Abstract
Introduction
The transient receptor potential canonical (TRPC) ion channels have been implicated in the pathophysiology of major depressive disorder (MDD), and TRPC inhibition has been shown to reduce depressive-like behaviour in rodent models of depression. BI 1358894, a small-molecule inhibitor of TRPC ion channels, is currently being developed for the treatment of MDD.
Objective
Two phase I studies assessed the safety, tolerability, and pharmacokinetics (PK) of oral BI 1358894 in fed and fasted states following a single ascending dose (SAD) [NCT03210272/1402-0001] and multiple ascending doses (MAD) [NCT03754959/1402-0002] in healthy male volunteers. In addition, any potential food effect was evaluated after a single dose.
Methods
In both studies, eligible healthy male volunteers (aged 18–45 years; body mass index of 18.5–29.9 kg/m2) were allocated to receive BI 1358894 or placebo. In the SAD study (1402-0001), volunteers were randomised 3:1 to receive BI 1358894 or placebo in fasted (3, 6, 10, 25, 50, 100, or 200 mg) and fed states (200 mg). The food effect part was conducted as an open-label, randomised, two-way crossover study at doses of 50 and 100 mg in fasted and fed states (high-calorie, high-fat breakfast). For the MAD study (1402-0002), volunteers were randomised 4:1 to receive BI 1358894 (10, 25, 50, 100, or 200 mg) or placebo once daily for 14 days under fed conditions. Primary endpoint (both studies): number of volunteers with drug-related adverse events (DRAEs). Secondary PK endpoints for study 1402-0001: area under the concentration–time curve (AUC) from time zero extrapolated to infinity (AUC∞), maximum plasma concentration (Cmax), and AUC from time zero to the last quantifiable data time point (AUC0–tz). Secondary PK endpoints for study 1402-0002: AUC over 0–24 h (AUC0–24), Cmax after the first dose, and steady-state AUC and Cmax over a uniform dosing interval (AUCτ,ss and Cmax,ss, respectively) after the last dose.
Results
BI 1358894 was well tolerated at doses ≤ 200 mg under all tested conditions and no dose dependency was observed in DRAE frequency for either study. In the SAD study, BI 1358894 exposure increased dose proportionally across 3–50 mg in the fasted state and across 50–200 mg in the fed state. A positive food effect was observed at the tested doses. In the MAD study, BI 1358894 exposure increased less than dose proportionally across 10–200 mg.
Conclusions
These studies demonstrate that BI 1358894 is well tolerated in healthy male volunteers following single and multiple doses, with no dose dependency observed in DRAE frequency. BI 1358894 exposure increased dose dependently in both the SAD and MAD studies, with higher exposure of BI 1358894 observed in the fed state.
ClinicalTrials Registration
These trials have been registered on ClinicalTrials.gov: NCT03210272/1402-0001 (registered on 6 July 2017) and NCT03754959/1402-0002 (registered on 27 November 2018).
Key Points
| Single and multiple doses of BI 1358894 had favourable safety profiles and were well tolerated. |
| BI 1358894 exposure increased dose dependently, and dose proportionality was observed: single doses of 50–200 mg (fed) and 3–50 mg (fasted). |
Introduction
Major depressive disorder (MDD) is a psychiatric disorder associated with affective disturbances [1] and was ranked among the top 13 leading causes of burden worldwide in 2019 [2]. Several recommended treatment options are available for patients with MDD, but no specific pharmacological treatment has been shown to be clinically superior [3–5]. Patients generally receive antidepressant therapy such as selective serotonin reuptake inhibitors as first-line treatment and if they do not respond it is usually recommended that they switch to an alternative antidepressant [3].
Symptoms associated with MDD, such as trait rumination, have been linked to amygdala hyperactivity [6]. Transient receptor potential canonical (TRPC) ion channels have been shown to be expressed in areas of the rodent brain associated with the processing of emotion and mood, such as the amygdala [7]. Riccio and colleagues observed abundant levels of TRPC expression in the amygdala of mice and reported that TRPC-/- mice exhibited diminished fear-related behaviours [8, 9]. Interactions between TRPC ion channels and neurotransmitter networks have been implicated in the pathophysiology of MDD, and TRPC ion channel inhibition has been demonstrated to ameliorate depression-like behaviour in rodents [10, 11]. BI 1358894, a small-molecule inhibitor of TRPC ion channels, is currently under development for the treatment of MDD. Data from two phase I clinical studies investigating the safety, tolerability and pharmacokinetics (PK) are presented here.
Objective
In the first study (ClinicalTrials.gov identifier: NCT03210272/1402-0001), the primary objective was to assess the safety and tolerability of BI 1358894 using a single ascending dose (SAD) schedule in healthy male volunteers. The secondary objectives were to explore the PK of BI 1358894 after single dosing, and to investigate the influence of food on the safety and relative bioavailability of BI 1358894. As such, this study was comprised of two parts: the SAD part and the food effect part.
In the second study (ClinicalTrials.gov identifier: NCT03754959/1402-0002), the primary objective was to assess the safety and tolerability of BI 1358894 following a multiple ascending dose (MAD) schedule in healthy male volunteers. The secondary objectives were to examine the PK of BI 1358894 following a MAD schedule and to assess the drug–drug interaction (DDI) effects of BI 1358894 on the PK of midazolam. Midazolam is a useful probe for assessing cytochrome P450 3A (CYP3A) metabolism, and it has been shown that microdoses are pharmacologically inactive [12]. The results of PK data showing no DDI with CYP3A have been published elsewhere and were not the focus of this manuscript [12, 13].
Methods
Study Design
1402-0001 Study Part 1
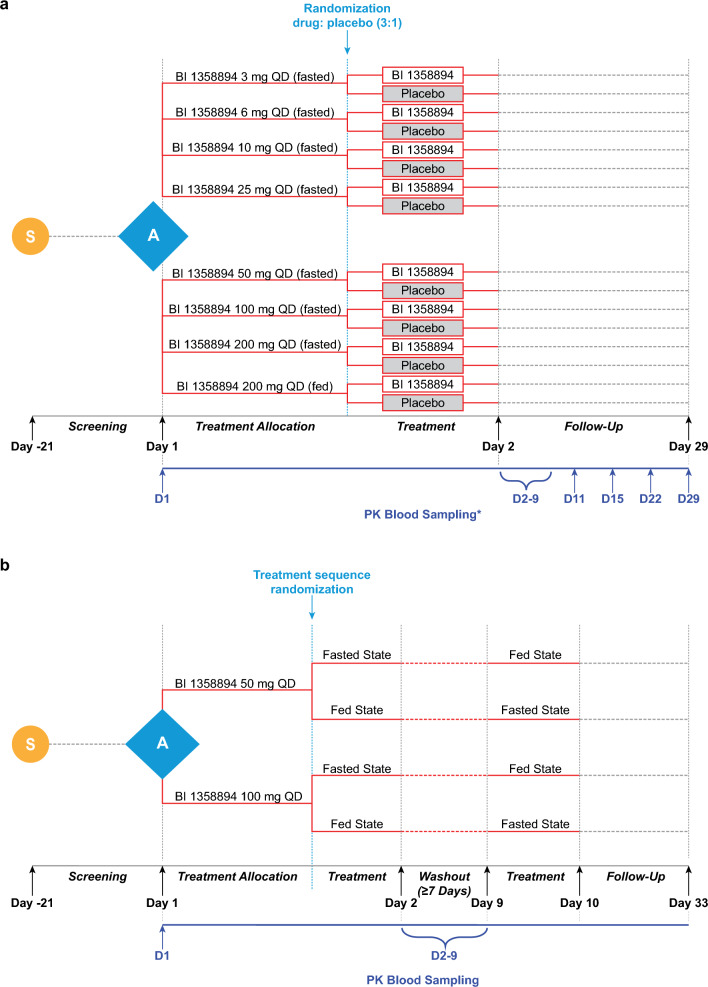
For the SAD part, eligible volunteers were enrolled in a single-blind, partially randomised, placebo-controlled parallel group study. Initially, volunteers were allocated to receive BI 1358894 3, 6, 10, 25, 50, 100, and 200 mg under fasted conditions, or BI 1358894 200 mg under fed conditions. The volunteers were then randomised within each dose group to receive BI 1358894 or placebo in a 3:1 (drug:placebo) randomisation ratio. Each dose group comprised six volunteers receiving BI 1358894 and two volunteers receiving placebo. Prior to receiving study treatment, volunteers were fasted, or, for the BI 1358894 200 mg fed group, received a high-fat, high-calorie breakfast. Each dose was investigated sequentially in ascending order, with each subsequent dose group only being investigated following a dose escalation review. Plasma PK samples were collected following BI 1358894 administration as follows: 3 mg dose group, Days 1–5; 6–200 mg (fasted) dose groups, Days 1–9; 200 mg (fed) dose group, Days 1–7 and then on Days 9, 11, 15, 22, and 29 [Fig. 1a]. For the quantification of BI 1358894 plasma concentrations in the blood samples, 2.7 mL of blood was drawn from the forearm vein into a potassium ethylenediaminetetraacetic acid anticoagulant blood drawing tube, tightly capped and stored at −20°C. The plasma samples were extracted by protein precipitation in a 96-well plate. An aliquot (50 μL) was mixed with 250 μL of an internal standard solution (10 nmol/L BI 1358894) dissolved in acetonitrile/methanol/water (50/45/5, v/v/v), centrifuged, and 160 μL supernatant was mixed with 200 μL of 10 mM ammonium formate buffer (pH 4). Blank human plasma was used for the preparation of calibration samples, quality control samples and blank samples. Chromatography was performed using an analytical reversed-phase ultra performance liquid chromatography column (ACQUITY UPLC BEH Shield RP18) with 10 μL of samples. BI 1358894 concentrations in plasma were analysed by a tandem mass spectrometer with electrospray ionisation in the positive ion mode.
