Key Points
Question
What will the global and regional burden of COPD be in terms of cases and prevalence by 2050?
Findings
In this modeling study, global COPD prevalence was projected to approach 600 million cases worldwide by 2050, which represents a relative growth of 23% in the number of individuals with COPD compared with 2020. The largest growth was projected to occur among females and within low- and middle-income income countries and regions.
Meaning
In this study, the global burden of COPD was projected to increase through 2050; effective governance is required to lower the future burden of COPD.
This modeling study assesses the global burden of chronic obstructive pulmonary disease through 2050.
Abstract
Importance
Chronic obstructive pulmonary disease (COPD) is a respiratory condition that is associated with significant health and economic burden worldwide. Previous studies assessed the global current-day prevalence of COPD, but to better facilitate resource planning and intervention development, long-term projections are needed.
Objective
To assess the global burden of COPD through 2050, considering COPD risk factors.
Design, Setting, and Participants
In this modeling study, historical data on COPD prevalence was extracted from a recent meta-analysis on 2019 global COPD prevalence, and 2010 to 2018 historical prevalence was estimated using random-effects meta-analytical models. COPD risk factor data were obtained from the Global Burden of Disease database.
Main Outcomes and Measures
To project global COPD prevalence to 2050, generalized additive models were developed, including smoking prevalence, indoor and outdoor air pollution, and development indices as predictors, and stratified by age, sex, and World Bank region.
Results
The models estimated that the number of COPD cases globally among those aged 25 years and older will increase by 23% from 2020 to 2050, approaching 600 million patients with COPD globally by 2050. Growth in the burden of COPD was projected to be the largest among women and in low- and middle-income regions. The number of female cases was projected to increase by 47.1% (vs a 9.4% increase for males), and the number of cases in low- and middle-income regions was expected to be more than double that of high-income regions by 2050.
Conclusions and Relevance
In this modeling study of future COPD burden, projections indicated that COPD would continue to affect hundreds of millions of people globally, with disproportionate growth among females and in low-middle income regions through 2050. Further research, prevention, and advocacy are needed to address these issues so that adequate preparation and resource allocation can take place.
Introduction
Chronic obstructive pulmonary disease (COPD) is a progressive respiratory condition with major sequelae including cardiovascular risk, respiratory failure, and lung cancer.1 Several risk factors have been proposed to contribute to COPD, including smoking, indoor and outdoor air pollution, genetics, occupational hazards, and childhood or adult infections.2,3 Furthermore, COPD inflicts a large and growing burden in both direct and indirect costs to society.4 In the European Union, for example, the total direct costs of respiratory diseases are estimated to be 6% of the total annual health care allocation, with COPD accounting for 56% (€38.6 billion) of the total cost of respiratory diseases.5 In the United States, COPD costs are projected to increase over the next 20 years, approaching $40 billion per year and translating into a total of $800 billion over 20 years.6
Given the considerable health and societal burden of COPD, previous studies have attempted to estimate the global epidemiology of COPD, but estimates vary widely. For example, studies conducted by the Global Burden of Disease (GBD) generated estimates of global age-standardized COPD prevalence that vary between 2% to 5% across years, representing variable estimates of 328 million people with COPD in 2010 (4.77% prevalence),2 299 million in 2017 (3.9% prevalence),7 and 212 million in 2019 (2.7% prevalence).8 One explanation for these inconsistent prevalence estimates is that it is not clear how different case definitions of COPD were addressed8 and that differences in methods between reports produce variable results.9
Other recent works suggest the prevalence of COPD, using the Global Initiative for Chronic Obstructive Lung Disease (GOLD) definition of COPD (ie, forced expiratory volume during the first second of forced breath [FEV1] / forced vital capacity [FVC] < 0.7),10 to be between 9% and 12%, translating to 300 to 400 million individuals with COPD globally in 2018 to 2019.9,11,12 The relatively large differences in COPD prevalence estimates within GBD studies, and between GBD studies and meta-analyses, demonstrate how differences in data sources, diagnosis definitions, methods, and statistical approaches can yield variable results.9
While these current-day estimation efforts are valuable, long-term projections of COPD prevalence and cases are needed. Such projections are essential for resource planning and informing COPD intervention programs. Also, it is imperative to understand epidemiologic trends to target and prioritize prevention efforts by region and at-risk group. Given current trends that might impact the development and progression of COPD, including growing and aging of the global population,13 industrialization in developing countries, global urbanization,14 increased immunization rates for pneumonia,15 and shifts in smoking prevalence and exposure to indoor and outdoor air pollution, projecting COPD prevalence is a timely topic. Therefore, we sought to provide a comprehensive set of estimates regarding regional and global burden of COPD from 2020 through 2050, incorporating all published population-level COPD prevalence studies in the literature, and accounting for projections of known COPD risk factors, including smoking, particulate matter pollution (including particles ≤2.5 microns diameter [PM2.5]), ozone pollution, household air pollution, and global human development trends, stratified by regional income and sex.
Methods
COPD Prevalence Data Set
To project global and regional COPD prevalence through 2050, we used data from a recent meta-analysis,8 which estimated global, regional, and national COPD prevalence in 2019 using 162 population-based studies from 65 countries, across both males and females 25 years or older. Since this concerns a literature-based study, ethical approval and informed consent were not required. Although COPD is commonly diagnosed after age 40 years, people have been shown to be diagnosed with COPD as early as their 20s or 30s.16 COPD was defined according to GOLD criteria (ie, FEV1 / FVC < 0.7). To generate future COPD prevalence projections, more historical data predating 2019 were needed; therefore, we performed random-effects meta-analytical models for the years 2010 to 2018, providing the crude pooled COPD prevalence for those years across 7 world regions according to the World Bank classification (East Asia and Pacific, Europe and Central Asia, Middle East and North Africa, North America, Latin America and Caribbean, South Asia, and sub-Saharan Africa). Due to the limited availability of historic regional data on COPD prevalence, we stopped extrapolating historical data to 2010. Subsequently, this historical COPD prevalence (2010-2019), as well as known COPD risk factors, were used to estimate COPD prevalence from 2020 to 2050.
