Abstract
Background
The definition of irreparable rotator cuff tear (IRCT) is controversial. This scoping review provides definitions used to describe IRCT in the literature. This scoping review (1) identified criteria used in the definition of IRCT and (2) investigated the current state of those criteria in prospective surgical therapeutic trials.
Methods
This scoping review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews. PubMed, Scopus, and Web of Science were searched in March 2023. Studies were screened against predetermined inclusion and exclusion criteria. Criteria regarding clinical symptoms, preoperative images, and intraoperative findings were captured respectively.
Results
A total of 41 prospective studies were eligible for inclusion, and 35 studies (85.4%) defined IRCT. IRCT was defined on the basis of the following main criteria: preoperative image findings (28/35), intraoperative findings (24/35), and symptoms (16/35). With regard to preoperative images, IRCT was mainly defined on the basis of retraction of the tendon in the coronal plane (22/28), the severity of fatty degeneration (19/28), and ruptured tendon number or width of the defect in the sagittal plane (17/28).
Conclusion
This scoping review highlights the lack of a standardized definition for IRCT in clinical practice, with common predictive criteria including a duration of over 6 months, retraction beyond 5 cm, Goutallier grade 3 fatty infiltration, and the rupture of two or more tendons. However, surgeons should apply more than one criterion when examining preoperative images and confirm reparability during surgery. A more objective manner of evaluating intraoperative reparability is necessary.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12891-023-07067-5.
Keywords: Irreparable rotator cuff tear, Retraction, Patte grade, Fatty degeneration, Tangent sign
Introduction
Rotator cuff tears (RCTs) are the most common shoulder disease in patients with shoulder problems, and the reported prevalence is up to 20% in the general population [1]. Among RCTs, irreparable rotator cuff tears (IRCTs) present a significant challenge to orthopedic surgeons because of the high failure rate of repair [2]. Various treatment strategies have been reported, but the optimal therapy remains controversial [3, 4]. This controversy results from both the lack of high-quality comparative studies and the unclear definition of IRCT.
Some surgeons define IRCTs on the basis of their size and the number of tendons involved. Cofield et al. define a tear larger than 5 cm as a massive tear [5], and Gerber et al. describe a massive rotator cuff tear as involving two or more tendons [6]. However, tear size and reparability are not always related. Denard et al. [7] identified that up to 80% of massive RCTs are completely repairable. They indicated that a massive tear displayed in preoperative images is not necessarily irreparable, and irreparable tears are not necessarily large in size.
IRCT can also be defined intraoperatively; Warner et al. [8] define them as involving “the inability to achieve a direct repair of the native tendon to the humerus despite mobilizing the soft tissue.” However, the ability to achieve direct repair is not only determined by the tendon itself, but also related to the quality of debridement and mobilization and even the surgical technique of the surgeon. Furthermore, surgeons are unable to form a definite preoperative plan if reparability is only determined intraoperatively.
Due to the heterogenous and subjective definitions of IRCT in the literature, surgeons may have difficulty in selecting criteria to define IRCT when performing clinical trials. Thus, this scoping review provides different definitions used to describe IRCTs. This review (1) identified criteria used to define IRCT and (2) investigated the current state of those criteria. We focused on prospective clinical research because diagnosis should occur preoperatively or intraoperatively.
Method
Search strategy
This scoping review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines (Appendix 1) [9]. PubMed, Scopus, and Web of Science were searched in March 2023 using the following keywords: “(irreparable rotator cuff tear) AND (prospective)” in titles, abstracts, or keyword sections (Appendix 2). After the database search, the keywords were entered into Google Scholar to identify potentially relevant omitted studies.
Eligibility criteria
After all publications were identified, duplicates were removed, and study selection was performed by two independent reviewers in two phases. During the first phase, titles and abstracts were reviewed for relevance. In the second phase, full-text articles were examined. A senior author was consulted in cases of disagreement over study inclusion, and these disagreements were resolved by consensus. The references of the included studies were screened using the aforementioned method to prevent the omission of relevant articles.
The selected studies satisfied the following criteria: (1) were prospective clinical studies, (2) included patients who received surgical treatment for IRCT, (3) had IRCT as their main subject, and (4) were written in English.
This systematic review excluded (1) retrospective studies, (2) studies related to diagnosis, nonsurgical treatment, or basic science, letters to editors, systematic reviews or meta-analyses, (3) studies without IRCT as the main subject, (4) studies not written in English, and (5) studies without full-text availability. Studies were assessed for eligibility against the criteria summarized in Table 1.
Table 1.
Inclusion and exclusion criteria for study selection
| Characteristics | Inclusion | Exclusion |
|---|---|---|
| Study availability | Full text is available | Only abstract or title |
| Study type | Original study | Systematic review, letter to editor |
| Study contains |
Therapeutic IRCT as the main subject |
Diagnostic IRCT not the main subject |
| Study design | Prospective | Retrospective |
| Language | English | Other than English |
IRCT, irreparable rotator cuff tear
Data extraction, analysis, and critical appraisal
Data were gathered from all selected studies by two authors. Data on study design, sample size, surgical methods, and the definition of IRCT were gathered. All recorded definitions were copied verbatim to an Excel database, and the criteria embedded in each definition were extracted; these criteria were as follows. The criteria relating to symptoms were duration of shoulder pain or other specific symptoms. The criteria relating to preoperative included tendon retraction, fatty infiltration, ruptured tendon number, and width of the defect in the sagittal plane. The criterion related to intraoperative findings was tendon irreparable after mobilization. We also recorded whether the criteria were part of the definition or the final confirmation. The criteria were listed separately to allow for quantitative, descriptive statistical analysis.
