Abstract
Background
Globally, Internet is a recognized form of leisure, but there are growing apprehensions about the increasing number of individuals developing an addiction to it. Recent research has focused on social issues associated with internet addiction (IA). However, the treatment of IA is currently unclear. This study aimed to explore the relationship between IA treatment outcomes and different intervention strategies through systematic review and data analysis of patients who received different intervention modes.
Methods
A meta-analysis was conducted using RevMan 5.4 and Stata 14.2 on 57 literature research data from five Chinese and English databases, PubMed, Embase, Web of Science, Wanfang and CNKI.
Result
A total of 57 randomized controlled trials (RCTs) were included in this network meta-analysis involving 3538 IA patients and 13 different interventions. The network meta-analysis results demonstrated that the top four interventions were: rTMS + CBT, drug + others, rTMS, and electro-acupuncture + CBT.
Conclusion
Our study indicated that comprehensive therapy had an optimal therapeutic effect on IA patients and rTMS + CBT ranked first among all therapeutic indicators of intervention, indicating optimal clinical effectiveness.
Keywords: Internet addiction, Intervention, Network meta-analysis
Background
The internet has revolutionized communication, work, and access to information, becoming an integral part of modern life with numerous benefits and conveniences for users. However, this ubiquitous technology also has a darker side. Concerns about excessive Internet use have been raised in recent years, leading to the concept of Internet addiction (IA). According to statistics, the incidence of IA among Chinese college students is 11% [1]. IA was first proposed by psychologist Goldberg I. In 1996, Young confirmed that IA should be a true clinical psychological disorder [2]. IA was defined as the uncontrolled behavior of accessing the internet without substance, manifested as significant social and psychological impairment of individuals due to excessive use of the internet [3]. Although IA has not yet been formally incorporated into the framework of psychopathology, it is a potential problem both in terms of prevalence and public awareness, with many similarities to existing recognized barriers. Some studies have shown that IA may be related to abnormal activity in multiple brain regions and neurotransmitter systems, such as the prefrontal cortex, amygdala, ventral prefrontal cortex, striatum, and hippocampus [4]. The Anterior Cingulate Cortex is associated with cognitive control, impulse control, and attention regulation, and may play a role in regulating and controlling behavior in IA [5]. The amygdala is involved in emotional regulation and reward processing, and may play a role in emotional factors and reinforcement mechanisms in IA [6]. Symptoms of IA may include loss of control over internet use, preoccupation with online activities, neglect of personal responsibilities, and withdrawal symptoms when internet use is reduced or eliminated [7]. A range of negative consequences are associated with IA, including impaired social functioning, academic and work-related problems, and physical and mental health problems. Research has shown that IA is associated with symptoms of ADHD and depressive disorders [8].
In 2013, Internet gaming addiction (IGD) was first introduced by the American Psychiatric Association in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) and nine diagnostic criteria for IGD were listed [9]. Although both IA and IGD are related to internet usage, IGD is a specific form of IA, which is addiction to internet games. Therefore, IGD is a subcategory of IA.
While cognitive-behavioral therapy (CBT), medication, and group therapy are common treatments for IA, it is true that there is a lack of data on their effectiveness. This is because research on IA treatment is still relatively new and ongoing. More research is needed to fully understand the most effective treatments for IA and how to tailor treatment approaches to individual needs. Research on IA treatment can help us determine which interventions are most effective for individuals with IA and improve prognosis. In the meantime, clinicians may use a combination of different treatments and strategies to help individuals with IA manage their symptoms and improve their quality of life. This article summarizes the effects of different intervention models on IA and explores the relationship between intervention models and effects.
This study focuses on randomized controlled trials (RCTs) as the research object. This study employed network meta-analysis methods to compare the effectiveness of different treatment methods for treating IA. This study aims to provide reference and evidence-based medicine data for clinical diagnosis and therapy by evaluating the impacts of various intervention models on IA and examining the relationship between various intervention techniques and treatment outcomes.
Materials and methods
Inclusion and exclusion standard
Inclusion criteria: (1) Published studies on randomized controlled trials on IA, regardless of whether allocation concealment and blinding were mentioned in Chinese or English language; (2) Study subjects meeting one of two criteria: (a) Diagnosis criteria for IGD in DSM-5, Young's Diagnostic Questionnaire for IA, 1997 American Psychological Association Diagnostic Criteria for IA, or other clinical diagnostic criteria for IA; (b) A score of 40 or higher on either the Internet Addiction Test (IAT) or Chen's Internet Addiction Scale (CIAS) [10–12]; (3) Various scores from relevant internet addiction scales were used as evaluation indicators for the treatment effects of different intervention measures and their combinations; (4) Data extraction was limited to studies with full texts only.