COPD Risk Factor Projection
The models adjusted for COPD risk factors at the regional level, including smoking prevalence (measured as the proportion [%] of current smokers within a population), household air pollution (HAP) from solid fuels (measured as the annual proportion [%] of households per country exposed to unhealthy indoor air), human development index (HDI; a marker of human welfare within a country), PM2.5 (micrograms per meter, annual average per country), and ambient ozone concentrations (parts per billion, measured as the highest seasonal average 8-hour maximum per region). Data and their sources are described in detail in eAppendix 1 in Supplement 1. Separate generalized additive models (GAMs; eAppendix 2 in Supplement 1) were developed to project each risk factor individually to 2050. HDI, which was previously projected through 2050 by prior published work,17 was used in these GAMs to forecast estimates of each COPD risk factor to 2050.
Statistical Analysis
Model Development and Evaluation
GAMs were developed to project global and regional COPD prevalence through 2050. Forecasted data on COPD risk factors through 2050 were included in GAM models to estimate the regional COPD prevalence in 2050. Future estimations of COPD prevalence were made by splitting the data into a training and a test data set. The training data set consisted of historical (2010-2019) trends of regional COPD prevalence, all COPD risk factors, and HDI. The test data set included data on projected future COPD risk factor trends and HDI (2020-2050), which was used to project regional COPD prevalence up to 2050. Separate GAMs were estimated for females and males. All GAMs were performed using the mgcv package in R version 4.1.0 (R Project for Statistical Computing). For each GAM, t distribution for tailed data and a thin plate regression spline were selected. The performance of each GAM model was evaluated by multiple performance indices, including R2, deviance, mean squared error (MSE), Aikake information criteria (AIC), and bayesian information criteria (BIC) (eAppendix 2 in Supplement 1). Analyses were performed in July 2022.
Global and Regional Prevalence and Case Estimates
We generated global and regional estimates about current (2020) and future COPD prevalence (% of eligible population aged ≥25 years for each year up to 2050) and the number of people with COPD (cases) for both males and females. First, the total regional number of people with COPD was obtained by multiplying regional COPD prevalence by regional eligible population estimates from the World Bank, each year from 2020 to 2050, which was then summed to achieve the global number of COPD cases per year. Global COPD prevalence was calculated by dividing the total population with COPD in a given year by the total global population meeting inclusion criteria in that same year. Since global and regional COPD prevalence was averaged based on model output by region and sex and global and regional COPD cases were calculated and aggregated using data not included in the models, confidence intervals for averaged COPD prevalence and calculated COPD cases are not available. However, confidence intervals by region and sex were generated as part of the model and are presented in eAppendix 3 in Supplement 1. Additionally, within the regional data, a distinction was made between low- and middle-income regions, containing low- and middle-income countries (LMICs) and high-income regions, hosting high-income countries (HICs).
Results
Model Fit Results
The performance of each GAM was evaluated through R2, deviance, MSE, AIC, and BIC. Across all measures, both the female and male GAMs showed satisfactory prediction accuracy. Full details on model performance are available in eAppendix 2 in Supplement 1.
Global Trends
At a global level, COPD prevalence in 2020, across both males and females, was estimated to be 10.6%, which translates to 480 million cases (Table). The number of COPD cases was projected to increase by 112 million to a total of 592 million by 2050 (9.5% of the total eligible population), a relative increase of 23.3% from 2020 to 2050. This increase was estimated to be largely driven by an increasing burden of COPD among females and within LMICs. Among females, COPD prevalence was projected to increase from 7.8% in 2020 to 8.3% in 2050, representing a 6.4% relative increase. The number of COPD cases among females was estimated to increase from 177 million in 2020 to 260 million by 2050, which translates to an increase of 83 million cases, a 47.1% relative increase. Global COPD prevalence among males was projected to decrease from 13.4% in 2020 to 10.6% in 2050. However, the number of male cases was estimated to increase from 303 million in 2020 to 331 million by 2050, translating to an increase of 28 million cases, a 9.4% relative increase.
Table. Global Projected COPD Prevalence, Cases, and Relative Change From 2020 to 2050 by Sex.
| Sex | 2020 | 2030 | 2040 | 2050 |
|---|---|---|---|---|
| Female | ||||
| Prevalence, % | 7.8 | 8.1 | 8.34 | 8.33 |
| Cases, No. | 176 776 887 | 210 351 803 | 240 030 181 | 260 106 028 |
| Relative change in prevalence, % | NA | 3.8 (vs 2020) | 2.5 (vs 2030) | −0.12 (vs 2040); 6.4 (vs 2020) |
| Relative change in cases, % | NA | 19.0 (vs 2020) | 14.1 (vs 2030) | 8.4 (vs 2040); 47.1 (vs 2020) |
| Male | ||||
| Prevalence, % | 13.4 | 12.5 | 11.6 | 10.6 |
| Cases | 303 080 615 | 322 532 353 | 333 145 741 | 331 449 760 |
| Relative change in prevalence, % | -NA | −6.7 (vs 2020) | −7.2 (vs 2030) | −8.6 (vs 2040); −20.9 (vs 2020) |
| Relative change in cases, % | NA | 6.4 (vs 2020) | 3.3 (vs 2030) | −0.5 (vs 2040); 9.4 (vs 2020) |
| Global | ||||
| Prevalence, % | 10.6 | 10.3 | 9.7 | 9.5 |
| Cases, No. | 479 857 502 | 532 884 156 | 573 175 922 | 591 555 788 |
| Relative change in prevalence, % | NA | −2.8 (vs 2020) | −5.8 (vs 2030) | −2.1 (vs 2040); −10.4 (vs 2020) |
| Relative change in cases, % | NA | 11.0 (vs 2020) | 7.6 (vs 2030) | 3.2 (vs 2040); 23.3 (vs 2020) |
Abbreviation: NA, not applicable.
