Abstract
Rationale
Social isolation and loneliness are gaining recognition for their role in health outcomes, yet they have not been defined in people with chronic obstructive pulmonary disease (COPD).
Objective
To determine the national prevalence of and characteristics associated with social isolation and loneliness in people with COPD.
Methods
This is a cross-sectional study of community-dwelling adults aged ⩾50 years in the nationally representative HRS (Health and Retirement Study) (2016–2018). Participants self-reported COPD and supplemental oxygen use and were categorized into three groups: 1) no COPD; 2) COPD; and 3) COPD on oxygen. Social isolation was defined using a nine-item scale indicating minimal household contacts, social network interaction, and community engagement. Loneliness was measured using the 3-Item UCLA Loneliness Scale. Multivariable logistic regression defined prevalence and associated characteristics for both.
Results
Participants (n = 10,384) were on average 68 years old (standard deviation, ±10.5), 54% female, 10% Black, 11% self-reported COPD, and 2% self-reported supplemental oxygen. Overall, 12% were socially isolated, 12% lonely, and 3% both socially isolated and lonely. People with COPD had a higher adjusted prevalence of social isolation (no COPD: 11%; COPD: 16%; COPD on oxygen: 20%; P < 0.05) and loneliness (no COPD: 11%; COPD: 18%; COPD on oxygen: 22%; P < 0.001). In those with COPD, characteristics associated with social isolation (P < 0.05) included sex (men: 22%; women: 13%), non-Hispanic White ethnicity (White: 19%; Black: 7%), low net worth (<$6,000: 32%; $81,001–$239,000: 10%), depression (depression: 24%; no depression: 14%), having difficulty with one or more activities of daily living (one or more difficulty: 22%; no difficulty: 14%), and current cigarette use (current: 24%; never: 13%). Characteristics associated with loneliness (P < 0.05) included younger age (50–64 yr: 22%; 75–84 yr: 12%), being single (single: 32%; married: 12%), depression (depression: 36%; no depression: 13%), having difficulty with one or more activities of daily living (one or more difficulty: 29%; no difficulty: 15%), diabetes (diabetes: 26%; no diabetes: 17%), and heart disease (heart disease 23%; no heart disease: 17%).
Conclusions
Nearly one in six adults with COPD experience social isolation, and one in five experience loneliness, with almost twice the prevalence among those on supplemental oxygen compared with the general population. Demographic and clinical characteristics identify those at highest risk to guide clinical and policy interventions.
Keywords: social determinants of health, respiratory insufficiency, social support, social environment
Chronic obstructive pulmonary disease (COPD) disproportionately affects older individuals and is the third leading cause of death worldwide (1). Social determinants of health play an important role in COPD disease outcomes, health-related quality of life, and healthcare use (2). Social isolation and loneliness are key social determinants of health that are gaining increasing recognition and are linked to poor health outcomes, including increased incidence of cardiovascular disease and stroke, poor disease control, worse functional impairment, poor outcomes after intensive care unit (ICU) admissions, and mortality (3–7). Social isolation is defined as an objective deficit in the number and frequency of contacts with family, friends, and community, whereas loneliness is the subjective emotional distress that arises from the feeling that one’s social life is inadequate. To date, little is known about the epidemiology of these key markers of social well-being among persons with COPD. Notably, prior studies suggest there is a low correlation between loneliness and social isolation (r < 0.20), but the correlation among persons with COPD has not been investigated (8).
Individuals with COPD may be uniquely vulnerable to experiencing social isolation and loneliness and their downstream health consequences (9). People with COPD may be more objectively isolated and lonely because of a high burden of symptoms, such as fatigue, dyspnea, and depression, as well as disease-related functional limitations (10). In particular, supportive therapies, such as supplemental oxygen, may be stigmatizing and lead to social withdrawal, shame, physical inadequacy, and loneliness (8, 11).
It is therefore imperative for clinicians, researchers, and policymakers to understand the magnitude of loneliness and social isolation in COPD. In this study, we used the nationally representative HRS (Health and Retirement Study), which includes a comprehensive description of the health and social lives of older adults. We had two primary objectives: 1) to compare the adjusted prevalence of social isolation and loneliness in adults aged ⩾50 years between those with and without COPD, including those on supplemental oxygen; and 2) to identify characteristics associated with social isolation and loneliness among those with COPD. We hypothesized that adults with COPD, and particularly those with COPD on supplemental oxygen, were more likely to experience social isolation and loneliness than the general population of U.S. adults. Some of the results of this study have been previously reported in the form of an abstract (12, 13).
Methods
Study Sample
This study uses the HRS, a nationally representative survey of American adults aged ⩾50 years conducted biennially until death. A psychosocial leave-behind questionnaire (LBQ) that measures loneliness and social isolation is administered to alternating halves of the HRS cohort every 2 years (response rate, 90%) (14). Among the 12,029 participants from the 2016 and 2018 HRS waves with at least one response to the LBQ, we excluded 1,645 participants because of incomplete information on social isolation, loneliness, or other key covariates, yielding a final sample of 10,384 participants. This study was approved by the Institutional Review Board at the University of Michigan and University of California, San Francisco.
Exposure
Subjects self-reported COPD with the question “Has a doctor ever told you that you have chronic lung disease, such as chronic bronchitis or emphysema?” as has been done in prior studies (15). The prevalence of COPD in our study was consistent with national prevalence data using alternative strategies to identify COPD (16). Self-reported supplemental oxygen use was identified with the question “Are you receiving oxygen for your lung condition?” We categorized participants into three groups: 1) no COPD; 2) COPD; and 3) COPD on oxygen. There were no participants without COPD who reported supplemental oxygen use.
Outcomes: Social Isolation and Loneliness
We defined social isolation using a previously published scale used to study older adults with serious illness (17). This social isolation scale includes three subscales (each scored 0–2) based on the three dimensions of social isolation strongly associated with health outcomes: 1) household and core contacts; 2) social network interaction; and 3) community engagement. First, household and core contacts included marital status, household size, and having nearby children (<10 miles). People who live alone or are single are less likely to have access to a daily caregiver and are at higher risk of mortality and prolonged nursing home stays after hospitalizations (18). Second, we measured social network interaction, which assesses the frequency of contact with children, family, or friends through in-person, e-mail, or phone communication. Social network interaction reflects the web of connections between relationships and a pathway to the provision of material and psychosocial support; this domain has been tied strongly to healthcare use in prior studies (3, 5). Third, we assessed community engagement with participation in religious services, other community groups, or volunteering. Community engagement can indicate the level of integration with one’s local community and the ability to access local resources of support; it is associated with reduced depression, functional decline, and mortality (19, 20). When combined, the three subscales create an overall social isolation score (range, 0–6) where <3 points identified social isolation.
