments [7]. Thus, behavior management is a challenge that must be overcome in pediatric dentistry for optimal conductance of more complex procedures. There are various behavior management techniques used in pediatric dentistry—including non-verbal communication, empathy, tell-show-do, positive and negative reinforcement, behavior shaping, behavioral modeling, distraction, voice control, and others [1,4]. However, many newer techniques and advancements have also been developed more recently, such as tell-play-do, audiovisual and video-game distraction, mobile dental app, virtual reality-based distraction, Snoezelen environment, the child-centered approach, hypnosis, muscle relaxation techniques, and many more [15]. Thus, considering the need for behavior management and the ever-evolving techniques available, this study introduces a novel therapy that may not only address anxiety related to dental procedures, but may also help some children reprocess any past negative beliefs, thus instilling a positive attitude and better willingness to accept future treatments.
EMDR, which works on the principle of adaptive information processing (AIP), helps in the reprocessing of traumatic memories into more semantic ones. Some upsetting negative occurrences appear to overburden the information processing system, preventing their integration through adaptation [6]. According to one theory, the recollection of a traumatic incident contains the upsetting feelings, bodily sensations, and viewpoints that were present at the time. In such circumstances, the negative event information is kept in isolation and is unable to connect with the adaptive memory networks. The person may experience some or all of the sensory, cognitive, emotional, and physical features of the previous memory as a result of current circumstances, leading to maladaptive or symptomatic behavior [6]. The AIP model sees dysfunctionally stored memories as the cause of negative attitudes, behaviors, and personality traits [6]. This view of psychological pathology is the theoretical core of EMDR therapy.
EMDR therapy has been used in the medical field for a number of different conditions, including PTSD with a dissociative component, complex trauma, and single-episode trauma [9]. The treatment has also been effective for conduct issues, self-esteem, body dysmorphic disorder, olfactory reference syndrome [16], sexual dysfunction, performance anxiety [17], pain management [18], bipolar disorder, psychosis, unipolar depression, obsessive-compulsive disorder, and alcoholism [6].
As the effectiveness of EMDR therapy depends on the body and mind's capacity to work through emotions and thoughts, it may not work if one is unable to process information in a way that might be related to any medical condition.
A study by Doering et al. [19] showed that EMDR was associated with significant reductions in dental procedure-related anxiety and avoidance behavior, as well as in symptoms of PTSD. De Jongh et al. [20] evaluated the use of EMDR for treating trauma-induced dental phobias. They noted that, after receiving the therapy, a majority of their patients were able to overcome their anxieties (both self- and observer-rated), and the researchers succeeded in instilling positive frames of mind toward dental treatments in the patients. EMDR therapy has also been used in children for the prevention of anxiety prior to surgical invasive procedures, as well as in a number of medical fields [8].
There has been a scarcity of studies conducted on behavior management in dentistry, which has led to very limited practice of these techniques in pediatric dental patients. In a study by Tirupathi et al. [7], eye movement distraction was used and found to be effective for limiting dental anxiety. Thus, considering results such as these, we introduced all phases of the EMDR therapy—a recent and novel approach—to evaluate the outcome measures on anxiety among pediatric dental patients.
The main limitation of our study is its low sample size. With a greater one, greater generalizability of the findings could be expected. To verify the anxiety trends more precisely, complex scales and other indicators such as heart rate, oxygen saturation levels, and blood pressure could be monitored as well.
This study provides preliminary evidence for the efficacy of EMDR in reducing anxiety among pediatric dental patients undergoing LA injection and dental extraction procedures, compared to those who received only routine behavior management therapy. These results shed light on the need for more studies of this nature to be conducted in the future.
ACKNOWLEDGEMENT
The authors would like to express their gratitude to the patient and their parents who consented to take part in this study.
Footnotes
- Namita Kalra: Conceptualization, Formal analysis, Methodology, Supervision, Visualization, Writing – original draft, Writing – review & editing.
- Apoorva Rathore: Conceptualization, Data curation, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing.
- Rishi Tyagi: Conceptualization, Data curation, Methodology, Visualization, Writing – original draft, Writing – review & editing.
- Amit Khatri: Conceptualization, Formal analysis, Supervision, Visualization, Writing – review & editing.
- Deepak Khandelwal: Conceptualization, Formal analysis, Supervision, Writing – original draft, Writing – review & editing.
- Padma Yangdol: Conceptualization, Methodology, Visualization, Writing – original draft, Writing – review & editing.
CONFLICT OF INTEREST: None.