Fig. 1.
Design for study 1402-0001 for (a) the SAD part and (b) the food effect part. *Plasma samples for PK assessment of BI 1358894 in the 3 mg fasted dose group were collected on Days 1–5 following BI 1358894 administration. In the BI 1358894 6–200 mg dose groups, plasma samples for PK assessment were collected on Days 1–9 following BI 1358894 administration. In the BI 1358894 200 mg fed group, plasma samples for PK assessment were collected on Days 1–7, and then on Days 9, 11, 15, 22 and 29, following drug administration. A allocation, D day, PK pharmacokinetic, QD once daily, S screening, SAD single ascending dose
1402-0001 Study Part 2
For the food effect part, eligible volunteers were enrolled in an open-label, randomised, two-way crossover study. Volunteers were randomised to two treatment sequences: fed followed by fasted, or fasted followed by fed. For each sequence, they received either BI 1358894 50 or 100 mg as a single dose after fasting or after having received a high-fat, high-calorie breakfast. There was a washout period of at least 7 days between treatment administrations within each sequence. Plasma PK samples were collected on Days 1–9 following BI 1358894 administration (Fig. 1b) and analysed as reported in Sect. 2.1.1.
1402-0002 Study Part 1
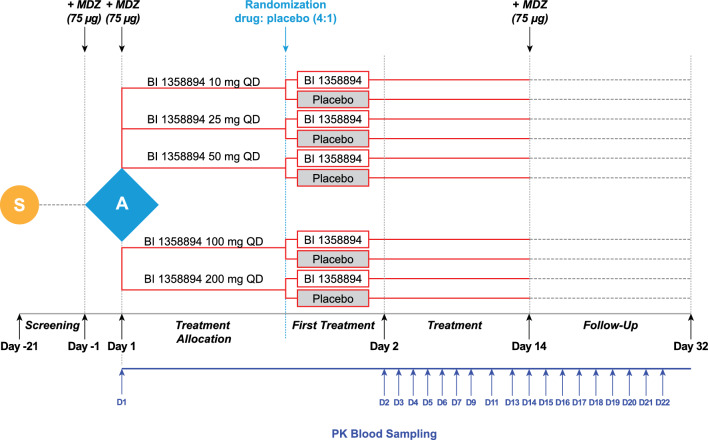
For the MAD part, eligible volunteers were initially allocated to a BI 1358894 dose group (10, 25, 50, 100, or 200 mg) before being randomised to receive BI 1358894 or placebo (4:1 ratio) within each group. Volunteers received BI 1358894 or placebo once daily for 14 days under fed conditions. Each dose of BI 1358894 was investigated sequentially, in ascending order, with each subsequent dose group only being investigated following a dose-escalation review. Plasma samples for PK assessment of BI 1358894 were collected on Days 1–7, Day 9, Day 11, and Days 13–22 (Fig. 2) and analysed as reported in Sect. 2.1.1.
Fig. 2.
Study design for study 1402-0002. A allocation, D day, MDZ midazolam, PK pharmacokinetic, QD once daily, S screening
1402-0002 Study Part 2
The DDI assessment was conducted by using a microdose of midazolam as part of the regular MAD trial (part 1). Midazolam (75 µg) was administered to volunteers across all dose groups 1 day prior to receiving their first dose of BI 1358894 or placebo, and in parallel to receiving BI 1358894 or placebo on Days 1 and 14. It should be noted that the DDI PK data have been published elsewhere and will not be reported here [12, 13].
Participants
Both phase I studies were conducted in healthy male volunteers at sites in Germany. Demographic data are presented in Tables 1 and 2. Volunteers were included in the studies if they were healthy according to the investigator’s assessment, were 18–45 years of age, and had a body mass index (BMI) of 18.5–29.9 kg/m2. Volunteers were excluded if they had any finding in the medical examination deviating from normal, laboratory values outside the reference range, or evidence of concomitant disease considered clinically relevant by the investigator. Other exclusion criteria included the use of drugs that might influence the study results within 30 days prior to administration of study treatment, smoking (>10 cigarettes per day), a previous history of suicidal ideation, or alcohol or drug abuse. Recruitment was limited to male volunteers as conclusive data on reproductive toxicology were not yet available for these early clinical studies.
Table 1.
Participant demographics and baseline characteristics by treatment group for the single ascending dose part of study 1402-0001
| BI 1358894 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Placebo | 3 mg | 6 mg | 10 mg | 25 mg | 50 mg | 100 mg | 200 mg | 200 mg fed | Total | |
| [n = 15] | [n = 6] | [n = 6] | [n = 6] | [n = 6] | [n = 6] | [n = 6] | [n = 6] | [n = 6] | [N = 63] | |
| Completed, n | 15 | 6 | 6 | 6 | 6 | 6 | 6 | 6 | 6 | 63 |
| White, n | 15 | 6 | 5 | 6 | 5 | 6 | 6 | 6 | 5 | 60 |
| Black or African American, n | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 3 |
| Mean age, years (SD) | 33.7 (5.8) | 40.2 (7.4) | 33.7 (7.4) | 36.2 (6.0) | 36.2 (7.3) | 40.2 (3.5) | 35.5 (6.6) | 38.3 (7.0) | 28.0 (3.6) | 35.5 (6.7) |
| Mean BMI, kg/m2 (SD) | 26.4 (2.3) | 24.9 (3.2) | 23.4 (3.1) | 26.6 (2.0) | 24.9 (3.0) | 27.5 (2.5) | 27.1 (2.9) | 26.6 (1.4) | 24.6 (2.9) | 25.9 (2.7) |
BMI body mass index, SD standard deviation
Table 2.