We defined loneliness using the widely used UCLA 3-Item Loneliness Scale which comprises three questions assessing the frequency with which participants feel they lack companionship, are left out, or are isolated from others (responses: “hardly ever” [0 points], “some of the time” [1 point], and “often” [2 points]; overall range, 0–6 points). We used previously defined cut-offs, including “occasional loneliness” (⩾1 point), and “frequent loneliness” (⩾4 points), which corresponds with at least one answer of “often.” (21) Although even “occasional” loneliness is associated with poor health outcomes, we primarily focused on “frequent” loneliness for this study to identify those at the highest need of intervention (22).
Covariates
Sociodemographic and health information included age, sex, education level, race and ethnicity, net worth, and self-reported comorbidities (diabetes, cancer, stroke, and heart disease). We determined the presence of depressive symptoms using a modified center for epidemiologic studies depression scale (CES-D) (8 items with yes or no answers, scale 0–8, where ⩾4 indicates clinically relevant depression) (23, 24).
Statistical Analysis
We first compared the national prevalence of social isolation and loneliness among the three groups based on COPD status using Rao-Scott chi-square tests. We then used logistic regression to determine the adjusted national prevalence of social isolation and loneliness for each of the three groups. We selected clinically meaningful sociodemographic factors a priori, including age, sex, race and ethnicity, marital status, and net worth, which are known to impact social isolation and loneliness (22, 25, 26). We removed marital status in the social isolation analysis, as it is included in the social isolation scale. We did not adjust for comorbidities or functional status, as we conceptualized that these factors were on the causal pathway between COPD and social isolation and loneliness (27). Given the importance of each of the social isolation subscales to health outcomes as described above, we used Rao-Scott chi-square tests to examine the prevalence of each social isolation subscale by COPD status.
We next used logistic regression within the subpopulation of participants with COPD to identify sociodemographic and health characteristics (after adjusting for age, sex, race and ethnicity, and net worth) associated with social isolation and loneliness. We adjusted for marital status in loneliness models but not in social isolation models, as marital status is included in the social isolation scale. We did not adjust for multiple comparisons, as the goal of the analysis was exploratory in nature (28). For all analyses, we applied survey weights provided by the HRS to adjust for the complex survey design and nonresponse to the core interview and LBQ (29). We performed statistical analysis using STATA v.16.1 (30).
Results
National Prevalence Estimates of Social Isolation and Loneliness
Demographics, health characteristics, and unadjusted national prevalence estimates of social isolation, loneliness, or both in our sample are summarized in Table 1. Of the 10,384 participants, the mean age was 67.9 (±10.5) years old. Overall, 54% were female, 10% were African American/Black, and 66% were married/partnered, with 1,100 (11%) having COPD (909 [9%] had COPD, and 191 [2%] had COPD on supplemental oxygen). Those with COPD had a higher unadjusted prevalence of social isolation (no COPD: 11%; COPD: 19%; COPD on oxygen: 26%; P < 0.001) and frequent loneliness (no COPD: 10%; COPD: 22%; COPD on oxygen: 29%; P < 0.001).
Table 1.
Baseline characteristics in 2016–2018 Health and Retirement Study (N = 10,384)
| No COPD | COPD without Oxygen | COPD with Oxygen | Overall | P Value | |
|---|---|---|---|---|---|
| Total | 9,284 (89.4) | 909 (8.8) | 191 (1.9) | 10,384 | |
| Age, yr | |||||
| 50–64 | 3,997 (53.8) | 340 (46.3) | 52 (35.4) | 4,389 (52.8) | <0.001 |
| 65–74 | 2,528 (28.2) | 254 (31.1) | 48 (24.7) | 2,830 (28.4) | |
| 75–84 | 2,071 (13.1) | 254 (16.7) | 80 (29.7) | 2,405 (13.6) | |
| 85–102 | 623 (5.0) | 63 (5.8) | 14 (10.2) | 700 (5.1) | |
| Mean (SD) | 67.7 (±10.5) | 69.1 (±10.4) | 71.7 (±10.0) | 67.9 (±10.5) | |
| Sex | |||||
| Male | 3,764 (47.1) | 324 (40.9) | 69 (36.1) | 4,157 (46.4) | 0.006 |
| Female | 5,407 (52.9) | 577 (59.1) | 122 (63.9) | 6,106 (53.6) | |
| Race and ethnicity | |||||
| White | 6,029 (75.8) | 634 (78.1) | 127 (71.9) | 6,790 (76.0) | 0.261 |
| African American/Black | 1,602 (10.0) | 162 (10.3) | 35 (11.6) | 1,799 (10.0) | |
| Hispanic/Latino | 1,171 (9.8) | 64 (6.3) | 19 (10.0) | 1,254 (9.5) | |
| Another race | 369 (4.5) | 41 (5.3) | 10 (6.5) | 420 (4.6) | |
| Education | |||||
| ⩽High school education | 1,534 (13.9) | 266 (27.2) | 70 (35.5) | 1,870 (15.3) | <0.001 |