Results
Overview of selected studies
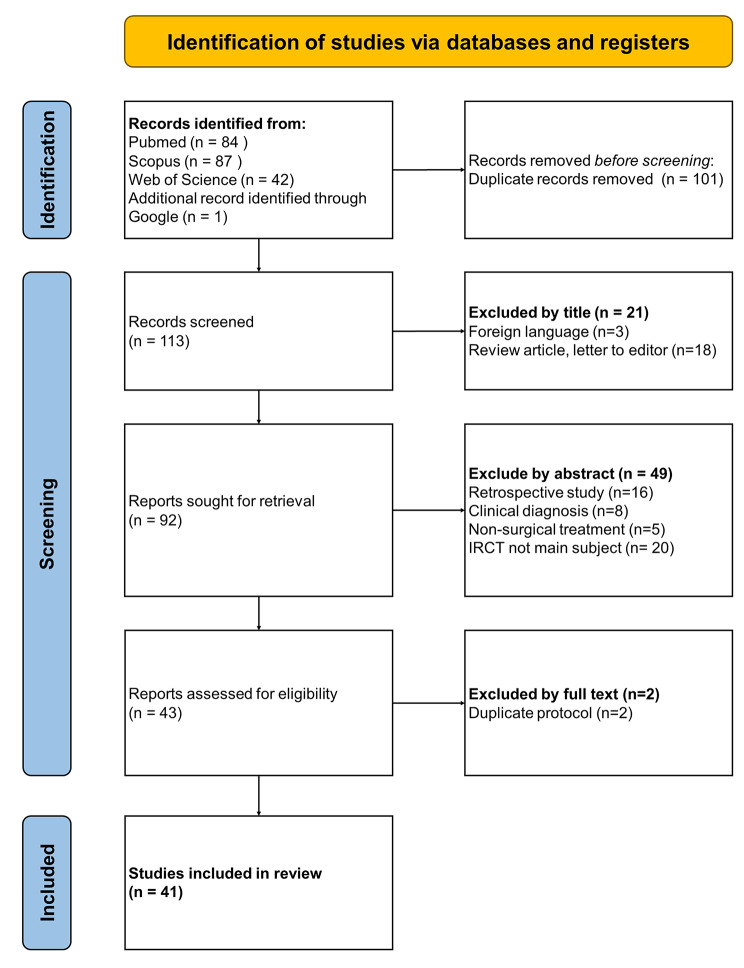
A total of 113 articles were obtained for review. According to our selection criteria, 41 prospective studies published between 1997 and 2022 were suitable for inclusion (Fig. 1). Of the included studies, 32 were case series (78.0%), 6 were nonrandomized control studies (14.6%) and 3 were randomized control studies (7.3%). The reported surgical methods included subacromial spacer placement, partial repair, superior capsule reconstruction, bridging graft, tendon transfer, reverse shoulder arthroplasty (RSA), and other arthroscopic treatment (including debridement, tenodesis, and acromioplasty or tuberoplasty). The characteristics of the included studies are detailed in Table 2.
Fig. 1.
Flowchart of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines
Table 2.
Description of included studies
| Author (Year) | Journal/Book | Surgical method | Number of the patient | Definition | ||
|---|---|---|---|---|---|---|
| Clinical symptoms | Preoperative images | Intraoperative findings | ||||
| Randomized control study | ||||||
| Verma, N. et al. (2022) [36] | J Bone Joint Surg Am | Subacromial spacer | 93 | V | V | |
| Partial repair | 91 | |||||
| Ono, Y. et al. (2022) [37] | Arthroscopy | SCR | 25 | V | V | |
| BG | 25 | |||||
| Ozturk, B. Y. et al. (2021) [38] | J Shoulder Elbow Surg | Tendon transfer | 21 | V | ||
| SCR | 21 | |||||
| Non-randomized control study | ||||||
| Kandeel, A. A. (2023) [39] | Orthop J Sports Med | Partial repair + SCR | 15 | V | V | |
| Partial repair + SCR + Tendon transfer | 9 | |||||
| Greiner, S. et al. (2021) [40] | Orthop J Sports Med | SCR | 20 | V | V | |
| Partial repair | 20 | |||||
| Cavalier, M. et al. (2018) [41] | Orthop Traumatol Surg Res | Non-operative | 71 | V | ||
| Others | 26 | |||||
| Partial repair | 61 | |||||
| Tendon transfer | 25 | |||||
| RSA | 35 | |||||
| Kolk, A. et al. (2018) [42] | Bone Joint J | Tendon transfer | 39 | V | ||
| Pandey, R. et al(2017) [43] | Shoulder Elbow | Partial repair | 13 | V | V | V |
| Partial repair with BG | 13 | |||||
| Franceschi, F. et al. (2015) [44] | Knee Surg Sports Traumatol Arthrosc | Others | 34 | V | ||
| Partial repair | 34 | |||||
| Case series | ||||||
| Dhir, R. et al. (2022) [45] | JSES Reviews, Reports, and Techniques | Subacromial spacer | 4 | V | ||
| Gbejuade, H. et al. (2022) [46] | Shoulder Elbow | SCR | 17 | V | V | V |
| Shin, S. J. et al. (2022) [47] | Arthroscopy | SCR | 21 | V | V | |
| Reinares, F. et al. (2022) [48] | Eur J Orthop Surg Traumatol | Tendon transfer | 15 | V | V | |
| Liao, Y. T. et al. (2022) [49] | J Orthop Surg Res | SCR | 19 | |||
| Haque, A. et al. (2021) [50] | J Clin Orthop Trauma | BG | 22 | V | V | V |
| Familiari, F. et al. (2021) [51] | Arthroscopy | Subacromial spacer | 51 | V | V | |
| Zafra, M. et al. (2021) [52] | J Orthop | SCR | 5 | V | V | |
| Lacheta, L. et al. (2020) [53] | Arthroscopy | SCR | 22 | V | V | |
| Ulstrup, A. et al. (2020) [54] | JSES Int | SCR | 13 | V | V | V |
| Azevedo, C. I. C. et al. (2020) [55] | Am J Sports Med | SCR | 22 | V | ||
| Polacek, M. (2019) [56] | Arthrosc Sports Med Rehabil | SCR | 19 | V | V | |
| Mirzaee, F. et al. (2019) [57] | Arch Bone Jt Surg | Others | 12 | |||
| Valenti, P. et al. (2019) [58] | Int Orthop | Tendon transfer | 31 | V | V | |
| Matsen, F. A., 3rd et al. (2019) [59] | Int Orthop | Others | 40 | V | ||
| Iban, M. A. R. et al. (2018) [60] | Knee Surgery Sports Traumatology Arthroscopy | Subacromial spacer | 15 | V | V | V |
| Yallapragada, R. K. et al. (2018) [61] | J Orthop | Subacromial spacer | 14 | V | V | |
| Piekaar, R. S. M. et al(2018) [62] | Musculoskelet Surg | Subacromial spacer | 44 | |||
| Ruiz Iban, M. A. et al(2018) [63] | Knee Surg Sports Traumatol Arthrosc | Subacromial spacer | 15 | V | V | V |
| Denard, P. J. et al. (2018) [64] | Arthroscopy | SCR | 59 | |||
| Hirahara, A. M. et al. (2017) [65] | Am J Orthop (Belle Mead NJ) | SCR | 9 | |||
| Kany, J. et al. (2016) [66] | Eur J Orthop Surg Traumatol | Tendon transfer | 5 | V | ||
| Grimberg, J. et al. (2015) [67] | Arthroscopy | Tendon transfer | 54 | V | V | |
| Modi A, et al. (2013) [68] | Shoulder Elbow | BG | 61 | V | V | |
| Senekovic, V. et al. (2013) [69] | Eur J Orthop Surg Traumatol | Subacromial spacer | 20 | V | V | |
| Gupta, A. K. et al. (2013) [70] | Am J Sports Med | BG | 26 | V | V | V |
| Henseler, J. F. et al. (2013) [71] | Bone Joint J | Tendon transfer | 28 | V | ||
| Gupta, A. K. et al. (2012) [72] | Am J Sports Med | BG | 24 | V | V | V |
| John, M. et al. (2010) [73] | Int Orthop | RSA | 15 | V | V | |
| Gerber, C. et al. (2006) [74] | J Bone Joint Surg Am | Tendon transfer | 14 | |||
| Malkani, A. L. et al. (2004) [75] | Clin Orthop Relat Res | Tendon transfer | 18 | V | ||
| Gartsman, G. M. (1997) [76] | J Bone Joint Surg Am | Others | 33 | V | V | |
BG, bridging grafting; RSA, reverse shoulder arthroplasty; SCR, superior capsule reconstruction
Definition of IRCT
In total, 35 studies (85.4%; 35/41) defined IRCT. IRCT was defined on the basis of criteria relating to preoperative image findings (80.0%; 28/35), intraoperative findings (68.6%, 24/35), and symptoms (45.7%, 16/35). In the remaining six eligible studies (14.6%, 6/41), the full-text article did not contain any definition of IRCT, even though each article described IRCT as its main study subject. The details of the three main criteria are listed in Table 3.