Participant demographics and baseline characteristics by treatment group for the food effect part of study 1402-0001
| 50 mg fed/50 mg fast | 50 mg fast/50 mg fed | 100 mg fed/100 mg fast | 100 mg fast/100 mg fed | Total | |
|---|---|---|---|---|---|
| [n = 4] | [n = 4] | [n = 6] | [n = 6] | [N = 20] | |
| Completed, n | 4 | 4 | 6 | 6 | 20 |
| White, n | 4 | 4 | 6 | 6 | 20 |
| Other race, n | 0 | 0 | 0 | 0 | 0 |
| Mean age, years (SD) | 36.8 (8.8) | 32.5 (8.3) | 34.2 (10.2) | 30.0 (8.1) | 33.1 (8.6) |
| Mean BMI, kg/m2 (SD) | 23.4 (4.0) | 26.7 (1.4) | 25.7 (2.9) | 25.1 (2.7) | 25.3 (2.8) |
BMI body mass index, SD standard deviation
Endpoints and Assessments
1402-0001
The primary endpoint for study 1402-0001 was the number of volunteers with drug-related adverse events (DRAEs). Serious adverse events (SAEs) were defined as any AE that resulted in death, was immediately life-threatening, required inpatient hospitalisation, prolonged existing hospitalisation, resulted in persistent disability, was a congenital anomaly/birth defect, or was deemed serious for any other reason. Cancers of new histology and exacerbations of existing cancer were classified as an SAE regardless of the duration between discontinuation of the drug. An adverse event of special interest (AESI) was defined as any specific AE identified as being of particular concern for prospective safety monitoring and assessment within the trial; hepatic injury was the only protocol-specified AESI. The intensity of AEs was classified as mild (awareness of signs/symptoms that were easily tolerated), moderate (enough discomfort to cause interference with usual activity) or severe (incapacitating or causing inability to work or perform usual activities).
Safety was further assessed by collating treatment-emergent AEs (TEAEs), routine laboratory tests, and the evaluation of vital signs, electrocardiograms (ECGs), visual analogue scales (VAS), and suicidality assessment via the Columbia Suicidal Severity Rating Scale (C-SSRS).
The secondary PK endpoints of interest were the area under the concentration–time curve (AUC) of BI 1358894 in plasma from administration time (t = 0) to the last quantifiable data point (AUC0–tz); AUC of BI 1358894 in plasma from administration time (t = 0) extrapolated to infinity (AUC0–∞); and maximum measured concentration of BI 1358894 in plasma (Cmax).
1402-0002
For study 1402-0002, the primary endpoint was the number of volunteers with DRAEs. The SAEs and AESIs were as defined in Sect. 2.3.1. Safety was also evaluated using TEAEs, laboratory tests, vital signs, ECGs, VAS, and the C-SSRS.
The secondary PK endpoints of interest were AUC of BI 1358894 in plasma from administration time (t = 0) to 24 h (AUC0–24) after administration of the first dose; Cmax of BI 1358894 in plasma after administration of the first dose; AUC of BI 1358894 in plasma at steady state over a uniform dosing interval (AUCτ,ss) after the last dose; and Cmax of BI 1358894 in plasma at steady state over a uniform dosing interval (Cmax,ss) after the last dose.
Ethical Considerations
The studies were carried out in accordance with the principles of the Declaration of Helsinki, the International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use (ICH) Good Clinical Practice (GCP) guidelines, applicable regulatory requirements and Boehringer Ingelheim standard operating procedures. All participants provided informed written consent in accordance with ICH GCP and local procedures. The study protocol was reviewed and approved by the local independent ethics committees and relevant local authorities.
Statistical Analysis
For both studies, all primary safety and PK endpoints were calculated descriptively. For study 1402-0001, the PK parameters of AUC and Cmax were assessed for dose proportionality using a regression model applied to log-transformed data. Based on the estimate for the slope parameter, a two-sided 95% confidence interval (CI) of the slope was computed. The relative bioavailability based on AUC0–tz, AUC0–∞ and Cmax was analysed using an analysis of variance (ANOVA) model on log-transformed data. Exposure ratio of test versus reference treatment (geometric mean [gMean]) was calculated.
The SAD part planned to include 64 volunteers; this was not based on a power calculation. The size of eight volunteers per dose group (six receiving BI 1358894 and two receiving placebo) is commonly used in SAD studies and is considered sufficient for the exploratory evaluation of single-dose safety and PK endpoints. For the food effect part, a maximum of 24 volunteers (12 receiving BI 1358894 50 mg and 12 receiving BI 1358894 100 mg) were planned for enrolment. With this sample size, a certain precision in estimating the ratio of gMeans could be expected with 95% probability. As this was a first-in-man trial, no information on intrasubject variability was available.
For study 1402-0002, dose proportionality was assessed using a linear regression model applied to log-transformed data. Based on the estimate for the slope parameter, a two-sided 90% CI for the slope was computed. Attainment of steady state was analysed for each dose level by a repeated measures linear model on a logarithmic scale using the trough predose concentrations of the analyte in plasma immediately before administration of the Nth dose after N-1 doses were administered (Cpre,N). Trough concentrations of Cpre,9, Cpre,11, Cpre,13 and Cpre,14, and the concentrations taken directly at the end of the first and last dosing interval of BI 1358894, were used.
The MAD part planned to include 50 volunteers, which was not based on a power calculation. The size of 10 volunteers per dose group (eight receiving active treatment and two receiving placebo) is commonly used in MAD studies and is considered sufficient for the exploratory evaluation of multiple-dose safety and PK endpoints.
Results
Disposition of Volunteers
Study 1402-0001
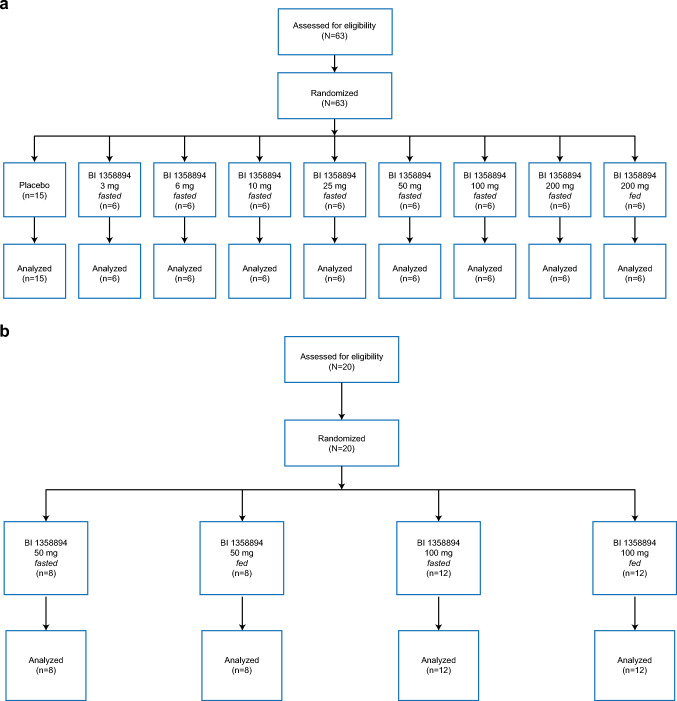
A total of 83 volunteers entered the trial, with 63 volunteers enrolled to the SAD part and 20 volunteers enrolled to the food effect part. All volunteers completed the planned observation time (Fig. 3). For the SAD part (Fig. 3a), the mean (standard deviation [SD]) age was 35.5 (6.7) years, and the mean (SD) BMI was 25.9 (2.72) kg/m2 (Table 1). For the food effect part (Fig. 3b), the mean (SD) age was 33.1 (8.6) years, and the mean (SD) BMI was 25.3 (2.84) kg/m2 (Table 2). The baseline demographic characteristics were generally similar across all treatment groups.
Fig. 3.