Exclusion criteria: (1) Review systematic reviews; (2) Duplicate literature and non-peer-reviewed material; (3) Studies with outcome indicators that failed to meet the inclusion requirements or had apparent errors or omissions.
Search strategy
To identify studies that comply with the inclusion criteria, computer searches were performed in several databases, including PubMed, Embase, Web of Science, Wanfang, and China’s National Knowledge Infrastructure (CNKI). The databases were searched up to December 31, 2022, using a combination of controlled vocabulary and free text terms according to each database's search rules. The search terms included: Internet gaming addiction, electronic gaming addiction, online gaming, pathological internet use, addictive internet use, gaming disorder, internet addiction, excessive internet use, computer game addiction, internet dependence, efficacy, randomized, drug therapy, psychotherapy, antidepressants, cognitive behavior, randomized controlled, case–control, clinical trial, intervention, bupropion, methylphenidate, aripiprazole, sertraline, and fluoxetine. Two investigators independently conducted computer and manual searches, with a third expert consulted in the event of disagreement.
Data extraction
Two researchers independently conducted literature screening following the predetermined inclusion and exclusion criteria. The retrieved literature was imported into literature management software and initially screened by title and abstract after duplicate removal. This led to a thorough reading of the complete text and the final decision regarding inclusion. All data were cross-checked and extracted from the included literature and any discrepancies were resolved by consultation with a third party. The data extracted included basic information about the literature, intervention measures, and outcome indicators.
Quality assessment
Two researchers strictly assessed the quality of the included studies according to the Cochrane Handbook for Systematic Reviews of Randomized Trials. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration). The tool includes seven items: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other biases. Each item was assessed as "low risk," "unclear risk," and "high risk."
Statistical analysis
The network Meta-analysis package of Stata14.2 was used for network meta-analysis and drawing the network map, and RevMan5.4 was used to evaluate the quality of the included studies. In the statistical process of network meta-analysis, since the outcome measurement indicators of the included studies were continuous data and the scale scoring methods of each study were different, the standard mean difference (SMDs) of different studies and the corresponding 95% confidence intervals (CIs) were used as the effect size to merge the results. First of all, the collected data is tested with the inconsistency model to check whether there is good consistency between the groups and the local areas. If there is consistency, the consistency model is used for further analysis of the data; if the inconsistency is significant, the consistency model cannot be used for subsequent steps. Then, the processed data were sorted using surface under the cumulative ranking curve (SUCRA) values [13], and all the processing results were summarized in a rank-heat map [14] to obtain the ranking of the therapeutic effects of various interventions. The SUCRA value refers to the area under the cumulative sequencing probability curve of an intervention, with the value ranging from 0 to 100%. League tables were also drawn to analyze pairwise comparisons between interventions, including SMD values and 95% confidence intervals. Finally, the funnel plot was drawn using Stata 14.2 to identify whether there was a small sample effect.
Results
Literature search
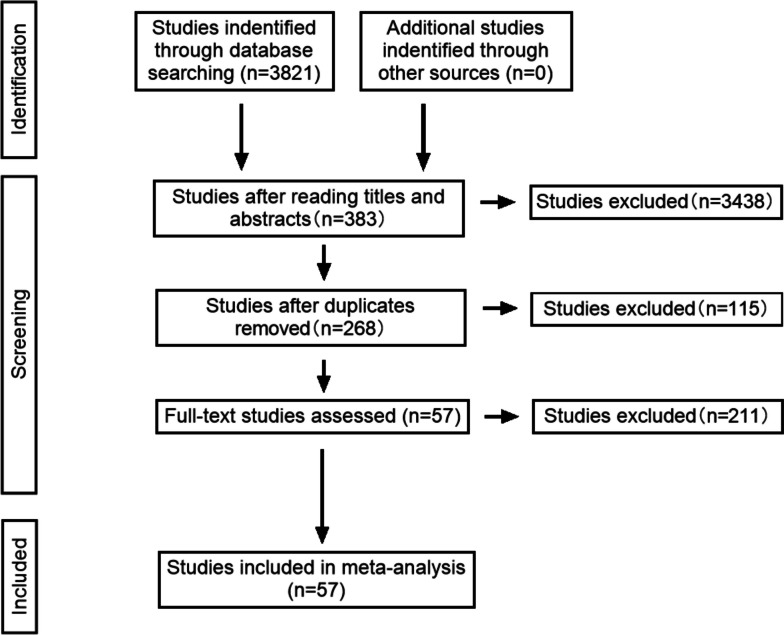
A preliminary search yielded 809 English-language studies and 3012 Chinese-language studies. After reviewing the titles and abstracts, 383 articles remained; following a duplication check and full-text reading, 57 studies were finally included for the network meta-analysis, comprising 63 comparisons. The steps for literature retrieval are shown in Fig. 1.