Regional Trends
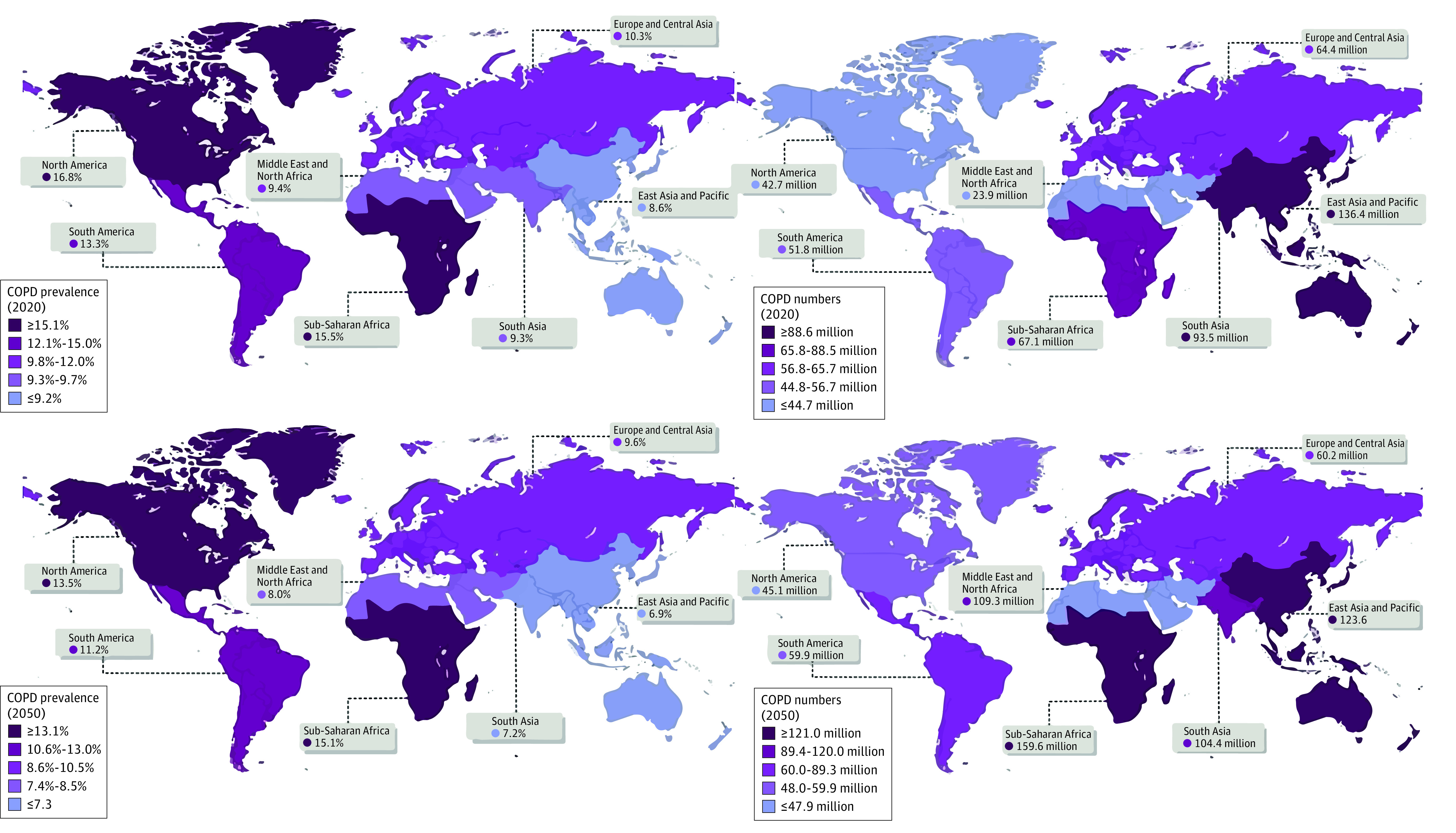
In 2020, the region with the highest projected COPD prevalence was North America (16.8%) (Figure 1). By 2050, with a prevalence of 15.1%, sub-Saharan Africa was projected to become the most prevalent region, translating into 160 million cases (eAppendix 3 in Supplement 1). As to the number of COPD cases, East Asia and Pacific was projected to be the leading region in 2020 with 136 million cases. By 2050, East Asia and Pacific as well as South Asia were projected to be the second and third leading regions, with 124 million and 109 million COPD cases, respectively. Overall, from 2020 to 2050, across both males and females, increases in COPD cases were projected in all regions except for East Asia and Pacific and Europe and Central Asia, where decreases are expected. Sub-Saharan Africa was expected to observe a moderate increase in female COPD prevalence from 13.7% in 2020 to 14.9% by 2050. However, the number of COPD cases among females in sub-Saharan Africa was expected to have a steep increase from 30 million in 2020 to 80 million people with COPD by 2050, translating into 62.5% growth. Among males, the number of COPD cases in sub-Saharan Africa was projected to increase from 37 million in 2020 to 80 million in 2050.