Volunteer disposition for study 1402-0001 for (a) the SAD part and (b) the food effect part. SAD single ascending dose
Study 1402-0002
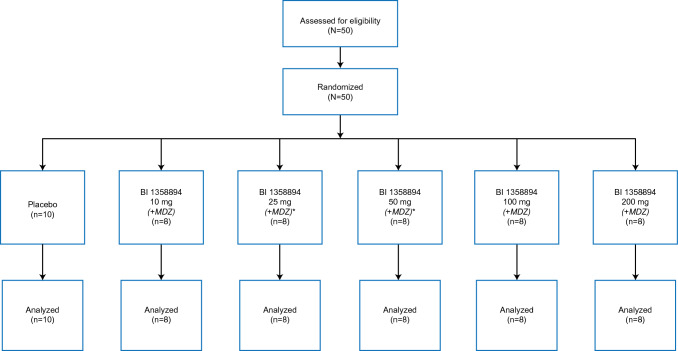
A total of 50 volunteers entered the MAD part and all volunteers completed the observation period, although two volunteers prematurely discontinued trial medication due to an AE (headache and nausea [BI 1358894 25 mg]; ventricular escape rhythm [midazolam prior to BI 1358894 administration]) (Fig. 4). The mean (SD) age was 30.8 (7.2) years and the mean BMI was 24.3 (2.7) kg/m2 (Table 3). The mean (SD) age was slightly lower in the BI 1358894 200 mg group (26.3 [5.1] years) than the other treatment groups (29.3 [1.8] years–32.4 [6.8] years). All other demographic characteristics at baseline were similar across all treatment groups.
Fig. 4.
Volunteer disposition for study 1402-0002. *One volunteer in the 25 mg and one volunteer in the BI 1358894 50 mg dose group prematurely discontinued the trial medication due to an adverse event. MDZ midazolam
Table 3.
Participant demographics and baseline characteristics by treatment group for the multiple ascending doses study
| BI 1358894 | |||||||
|---|---|---|---|---|---|---|---|
| Placebo | 10 mg | 25 mg | 50 mg | 100 mg | 200 mg | Total | |
| [n = 10] | [n = 8] | [n = 8] | [n = 8] | [n = 8] | [n = 8] | [N = 50] | |
| Completed, n | 10 | 8 | 8 | 8 | 8 | 8 | 50 |
| White, n | 10 | 8 | 7 | 8 | 8 | 8 | 49 |
| Black or African American, n | 0 | 0 | 1 | 0 | 0 | 0 | 1 |
| Mean age, years (SD) | 32.1 (9.7) | 32.0 (8.1) | 32.4 (6.8) | 32.3 (7.7) | 29.3 (1.8) | 26.3 (5.1) | 30.8 (7.2) |
| Mean BMI, kg/m2 (SD) | 23.4 (1.9) | 24.8 (2.8) | 26.3 (3.8) | 24.1 (2.3) | 22.6 (1.8) | 25.0 (2.4) | 24.3 (2.7) |
BMI body mass index, SD standard deviation
Safety Profile
Study 1402-0001 Single Ascending Dose (SAD) Part
In the SAD part of the study, a higher proportion of investigator-defined DRAEs were reported in volunteers who received BI 1358894 (21/48 [43.8%]) than in volunteers who received placebo (0/15 [0%]). The most common DRAEs were headache, which occurred in 17/48 (35.4%) volunteers, and dizziness, which occurred in 2/48 (4.2%) volunteers receiving BI 1358894 (Table 4). The frequency of DRAEs in volunteers who received BI 1358894 at doses of >50 mg was generally higher than in the lower dose groups, although no clear dose relationship in the incidence or nature of DRAEs was observed between BI 1358894 dose groups, or between the fed and fasted condition (200 mg dose) [Table 4].
Table 4.
Overall summary of TEAEs and DRAEs following a SAD schedule with BI 1358894 in study 1402-0001
| Placebo | BI 1358894 | Total receiving BI treatment [N = 48] |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| [n = 15] | 3 mg fasted [n = 6] |
6 mg fasted [n = 6] |
10 mg fasted [n = 6] |
25 mg fasted [n = 6] |
50 mg fasted [n = 6] |
100 mg fasted [n = 6] | 200 mg fasted [n = 6] | 200 mg fed [n = 6] |
|||
| Any TEAE [n (%)] | 3 (20.0) | 3 (50.0) | 6 (100.0) | 0 (0) | 2 (33.3) | 4 (66.7) | 4 (66.7) | 3 (50.0) | 6 (100.0) | 28 (58.3) | |
| Any DRAE [n (%)] | 0 (0) | 1 (16.7) | 3 (50.0) | 0 (0) | 2 (33.3) | 4 (66.7) | 4 (66.7) | 3 (50.0) | 4 (66.7) | 21 (43.8) | |
| Nervous system disorders | 0 (0) | 1 (16.7) | 3 (50.0) | 0 (0) | 2 (33.3) | 3 (50.0) | 4 (66.7) | 3 (50.0) | 4 (66.7) | 20 (41.7) | |
| Headache | 0 (0) | 1 (16.7) | 2 (33.3) | 0 (0) | 2 (33.3) | 3 (50.0) | 3 (50.0) | 3 (50.0) | 3 (50.0) | 17 (35.4) | |
| Dizziness | 0 (0) | 0 (0) | 1 (16.7) | 0 (0) | 0 (0) | 1 (16.7) | 0 (0) | 0 (0) | 0 (0) | 2 (4.2) | |
| Disturbance in attention | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (16.7) | 1 (2.1) | |
| Head discomfort | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (16.7) | 0 (0) | 0 (0) | 1 (2.1) | |
| Ear and labyrinth disorders | 0 (0) | 0 (0) | 1 (16.7) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (2.1) | |
| Auditory disorder | 0 (0) | 0 (0) | 1 (16.7) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (2.1) | |
| General disorders and administrative site conditions | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (16.7) | 0 (0) | 0 (0) | 1 (2.1) | |
| Fatigue | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (16.7) | 0 (0) | 0 (0) | 1 (2.1) | |
| Musculoskeletal and connective tissue disorders | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (16.7) | 0 (0) | 0 (0) | 0 (0) | 1 (2.1) | |
| Back pain | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (16.7) | 0 (0) | 0 (0) | 0 (0) | 1 (2.1) | |
No severe AEs, SAEs, deaths, AESI or other significant AEs were recorded
AEs adverse events, AESI adverse events of special interest, DRAEs drug-related adverse events, SAEs severe adverse events, SAD single ascending dose, TEAEs treatment-emergent adverse events
Overall, in the SAD part of the study, the proportion of volunteers experiencing at least one TEAE was higher with BI 1358894 (28/48 [58.3%] volunteers) than placebo (3/15 [20.0%] volunteers) [Table 4]. No AEs of severe intensity, protocol-specified AESIs, SAEs, deaths, or other significant AEs were reported.
There were no clinically relevant findings according to laboratory tests, vital signs, ECGs and VAS, and no concerns related to suicidality were raised as a result of the C-SSRS assessment.
Study 1402-0001 Food Effect Part
In the food effect part of the study, TEAEs were reported in 16/20 (80%) volunteers, and all were reported as DRAEs (Table 5). The most frequently occurring DRAEs were headache (15/20 [75.0%]) and dizziness (7/20 [35.0%]). Skin and subcutaneous tissue DRAEs were reported in 2/20 (10%) volunteers and gastrointestinal DRAEs were reported in 1/20 (5%) volunteers (Table 5). No relevant differences were observed between the BI 1358894 dose groups, or the fed and fasted conditions. No consistent difference in the incidence or nature of investigator-defined DRAEs were observed between the BI 1358894 dose groups, or between the fed and fasted condition (Table 5).
Table 5.