Table 3.
Definition of irreparable rotator cuff tears in prospective surgical therapeutic trials
| Classification | Characteristics | Detail | Number of articles | Reference |
|---|---|---|---|---|
| Symptoms | Duration of symptoms | ≥ 6 months | 13 | [38, 43, 44, 46–48, 51, 56, 60, 63, 69, 70, 72] |
| ≥ 3 months | 2 | [50, 54] | ||
| Pseudoparalysis | 1 | [73] | ||
| Images | Tendon retraction | Retraction ≥ 5 cm | 9 | [36, 37, 43, 46, 50, 56, 70, 72, 76] |
| Retraction ≥ 3 cm | 5 | [51, 60, 63, 68, 71] | ||
| ≥ Patte grade 3 | 6 | [40, 45, 48, 53, 61, 67] | ||
| ≥ Patte grade 2 | 2 | [39, 42] | ||
| Fatty infiltration | ≥ Goutallier grade 3 (or infiltration ≥ 50%) | 11 | [39, 40, 45, 51–54, 60, 61, 63, 67] | |
| ≥ Goutallier grade 2 (or ≥ Fuchs grade 2) | 5 | [41, 42, 48, 58, 73] | ||
| Goutallier grade 1–3 | 1 | [70] | ||
| Goutallier grade 4 | 2 | [56, 66] | ||
| Ruptured tendon number or width of the defect in sagittal plain | ≥ 2 tendons | 12 | [36, 37, 41, 42, 46, 48, 50, 58, 67, 68, 70, 76] | |
| Anterior to posterior defect ≥ 5 cm | 1 | [39] | ||
| Anterior to posterior defect ≥ 3 cm | 3 | [51, 60, 63] | ||
| ≥ Bayne and Bateman grade 3 | 1 | [40] | ||
| Muscle atrophy | ≥ Thomazeau grade 3 | 2 | [39, 53] | |
| Positive tangent sign | 1 | [54] | ||
| Other – Defect area | Davidson group 3 | 1 | [42] | |
| Other – AH interval | ≤ 6 mm AHD | 1 | [52] | |
| Intraoperative finding | Irreparable after mobilization | Act as final conform | 18 | [36, 37, 40, 43, 46, 47, 50, 52, 53, 55, 59–61, 68–70, 75, 76] |
| Part of the criteria | 5 | [54, 58, 63, 67, 72] | ||
| Poor tendon quality | Part of the criteria | 1 | [39] |
AHD, acromial humeral distance
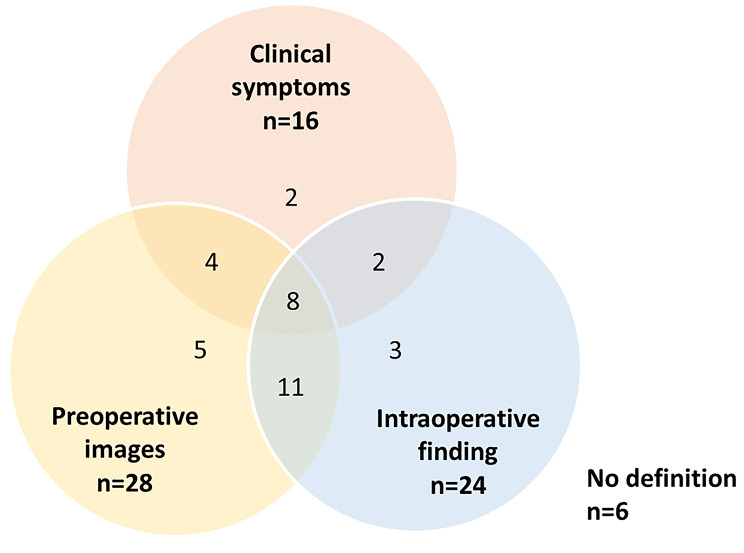
Of the 35 studies that defined IRCT, 8 (22.9%) used all three main criteria to define IRCT. In 17 (48.6%) studies, two different main criteria were applied, of which the combination of intraoperative findings and preoperative images was most common. In 10 (28.6%) studies, only one main criteria was used, which most commonly related to preoperative images (Fig. 2).
Fig. 2.
Venn diagram displaying number of studies using three main criteria to define irreparable rotator cuff tear
Moreover, there was no significant difference (p = 0.451) in the number of criteria used between randomized controlled studies, non-randomized controlled studies, and case series (Table 4).
Table 4.
The number of used three main criteria and three main preoperative image factors in predicting irreparable rotator cuff tears between different level articles
| Randomized control study |
Non-randomized control study | Case series | P-value | |
|---|---|---|---|---|
| Number of used three main criteria | 0.451 | |||
| 0 | 0 | 0 | 6 | |
| 1 | 1 | 3 | 6 | |
| 2 | 2 | 2 | 13 | |
| 3 | 0 | 1 | 7 | |
| Number of used three main preoperative image factors | 0.787 | |||
| 0 | 1 | 1 | 11 | |
| 1 | 0 | 1 | 5 | |
| 2 | 2 | 2 | 10 | |
| 3 | 0 | 2 | 6 |
Definition of clinical symptoms
Among the studies providing a definition of IRCT, 45.7% (16/35) applied clinical criteria. The most common clinical feature was symptoms lasting for more than 6 months after conservative treatment followed by symptoms lasting for more than 3 months.