| >High school education | 7,637 (86.1) | 635 (72.8) | 121 (64.5) | 8,393 (84.7) | |
| Marital status | |||||
| Married or partnered | 5,843 (67.4) | 459 (53.0) | 88 (41.0) | 6,390 (65.7) | <0.001 |
| Net worth,* in dollars | |||||
| <6,000 | 1,414 (13.1) | 266 (28.1) | 65 (39,5) | 1,745 (14.8) | <0.001 |
| 6,000 to <81,000 | 1,614 (16.0) | 188 (21.5) | 43 (22.0) | 1,845 (16.5) | |
| 81,000 to <239,000 | 1,941 (20.2) | 176 (20.4) | 42 (18.0) | 2,159 (10.2) | |
| >239,000 | 4,202 (50.7) | 271 (30.0) | 41 (20.5) | 4,514 (48.5) | |
| Tobacco cigarette use | |||||
| Never | 4,497 (48.8) | 208 (21.1) | 28 (17.3) | 4,733 (46.0) | <0.001 |
| Former | 3,763 (40.9) | 453 (46.8) | 119 (58.2) | 4,335 (41.7) | |
| Current | 924 (10.3) | 248 (32.1) | 46 (24.6) | 1,218 (12.4) | |
| Comorbidities† | |||||
| Cancer | 1,446 (14.3) | 199 (19.1) | 43 (22.1) | 1,688 (14.8) | 0.003 |
| Diabetes | 2,407 (23.3) | 287 (29.5) | 77 (42.6) | 2,771 (24.1) | <0.001 |
| Stroke | 668 (6.1) | 119 (12.1) | 40 (24.1) | 827 (6.9) | <0.001 |
| Heart disease | 2,108 (20.8) | 373 (40.1) | 104 (53.1) | 2,585 (22.9) | <0.001 |
| High depressive symptoms | 1,033 (11.0) | 236 (27.1) | 72 (43.0) | 1,341 (12.8) | <0.001 |
| Social Isolation | |||||
| Socially isolated‡ | 931 (11.1) | 163 (18.9) | 36 (25.9) | 1,130 (12.0) | <0.001 |
| Household and core contacts§ | |||||
| None | 1,135 (12.7) | 141 (16.5) | 26 (17.5) | 1,302 (13.1) | <0.001 |
| Low | 1,403 (13.4) | 199 (19.3) | 40 (22.8) | 1,642 (14.0) | |
| Moderate/high | 6,633 (73.9) | 561 (64.2) | 125 (59.7) | 7,319 (72.9) | |
| Social network interactionǁ | |||||
| None | 1495 (17.4) | 192 (22.2) | 42 (24.9) | 1,729 (17.9) | 0.004 |
| Low | 3532 (38.6) | 330 (37.7) | 78 (43.1) | 3,940 (38.6) | |
| Moderate/high | 4144 (44.0) | 379 (40.1) | 71 (32.0) | 4,594 (43.5) | |
| Community engagement¶ | |||||
| None | 1508 (17.5) | 249 (30.5) | 58 (35.2) | 1,815 (18.9) | <0.001 |
| Low | 1197 (13.8) | 126 (15.4) | 32 (14.4) | 1,355 (14.0) | |
| Moderate/high | 6466 (68.7) | 526 (54.1) | 101 (50.4) | 7,093 (67.2) | |
| Loneliness** | |||||
| Occasional loneliness (1–3 points) | 4269 (47.6) | 428 (46.5) | 102 (48.7) | 4,799 (47.5) | <0.001 |
| Frequent loneliness (4–6 points) | 944 (10.2) | 171 (21.7) | 48 (29.1) | 1,163 (11.5) | <0.001 |
| Both social isolation and loneliness | 207 (2.6) | 56 (7.3) | 17 (14.7) | 280 (3.1) | <0.001 |
Definition of abbreviations: COPD = chronic obstructive pulmonary disease; SD = standard deviation.
Data are presented as n (%) unless otherwise noted. Percentages in the table are adjusted for survey weights and thus may not correspond directly to the unadjusted number listed in each cell.
Net worth was calculated as the sum of all assets minus the sum of all debts.
Comorbidities were self-reported.
Overall social isolation was defined by the summary score 0–6 of household, social network interaction, and community engagement subscales, each ranging from 0 to 2 points. Social isolation was defined with 0–2 points.
Household contact items included marital status, household size, and presence of children <10 miles away.
Social network interaction items included the frequency of interaction with children, family, and friends through in-person, e-mail, or phone.
Community engagement items included volunteering, participating in community groups, and religious services.
Loneliness was defined using the UCLA 3-Item Loneliness Scale (range, 0–6 points).
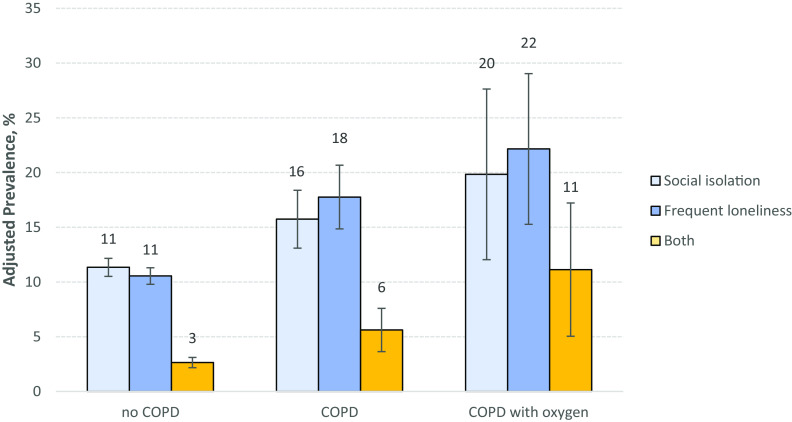
After multivariable adjustment, both prevalence estimates remained significant (Figure 1): participants with COPD had a higher adjusted prevalence of social isolation (no COPD: 11%; COPD: 16%; COPD with oxygen: 20%; P < 0.001) and frequent loneliness (no COPD: 11%; COPD: 18%; COPD with oxygen: 22%; P < 0.001) (Figure 1). In addition, persons with COPD reported higher prevalence of both social isolation and frequent loneliness (no COPD: 3%; COPD: 6%; COPD with oxygen: 11%; P < 0.001), although the correlation between social isolation and loneliness among persons with COPD was low (r = 0.19).
Figure 1.
The adjusted prevalence of social isolation, frequent loneliness, and both social isolation and frequent loneliness by chronic obstructive pulmonary disease (COPD) status. Rates represent the model-based probabilities adjusted for age, sex, race and ethnicity, marital status, and net worth. Error bars represent the 95% confidence intervals. All displayed comparisons reached a significance threshold of P < 0.05. P values represent the overall association across COPD groups with social isolation, loneliness, or both in multiple logistic regression models using joint Wald tests. Social isolation was defined with a score ⩽2. Frequent loneliness is defined using the validated 3-Item UCLA Loneliness Scale, where a score of ⩾4 indicates frequent loneliness. COPD and oxygen use are self-reported.