Figure 1. Chronic Obstructive Pulmonary Disease (COPD) Prevalence and Cases Across World Regions From 2020 to 2050.
Trends by Sex
The global burden of COPD among males (Figure 2) will remain higher than females (Figure 3) through 2050 (10.6% vs 8.3%, respectively); however, increasing trends in prevalence among females will begin to approach that of males, driven by increases in LMICs (Figure 4). For males, the number of COPD cases was projected to decrease from 2020 to 2050 in East Asia and Pacific as well as Europe and Central Asia, whereas an increase is estimated to be observed in Middle East and North Africa, North America, Latin America and Caribbean, South Asia, and sub-Saharan Africa. Female COPD prevalence was projected to increase across all regions from 2020 to 2050, except for Europe and Central Asia, which is estimated to observe a small decrease.
Figure 2. Chronic Obstructive Pulmonary Disease (COPD) Prevalence and Cases Among Males From 2020 to 2050 .
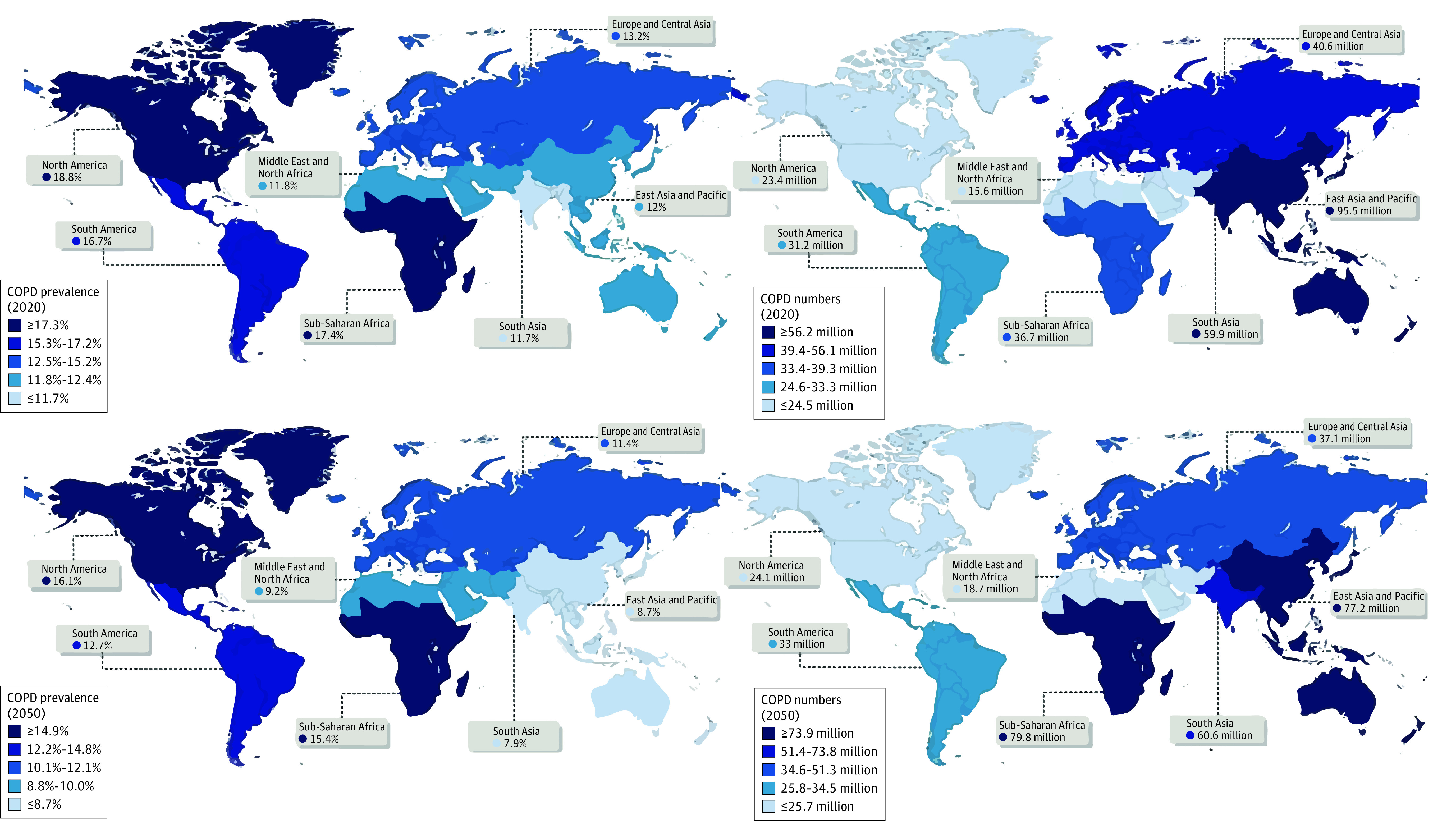
Figure 3. Chronic Obstructive Pulmonary Disease (COPD) Prevalence and Cases Among Females From 2020 to 2050.