Definition of preoperative findings
In total, 28 studies used preoperative image findings to define IRCT. In these studies, IRCT was defined on the basis of the following characteristics: retraction of the tendon in the coronal plane (22/28, 78.6%), the severity of fatty degeneration (19/28, 67.9%), and ruptured tendon number or width of the defect in the sagittal plane (17/28, 60.7%). Other characteristics included the severity of muscle atrophy, defect area, and acromiohumeral distance (Table 3). The utilization of three primary preoperative image factors did not exhibit significant differences (p = 0.787) among randomized controlled studies, non-randomized controlled studies, and case series (Table 4).
For retraction of the tendon in the coronal plane, retraction of more than 5 cm was most commonly used for definitions of IRCT. However, retraction of more than 3 cm and Patte grades [10] 3 and 2 were also used. For fatty infiltration, Goutallier grades [11] 3 and higher were most commonly used for definitions, whereas some authors considered tears of Goutallier grades 2 and higher to also be irreparable. With regard to ruptured tendon number or width of the defect in the sagittal plane, more than two ruptured tendons was mostly considered to indicate irreparability.
Of the 28 studies that used preoperative findings to define IRCT, 8 (28.6%) applied all three main criteria to define IRCT, 14 (50.0%) used two different main criteria, and 6 (21.4%) used only one main criterion (Fig. 3).
Fig. 3.
Venn diagram displaying number of studies using three main preoperative image factors to define irreparable rotator cuff tear
Role of intraoperative findings
The criterion “the tendon is irreparable after mobilization” was used to define IRCT in 23 articles, but the role of this criterion differed. In 18 articles, this criterion was used for final confirmation of irreparability, whereas it was part of the definition in the other 6 articles. “Poor quality of the ruptured tendon” was a criterion used in one article.
Discussion
The present scoping review revealed that clinical symptoms, preoperative images, and intraoperative findings were the three main considerations used to define IRCT. Among preoperative image criteria, tendon retraction, fatty infiltration, and ruptured tendon number or width of defect were primarily used to define IRCT. However, no standardized definition of IRCT is used in clinical trials.
Clinical symptoms are the first criteria used to evaluate patients, but the relationship between clinical symptoms and IRCT is controversial. Although Kuptniratsaikul et al. [12] found that older adulthood (age > 65 years) predicts IRCT, others [13, 14] have not identified this relationship. Pseudoparalysis [15] and lower functional score [13] are also correlated with IRCT. However, these criteria are not widely employed, possibly due to the lack of consensus regarding the definition of pseudoparalysis [16], limited agreement on its diagnosis, and the absence of a clear-cut threshold in the functional score to determine reparability. Anterosuperior escape presents as another robust indicator of IRCT. However, it’s important to note that the treatment for patients exhibiting anterosuperior escape primarily focuses on addressing the associated arthropathy, rather than the rotator cuff itself. As a result, this aspect is seldom discussed in articles pertaining to IRCT. The present review observed that the duration of symptoms was listed in the inclusion criteria for patients with IRCTs in 13 articles, but this was rarely applied as a single criterion. This indicates that this criterion is applied for screening rather than definitive diagnosis.
Preoperative images were used in 80% of the articles to define IRCT, but these criteria were heterogenous. Tendon retraction is correlated with reparability [12, 13, 17, 18] and retear rate [19]; thus, it was applied as a criterion in most articles. However, the retraction cut-off point for determining reparability was controversial. Reparability is indicated by a medial–lateral tear size of smaller than 26 mm per Park et al. [13], 31 mm per Yoo et al. [20], 36 mm per Kuptniratsaikul et al. [12], and 4.2 cm per Kim et al. [21]. Retraction of Patte grade 3 is also a predictor of IRCT [22, 23], but Patte 2 tears were also considered irreparable in two articles. This discrepancy may be attributed to the cutoff Patte stage of IRCT reported by Kim et al. [21], which is 2.5. Consequently, some authors define both Patte 2 and Patte 3 retractions as IRCT. Moreover, it’s possible that they utilized the definition of a large and massive tear, which stipulates that at least one of the two tendons must retract beyond the apex of the humeral head (Patte 2) [24], to categorize it as IRCT. This could be a contributing factor to the variability in the definition. Additionally, examining only one section to assess tendon retraction was insufficient; Guo et al. [25] used a modified Patte classification by using two coronal sections to provide more accurate predictions of reparability.
Fatty infiltration also exhibited significant correlation with tendon reparability, but the cut-off point varied by article. Goutallier grades 2 and 3 are correlated with irreparability [12–14, 21–23]; thus, both were used to define IRCT. However, the cut-off point for fat infiltration may differ between the supraspinatus and infraspinatus muscles [12, 20, 22]. Surgeons should apply this criterion cautiously. Ruptured tendon number, or width of the defect in the sagittal plane, was another predictor of IRCT with reported cut-off points ranging from 22 to 37 mm [12, 13, 20, 21]. However, only one article used a definite value as a criterion. Others evaluated reparability only according to the number of ruptured tendons in the sagittal plane, which is easily assessed in clinical practice.
Factors related to muscle atrophy, such as the tangent sign [15, 21, 22] and muscle occupation ratio [17, 26]) are frequently employed criteria for defining IRCT. It is worth knowing that the tangent sign, which assesses the failure of the supraspinatus to cross a line extending from the superior border of the coracoid process to the superior border of the scapular spine, is a readily performed and reproducible tool with good intraobserver and interobserver reliability [27]. Moreover, it exhibits a high level of accuracy, with a substantial odds ratio for predicting IRCT [28]. In addition to the aforementioned criteria, humeral head upper migration (acromiohumeral interval [13] and inferior glenohumeral distance [21]), and ultrasonography images [29–31] have also been used to evaluate reparability. Surgeons can also use those factors to identify IRCT before surgery when performing prospective clinical studies.
IRCT was defined on the basis of the inability to achieve direct repair after mobilization in 23 of 35 articles. Although this is considered the gold standard for defining repairability in patients with RCTs [15, 22], it was not applied in all articles. This may be because defining irreparability intraoperatively is subjective because no consensus exists, despite the ability of surgeons to intuitively recognize irreparability. To evaluate reparability, repair tension can also be measured. Repair tension is correlated with preoperative retraction and postoperative integrity [32]. Repair tension of more than 30 to 35 N is related to a high retear rate and may not indicate primary repair [33, 34]. Nonetheless, repairability is determined only intraoperatively, not preoperatively, which can complicate surgical decision-making.
Another finding of this scoping review is that more than two factors were applied to define IRCT in approximately 70% of the articles. More than two preoperative image finding factors were used to define IRCT in more than 75% of the articles that included image findings within their criteria. This indicates that surgeons attempt to select patients with relatively strict criteria. Kim et al. [22] and Prasathaporn [35] also identified that the specificity of prediction increases with the application of multiple factors. Moreover, each factor may contribute to prediction of reparability to a different extent. Kim et al. [15] and Park et al. [13] designed a scoring system with different weightings for each factor to predict the reparability of rotator cuffs. The scoring system can also be used to select patients for studies related to IRCT.