Overall summary of TEAEs and DRAEs following a SAD schedule with BI 1358894 in study 1402-0001 (food effect part)
| BI 1358894 | Total receiving BI treatment [N = 20] |
|||||
|---|---|---|---|---|---|---|
| 50 mg fed [n = 8] | 50 mg fasted [n = 8] | 100 mg fed [n = 12] | 100 mg fasted [n = 12] | |||
| Any TEAE [n (%)] | 7 (87.5) | 7 (87.5) | 6 (50.0) | 8 (66.7) | 16 (80.0) | |
| Any DRAE [n (%)] | 7 (87.5) | 7 (87.5) | 6 (50.0) | 8 (66.7) | 16 (80.0) | |
| Nervous system disorders | 7 (87.5) | 7 (87.5) | 5 (41.7) | 8 (66.7) | 16 (80.0) | |
| Headache | 6 (75.0) | 7 (75.0) | 4 (33.3) | 7 (58.3) | 15 (75.0) | |
| Dizziness | 2 (25.0) | 3 (37.5) | 2 (16.7) | 3 (25.0) | 7 (35.0) | |
| Disturbance in attention | 0 (0) | 2 (25.0) | 0 (0) | 0 (0) | 2 (10.0) | |
| Head discomfort | 1 (12.5) | 0 (0) | 0 (0) | 0 (0) | 1 (5.0) | |
| General disorders and administration site conditions | 0 (0) | 1 (12.5) | 2 (16.7) | 0 (0) | 3 (15.0) | |
| Fatigue | 0 (0) | 1 (12.5) | 2 (16.7) | 0 (0) | 3 (15.0) | |
| Musculoskeletal and connective tissue disorders | 0 (0) | 0 (0) | 0 (0) | 2 (16.7) | 2 (10.0) | |
| Arthralgia | 0 (0) | 0 (0) | 0 (0) | 1 (8.3) | 1 (5.0) | |
| Back pain | 0 (0) | 0 (0) | 0 (0) | 1 (8.3) | 1 (5.0) | |
| Skin and subcutaneous tissue disorders | 1 (12.5) | 0 (0) | 1 (8.3) | 0 (0) | 2 (10.0) | |
| Acne | 0 (0) | 0 (0) | 1 (8.3) | 0 (0) | 1 (5.0) | |
| Pruritus generalised | 1 (12.5) | 0 (0) | 0 (0) | 0 (0) | 1 (5.0) | |
| Rash macular | 1 (12.5) | 0 (0) | 0 (0) | 0 (0) | 1 (5.0) | |
| Gastrointestinal disorders | 1 (12.5) | 0 (0) | 0 (0) | 0 (0) | 1 (5.0) | |
| Flatulence | 1 (12.5) | 0 (0) | 0 (0) | 0 (0) | 1 (5.0) | |
No severe AEs, SAEs, deaths, AESI or other significant AEs were recorded
AEs adverse events, AESI adverse events of special interest, DRAEs drug-related adverse events, SAEs severe adverse events, SAD single ascending dose, TEAEs treatment-emergent adverse events
No AEs of severe intensity, protocol-specified AESI, SAEs, deaths, or other significant AEs were reported. Evaluation of laboratory tests, vital signs, ECGs and VAS revealed no clinically relevant findings. The C-SSRS assessment revealed no concerns with respect to suicidality. All AEs were resolved or followed up sufficiently by the end of the trial.
Study 1402-0002
Of the 50 volunteers treated with BI 1358894 or placebo (with or without a microdose of midazolam), 32 experienced investigator-defined DRAEs and the proportion was similar between the BI 1358894 (26/40 [65%]) and placebo (+ midazolam: 1/10 [10%]; − midazolam 6/10 [60%]) groups (Table 6). No dose dependence was observed for these DRAEs across the BI 1358894 dose groups. The most frequently reported DRAEs were headache (BI 1358894: 17/40 [42.5%]; placebo + midazolam: 1/10 [10%]; placebo − midazolam: 4/10 [40%]), orthostatic intolerance (BI 1358894: 6/40 [15%]; placebo + midazolam: 1/10 [10%]; placebo—midazolam: 4/10 [40%]), and dizziness (BI 1358894: 5/40 [12.5%]; placebo + midazolam: 0/10 [0%]; placebo—midazolam: 1/10 [10%]) [Table 6].
Table 6.
Summary of volunteers with TEAEs and DRAEs following a multiple dosing schedule with BI 1358894 in study 1402-0002
| + Midazolam (Days 1 and 14)a | − Midazolam (Days 2–13)b | Total BI 1358894 [N = 40] |
Total receiving treatment [N = 50] | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Placebo | BI 1358894 | Placebo | BI 1358894 | |||||||||||||
| [n = 10] | 10 mg [n = 8] |
25 mg [n = 8] |
50 mg [n = 8] |
100 mg [n = 8] |
200 mg [n = 8] |
[n = 10] | 10 mg [n = 8] |
25 mg [n = 8] |
50 mg [n = 8] |
100 mg [n = 8] |
200 mg [n = 8] |
|||||
| Any TEAE [n (%)] | 1 (10.0) | 4 (50.0) | 4 (50.0) | 3 (37.5) | 4 (50.0) | 5 (62.5) | 7 (70.0) | 3 (37.5) | 6 (75.0) | 1 (12.5) | 4 (50.0) | 5 (62.5) | 26 (65.0) | 34 (68.0) | ||
| DRAEs [n (%)] | 1 (10.0) | 4 (50.0) | 4 (50.0) | 3 (37.5) | 4 (50.0) | 5 (62.5) | 6 (60.0) | 2 (25.0) | 5 (62.5) | 1 (12.5) | 4 (50.0) | 5 (62.5) | 26 (65.0) | 32 (64.0) | ||
| Nervous system disorders | 1 (10.0) | 4 (50.0) | 4 (50.0) | 3 (37.5) | 4 (50.0) | 5 (62.5) | 6 (60.0) | 1 (12.5) | 5 (62.5) | 1 (12.5) | 2 (25.0) | 5 (62.5) | 24 (60.0) | 30 (60.0) | ||
| Headachec | 1 (10.0) | 3 (37.5) | 3 (37.5) | 2 (25.0) | 2 (25.0) | 3 (37.5) | 4 (40.0) | 0 (0) | 5 (62.5) | 1 (12.5) | 1 (12.5) | 5 (62.5) | 17 (42.5) | 21 (42.0) | ||
| Orthostatic intolerancec | 1 (10.0) | 1 (12.5) | 1 (12.5) | 1 (12.5) | 0 (0) | 1 (12.5) | 4 (40.0) | 1 (12.5) | 0 (0) | 0 (0) | 1 (12.5) | 1 (12.5) | 6 (15.0) | 11 (22.0) | ||
| Dizzinessc | 0 (0) | 1 (12.5) | 0 (0) | 1 (12.5) | 1 (12.5) | 1 (12.5) | 1 (10.0) | 0 (0) | 0 (0) | 1 (12.5) | 0 (0) | 0 (0) | 5 (12.5) | 6 (12.0) | ||
The AE data reported here are for the 50 volunteers, split by AEs during and after midazolam dosing
a Includes all AEs that occurred between the intake of placebo/BI 1358894 + midazolam until 24 h thereafter
bIncludes all AEs that occurred during the intake of placebo/BI 1358894 plus the 14-day residual effect period, excluding the 24 h after the intake of BI 1358894 + midazolam
cMost frequently reported DRAEs
AE adverse event, DRAEs drug-related adverse events, TEAEs treatment-emergent adverse events
Overall, TEAEs were reported in 34 of the 50 treated volunteers, and similar proportions of volunteers with at least one TEAE were observed in the BI 1358894 (26/40 [65%]) versus the placebo (placebo + midazolam: 1/10 [10%]; placebo—midazolam: 7/10 [70%]) groups (Table 6). Other significant AEs were reported in two volunteers. One volunteer experienced moderate headache and mild nausea, which was assessed by the investigator as possibly drug-related. Another volunteer experienced mild ventricular escape rhythm during midazolam treatment prior to BI 1358894 administration on Day 1. No AEs of severe intensity, protocol-specified AESIs, deaths, or other SAEs were reported.
Laboratory tests and the evaluation of vital signs and ECGs revealed no clinically relevant findings for those receiving BI 1358894. However, a clinically relevant increase in aspartate aminotransferase and increased blood creatine phosphokinase was reported for one volunteer receiving placebo. No clinically relevant findings were observed from the VAS and C-SSRS assessments.
Pharmacokinetics
Study 1402-0001 SAD Part
BI 1358894 exposure in terms of AUC0–∞, AUC0–tz, and Cmax increased in a dose-dependent manner over the entire dose range of 3–200 mg in volunteers who had fasted, but was less than dose proportional, as indicated by slopes and 90% CIs <1 (AUC0–∞ 0.8003 [90% CI 0.6304–0.9703]; AUC0–tz 0.8016 [90% CI 0.6176–0.9856]; Cmax 0.5506 [90% CI 0.3969–0.7044]). However, dose proportionality was observed for AUC0–∞ and AUC0–tz across the dose range of 3–50 mg in fasted volunteers, with slopes [90% CI] for these endpoints being 0.9389 [0.8606–1.0172] and 0.9636 [0.8883–1.0388], respectively. In contrast, Cmax still showed a less than dose-proportional increase, with a slope [90% CI] of 0.6543 [0.5402–0.7685].