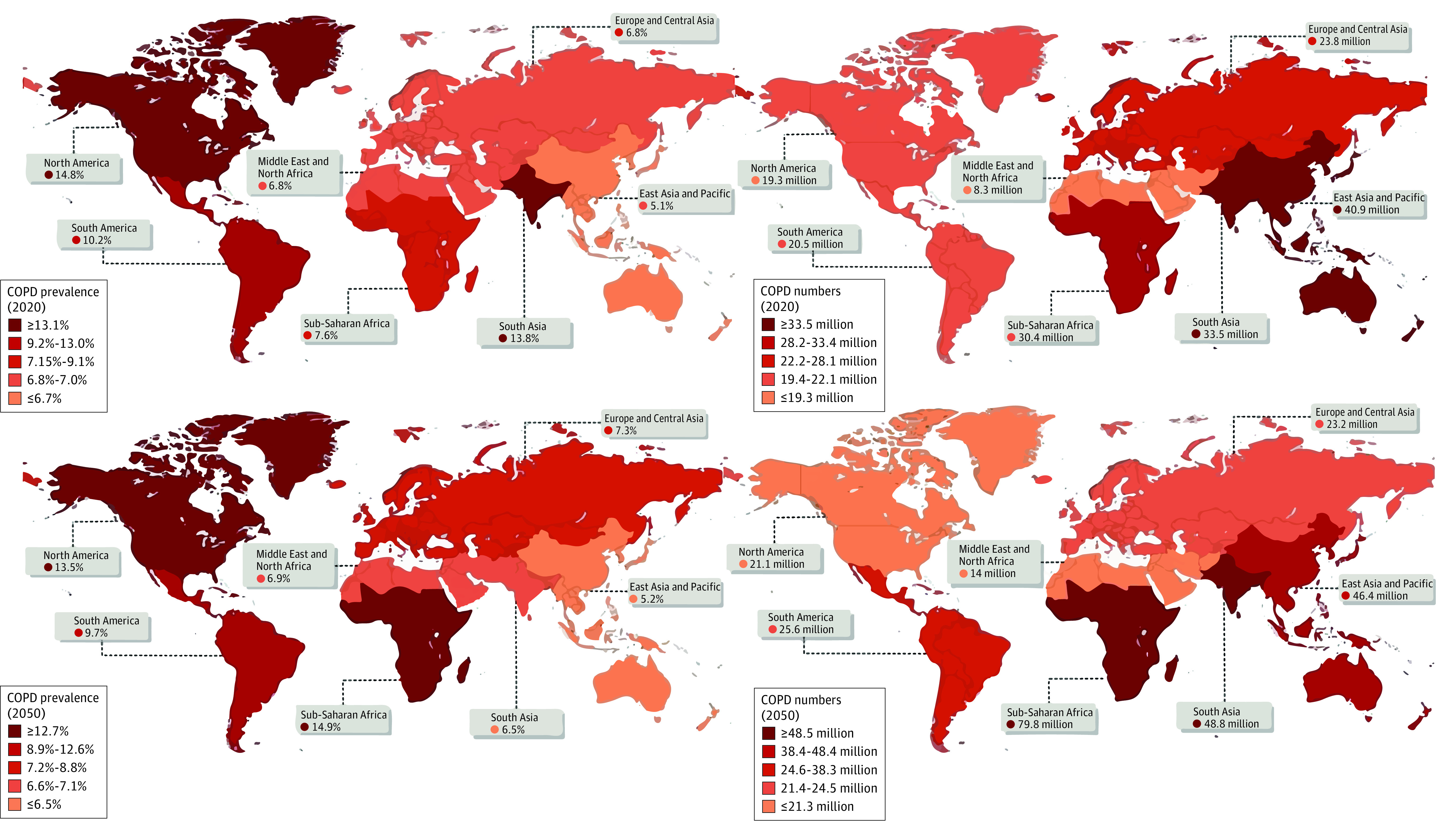
Figure 4. Chronic Obstructive Pulmonary Disease (COPD) Cases Calculated Based on Generalized Additive Models Prevalence Estimates Across Low- and Middle-Income Countries (LMICs) and High-Income Countries (HICs).