Social Isolation Subscales
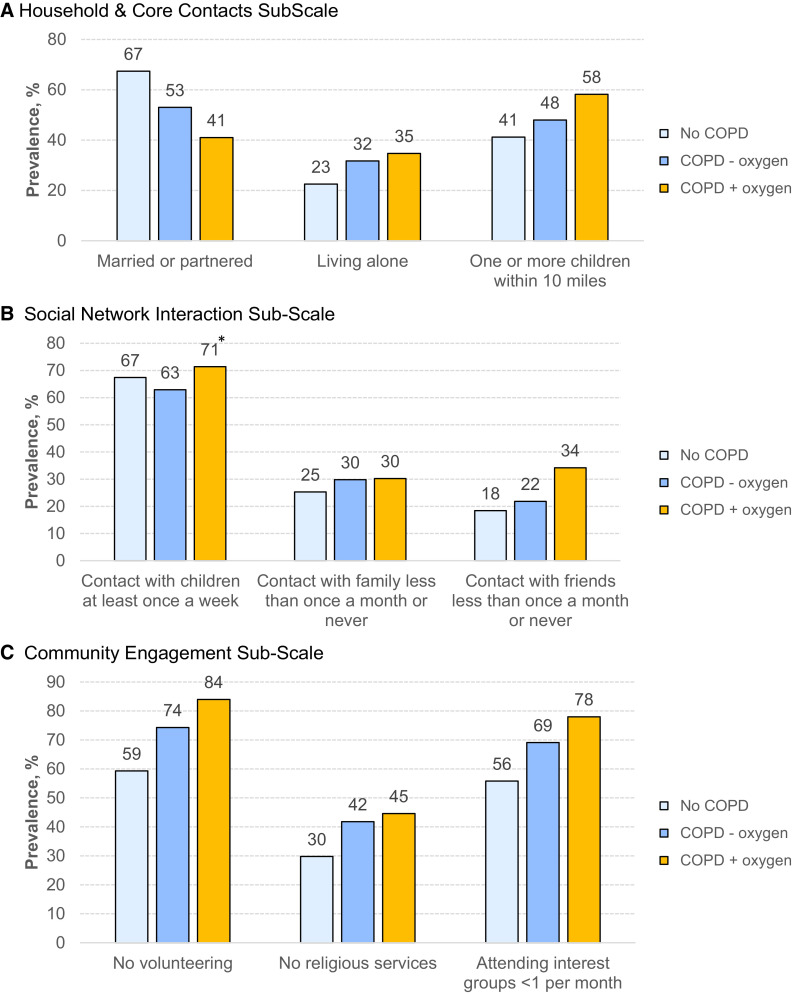
We next examined the social isolation subscales (Figure 2A). Participants with COPD and those with COPD on supplemental oxygen were more likely to be single (no COPD: 33%; COPD: 47%; COPD on oxygen: 59%; P < 0.001), live alone (no COPD: 23%; COPD: 32%; COPD on oxygen: 35%; P < 0.001), and have minimal interaction with nonchildren family (no COPD: 25%; COPD: 30%; COPD on oxygen: 30%; P = 0.02) and friends (no COPD: 18%; COPD: 22%; COPD on oxygen: 34%; P < 0.001). Persons with COPD were more likely to report no volunteer work in the last 12 months (no COPD: 59%; COPD: 74%; COPD on oxygen: 84%; P < 0.001), no religious service attendance in the last 12 months (no COPD: 30%; COPD: 42%; COPD on oxygen: 45%; P < 0.001), and less than monthly participation in community groups (no COPD: 56%; COPD: 69%; COPD on oxygen: 78%; P < 0.001). However, persons with COPD were more likely to live near their children (no COPD: 41%; COPD: 48%; COPD on oxygen: 58%; P < 0.001). Social interaction subscales are summarized in Table E1 in the data supplement.
Figure 2.
The distribution of social isolation subscales by COPD status. (A) Household and core contacts subscale. (B) Social network interaction subscale. (C) Community engagement subscale. Unless noted with an asterisk, all displayed comparisons reached a significance threshold of P < 0.05. COPD = chronic obstructive pulmonary disease.
Clinical Characteristics Associated with Social Isolation and Loneliness
Within the sample of persons with COPD (n = 1,100), characteristics associated with social isolation after adjustment included male sex (men: 22%; women: 13%; P < 0.001), self-reported non-Hispanic White ethnicity (White: 19%; Latinx: 15%; Black: 7%; P < 0.001), low net worth (<$6,000: 32%; $6,001–$81,000: 28%; $81,001–$239,000: 10%; >$239,000: 12%; P < 0.001), depression (depression: 24%; no depression: 14%; P = 0.005), having difficulty with one or more activities of daily living (ADLs) (one or more difficulty: 22%; no difficulty: 14%; P = 0.033), and current cigarette use (current: 24%; former: 14%; never: 13%; P = 0.01) (Figure 3A). Characteristics independently associated with frequent loneliness in participants with COPD after adjustment included younger age (50–64 yr: 22%; 65–74 yr: 19%; 75–84 yr: 12%, 85–102 yr: 10%; P < 0.005), being single (single: 32%; married: 13%; P < 0.001), depression (depression: 36%; no depression: 13%; P < 0.001), having difficulty with one or more ADL (one or more difficulty: 29%; no difficulty: 15%; P = 0.001), and having diabetes (diabetes: 26%; no diabetes: 17%; P = 0.012) and heart disease (heart disease: 23%; no heart disease: 17%; P = 0.023) (Figure 3B).
Figure 3.