The current review has some limitations. First, our aim was to incorporate high-quality publications and gain insight into the criteria established prior to surgery rather than postoperatively. Unfortunately, this exclusion of retrospective studies might have resulted in missing potentially valuable insights from such studies. Second, this was a deliberate choice because our analysis focused solely on the “criteria” presented in the articles, rather than their outcomes. However, this selection may impact the results of this scoping review. Third, the inclusion criteria in each article may have been affected by the surgical methods used. For example, patients who expected to receive RSA may not have been assessed for rotator cuff reparability during operation, and surgeons may have administered debridement only to older patients. Finally, this article primarily addressed the criteria for selecting IRCT patients, but it did not delve into the actual relationship between these criteria and IRCT. Future research endeavors could center on examining the clinical evidence associated with these criteria and assessing their predictive capability for IRCT.
While this scoping review reveals the absence of a standardized definition for IRCT in clinical practice, certain criteria were commonly employed to predict IRCT. These criteria encompass a duration of more than 6 months, retraction exceeding 5 cm, Goutallier grade 3 in fatty infiltration, and the rupture of two or more tendons. However, a more objective manner of evaluating intraoperative reparability is necessary.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We thank Medical Device R & D Core Laboratory, National Cheng Kung University Hospital, Tainan, Taiwan, and Ms. Shing-Yun Chang BS, MSc (Department of Orthopedic Surgery, National Cheng Kung University Hospital, College of Medicine, National Cheng Kung University, Tainan, Taiwan) for assistance with this project.
We thank the Skeleton Materials and Bio-compatibility Core Lab, Research Center of Clinical Medicineand Ministry of Science and Technology (MOST 111-2314-B-006-058) for the assistance of this project.
Authors’ contributions
K.L.H: Conceptualization, Writing – original draft preparation. F.C.K, C.A.S: Methodology and software. W.R.S: Supervision. A.V.G: Writing – review and editing. T.K: Investigation and resources. N.I: Data Curation. All authors reviewed the manuscript.
Funding
Not applicable.
Data Availability
All data included in this study are available upon request by contact with the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare that there are no conflicts of interest regarding the publication of this article.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Minagawa H, Yamamoto N, Abe H, Fukuda M, Seki N, Kikuchi K, Kijima H, Itoi E. Prevalence of symptomatic and asymptomatic rotator cuff tears in the general population: from mass-screening in one village. J Orthop. 2013;10(1):8–12. doi: 10.1016/j.jor.2013.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chung SW, Kim JY, Kim MH, Kim SH, Oh JH. Arthroscopic repair of massive rotator cuff tears: outcome and analysis of factors associated with healing failure or poor postoperative function. Am J Sports Med. 2013;41(7):1674–83. doi: 10.1177/0363546513485719. [DOI] [PubMed] [Google Scholar]
- 3.Kovacevic D, Suriani RJ, Jr, Grawe BM, Yian EH, Gilotra MN, Hasan SA, Srikumaran U, Hasan SS, Cuomo F, Burks RT, et al. Management of irreparable massive rotator cuff tears: a systematic review and meta-analysis of patient-reported outcomes, reoperation rates, and treatment response. J Shoulder Elb Surg / Am Shoulder Elb Surg [et al] 2020;29(12):2459–75. doi: 10.1016/j.jse.2020.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cvetanovich GL, Waterman BR, Verma NN, Romeo AA. Management of the irreparable rotator cuff tear. J Am Acad Orthop Surg. 2019;27(24):909–17. doi: 10.5435/JAAOS-D-18-00199. [DOI] [PubMed] [Google Scholar]
- 5.Cofield RH, Parvizi J, Hoffmeyer PJ, Lanzer WL, Ilstrup DM, Rowland CM. Surgical repair of chronic rotator cuff tears. A prospective long-term study. J bone Joint Surg Am Volume. 2001;83(1):71–7. doi: 10.2106/00004623-200101000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J bone Joint Surg Am Volume. 2000;82(4):505–15. doi: 10.2106/00004623-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Denard PJ, Jiwani AZ, Ladermann A, Burkhart SS. Long-term outcome of arthroscopic massive rotator cuff repair: the importance of double-row fixation. Arthroscopy. 2012;28(7):909–15. doi: 10.1016/j.arthro.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 8.Warner JJ, Parsons, IMt Latissimus dorsi tendon transfer: a comparative analysis of primary and salvage reconstruction of massive, irreparable rotator cuff tears. J Shoulder Elb Surg / Am Shoulder Elb Surg [et al] 2001;10(6):514–21. doi: 10.1067/mse.2001.118629. [DOI] [PubMed] [Google Scholar]
- 9.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, et al. PRISMA Extension for scoping reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–73. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 10.Patte D. Classification of rotator cuff lesions. Clin Orthop Relat Res 1990(254):81–6. [PubMed]
- 11.Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res 1994(304):78–83. [PubMed]
- 12.Kuptniratsaikul V, Laohathaimongkol T, Umprai V, Yeekian C, Prasathaporn N. Pre-operative factors correlated with arthroscopic reparability of large-to-massive rotator cuff tears. BMC Musculoskelet Disord. 2019;20(1):111. doi: 10.1186/s12891-019-2485-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Park I, Kang JS, Lee HA, Jo YG, Shin SJ. A Novel Reparability Assessment Scoring System for full-thickness rotator cuff tears. Orthop J Sports Med. 2020;8(8):2325967120940979. doi: 10.1177/2325967120940979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Park SH, Choi CH, Yoon HK, Ha JW, Lee C, Chung K. What can the radiological parameters of superior migration of the humeral head tell us about the reparability of massive rotator cuff tears? PLoS ONE. 2020;15(4):e0231843. doi: 10.1371/journal.pone.0231843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim IB, Jung DW, Suh KT. Prediction of the irreparability of Rotator Cuff tears. Arthroscopy. 2018;34(7):2076–84. doi: 10.1016/j.arthro.2018.02.033. [DOI] [PubMed] [Google Scholar]