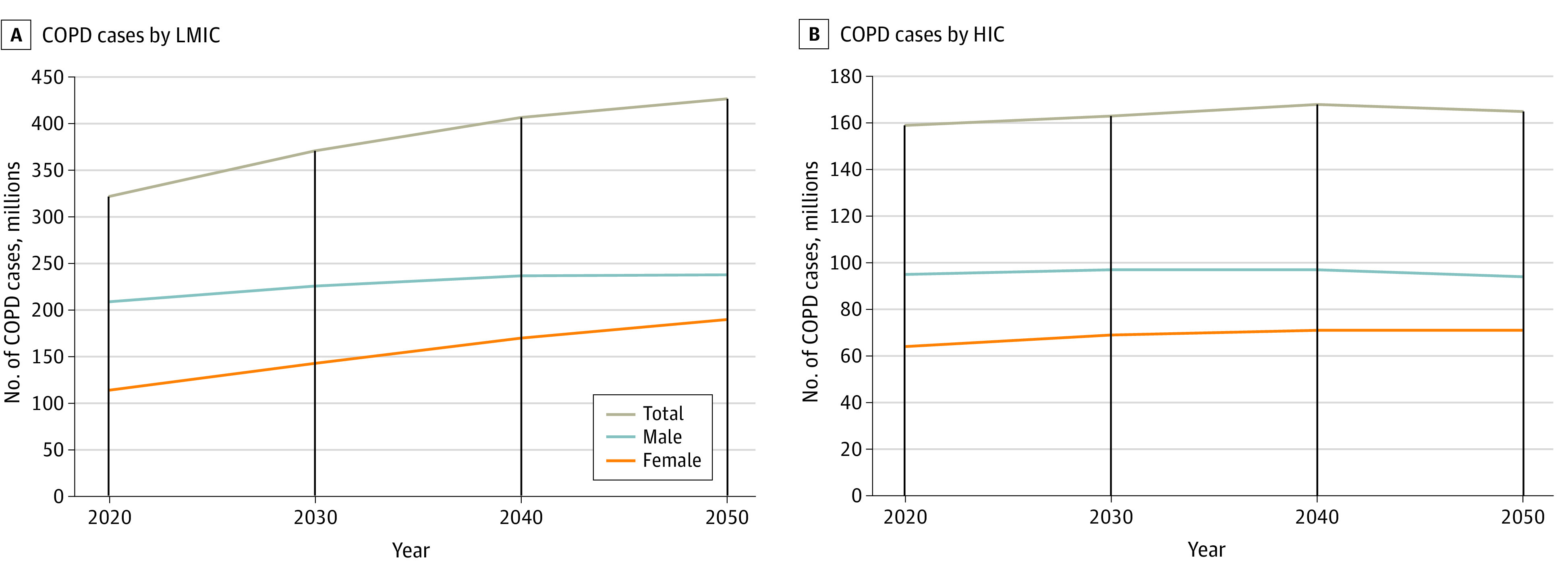
Trends by Income
In 2020, models estimated that LMICs would host 321 million people with COPD vs 159 million in HICs, a 2.0 ratio. By 2050, it was projected that 426 million people with COPD would reside in LMICs vs 166 million residing in HICs, growing the ratio of cases in LMIC:HIC to 2.6. In other words, the disparity of COPD burden in LMICs vs HICs is expected to grow, with an projected growth of 32.7% in LMICs and 3.8% in HICs from 2020 to 2050. Overall, regarding COPD cases, LMICs appear to be growing at a much more rapid pace than HICs, which were projected to observe modest growth from 2020 to 2050 (Figure 4).
Discussion
This study is the first, to our knowledge, to project the prevalence and number of cases of COPD through 2050, at global and regional levels, by income and sex, using spirometry-based data according to the GOLD definition. Due to current trends, including a growing and aging population,13 COPD will continue to be a large burden worldwide, with a relative increase of 23% in the number of cases of COPD, approaching 600 million, with a growing and disparate burden among women and LMICs. Globally, projections indicate overall COPD prevalence may decrease slightly from 10.6% in 2020 to 9.5% by 2050. Factors contributing to this decrease might include urbanization and modernization of technology. Although air pollution is generally found to be worse in urban areas than in rural areas,17 with global urbanization, COPD prevalence might improve because more households are shifting from traditional cooking methods in poorly ventilated homes to gas or electric cooking in better ventilated homes.18 Furthermore, with modernization of air polluting industries in developing countries, outdoor air pollution, such as PM2.5, is generally improving or remaining stable.19 Nevertheless, the number of cases of COPD was projected to increase to 592 million by 2050, a 23% relative increase, likely due to a growing and aging population that continues to be exposed to these underlying risk factors.
When examining the trends by regional income, we observed a growing burden among LMICs. COPD prevalence is estimated to be higher in HICs; however, most absolute cases are projected to be in LMICs both now and in the future, which aligns with previous studies showing that more than three-quarters of global COPD cases exist in LMICs.7,20,21 By 2050, the number of people with COPD in LMICs is expected to be more than double that of HICs. For example, we projected a 59% increase in COPD cases in sub-Saharan Africa, which will surpass other world regions in both COPD prevalence and cases by 2040.8,11,12 This trend likely reflects a growing and aging population, increased exposure to risk factors such as tobacco smoking, continued exposure to indoor pollution due to biomass fuels used for cooking and heating,16,17 outdoor air pollution, inadequate health care access, industrialization, urbanization, and a large burden of childhood and adult lower-respiratory tract infections.2,6,15 Additionally, LMICs largely focus their clinical prevention efforts on communicable diseases, including HIV/AIDS, malaria, and tuberculosis, and to a lesser extent on noncommunicable diseases, such as COPD.22 However, the long-term impact of such communicable diseases includes development of COPD, but long-term follow-up of cases is rarely done.23
When looking at trends by sex, male prevalence and cases will continue to be higher than females through 2050, but growth among females is projected to be steeper. A similar trend has been observed by a study assessing COPD prevalence in the European Union, demonstrating overall increases in female prevalence, but decreases in males from 2001 to 2019.24 The rise of COPD among females has been attributed to increases in smoking prevalence and exposure to biomass smoke during cooking in poorly ventilated homes within LMICs.25 Moreover, to develop COPD, it has been demonstrated that females require less cumulative smoking exposure than males.26 A recent study on COPD mortality worldwide found a consistent decrease in mortality in most countries for males, while an opposite trend was observed in females. These trends were similarly attributed to increased smoking among females and continued indoor air exposure.27 In a spirometry-based study in rural Uganda, a higher COPD prevalence was identified among females (16.8%) vs males (15.4%), attributed to sources of indoor air pollution.28
One challenge in estimating COPD globally is that of accurate diagnosis across varying health systems and especially across regions with differing levels of health-system development. At present, the diagnosis of COPD requires spirometry to demonstrate reductions in airflow.6,12 However, spirometry is not readily and equally available in all areas, leading to potential underdiagnosis, particularly in LMICs. According to a World Health Organization report, at least half of the global population does not have access to essential health services, with wide gaps observed in LMIC regions sub-Saharan Africa and South Asia.14 Distribution of available and appropriate diagnostic and disease-management services will be critical for COPD into the future.