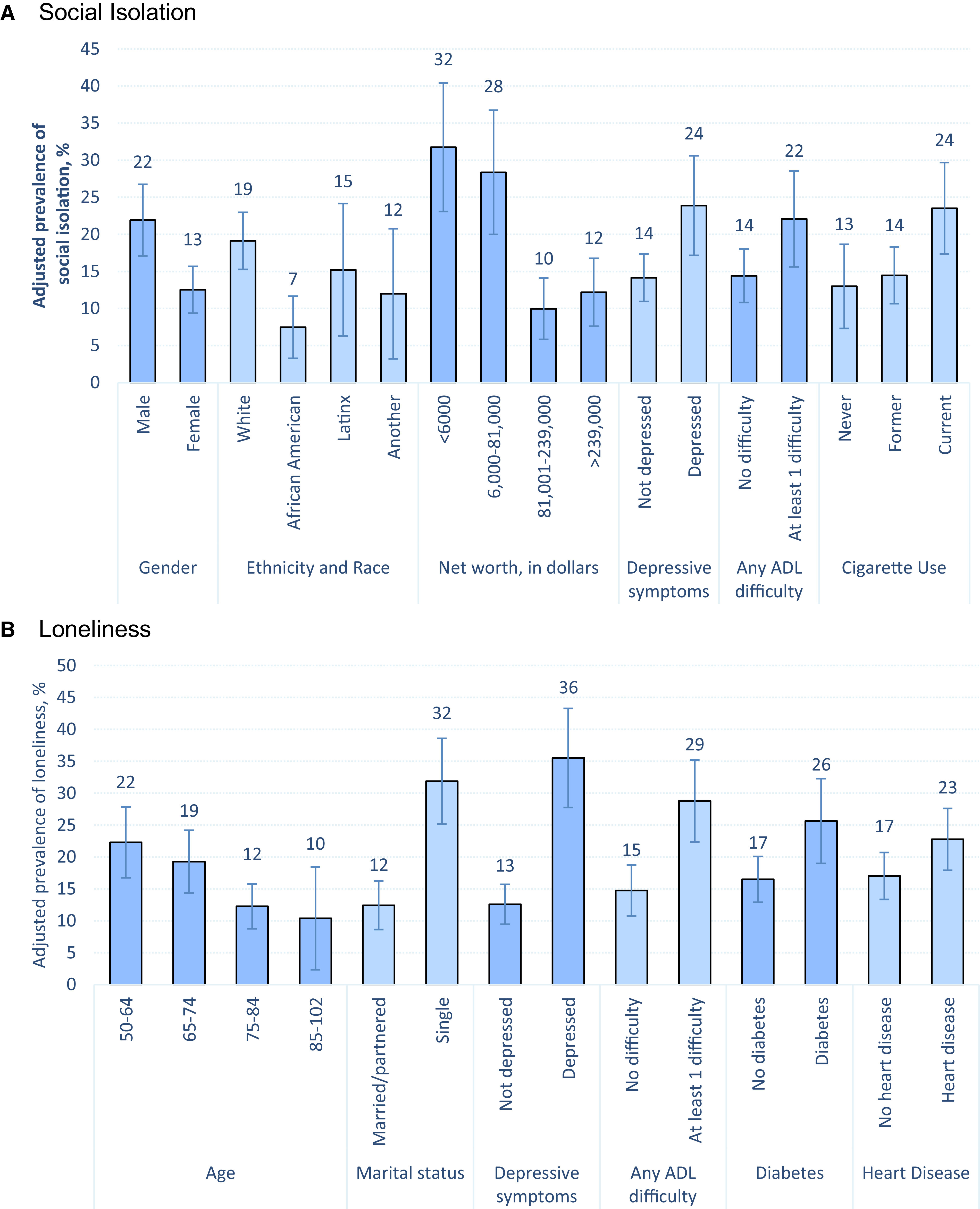
Identified subgroups at risk for (A) social isolation and (B) loneliness among persons with chronic obstructive pulmonary disease (n = 1,100). All displayed comparisons reached a significance threshold of P < 0.05. For ordinal categorical variables, P values were derived from joint Wald tests, which provide an overall test of significance. ADL = activities of daily living.
Discussion
In a nationally representative sample, one in six people with COPD experienced social isolation, and one in five experienced frequent loneliness. In particular, among those with COPD on supplemental oxygen, the prevalence of social isolation and frequent loneliness was almost double that of the general population, suggesting that this group is particularly vulnerable (22, 31, 32). Consequently, our study demonstrates the substantial and underrecognized problem of social isolation and loneliness in COPD, and the key demographic and clinical characteristics that we identified can guide the design of interventions that promote social participation and wide-scale policy changes that better support this population.
The high prevalence of social isolation is striking, as we used a relatively strict definition that takes into account how social networks tend to constrict with age and serious illness (socioemotional selectivity theory) (33). Our analysis of social isolation subscales revealed that the primary drivers of social isolation included a substantially higher prevalence of being unmarried, living alone, having less than monthly social interaction with friends, and reduced or nearly nonexistent community engagement. This is consistent with prior qualitative studies in which people with COPD describe the disease restricting their social activities and physical movement inside and outside the home because of debilitating symptoms and reduced functional status (34). Subgroups associated with social isolation identified by our study and consistent with prior literature included individuals reporting male sex, lower socioeconomic status, depression symptoms, any difficulty with ADLs, and current cigarette use (20, 25, 35, 36). Social isolation is known to be strongly associated with numerous poor health outcomes in the general U.S. population and uniquely among persons with COPD may be tied to acute COPD exacerbations, worsening health-related quality of life, and mortality after ICU admissions (36–39).
We found that the high prevalence of loneliness in people with COPD was similar to a study of individuals with other serious illnesses or the end of life (17). In contrast to prior literature, we found middle-aged adults (50–65 yr old) had a higher prevalence of loneliness than older adults (25% vs. 16%). Potential explanations include physical limitations or symptoms interfering with the ability to work or participate in activities with similar-aged peers. Alternatively, middle-aged adults with COPD may experience heightened feelings of stigma and shame. Additional characteristics associated with loneliness and aligned with prior literature included low socioeconomic status, depression symptoms, and difficulties with ADLs (22, 40). Our definition of “frequent” loneliness indicates a high level of emotional distress and difficulty coping. Loneliness has been further linked to cognitive and functional decline, as well as increased depression and anxiety. These factors may contribute to poor health outcomes and health-related quality of life among persons with COPD (22, 41, 42).
As hypothesized, supplemental oxygen use was associated with a significantly higher frequency of social isolation and loneliness among people with COPD compared with the general population. Consequently, supplemental oxygen is a significant marker that has both clinical and socially significant ramifications, either as a reflection of worsening disease status or as a direct consequence of supplemental oxygen. Although studies have demonstrated increased survival and improved health-related quality of life in certain subgroups of people with COPD who use oxygen (43–45), our study raises a level of caution on the potentially socially harmful tradeoffs that supplemental oxygen can unwittingly impose, especially for older adults. It may be stigmatizing to carry oxygen and lead to perceptions of weakness or frailty (11, 34, 46, 47). Supplemental oxygen tanks, the mainstay for oxygen therapy when leaving the home, are heavy and often difficult to carry; patients report heightened fear of tripping and falling over the oxygen tubing or tank (46, 48, 49). Researchers should develop more portable and lightweight supplemental oxygen delivery methods, and policymakers should expand Medicare coverage for modalities that are safe, easy to carry, and promote functional independence, such as portable oxygen concentrators, which are currently too expensive for most, and liquid oxygen, which has virtually disappeared from the market because of competitive bidding (50). In addition, those with COPD on supplemental oxygen have higher symptom burden and consequently may benefit from proactive referral to specialist palliative care; clinicians should further consider using oxygen initiation to trigger conversations about social well-being (51).