- 16.Verma NN, Dasari SP, Menendez ME, Khan ZA, Vadhera AS, Garrigues GE, Nicholson GP, Group P. Minimal inter-surgeon agreement on the diagnosis of pseudoparalysis in patients with massive rotator cuff tears. J Shoulder Elb Surg / Am Shoulder Elb Surg [et al] 2023;32(9):1960–6. doi: 10.1016/j.jse.2023.03.014. [DOI] [PubMed] [Google Scholar]
- 17.Dwyer T, Razmjou H, Henry P, Gosselin-Fournier S, Holtby R. Association between pre-operative magnetic resonance imaging and reparability of large and massive rotator cuff tears. Knee Surg Sports Traumatol Arthrosc. 2015;23(2):415–22. doi: 10.1007/s00167-013-2745-z. [DOI] [PubMed] [Google Scholar]
- 18.Lambers Heerspink FO, Dorrestijn O, van Raay JJ, Diercks RL. Specific patient-related prognostic factors for rotator cuff repair: a systematic review. J Shoulder Elb Surg / Am Shoulder Elb Surg [et al] 2014;23(7):1073–80. doi: 10.1016/j.jse.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 19.Kim YK, Jung KH, Kim JW, Kim US, Hwang DH. Factors affecting rotator cuff integrity after arthroscopic repair for medium-sized or larger cuff tears: a retrospective cohort study. J Shoulder Elb Surg / Am Shoulder Elb Surg [et al] 2018;27(6):1012–20. doi: 10.1016/j.jse.2017.11.016. [DOI] [PubMed] [Google Scholar]
- 20.Yoo JC, Ahn JH, Yang JH, Koh KH, Choi SH, Yoon YC. Correlation of arthroscopic repairability of large to massive rotator cuff tears with preoperative magnetic resonance imaging scans. Arthroscopy. 2009;25(6):573–82. doi: 10.1016/j.arthro.2008.12.015. [DOI] [PubMed] [Google Scholar]
- 21.Kim SJ, Park JS, Lee KH, Lee BG. The development of a quantitative scoring system to predict whether a large-to-massive rotator cuff tear can be arthroscopically repaired. The bone & Joint Journal. 2016;98–B(12):1656–61. doi: 10.1302/0301-620X.98B12.BJJ-2016-0316. [DOI] [PubMed] [Google Scholar]
- 22.Kim JY, Park JS, Rhee YG. Can Preoperative magnetic resonance imaging predict the reparability of massive rotator cuff tears? Am J Sports Med. 2017;45(7):1654–63. doi: 10.1177/0363546517694160. [DOI] [PubMed] [Google Scholar]
- 23.Di Benedetto P, Beltrame A, Cicuto C, Battistella C, Gisonni R, Cainero V, Causero A. Rotator cuff tears reparability index based on pre-operative MRI: our experience. Acta Biomed. 2019;90(1–S):36–46. doi: 10.23750/abm.v90i1-S.8074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ladermann A, Denard PJ, Collin P. Massive rotator cuff tears: definition and treatment. Int Orthop. 2015;39(12):2403–14. doi: 10.1007/s00264-015-2796-5. [DOI] [PubMed] [Google Scholar]
- 25.Guo S, Zhu Y, Song G, Jiang C. Assessment of Tendon Retraction in large to massive rotator cuff tears: a modified patte classification based on 2 coronal sections on preoperative magnetic resonance imaging with higher specificity on Predicting Reparability. Arthroscopy. 2020;36(11):2822–30. doi: 10.1016/j.arthro.2020.06.023. [DOI] [PubMed] [Google Scholar]
- 26.Jeong JY, Chung PK, Lee SM, Yoo JC. Supraspinatus muscle occupation ratio predicts rotator cuff reparability. J Shoulder Elb Surg / Am Shoulder Elb Surg [et al] 2017;26(6):960–6. doi: 10.1016/j.jse.2016.11.001. [DOI] [PubMed] [Google Scholar]
- 27.Kissenberth MJ, Rulewicz GJ, Hamilton SC, Bruch HE, Hawkins RJ. A positive tangent sign predicts the repairability of rotator cuff tears. J Shoulder Elb Surg / Am Shoulder Elb Surg [et al] 2014;23(7):1023–7. doi: 10.1016/j.jse.2014.02.014. [DOI] [PubMed] [Google Scholar]
- 28.Sheean AJ, Hartzler RU, Denard PJ, Ladermann A, Sanders TG, Zlatkin MB, Burkhart SS. Preoperative radiographic risk factors for incomplete arthroscopic Supraspinatus Tendon repair in massive rotator cuff tears. Arthroscopy. 2018;34(4):1121–7. doi: 10.1016/j.arthro.2017.09.046. [DOI] [PubMed] [Google Scholar]
- 29.Chen PC, Wu KT, Chen YC, Huang YC, Chang CD, Lin WC, Chou WY. Predicting the surgical reparability of large-to-massive rotator cuff tears by B-mode ultrasonography: a cross-sectional study. Ultrasonography. 2022;41(1):177–88. doi: 10.14366/usg.20192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cox JL, Laughlin MS, Elkousy HA, Baker HM, Badman BL, Ziegler DW, Buford DA, Kruse KK. Determination of rotator cuff tear reparability: an ultrasound-based investigation. JSES Int. 2023;7(1):21–4. doi: 10.1016/j.jseint.2021.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tseng YH, Chou WY, Wu KT, Chang CD, Chen YC, Huang YC, Lin WC, Chen PC. Use sonoelastography to predict the reparability of large-to-massive rotator cuff tears. Med (Baltim) 2020;99(27):e21139. doi: 10.1097/MD.0000000000021139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Takeda Y, Fujii K, Suzue N, Miyatake K, Kawasaki Y, Yokoyama K. Repair tension during arthroscopic rotator cuff repair is correlated with preoperative Tendon Retraction and Postoperative Rotator Cuff Integrity. Arthroscopy. 2021;37(9):2735–42. doi: 10.1016/j.arthro.2021.03.069. [DOI] [PubMed] [Google Scholar]
- 33.Yokoya S, Nakamura Y, Harada Y, Negi H, Matsushita R, Matsubara N, Sumimoto Y, Adachi N. Effectiveness of measuring tension during arthroscopic rotator cuff repair. J Exp Orthop. 2021;8(1):21. doi: 10.1186/s40634-021-00341-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Park SG, Shim BJ, Seok HG. How much Will High Tension adversely affect Rotator Cuff Repair Integrity? Arthroscopy 2019, 35(11):2992–3000. [DOI] [PubMed]
- 35.Prasathaporn N, Kuptniratsaikul V, Thamrongskulsiri N, Itthipanichpong T. Accuracy of the rotator cuff reparability score. World J Orthop. 2022;13(12):1038–46. doi: 10.5312/wjo.v13.i12.1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Verma N, Srikumaran U, Roden CM, Rogusky EJ, Lapner P, Neill H, Abboud JA. On behalf of the SG: InSpace Implant Compared with partial repair for the treatment of full-thickness massive rotator cuff tears: a Multicenter, Single-Blinded, randomized controlled trial. J bone Joint Surg Am Volume. 2022;104(14):1250–62. doi: 10.2106/JBJS.21.00667. [DOI] [PubMed] [Google Scholar]