Limitations
We acknowledge several limitations in this study. First, based on our modeling approach, we were reliant on published data regarding COPD prevalence; therefore, our analyses are subject to the same limitations as the original data. For example, COPD is disproportionately underdiagnosed in developing regions, which is reflected by the general lack of available literature from these regions. Second, to forecast COPD risk factors through 2050, we solely relied on HDI, which was projected through 2050 by other work.17 Although HDI was shown to be strongly and positively correlated with the COPD risk factors included in our models, we recognize that there might be other relevant variables that could be used for forecasting COPD risk factors, including seasonal variation and climatic factors.29 Third, in lacking individual data, we relied on aggregate data for our modeling approach, which can be considered a limitation for all such modeling studies. For example, we have annual PM2.5 data at a national level but lack granular data regarding local variations and individual exposures. Consequently, our models and previously published modeling work were not capable of adjusting adequately for relevant confounders, such as demographic information beyond age and sex, socioeconomic status, and information on disease-related behaviors (eg, treatment behavior, health literacy). Fourth, we did not account for competing risks over time. For example, as mortality in the African regions from communicable disease and malnutrition improve, more people will be projected to survive over time, perhaps putting them at more risk for noncommunicable diseases such as COPD. Fifth, we did not account for increased use of vaping (e-cigarettes). For instance, it has been reported that, while controlling for combustible tobacco smoking, the odds of developing respiratory disease were 1.29.30 However, the impact of e-cigarettes on COPD development is unclear but may well become a major contributor in the future beyond what our models would predict. Finally, our study relied on data from the GBD and a recent meta-analysis, both of which did not consider certain genetic risk factors in COPD (eg, stress-induced protein, family history, and interleukin) as discussed by COPDGene,31 and neither were we able to control for all other relevant risk factors across the life course that make COPD a heterogenous disease.32
Conclusions
Our findings provide insight into the contemporary and future global burden of COPD, affecting hundreds of millions of people globally. Furthermore, our findings suggest that COPD may disproportionately impact LMICs and females, who already face high health burdens. Further research, prevention and advocacy is needed to address these issues so that adequate preparation and resource allocation can take place.
eAppendix 1. Risk Factor Data Sources
eAppendix 2. GAM Model Fit
eAppendix 3. Regional COPD Prevalence (2020-2050) and 95% CIs
Data Sharing Statement
References
- 1.Rodríguez-Roisin R, Soriano JB. Chronic obstructive pulmonary disease with lung cancer and/or cardiovascular disease. Proc Am Thorac Soc. 2008;5(8):842-847. doi: 10.1513/pats.200807-075TH [DOI] [PubMed] [Google Scholar]
- 2.López-Campos JL, Tan W, Soriano JB. Global burden of COPD. Respirology. 2016;21(1):14-23. doi: 10.1111/resp.12660 [DOI] [PubMed] [Google Scholar]
- 3.Mannino DM, Buist AS. Global burden of COPD: risk factors, prevalence, and future trends. Lancet. 2007;370(9589):765-773. doi: 10.1016/S0140-6736(07)61380-4 [DOI] [PubMed] [Google Scholar]
- 4.Viegi G, Pistelli F, Sherrill DL, Maio S, Baldacci S, Carrozzi L. Definition, epidemiology and natural history of COPD. Eur Respir J. 2007;30(5):993-1013. doi: 10.1183/09031936.00082507 [DOI] [PubMed] [Google Scholar]
- 5.Rehman AU, Hassali MAA, Muhammad SA, Harun SN, Shah S, Abbas S. The economic burden of chronic obstructive pulmonary disease (COPD) in Europe: results from a systematic review of the literature. Eur J Health Econ. 2020;21(2):181-194. doi: 10.1007/s10198-019-01119-1 [DOI] [PubMed] [Google Scholar]
- 6.Soriano JB, Kendrick PJ, Paulson KR, et al. ; GBD Chronic Respiratory Disease Collaborators . Prevalence and attributable health burden of chronic respiratory diseases, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Respir Med. 2020;8(6):585-596. doi: 10.1016/S2213-2600(20)30105-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vos T, Lim SS, Abbafati C, et al. ; GBD 2019 Diseases and Injuries Collaborators . Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-1222. doi: 10.1016/S0140-6736(20)30925-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adeloye D, Song P, Zhu Y, Campbell H, Sheikh A, Rudan I; NIHR RESPIRE Global Respiratory Health Unit . Global, regional, and national prevalence of, and risk factors for, chronic obstructive pulmonary disease (COPD) in 2019: a systematic review and modelling analysis. Lancet Respir Med. 2022;10(5):447-458. doi: 10.1016/S2213-2600(21)00511-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Global Initiative for Chronic Obstructive Lung Disease (GOLD) . Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. November 15, 2020. Accessed November 7, 2023. https://goldcopd.org/digital-gold-report/
- 10.Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS; GOLD Scientific Committee . Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med. 2001;163(5):1256-1276. doi: 10.1164/ajrccm.163.5.2101039 [DOI] [PubMed] [Google Scholar]