Our study has several additional implications for clinical practice and policy. Clinicians and their clinical teams should consider using validated screening tools to screen for social isolation and loneliness as part of their routine management in COPD (52, 53). COPD is a chronic disease with slow progression over time, and people living with COPD have described a coping strategy of normalization (34); consequently, it is important for clinicians not to assume who is or is not lonely or isolated. Given the current timing constraints on clinicians, studies are needed to identify evidence-based screening practices by different members of clinical teams and health systems.
Once identified, we suggest an individualized approach based on each patient’s unique needs. This is an active area of research, and further studies are needed of evidence-based interventions to address social isolation and loneliness for persons with COPD. Clinical frameworks exist and consider the need to partner with interdisciplinary teams (such as mental health, social work, and case management), given the time and complex nature of addressing social needs (54–56). Awareness of modifiable clinical risk factors, such as treating depression and providing digital technology devices, assistive therapies such as walkers, and hearing or visual aids, can optimize a patient’s ability to be socially connected (57). Pulmonary rehabilitation, an evidence-based program that helps people with COPD to self-manage dyspnea symptoms, may improve exercise capacity and facilitate active social participation.
Clinicians should understand how social isolation and loneliness may be deeply intertwined with symptoms of dyspnea, pain, and fatigue and consider using social interventions to supplement traditional pharmacologic or nonpharmacologic approaches to symptom management (42). Moreover, given the risk of ICU-level care among persons with COPD, early identification of healthcare proxies and potential caregivers for socially isolated adults with COPD should be a high priority.
Policymakers should consider sustained funding for programs addressing isolation and loneliness among persons with COPD who have a harder time accessing healthcare or leaving their home (57). Examples include expanded access to virtual clinic visits and virtual pulmonary rehabilitation, provision of cell phones, internet, and teleconferencing tools, and social support programs that provide transportation or go to one’s home. No financial structure currently exists wherein healthcare professionals are compensated to address social determinants of health. Efforts to improve reimbursement for addressing social needs are therefore needed (58).
Limitations
Our study has several limitations. First, COPD and supplemental oxygen use were self-reported. Previous studies suggest self-reported COPD has high specificity but may miss individuals with undiagnosed COPD based on pulmonary function tests (59). Reassuringly, our study prevalence of approximately 11% is consistent with other reported national prevalence estimates for this age group (16). Second, we do not have pulmonary function tests, arterial blood gas data, or more information about the frequency or timing of oxygen use to understand the severity of COPD or cooccurring conditions necessitating long-term oxygen therapy. Third, our data are cross-sectional, and our ability to determine causality is limited. Last, there may be selection effects in response to the HRS and LBQ. A comparison of responders and nonresponders to the LBQ showed similar demographic and clinical characteristics and small differences by race/ethnicity and education; we addressed these differences using survey weights that account for nonresponse and covariate adjustment. Nevertheless, use of survey weights may not completely mitigate nonresponse bias among individuals with advanced disease or functional impairments preventing study participation.
Conclusions
Our nationally representative study demonstrates that people living with COPD, especially those on supplemental oxygen, experience a high prevalence of social isolation and loneliness. Identifying and addressing these social needs represents a critical opportunity to improve social well-being and health outcomes in this population.
Footnotes
Supported by National Institute of Health (NIH) grants T32HL007185-45 (A.O.S.), K76AG064327 (A.S.I.), K24 H148314 (D.B.W.), U01HL145435 (J.S.), K24AG054415 (R.S.), K23AG065438 (A.K.), and National Heart, Lung, and Blood Institute (NHLBI) grant U01HL163242 (J.S.).
Author Contributions: A.O.S. and A.K. had full access to all study data and take responsibility for data integrity and accuracy. Concept and design: A.O.S., A.S.I., A.K. Acquisition, analysis, or data interpretation: A.O.S., A.S.I., I.C., A.K. Manuscript writing and revision: A.O.S., A.S.I., I.C., E.F., D.B.W., J.S., R.S., A.K. Administrative, technical, or material support: I.C., A.K. Supervision: R.S., A.K.
This article has a data supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd).
- 2. Pleasants RA, Riley IL, Mannino DM. Defining and targeting health disparities in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis . 2016;11:2475–2496. doi: 10.2147/COPD.S79077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gerst-Emerson K, Jayawardhana J. Loneliness as a public health issue: the impact of loneliness on health care utilization among older adults. Am J Public Health . 2015;105:1013–1019. doi: 10.2105/AJPH.2014.302427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Manemann SM, Chamberlain AM, Roger VL, Griffin JM, Boyd CM, Cudjoe TKM, et al. Perceived social isolation and outcomes in patients with heart failure. J Am Heart Assoc . 2018;7:e008069. doi: 10.1161/JAHA.117.008069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mosen DM, Banegas MP, Tucker-Seeley RD, Keast E, Hu W, Ertz-Berger B, et al. Social isolation associated with future health care utilization. Popul Health Manag . 2021;24:333–337. doi: 10.1089/pop.2020.0106. [DOI] [PubMed] [Google Scholar]
- 6. Hackett RA, Hudson JL, Chilcot J. Loneliness and type 2 diabetes incidence: findings from the English Longitudinal Study of Ageing. Diabetologia . 2020;63:2329–2338. doi: 10.1007/s00125-020-05258-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Valtorta NK, Kanaan M, Gilbody S, Ronzi S, Hanratty B. Loneliness and social isolation as risk factors for coronary heart disease and stroke: systematic review and meta-analysis of longitudinal observational studies. Heart . 2016;102:1009–1016. doi: 10.1136/heartjnl-2015-308790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Coyle CE, Dugan E. Social isolation, loneliness and health among older adults. J Aging Health . 2012;24:1346–1363. doi: 10.1177/0898264312460275. [DOI] [PubMed] [Google Scholar]
- 9. Franssen FME, Smid DE, Deeg DJH, Huisman M, Poppelaars J, Wouters EFM, et al. The physical, mental, and social impact of COPD in a population-based sample: results from the Longitudinal Aging Study Amsterdam. NPJ Prim Care Respir Med . 2018;28:30. doi: 10.1038/s41533-018-0097-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Witt LJ, Wroblewski KE, Pinto JM, Wang E, McClintock MK, Dale W, et al. Beyond the lung: geriatric conditions afflict community-dwelling older adults with self-reported chronic obstructive pulmonary disease. Front Med (Lausanne) . 2022;9:814606. doi: 10.3389/fmed.2022.814606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. AlMutairi HJ, Mussa CC, Lambert CTM, Vines DL, Strickland SL. Perspectives from COPD subjects on portable long-term oxygen therapy devices. Respir Care . 2018;63:1321–1330. doi: 10.4187/respcare.05916. [DOI] [PubMed] [Google Scholar]
- 12. Suen A, Cenzer I, Iyer A, Sudore R, Kotwal A. National prevalence and risk factors for loneliness and social isolation among adults with chronic obstructive pulmonary disease [abstract] Am J Respir Crit Care Med . 2023;207:A6635. [Google Scholar]
- 13. Suen A, Iyer A, Cenzer I, et al. National prevalence of social isolation and loneliness in older adults with chronic obstructive pulmonary disease [abstract] J Am Geriatr Soc . 2023;71:S134. doi: 10.1513/AnnalsATS.202304-288OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clarke P, Fisher G, House J, Smith J, Weir D.