- 37.Ono Y, LeBlanc J, Bois AJ, Tsuchiya S, Thangarajah T, More KD, Lo IKY. Graft Healing is more important than graft technique: Superior Capsular Reconstruction Versus bridging Grafts-A prospective Randomized Controlled Trial. Arthroscopy. 2022;38(12):3109–17. doi: 10.1016/j.arthro.2022.06.033. [DOI] [PubMed] [Google Scholar]
- 38.Ozturk BY, Ak S, Gultekin O, Baykus A, Kulduk A. Prospective, randomized evaluation of latissimus dorsi transfer and superior capsular reconstruction in massive, irreparable rotator cuff tears. J Shoulder Elb Surg / Am Shoulder Elb Surg [et al] 2021;30(7):1561–71. doi: 10.1016/j.jse.2021.01.036. [DOI] [PubMed] [Google Scholar]
- 39.Kandeel AA. Middle Trapezius Tendon transfer for augmentation of in situ Superior Capsular Reconstruction-Reinforced partial rotator cuff repair: short-term outcomes of a prospective cohort study. Orthop J Sports Med. 2023;11(2):23259671221147537. doi: 10.1177/23259671221147537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Greiner S, Kaeaeb M, Voss A, Lawton R, Bhide P, Achenbach L. Comparison of Superior Capsular Reconstruction and partial Infraspinatus repair: a matched-pair analysis of irreparable rotator cuff tears. Orthop J Sports Med. 2021;9(2):2325967120984264. doi: 10.1177/2325967120984264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cavalier M, Jullion S, Kany J, Grimberg J, Lefebvre Y, Oudet D, Grosclaude S, Charousset C, Boileau P, Joudet T, et al. Management of massive rotator cuff tears: prospective study in 218 patients. Orthop Traumatol Surg Res. 2018;104(8S):193–S197. doi: 10.1016/j.otsr.2018.09.007. [DOI] [PubMed] [Google Scholar]
- 42.Kolk A, Henseler JF, Overes FJ, Nagels J, Nelissen R. Teres major tendon transfer in the treatment of irreparable posterosuperior rotator cuff tears: long-term improvement of shoulder function and pain reduction at eight to 12 years’ follow-up. The bone & Joint Journal. 2018;100–B(3):309–17. doi: 10.1302/0301-620X.100B3.BJJ-2017-0920.R1. [DOI] [PubMed] [Google Scholar]
- 43.Pandey R, Tafazal S, Shyamsundar S, Modi A, Singh HP. Outcome of partial repair of massive rotator cuff tears with and without human tissue allograft bridging repair. Shoulder Elb. 2017;9(1):23–30. doi: 10.1177/1758573216665114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Franceschi F, Papalia R, Vasta S, Leonardi F, Maffulli N, Denaro V. Surgical management of irreparable rotator cuff tears. Knee Surg Sports Traumatol Arthrosc. 2015;23(2):494–501. doi: 10.1007/s00167-012-2317-7. [DOI] [PubMed] [Google Scholar]
- 45.Dhir R, Prinja A, Singh J, Monga P. The role of biodegradable spacer implantation under local anesthesia for patients with massive rotator cuff tears and significant medical comorbidities. JSES Reviews Reports and Techniques. 2022;2(3):310–4. doi: 10.1016/j.xrrt.2022.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gbejuade H, Patel MS, Singh H, Modi A. Reconstruction of irreparable rotator cuff tears with an acellular dermal matrix in elderly patients without joint arthritis. Shoulder Elb. 2022;14(1 Suppl):83–9. doi: 10.1177/1758573220965535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shin SJ, Lee S, Hwang JY, Lee W, Koh KH. Superior Capsular Reconstruction using Acellular dermal allograft combined with remaining Rotator Cuff Augmentation Improved Shoulder Pain and function at 1 year after the Surgery. Arthroscopy. 2022;38(4):1089–98. doi: 10.1016/j.arthro.2021.10.027. [DOI] [PubMed] [Google Scholar]
- 48.Reinares F, Calvo A, Bernal N, Lizama P, Valenti P, Toro F. Arthroscopic-assisted latissimus dorsi transfer for irreparable posterosuperior cuff tears: clinical outcome of 15 patients. Eur J Orthop Surg Traumatology: Orthopedie Traumatologie. 2022;32(4):667–74. doi: 10.1007/s00590-021-03025-w. [DOI] [PubMed] [Google Scholar]
- 49.Liao YT, Li HS, Li Y, Tang KL, Li J, Zhou BH. Revascularization character of autologous fascia lata graft following shoulder superior capsule reconstruction by enhanced magnetic resonance imaging. J Orthop Surg Res. 2022;17(1):485. doi: 10.1186/s13018-022-03375-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Haque A, Pal Singh H, Pandey R. Treatment of massive irreparable rotator cuff tears using dermal allograft bridging reconstruction. J Clin Orthop Trauma. 2021;22:101593. doi: 10.1016/j.jcot.2021.101593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Familiari F, Nayar SK, Russo R, De Gori M, Ranuccio F, Mastroianni V, Giuzio E, Galasso O, Gasparini G, McFarland EG, et al. Subacromial balloon spacer for massive, irreparable rotator cuff tears is Associated with improved shoulder function and high patient satisfaction. Arthroscopy. 2021;37(2):480–6. doi: 10.1016/j.arthro.2020.09.048. [DOI] [PubMed] [Google Scholar]
- 52.Zafra M, Uceda P. Arthroscopic superior capsule reconstruction using semitendinosus tendon autograft for irreparable rotator cuff tears: preliminary results. J Orthop. 2021;28:107–11. doi: 10.1016/j.jor.2021.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lacheta L, Horan MP, Schairer WW, Goldenberg BT, Dornan GJ, Pogorzelski J, Millett PJ. Clinical and Imaging outcomes after Arthroscopic Superior Capsule Reconstruction with Human dermal allograft for irreparable Posterosuperior Rotator Cuff tears: a minimum 2-Year Follow-Up. Arthroscopy. 2020;36(4):1011–9. doi: 10.1016/j.arthro.2019.12.024. [DOI] [PubMed] [Google Scholar]
- 54.Ulstrup A, Reinhold M, Falster O. Superior capsular reconstruction: 2-year follow-up results. JSES Int. 2020;4(4):893–9. doi: 10.1016/j.jseint.2020.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Azevedo CIC, Catarina Leiria Pires Gago Angelo A, Campos-Correia D, Delgado L, Ferreira N, Sevivas N. Clinical importance of Graft Integrity in Arthroscopic Superior Capsular Reconstruction using a minimally invasively harvested Midthigh Fascia Lata Autograft: 3-Year clinical and magnetic resonance imaging outcomes. Am J Sports Med. 2020;48(9):2115–28. doi: 10.1177/0363546520928649. [DOI] [PubMed] [Google Scholar]