- 11.Ntritsos G, Franek J, Belbasis L, et al. Gender-specific estimates of COPD prevalence: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis. 2018;13:1507-1514. doi: 10.2147/COPD.S146390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Varmaghani M, Dehghani M, Heidari E, Sharifi F, Moghaddam SS, Farzadfar F. Global prevalence of chronic obstructive pulmonary disease: systematic review and meta-analysis. East Mediterr Health J. 2019;25(1):47-57. doi: 10.26719/emhj.18.014 [DOI] [PubMed] [Google Scholar]
- 13.Cho SJ, Stout-Delgado HW. Aging and lung disease. Annu Rev Physiol. 2020;82:433-459. doi: 10.1146/annurev-physiol-021119-034610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miele CH, Grigsby MR, Siddharthan T, et al. ; CRONICAS Cohort Study Group . Environmental exposures and systemic hypertension are risk factors for decline in lung function. Thorax. 2018;73(12):1120-1127. doi: 10.1136/thoraxjnl-2017-210477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lange P, Celli B, Agustí A, et al. Lung-function trajectories leading to chronic obstructive pulmonary disease. N Engl J Med. 2015;373(2):111-122. doi: 10.1056/NEJMoa1411532 [DOI] [PubMed] [Google Scholar]
- 16.National Heart, Lung, and Blood Institute . Alpha-1 antitrypsin deficiency. Updated October 23, 2023. Accessed November 7, 2023. https://www.nhlbi.nih.gov/health/alpha-1-antitrypsin-deficiency
- 17.Frederick S. Pardee Center for International Futures. Pardee Center delivers research for Population Services International. August 1, 2014. Accessed November 15, 2023. https://korbel.du.edu/pardee/news-events/all-articles/pardee-center-delivers-research-population-services-international
- 18.Tibrewal K, Venkataraman C. COVID-19 lockdown closures of emissions sources in India: lessons for air quality and climate policy. J Environ Manage. 2022;302(Pt B):114079. doi: 10.1016/j.jenvman.2021.114079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lin B, Zhu J. Changes in urban air quality during urbanization in China. J Clean Prod. 2018;188:312-321. doi: 10.1016/j.jclepro.2018.03.293 [DOI] [Google Scholar]
- 20.Rossaki FM, Hurst JR, van Gemert F, et al. Strategies for the prevention, diagnosis and treatment of COPD in low- and middle- income countries: the importance of primary care. Expert Rev Respir Med. 2021;15(12):1563-1577. doi: 10.1080/17476348.2021.1985762 [DOI] [PubMed] [Google Scholar]
- 21.World Health Organization. Chronic obstructive pulmonary disease (COPD). March 16, 2023. Accessed November 7, 2023. https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd)
- 22.Ezzati M, Pearson-Stuttard J, Bennett JE, Mathers CD. Acting on non-communicable diseases in low- and middle-income tropical countries. Nature. 2018;559(7715):507-516. doi: 10.1038/s41586-018-0306-9 [DOI] [PubMed] [Google Scholar]
- 23.Marais BJ, Lönnroth K, Lawn SD, et al. Tuberculosis comorbidity with communicable and non-communicable diseases: integrating health services and control efforts. Lancet Infect Dis. 2013;13(5):436-448. doi: 10.1016/S1473-3099(13)70015-X [DOI] [PubMed] [Google Scholar]
- 24.Marshall DC, Al Omari O, Goodall R, et al. Trends in prevalence, mortality, and disability-adjusted life-years relating to chronic obstructive pulmonary disease in Europe: an observational study of the global burden of disease database, 2001-2019. BMC Pulm Med. 2022;22(1):289. doi: 10.1186/s12890-022-02074-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aryal S, Diaz-Guzman E, Mannino DM. Influence of sex on chronic obstructive pulmonary disease risk and treatment outcomes. Int J Chron Obstruct Pulmon Dis. 2014;9:1145-1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Perez TA, Castillo EG, Ancochea J, et al. Sex differences between women and men with COPD: a new analysis of the 3CIA study. Respir Med. 2020;171:106105. doi: 10.1016/j.rmed.2020.106105 [DOI] [PubMed] [Google Scholar]
- 27.Mei F, Dalmartello M, Bonifazi M, et al. Chronic obstructive pulmonary disease (COPD) mortality trends worldwide: an update to 2019. Respirology. 2022;27(11):941-950. doi: 10.1111/resp.14328 [DOI] [PubMed] [Google Scholar]
- 28.van Gemert F, Kirenga B, Chavannes N, et al. Prevalence of chronic obstructive pulmonary disease and associated risk factors in Uganda (FRESH AIR Uganda): a prospective cross-sectional observational study. Lancet Glob Health. 2015;3(1):e44-e51. doi: 10.1016/S2214-109X(14)70337-7 [DOI] [PubMed] [Google Scholar]
- 29.Balogun AL, Tella A, Baloo L, Adebisi N. A review of the inter-correlation of climate change, air pollution and urban sustainability using novel machine learning algorithms and spatial information science. Urban Clim. 2021;40:100989. doi: 10.1016/j.uclim.2021.100989 [DOI] [Google Scholar]
- 30.Bhatta DN, Glantz SA. Association of e-cigarette use with respiratory disease among adults: a longitudinal analysis. Am J Prev Med. 2020;58(2):182-190. doi: 10.1016/j.amepre.2019.07.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ragland MF, Benway CJ, Lutz SM, et al. Genetic advances in chronic obstructive pulmonary disease: insights from COPDGene. Am J Respir Crit Care Med. 2019;200(6):677-690. doi: 10.1164/rccm.201808-1455SO [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stolz D, Mkorombindo T, Schumann DM, et al. Towards the elimination of chronic obstructive pulmonary disease: a Lancet Commission. Lancet. 2022;400(10356):921-972. doi: 10.1016/S0140-6736(22)01273-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix 1. Risk Factor Data Sources
eAppendix 2. GAM Model Fit
eAppendix 3. Regional COPD Prevalence (2020-2050) and 95% CIs
Data Sharing Statement