- 15. Martinez CH, Richardson CR, Han MK, Cigolle CT. Chronic obstructive pulmonary disease, cognitive impairment, and development of disability: the health and retirement study. Ann Am Thorac Soc . 2014;11:1362–1370. doi: 10.1513/AnnalsATS.201405-187OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ford ES, Croft JB, Mannino DM, Wheaton AG, Zhang X, Giles WH. COPD surveillance: United States, 1999-2011. Chest . 2013;144:284–305. doi: 10.1378/chest.13-0809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kotwal AA, Cenzer IS, Waite LJ, Covinsky KE, Perissinotto CM, Boscardin WJ, et al. The epidemiology of social isolation and loneliness among older adults during the last years of life. J Am Geriatr Soc . 2021;69:3081–3091. doi: 10.1111/jgs.17366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Shah SJ, Fang MC, Wannier SR, Steinman MA, Covinsky KE. Association of social support with functional outcomes in older adults who live alone. JAMA Intern Med . 2022;182:26–32. doi: 10.1001/jamainternmed.2021.6588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Abe N, Ide K, Watanabe R, Hayashi T, Iizuka G, Kondo K. Social participation and incident disability and mortality among frail older adults: a JAGES longitudinal study. J Am Geriatr Soc . 2023;71:1881–1890. doi: 10.1111/jgs.18269. [DOI] [PubMed] [Google Scholar]
- 20. Shiba K, Torres JM, Daoud A, Inoue K, Kanamori S, Tsuji T, et al. Estimating the impact of sustained social participation on depressive symptoms in older adults. Epidemiology . 2021;32:886–895. doi: 10.1097/EDE.0000000000001395. [DOI] [PubMed] [Google Scholar]
- 21. Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging . 2004;26:655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Perissinotto CM, Stijacic Cenzer I, Covinsky KE. Loneliness in older persons: a predictor of functional decline and death. Arch Intern Med . 2012;172:1078–1083. doi: 10.1001/archinternmed.2012.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Steffick DE, Wallace RB, Herzog AR.2000.
- 24. Radloff LS. Appl Psychol Meas . 1977;1:385–401. [Google Scholar]
- 25. Cudjoe TKM, Roth DL, Szanton SL, Wolff JL, Boyd CM, Thorpe RJ. The epidemiology of social isolation: national health and aging trends study. J Gerontol B Psychol Sci Soc Sci . 2020;75:107–113. doi: 10.1093/geronb/gby037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JWR, Weir DR. Cohort profile: the Health and Retirement Study (HRS) Int J Epidemiol . 2014;43:576–585. doi: 10.1093/ije/dyu067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hawkley LC, Hughes ME, Waite LJ, Masi CM, Thisted RA, Cacioppo JT. From social structural factors to perceptions of relationship quality and loneliness: the Chicago Health, Aging, and Social Relations Study. J Gerontol B Psychol Sci Soc Sci . 2008;63:S375–S384. doi: 10.1093/geronb/63.6.s375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Goodman SN. Multiple comparisons, explained. Am J Epidemiol . 1998;147:8007–812. doi: 10.1093/oxfordjournals.aje.a009531. [DOI] [PubMed] [Google Scholar]
- 29.Lee S, Nishimura R, Burton P, Mccammon R.2021. https://hrs.isr.umich.edu/sites/default/files/biblio/HRS2016SamplingWeights.pdf
- 30.StataCorp. Stata statistical software: release 16. College Station, TX: StataCorp LP; 2019. [Google Scholar]
- 31. Iyer AS, Wells RD, Dionne-Odom JN, Bechthold AC, Armstrong M, Byun JY, et al. Project EPIC (Early Palliative Care in COPD): a formative and summative evaluation of the EPIC telehealth intervention. J Pain Symptom Manage . 2023;65:335–347.e3. doi: 10.1016/j.jpainsymman.2022.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kelley AS, Bollens-Lund E. Identifying the population with serious illness: the “denominator” challenge. J Palliat Med . 2018;21:S7–S16. doi: 10.1089/jpm.2017.0548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Carstensen LL, Isaacowitz DM, Charles ST. Taking time seriously: a theory of socioemotional selectivity. Am Psychol . 1999;54:165–181. doi: 10.1037//0003-066x.54.3.165. [DOI] [PubMed] [Google Scholar]
- 34. Marx G, Nasse M, Stanze H, Boakye SO, Nauck F, Schneider N. Meaning of living with severe chronic obstructive lung disease: a qualitative study. BMJ Open . 2016;6:e011555. doi: 10.1136/bmjopen-2016-011555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Philip KE, Bu F, Polkey MI, Brown J, Steptoe A, Hopkinson NS, et al. Relationship of smoking with current and future social isolation and loneliness: 12-year follow-up of older adults in England. Lancet Reg Health Eur . 2022;14:100302. doi: 10.1016/j.lanepe.2021.100302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Iyer A, Wells JM, Bhatt SP, Kirkpatrick DP, Sawyer P, Brown CJ, et al. Life-space mobility and clinical outcomes in COPD. Int J Chron Obstruct Pulmon Dis . 2018;13:2731–2738. doi: 10.2147/COPD.S170887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Panagioti M, Scott C, Blakemore A, Coventry PA. Overview of the prevalence, impact, and management of depression and anxiety in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis . 2014;9:1289–1306. doi: 10.2147/COPD.S72073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Matte DL, Pizzichini MMM, Hoepers ATC, Diaz AP, Karloh M, Dias M, et al. Prevalence of depression in COPD: a systematic review and meta-analysis of controlled studies. Respir Med . 2016;117:154–161. doi: 10.1016/j.rmed.2016.06.006. [DOI] [PubMed] [Google Scholar]