- 56.Polacek M. Arthroscopic Superior Capsular Reconstruction with Acellular Porcine dermal xenograft for the treatment of massive irreparable rotator cuff tears. Arthrosc Sports Med Rehabil. 2019;1(1):e75–e84. doi: 10.1016/j.asmr.2019.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mirzaee F, Aslani MA, Zafarani Z, Aslani H. Treatment of massive irreparable rotator cuff tear with arthroscopic subacromial bursectomy, biceps tenotomy, and Tuberoplasty. Arch Bone Jt Surg. 2019;7(3):263–8. [PMC free article] [PubMed] [Google Scholar]
- 58.Valenti P, Reinares F, Maroun C, Choueiry J, Werthel JD. Comparison of arthroscopically assisted transfer of the latissimus dorsi with or without partial cuff repair for irreparable postero-superior rotator cuff tear. Int Orthop. 2019;43(2):387–94. doi: 10.1007/s00264-018-4016-6. [DOI] [PubMed] [Google Scholar]
- 59.Matsen FA, Whitson A, Jackins SE, Hsu JE. Significant improvement in patient self-assessed comfort and function at six weeks after the smooth and move procedure for shoulders with irreparable rotator cuff tears and retained active elevation. Int Orthop. 2019;43(7):1659–67. doi: 10.1007/s00264-019-04310-4. [DOI] [PubMed] [Google Scholar]
- 60.Iban MAR, Moreno RL, Diaz RR, Sciamanna RA, Gonzalez AP, Gomez AL, Heredia JD. The absorbable subacromial spacer for irreparable posterosuperior cuff tears has inconsistent results. Knee Surg Sport Tr A. 2018;26(12):3848–54. doi: 10.1007/s00167-018-5083-3. [DOI] [PubMed] [Google Scholar]
- 61.Yallapragada RK, Apostolopoulos A, Katsougrakis I, Selvan TP. The use of a subacromial spacer-inspace balloon in managing patients with irreparable rotator cuff tears. J Orthop. 2018;15(3):862–8. doi: 10.1016/j.jor.2018.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Piekaar RSM, Bouman ICE, van Kampen PM, van Eijk F, Huijsmans PE. Early promising outcome following arthroscopic implantation of the subacromial balloon spacer for treating massive rotator cuff tear. Musculoskelet Surg. 2018;102(3):247–55. doi: 10.1007/s12306-017-0525-5. [DOI] [PubMed] [Google Scholar]
- 63.Ruiz Iban MA, Lorente Moreno R, Ruiz Diaz R, Alvarez Sciamanna R, Paniagua Gonzalez A, Lorente Gomez A, Diaz Heredia J. The absorbable subacromial spacer for irreparable posterosuperior cuff tears has inconsistent results. Knee Surg Sports Traumatol Arthrosc. 2018;26(12):3848–54. doi: 10.1007/s00167-018-5083-3. [DOI] [PubMed] [Google Scholar]
- 64.Denard PJ, Brady PC, Adams CR, Tokish JM, Burkhart SS. Preliminary results of Arthroscopic Superior Capsule Reconstruction with Dermal Allograft. Arthroscopy. 2018;34(1):93–9. doi: 10.1016/j.arthro.2017.08.265. [DOI] [PubMed] [Google Scholar]
- 65.Hirahara AM, Andersen WJ, Panero AJ. Superior Capsular Reconstruction: clinical outcomes after Minimum 2-Year Follow-Up. Am J Orthop. 2017;46(6):266–78. [PubMed] [Google Scholar]
- 66.Kany J, Guinand R, Croutzet P, Valenti P, Werthel JD, Grimberg J. Arthroscopic-assisted latissimus dorsi transfer for subscapularis deficiency. Eur J Orthop Surg Traumatology: Orthopedie Traumatologie. 2016;26(3):329–34. doi: 10.1007/s00590-016-1753-3. [DOI] [PubMed] [Google Scholar]
- 67.Grimberg J, Kany J, Valenti P, Amaravathi R, Ramalingam AT. Arthroscopic-assisted latissimus dorsi tendon transfer for irreparable posterosuperior cuff tears. Arthroscopy. 2015;31(4):599–607e591. doi: 10.1016/j.arthro.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 68.Modi A, Singh HP, Pandey R. Management of irreparable rotator cuff tears with the GraftJacket allograft as an interpositional graft. Shoulder Elb. 2013;5(3):188–94. doi: 10.1111/sae.12021. [DOI] [Google Scholar]
- 69.Senekovic V, Poberaj B, Kovacic L, Mikek M, Adar E, Dekel A. Prospective clinical study of a novel biodegradable sub-acromial spacer in treatment of massive irreparable rotator cuff tears. Eur J Orthop Surg Traumatology: Orthopedie Traumatologie. 2013;23(3):311–6. doi: 10.1007/s00590-012-0981-4. [DOI] [PubMed] [Google Scholar]
- 70.Gupta AK, Hug K, Boggess B, Gavigan M, Toth AP. Massive or 2-tendon rotator cuff tears in active patients with minimal glenohumeral arthritis: clinical and radiographic outcomes of reconstruction using dermal tissue matrix xenograft. Am J Sports Med. 2013;41(4):872–9. doi: 10.1177/0363546512475204. [DOI] [PubMed] [Google Scholar]
- 71.Henseler JF, Nagels J, van der Zwaal P, Nelissen RG. Teres major tendon transfer for patients with massive irreparable posterosuperior rotator cuff tears: short-term clinical results. The bone & Joint Journal. 2013;95–B(4):523–9. doi: 10.1302/0301-620X.95B4.30390. [DOI] [PubMed] [Google Scholar]
- 72.Gupta AK, Hug K, Berkoff DJ, Boggess BR, Gavigan M, Malley PC, Toth AP. Dermal tissue allograft for the repair of massive irreparable rotator cuff tears. Am J Sports Med. 2012;40(1):141–7. doi: 10.1177/0363546511422795. [DOI] [PubMed] [Google Scholar]
- 73.John M, Pap G, Angst F, Flury MP, Lieske S, Schwyzer HK, Simmen BR. Short-term results after reversed shoulder arthroplasty (Delta III) in patients with rheumatoid arthritis and irreparable rotator cuff tear. Int Orthop. 2010;34(1):71–7. doi: 10.1007/s00264-009-0733-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gerber C, Maquieira G, Espinosa N. Latissimus dorsi transfer for the treatment of irreparable rotator cuff tears. J bone Joint Surg Am Volume. 2006;88(1):113–20. doi: 10.2106/JBJS.E.00282. [DOI] [PubMed] [Google Scholar]
- 75.Malkani AL, Sundine MJ, Tillett ED, Baker DL, Rogers RA, Morton TA. Transfer of the long head of the triceps tendon for irreparable rotator cuff tears. Clin Orthop Relat Res 2004(428):228–36. [DOI] [PubMed]
- 76.Gartsman GM. Massive, irreparable tears of the rotator cuff. Results of operative debridement and subacromial decompression. – 1997, 79(5):715–721. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data included in this study are available upon request by contact with the corresponding author on reasonable request.