In the fasted state, following administration of single doses of 3–200 mg, BI 1358894 reached Cmax within 1–5 h (median time to reach Cmax [tmax]). Variability in plasma concentrations and PK parameters was low to moderate (Table 7). However, in one volunteer in the 100 mg dose group, the Cmax was substantially lower (1.9 nmol/L) than in the other volunteers of the same dose group (range 82.0–485.0 nmol/L) due to an unknown reason (data both with and without the volunteer are presented in Table 7). The median tmax and range for the 50, 100 and 200 mg dose groups in the fasted state were 1.0 (0.5–2.5), 3.0 (1.0–6.0) and 5.0 (1.0–8.0), respectively (Table 7). In comparison, when BI 1358894 was administered as a single 200 mg dose in the fed state, median tmax was reached later at 7 h (Table 7).
Table 7.
PK parameters of BI 1358894 after single-dose administration in study 1402-0001
| BI 1358894 | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 3 mg fasted [n = 6] |
6 mg fasted [n = 6] |
10 mg fasted [n = 6] |
25 mg fasted [n = 6] |
50 mg fasted [n = 6] | 100 mg fasted [n = 6] |
100 mg fasted [n = 5]a |
200 mg fasted [n = 6] |
200 mg fed [n = 6] |
||||||||||
| gMean | gCV % | gMean | gCV % | gMean | gCV % | gMean | gCV % | gMean | gCV % | gMean | gCV % | gMean | gCV % | gMean | gCV % | gMean | gCV % | |
| AUC0–∞ (nmol·h/L) | 341 | 20.7 | 596 | 33.3 | 922 | 20.4 | 2540 | 29.9 | 4470 | 25.5 | 2960 | 1570 | 7640 | 39.1 | 13700 | 45.7 | 33800 | 30.1 |
| AUC0–tz (nmol·h/L) | 288 | 18.5 | 569 | 32.7 | 861 | 17.7 | 2380 | 29.7 | 4170 | 26.2 | 2520 | 2670 | 7120 | 37.9 | 12600 | 42.0 | 32800 | 29.0 |
| Cmax (nmol/L) | 27.6 | 30.0 | 35.9 | 33.8 | 59.7 | 13.4 | 84.2 | 44.2 | 183 | 56.3 | 94.3 | 735 | 206 | 72.8 | 385 | 26.8 | 857 | 22.2 |
| CL/F (mL/min) | 280 | 20.7 | 319 | 33.3 | 344 | 20.4 | 312 | 29.9 | 355 | 25.5 | 1070 | 1570 | 416 | 39.1 | 464 | 45.7 | 188 | 30.1 |
| Vz/F (L) | 991 | 21.7 | 1280 | 31.9 | 1540 | 15.1 | 1410 | 30.7 | 1580 | 28.3 | 4180 | 1150 | 1710 | 33.9 | 2090 | 34.1 | 3050 | 40.3 |
| t½ (h) | 41.0 | 16.5 | 46.2 | 14.7 | 51.6 | 20.1 | 52.2 | 17.0 | 51.2 | 10.3 | 45.0 | 25.5 | 47.4 | 24.4 | 52.1 | 21.3 | 188 | 12.3 |
| tmax (h)b | 2.0 (1.0, 4.0) | 2.5 (1.0, 5.0) | 1.0 (1.0, 3.0) | 5.0 (1.0, 6.0) | 1.0 (0.5, 2.5) | 2.3 (1.0, 6.0) | 3.0 (1.0, 6.0) | 5.0 (1.0, 8.0) | 7.0 (4.0, 8.0) | |||||||||
aOne volunteer was excluded due to substantially lower plasma concentrations
bThe median and range (minimum, maximum) are reported for tmax
AUC0–∞ area under the concentration–time curve of the analyte in plasma over the time interval from time zero extrapolated to infinity, AUC0–tz area under the concentration–time curve of the analyte in plasma over the time interval from time zero to the last quantifiable data point, CL/F apparent clearance of the analyte in plasma after extravascular administration, Cmax maximum measured concentration of the analyte in plasma, gCV geometric coefficient of variation, gMean geometric mean, PK pharmacokinetic, t½ terminal half-life of the analyte in plasma, tmax time from (last) dosing to the maximum measured concentration of the analyte in plasma, VZ/F apparent volume of distribution during the terminal phase after extravascular administration
After reaching the maximum plasma concentrations, the BI 1358894 profiles showed a multicompartmental decline with low plasma concentrations, culminating in a long terminal phase that was associated with a terminal half-life (t½) of 188 h (based on extended PK sampling up to 672 h [Day 29]) for the 200 mg dose group in the fed state (Table 7). PK sampling in the 6–200 mg dose groups in the fasted state was conducted up until 192 h (Day 9) and t½ ranged from 45.0 to 52.2 h. In the 3 mg dose group, PK sampling was performed up to 96 h (Day 5) and demonstrated a t½ of 41 h (Table 7).
Study 1402-0001: Effect of Food on Pharmacokinetics
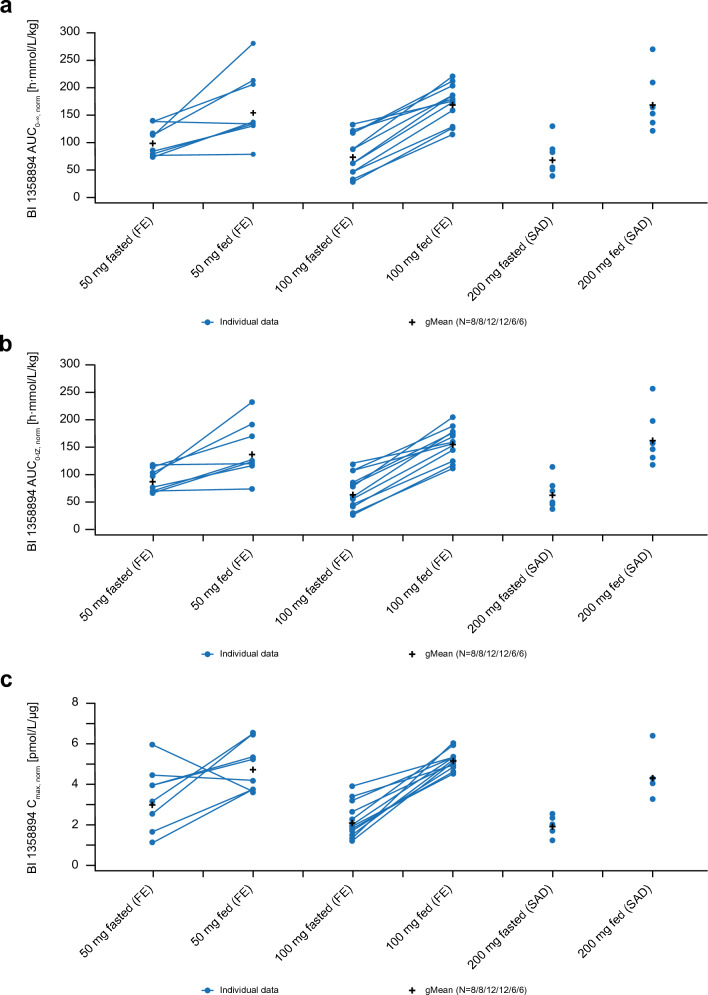
Administration of BI 1358894 after a high-fat, high-calorie breakfast resulted in approximately 1.6-fold higher exposure for BI 1358894 50 mg (gMean ratio: AUC0–∞ 156%; AUC0–tz 156%; Cmax 159%) and approximately 2.5-fold higher exposure for BI 1358894 100 mg (gMean ratio: AUC0–∞ 240%; AUC0–tz 246%; Cmax 246%) than administration in the fasted state (Fig. 5). Analysis of both study parts revealed that AUC0–∞ (Fig. 5a), AUC0–tz (Fig. 5b) and Cmax (Fig. 5c) were dose proportional across the BI 1358894 dose range of 50–200 mg under fed conditions (slopes: AUC0–∞ 1.0745 [90% CI 0.8815–1.2675]; AUC0–tz 1.1237 [90% CI 0.9487–1.2988]; Cmax 0.9396 [90% CI 0.8137–1.0654]).