References
- 1.Appukuttan DP. Strategies to manage patients with dental anxiety and dental phobia: literature review. Clin Cosmet Investig Dent. 2016;8:35–50. doi: 10.2147/CCIDE.S63626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Porritt J, Buchanan H, Hall M, Gilchrist F, Marshman Z. Assessing children's dental anxiety: a systematic review of current measures. Community Dent Oral Epidemiol. 2013;41:130–142. doi: 10.1111/j.1600-0528.2012.00740.x. [DOI] [PubMed] [Google Scholar]
- 3.Goodchild JH, Feck AS, Silverman MD. Anxiolysis ingeneral dental practice. Dent Today. 2003;22:106–111. [PubMed] [Google Scholar]
- 4.Liu Y, Gu Z, Wang Y, Wu Q, Chen V, Xu X, et al. Effect of audiovisual distraction on the management of dental anxiety in children: a systematic review. Int J Paediatr Dent. 2019;29:14–21. doi: 10.1111/ipd.12430. [DOI] [PubMed] [Google Scholar]
- 5.Shapiro F. Eye Movement Desensitization and Reprocessing (EMDR) and the anxiety disorders: clinical and research implications of an integrated psychotherapy treatment. J Anxiety Disord. 1999;13:35–67. doi: 10.1016/s0887-6185(98)00038-3. [DOI] [PubMed] [Google Scholar]
- 6.Oren EM, Solomon R. EMDR therapy: an overview of its development and mechanisms of action. Eur Rev Appl Psychol. 2012;62:197–203. [Google Scholar]
- 7.Tirupathi S, Krishna N, Rajasekhar S, Nuvvula S. Eye movement distraction: a new distraction technique for management of dental anxiety during intraoral local anesthesia administration in children. Int J Clin Pediatr Dent. 2019;12:507–509. doi: 10.5005/jp-journals-10005-1690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wigley IL, De Tommasi V, Bonichini S, Fernandez I, Benini F. EMDR and nonpharmacological techniques for anxiety prevention in children prior to invasive medical procedures: a randomized controlled trial. J EMDR Pract Res. 2019;13:163–175. [Google Scholar]
- 9.Shapiro F. The role of eye movement desensitization and reprocessing (EMDR) therapy in medicine: addressing the psychological and physical symptoms stemming from adverse life experiences. Perm J. 2014;18:71–77. doi: 10.7812/TPP/13-098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hase M, Balmaceda UM, Ostacoli L, Liebermann P, Hofmann A. The AIP model of EMDR therapy and pathogenic memories. Front Psychol. 2017;8:1578. doi: 10.3389/fpsyg.2017.01578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Landin-Romero R, Moreno-Alcazar A, Pagani M, Amann BL. How does eye movement desensitization and reprocessing therapy work? a systematic review on suggested mechanisms of action. Front Psychol. 2018;9:1395. doi: 10.3389/fpsyg.2018.01395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De Jongh A, van den Oord HJ, ten Broeke E. Efficacy of eye movement desensitization and reprocessing in the treatment of specific phobias: Four single-case studies on dental phobia. J Clin Psychol. 2002;58:1489–1503. doi: 10.1002/jclp.10100. [DOI] [PubMed] [Google Scholar]
- 13.Cao X, Yumul R, ElvirLazo OL, Friedman J, Durra O, Zhang X, et al. A novel visual facial anxiety scale for assessing preoperative anxiety. PLoS One. 2017;12:e0171233. doi: 10.1371/journal.pone.0171233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ferneini EM, Bennett J. In: McDonald and Avery’s dentistry for the child and adolescent. 10th ed. Dean JA, editor. Elsevier; 2016. Oral surgery for pediatric patient; pp. 627–644. [Google Scholar]
- 15.Swarna K, Prathima GS, Suganya M, Sanguida A, Selvabalaji A. Recent advances in non-pharmacological behavior management techniques in children–an overview. IOSR J Dent Med Sci. 2019;18:18–21. [Google Scholar]
- 16.McGoldrick T, Begum M, Brown KW. EMDR and olfactory reference syndrome: A case series. J EMDR Pract Res. 2008;2:63–68. [Google Scholar]
- 17.Barker RT, Barker SB. The use of EMDR in reducing presentation anxiety. J EMDR Pract Res. 2007;1:100–108. [Google Scholar]
- 18.Grant M, Threlfo C. EMDR in the treatment of chronic pain. J Clin Psychol. 2002;58:1505–1520. doi: 10.1002/jclp.10101. [DOI] [PubMed] [Google Scholar]
- 19.Doering S, Ohlmeier MC, de Jongh A, Hofmann A, Bisping V. Efficacy of a trauma focused treatment approach for dental phobia: a randomized clinical trial. Eur J Oral Sci. 2013;121:584–593. doi: 10.1111/eos.12090. [DOI] [PubMed] [Google Scholar]
- 20.De Jongh A, van den Oord HJ, ten Broeke E. Efficacy of eye movement desensitization and reprocessing in the treatment of specific phobias: Four single-case studies on dental phobia. J Clin Psychol. 2002;58:1489–1503. doi: 10.1002/jclp.10100. [DOI] [PubMed] [Google Scholar]