- 39. Iyer AS, Bhatt SP, Garner JJ, Wells JM, Trevor JL, Patel NM, et al. Depression is associated with readmission for acute exacerbation of chronic obstructive pulmonary disease. Ann Am Thorac Soc . 2016;13:197–203. doi: 10.1513/AnnalsATS.201507-439OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Barnes TL, MacLeod S, Tkatch R, Ahuja M, Albright L, Schaeffer JA, et al. Cumulative effect of loneliness and social isolation on health outcomes among older adults. Aging Ment Health . 2022;26:1327–1334. doi: 10.1080/13607863.2021.1940096. [DOI] [PubMed] [Google Scholar]
- 41. Lam JA, Murray ER, Yu KE, Ramsey M, Nguyen TT, Mishra J, et al. Neurobiology of loneliness: a systematic review. Neuropsychopharmacology . 2021;46:1873–1887. doi: 10.1038/s41386-021-01058-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Powell VD, Kumar N, Galecki AT, Kabeto M, Clauw DJ, Williams DA, et al. Bad company: loneliness longitudinally predicts the symptom cluster of pain, fatigue, and depression in older adults. J Am Geriatr Soc . 2022;70:2225–2234. doi: 10.1111/jgs.17796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Nocturnal Oxygen Therapy Trial Group. Continuous or nocturnal oxygen therapy in hypoxemic chronic obstructive lung disease: a clinical trial. Ann Intern Med . 1980;93:391–398. doi: 10.7326/0003-4819-93-3-391. [DOI] [PubMed] [Google Scholar]
- 44. Long term domiciliary oxygen therapy in chronic hypoxic cor pulmonale complicating chronic bronchitis and emphysema: report of the Medical Research Council Working Party. Lancet . 1981;1:681–686. [PubMed] [Google Scholar]
- 45. Eaton T, Lewis C, Young P, Kennedy Y, Garrett JE, Kolbe J. Long-term oxygen therapy improves health-related quality of life. Respir Med . 2004;98:285–293. doi: 10.1016/j.rmed.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 46. Goldbart J, Yohannes AM, Woolrych R, Caton S. ‘It is not going to change his life but it has picked him up’: a qualitative study of perspectives on long term oxygen therapy for people with chronic obstructive pulmonary disease. Health Qual Life Outcomes . 2013;11:124. doi: 10.1186/1477-7525-11-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Panos RJ, Krywkowski-Mohn SM, Sherman SN, Lach LA. Patient reported determinants of health: a qualitative analysis of veterans with chronic obstructive pulmonary disease. COPD . 2013;10:333–347. doi: 10.3109/15412555.2012.752805. [DOI] [PubMed] [Google Scholar]
- 48. Bueno GH, Campos CJG, Turato ER, Paschoal IA, Valladão LS, Baltieri L, et al. Experiences in elderly people with chronic obstructive pulmonary disease in relation to the use of long-term home oxygen therapy: a qualitative study about feelings attributed to therapy. BMC Pulm Med . 2022;22:96. doi: 10.1186/s12890-022-01891-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Jacobs SS, Lindell KO, Collins EG, Garvey CM, Hernandez C, McLaughlin S, et al. Patient perceptions of the adequacy of supplemental oxygen therapy: results of the American Thoracic Society Nursing Assembly Oxygen Working Group survey. Ann Am Thorac Soc . 2018;15:24–32. doi: 10.1513/AnnalsATS.201703-209OC. [DOI] [PubMed] [Google Scholar]
- 50. Duan KI, Wong ES, Liao JM, Sabbatini AK, Au DH. Long-term trends in home respiratory medical equipment among U.S. Medicare patients, 2013-2019. Am J Respir Crit Care Med . 2022;206:509–511. doi: 10.1164/rccm.202202-0238LE. [DOI] [PubMed] [Google Scholar]
- 51. Sullivan DR, Iyer AS, Enguidanos S, Cox CE, Farquhar M, Janssen DJA, et al. Palliative care early in the care continuum among patients with serious respiratory illness: an official ATS/AAHPM/HPNA/SWHPN policy statement. Am J Respir Crit Care Med . 2022;206:e44–e69. doi: 10.1164/rccm.202207-1262ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Kotwal AA, Cenzer IS, Waite LJ, Smith AK, Perissinotto CM, Hawkley LC. A single question assessment of loneliness in older adults during the COVID-19 pandemic: a nationally-representative study. J Am Geriatr Soc . 2022;70:1342–1345. doi: 10.1111/jgs.17700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Perissinotto C, Holt-Lunstad J, Periyakoil VS, Covinsky K. A practical approach to assessing and mitigating loneliness and isolation in older adults. J Am Geriatr Soc . 2019;67:657–662. doi: 10.1111/jgs.15746. [DOI] [PubMed] [Google Scholar]
- 54. Savage RD, Stall NM, Rochon PA. Looking before we leap: building the evidence for social prescribing for lonely older adults. J Am Geriatr Soc . 2020;68:429–431. doi: 10.1111/jgs.16251. [DOI] [PubMed] [Google Scholar]
- 55. Kotwal AA, Fuller SM, Myers JJ, Hill D, Tha SH, Smith AK, et al. A peer intervention reduces loneliness and improves social well-being in low-income older adults: a mixed-methods study. J Am Geriatr Soc . 2021;69:3365–3376. doi: 10.1111/jgs.17450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Hoyumpa G, Narro A, Law M, Ciavarra B, Phung V, Chiang S, et al. Medical student-led social phone calls with elder mistreatment victims: changes in loneliness, depression, and perspectives of aging. J Am Geriatr Soc . 2022;70:1876–1878. doi: 10.1111/jgs.17713. [DOI] [PubMed] [Google Scholar]
- 57. Han MK, Martinez CH, Au DH, Bourbeau J, Boyd CM, Branson R, et al. Meeting the challenge of COPD care delivery in the USA: a multiprovider perspective. Lancet Respir Med . 2016;4:473–526. doi: 10.1016/S2213-2600(16)00094-1. [DOI] [PubMed] [Google Scholar]
- 58. Escalante E, Golden RL, Mason DJ. Social isolation and loneliness: imperatives for health care in a post-COVID world. JAMA Health Forum . 2020;1:e201597. doi: 10.1001/jamahealthforum.2020.1597. [DOI] [PubMed] [Google Scholar]
- 59. Clark KA, Mazurek JM. Validity of self-reported health professional diagnosed chronic obstructive pulmonary disease (COPD)-National Health and Nutrition Examination Survey (NHANES) 2007–2012. Am J Respir Crit Care Med . 2018;197:A3546. [Google Scholar]