Fig. 5.
Comparison of individual and normalised geometric means for (a) AUC0–∞, (b) AUC0–tz, and (c) Cmax after administration of BI 1358894 in the fasted and fed state in study 1402-0001 (linear scale). AUC0–∞ area under the concentration–time curve of the analyte in plasma over the time interval from time zero extrapolated to infinity, AUC0–tz area under the concentration–time curve of the analyte in plasma over the time interval from time zero to the last quantifiable data point, Cmax maximum measured concentration of the analyte in plasma, FE food effect, gMean geometric mean, SAD single ascending dose
Study 1402-0002
BI 1358894 exposure (AUC0–24, Cmax, AUCτ,ss, and Cmax,ss) increased dose dependently, but less than dose proportionally, after multiple doses in the fed state across all groups, with slopes ranging from 0.7244 to 0.8000 (AUC0–24 0.8000 [90% CI 0.7472–0.8527]; Cmax 0.7244 [90% CI 0.6599–0.7888]; AUCτ,ss 0.7679 [90% CI 0.7037–0.8321]; Cmax,ss 0.7485 [90% CI 0.6940–0.8030]). Accumulation ratios of BI 1358894 ranged from approximately 1.6 to 1.8 for Cmax and from approximately 2.3 to 2.6 for AUCτ. Median BI 1358894 tmax was 1.5–4 h (Table 8) and steady state was generally attained by Days 9–11, suggesting an effective t½ of approximately 50 h. A multicompartmental disposition with a long, slow terminal phase was observed for BI 1358894; at steady state, terminal t½ ranged from 135 to 361 h (Table 8). Assessment of clinically relevant effects of BI 1358894 on CYP3A activity have been previously reported [12]. Variability in plasma concentrations and PK parameters was low to moderate (Table 8).
Table 8.
Pharmacokinetic parameters of BI 1358894 after multiple dose administration in study 1402-0002
| BI 1358894 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 10 mg [n = 8] | 25 mg [n = 8] | 50 mg [n = 8] | 100 mg [n = 8] | 200 mg [n = 8] | ||||||
| gMean | gCV % | gMean | gCV % | gMean | gCV % | gMean | gCV % | gMean | gCV % | |
| AUC0–24 (nmol·h/L) | 801 | 22.7 | 1570 | 28.0 | 2690 | 17.5 | 5520 | 18.3 | 8200 | 13.3 |
| AUCτ,ss (nmol·h/L) | 2070 | 27.1 | 3520 | 27.8 | 5890 | 35.1 | 12600 | 16.3 | 18900 | 13.5 |
| Cmax (nmol/L) | 78.8 | 16.0 | 152 | 34.7 | 217 | 28.3 | 491 | 17.2 | 634 | 20.8 |
| Cmax,SS (nmol/L) | 138 | 14.5 | 225 | 18.8 | 383 | 26.7 | 843 | 19.8 | 1150 | 13.8 |
| t½,SS (h) | 143 | 87.9 | 173 | 54.6 | 135 | 114 | 155 | 49.2 | 361 | 52.4 |
| RACmax | 1.76 | 15.1 | 1.64 | 22.6 | 1.75 | 23.9 | 1.72 | 14.6 | 1.82 | 23.9 |
| RAAUCτ | 2.58 | 12.3 | 2.44 | 27.6 | 2.38 | 16.3 | 2.28 | 14.9 | 2.31 | 16.4 |
| tmax (h)a | 1.5 (1.0, 4.0) | 3.0 (2.0, 6.0) | 4.0 (2.0, 6.00) | 2.0 (1.0, 6.0) | 4.0 (0.5, 6.0) | |||||
| tmax,SS (h)a | 2.0 (1.0, 6.0) | 3.0 (1.0, 4.0) | 3.0 (1.0, 4.0) | 3.0 (1.0, 6.0) | 3.5 (0.5, 4.0) | |||||
aThe median and range (minimum, maximum) are reported for tmax
AUC0–24 area under the concentration–time curve of the analyte in plasma over the time interval from time zero to 24 h, AUCτ,ss area under the concentration–time curve of the analyte in plasma at steady state over a uniform dosing interval τ, Cmax maximum measured concentration of the analyte in plasma, Cmax,SS maximum measured concentration of the analyte in plasma at steady state, gCV geometric coefficient of variation, gMean geometric mean, RACmax accumulation ratio according to Cmax, RAAUC accumulation ratio according to AUCτ, t½ terminal half-life of the analyte in plasma, tmax time from (last) dosing to the maximum measured concentration of the analyte in plasma
Discussion
The two first-in-human phase I clinical studies described here evaluated the safety and PK profiles of oral BI 1358894 in healthy volunteers. This included assessing the effect of food on BI 1358894 exposure and safety.
Single and multiple doses of BI 1358894 were generally well tolerated in the healthy male volunteers included in this study. No dose dependency in terms of DRAE frequency was observed across the SAD and MAD schedules, and no differences were observed in the safety profile of BI 1358894 under fed and fasted conditions. While 75% and 35% of volunteers reported headaches and dizziness, respectively, as DRAEs in the food effect part, these AEs were resolved at the end of the trial. Overall, these studies demonstrated BI 1358894 to have a favourable safety profile in healthy volunteers at doses of ≤ 200 mg.
At all tested doses across both SAD and MAD schedules, BI 1358894 exposure increased in a dose-dependent manner. A positive food effect was observed in the SAD and food effect study, whereby consumption of a high-fat, high-calorie breakfast prior to BI 1358894 administration increased exposure compared with the fasted state. Dose proportionality was observed in the fed state for PK parameters across the dose range of 50–200 mg, and in the fasted state for AUC0–∞ and AUC0–tz across the dose range of 3–50 mg (SAD and food effect study). The higher exposure observed after a high-calorie, high-fat meal is likely related to better gastrointestinal bioavailability and is not related to differences in the metabolism or elimination of BI 1358894, as the terminal rate constant and terminal t½ were comparable and decline in plasma concentrations across doses occurred in parallel. Based on these results, a predictable increase in systemic exposure of BI 1358894 can be expected when administered as a single or multiple dose under fasted or fed conditions.
During the SAD study, BI 1358894 200 mg administered under fed conditions exhibited a terminal t½ of 188 h, with very low and slow declining plasma concentrations (based on extended PK sampling up to 672 h). This contrasts with the MAD study in which steady state occurred between 9 and 11 days, and thus an effective t½ of approximately 50 h would be expected, as observed for the BI 1358894 6–200 mg SAD dose groups (t½ 45–52.2 h; PK sampling up to 192 h; fasted state). It should be noted that determination of terminal t½ was dependent on the sampling duration and that the late phase may not have solely represented elimination; therefore, the effective t½ of approximately 50 h may be more clinically relevant than the terminal t½ determined after very long sampling, as suggested for drugs with multicompartment kinetics [14]. This is because, unlike the terminal t½ calculated using the slope of the last drug elimination phase following single-dose administration, the effective t½ considers the entire concentration–time profile of a drug, drug dosing interval, and drug accumulation over time after multiple dose administration [14]. Thus, the effective t½ is less likely to be affected by sampling duration when compared with the terminal t½ [14]. As such, these results should be interpreted with caution; however, it should be noted that to determine terminal t½, the percentage of AUC extrapolation for the sampling period until 192 h and beyond the last measurable time point to infinity was <20%.
An additional objective of the MAD study was to evaluate the effect of BI 1358894 on the PK of the sensitive CYP3A substrate midazolam over the entire dose range of 10–200 mg. These results have been previously reported by Wiebe et al. and suggest no clinically relevant effect of BI 1358894 on CYP3A activity [12, 13].
Some limitations of this study should be considered. As this was a phase I trial in healthy volunteers, the translatability of the data to patients may be limited. The sample size of each treatment group was small and, as such, these findings will require confirmation in larger trials in the future.
Conclusions
Overall, SAD and MAD schedules of BI 1358894 were well tolerated at doses up to 200 mg, with no dose dependency observed in DRAE frequency. The PK of BI 1358894 after single and multiple dosing is associated with low to moderate variability. The PK results of the SAD study demonstrated dose dependence and proportionality in terms of exposure to BI 1358894 in the fed state. In the MAD study, steady state was attained after 9–11 days, suggesting an effective t½ of approximately 50 h, which is in line with the terminal t½ determined in the SAD study. The longer observed terminal t½ of the 200 mg dose in the fed state (SAD study) is likely related to the extended sampling duration. BI 1358894 exposure following MAD increased less than dose proportionally across 10–200 mg doses. No clinically relevant effect of BI 1358894 on CYP3A activity was observed. Taken together, these findings provide a basis for further clinical studies of BI 1358894 in patients with MDD.
Acknowledgements
Editorial support (in the form of writing assistance, assembling figures, collating author comments, grammatical editing and referencing) was provided by Katie Baker and Lieve Desbonnet, PhD, of Fishawack Communications Ltd, UK, and was funded by Boehringer Ingelheim International GmbH.
Declarations
Funding
This study was funded by Boehringer Ingelheim (BI study numbers NCT03210272/1402-0001 and NCT03754959/1402-0002). The funders of the study had a role in the study design, data analysis, data interpretation, and writing of the report.
Conflicts of interest
René Fuertig, Markus Goettel, and Sabrina T. Wiebe are employees of Boehringer Ingelheim Pharma GmbH & Co. KG. Lena Herich and Josef Hoefler are employees of Staburo GmbH, München, Germany, on behalf of Boehringer Ingelheim Pharma GmbH & Co. KG. Vikas Sharma is an employee of Boehringer Ingelheim International GmbH. The authors did not receive any direct compensation relating to the development of this manuscript.
Availability of data and material
To ensure independent interpretation of the clinical study results, Boehringer Ingelheim grants all external authors access to all relevant material, including participant-level clinical study data, and relevant material as needed by them to fulfil their role and obligations as authors under the International Committee of Medical Journal Editors (ICMJE) criteria. Furthermore, clinical study documents (e.g. study report, study protocol, statistical analysis plan) and participant clinical study data are available to be shared after publication of the primary manuscript in a peer-reviewed journal and if regulatory activities are complete and other criteria are met per the BI Policy on Transparency and Publication of Clinical Study Data (https://trials.boehringer-ingelheim.com/). Prior to providing access, documents will be examined, and, if necessary, redacted and the data will be de-identified, to protect the personal data of study participants and personnel and to respect the boundaries of the informed consent of the study participants. Clinical study reports and related clinical documents can also be requested via the link https://trials.boehringer-ingelheim.com/. All requests will be governed by a Document Sharing Agreement. Bona fide, qualified scientific and medical researchers may request access to de-identified, analysable participant clinical study data with corresponding documentation describing the structure and content of the datasets. Upon approval, and governed by a Data Sharing Agreement, data are shared in a secured data-access system for a limited period of 1 year, which may be extended upon request. Researchers should use the https://trials.boehringer-ingelheim.com/ link to request access to study data.
Ethics approval
The trial was carried out in compliance with the clinical trial protocol and approved by an independent ethics committee (Ethics Committee of the Medical Association in Baden-Wuerttemberg [Ethikkomission der Landesaerztekammer], Stuttgart-Vaihingen, Germany) and conducted in accordance with the principles of the 1964 Declaration of Helsinki.
Consent to participate
Each volunteer signed and dated an informed consent form according to the local regulatory and legal requirements and Good Clinical Practices.
Consent for publication
Not applicable.
Code availability
Not applicable.
Author contributions
RF, MG, STW, and VS contributed to the study concept and design. MG, STW, RF, JH, and LH were responsible for data analyses and interpretation. MG was involved in the acquisition of study data. All authors contributed towards the preparation of the manuscript, approved the final submitted version, and agreed to be listed as authors.
References
- 1.Tolentino JC, Schmidt SL. DSM-5 criteria and depression severity: implications for clinical practice. Front Psychiatry. 2018;9:450. doi: 10.3389/fpsyt.2018.00450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GBD 2019 Mental Disorders Collaborators Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9:137–150. doi: 10.1016/S2215-0366(21)00395-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cowen PJ. Backing into the future: pharmacological approaches to the management of resistant depression. Psychol Med. 2017;47:2569–2577. doi: 10.1017/s003329171700068x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Davies P, Ijaz S, Williams CJ, Kessler D, Lewis G, Wiles N. Pharmacological interventions for treatment-resistant depression in adults. Cochrane Database Syst Rev. 2019;12:10557. doi: 10.1002/14651858.CD010557.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dupuy JM, Ostacher MJ, Huffman J, Perlis RH, Nierenberg AA. A critical review of pharmacotherapy for major depressive disorder. Int J Neuropsychopharmacol. 2011;14:1417–1431. doi: 10.1017/s1461145711000083. [DOI] [PubMed] [Google Scholar]
- 6.Mandell D, Siegle GJ, Shutt L, Feldmiller J, Thase ME. Neural substrates of trait ruminations in depression. J Abnorm Psychol. 2014;123:35–48. doi: 10.1037/a0035834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fowler MA, Sidiropoulou K, Ozkan ED, Phillips CW, Cooper DC. Corticolimbic expression of TRPC4 and TRPC5 channels in the rodent brain. PLoS ONE. 2007;2:e573. doi: 10.1371/journal.pone.0000573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Riccio A, Li Y, Moon J, Kim KS, Smith KS, Rudolph U, et al. Essential role for TRPC5 in amygdala function and fear-related behavior. Cell. 2009;137:761–772. doi: 10.1016/j.cell.2009.03.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Riccio A, Li Y, Tsvetkov E, Gapon S, Yao GL, Smith KS, et al. Decreased anxiety-like behavior and Galphaq/11-dependent responses in the amygdala of mice lacking TRPC4 channels. J Neurosci. 2014;34:3653–3667. doi: 10.1523/jneurosci.2274-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kavuran Buran İ, OnalanEtem E, Tektemur A. Inhibition of TRPC1, TRPM4 and CHRNA6 ion channels ameliorates depression-like behavior in rats. Behav Brain Res. 2022;423:113765. doi: 10.1016/j.bbr.2022.113765. [DOI] [PubMed] [Google Scholar]
- 11.Just S, Chenard BL, Ceci A, Strassmaier T, Chong JA, Blair NT, et al. Treatment with HC-070, a potent inhibitor of TRPC4 and TRPC5, leads to anxiolytic and antidepressant effects in mice. PLoS ONE. 2018;13:e0191225. doi: 10.1371/journal.pone.0191225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wiebe ST, Huennemeyer A, Kadus W, Goettel M, Jambrecina A, Schultz A, et al. Midazolam microdosing applied in early clinical development for drug-drug interaction assessment. Br J Clin Pharmacol. 2021;887(1):178–188. doi: 10.1111/bcp.14389. [DOI] [PubMed] [Google Scholar]
- 13.Goettel M, Fuertig R, Wiebe S, Herich L, Sharma V. P.447 Multiple rising doses of oral BI 1358894 in healthy male volunteers: a phase I study investigating safety, tolerability and pharmacokinetics. Eur Neuropsychopharmacol. 2020;40:254–255. doi: 10.1016/j.euroneuro.2020.09.330. [DOI] [Google Scholar]
- 14.Gidal BE, Clark AM, Anders B, Gilliam F. The application of half-life in clinical decision making: Comparison of the pharmacokinetics of extended-release topiramate (USL255) and immediate-release topiramate. Epilepsy Res. 2017;129:26–32. doi: 10.1016/j.eplepsyres.2016.10.020. [DOI] [PubMed] [Google Scholar]