Fig. 1.
Steps of literature retrieval
Characteristics of the included studies
The characteristics of 57 included studies [3, 15–70] are shown in Table 1, which involved 13 interventions, including psychotherapy/CBT, group psychotherapy, Mindfulness-Based Cognitive Therapy (MBCT), placebo/non-intervention, health education, exercise therapy, electro-acupuncture, drug, EEG biofeedback, rTMS, rTMS + CBT, drug + others, and electro-acupuncture + CBT. A total of 3538 patients with IA were included, and all included studies had comparable descriptions.
Table 1.
Description of included studies
| First author | Year | Gender | Age | Comparison | Sample size | Scale | Treatment time | |
|---|---|---|---|---|---|---|---|---|
| Yuan JJ | 2022 | male:8, female:6/male:9, female:5 | 14.28 ± 1.73/13.92 ± 1.89 | MBCT/Health education | 14/14 | IAT | 7d | |
| Lu ZJ | 2021 | male:7, female:10/male:7, female:9 | not mentioned | Placebo(non-intervention)/Group psychotherapy | 17/16 | IAT | 5w | |
| Zhong YH | 2020 | male:19, female:13/male:22, female:10 | 20.23 ± 4.50/21.62 ± 3.72 | rTMS/Placebo(non-intervention) | 32/32 | IAT | 4w | |
| 2020 | male:19, female:13/male:22, female:10 | 20.23 ± 4.50/21.62 ± 3.72 | rTMS/Placebo(non-intervention) | 32/32 | VAS | 4w | ||
| Zhang LB | 2018 | male:20, female:13/male:19, female:14 | 17.15 ± 2.00/17.18 ± 1.78 | Psychotherapy (CBT)/Health education | 30/30 | IAT | 12w | |
| Cheng GJS | 2017 | male:21, female:4/male:23, female:2 | 15.37 ± 2.31/16.03 ± 1.72 | EEG biofeedback/Group psychotherapy | 25/25 | IAT | 12w | |
| Yu YG | 2017 | not mentioned | not mentioned | Exercise therapy/Placebo(non-intervention) | 26/26 | IAT | 8w | |
| Li M | 2014 | not mentioned | 15.41 ± 1.47/15.62 ± 1.78 | Exercise therapy/Placebo(non-intervention) | 27/24 | IAT | 10w | |
| Zhang CS | 2013 | not mentioned | not mentioned | Exercise therapy/Placebo(non-intervention) | 30/30 | IAT | 16w | |
| Yang Y | 2013 | not mentioned | 20.13 ± 1.77/21.65 ± 2.36 | Electro-acupuncture/Group psychotherapy | 15/14 | IAT | 6w | |
| Wang QZ | 2012 | not mentioned | not mentioned | Psychotherapy (CBT)/Health education | 36/36 | IAT | 12w | |
| Zhu TM | 2011 | male:24, female:15/male:24, female:1/male:25, female:12 | 21.00 ± 1.97/22.53 ± 2.26/ ± 22.41 ± 2.10 | Electro-acupuncture/Psychotherapy(CBT)/ Electro-acupuncture + CBT | 39/36/37 | IAT | 3w | |
| 2011 | male:24, female:15/male:24, female:1/male:25, female:12 | 21.00 ± 1.97/22.53 ± 2.26/ ± 22.41 ± 2.10 | Electro-acupuncture/Psychotherapy(CBT)/ Electro-acupuncture + CBT | 39/36/37 | VAS | 3w | ||
| Zheng WF | 2007 | not mentioned | not mentioned | Group psychotherapy/Placebo(non-intervention) | 30/31 | IAT | 8w | |
| Chen J | 2022 | not mentioned | not mentioned | rTMS + CBT/Psychotherapy(CBT) | 23/22 | IAT | 8w | |
| 2022 | not mentioned | not mentioned | rTMS + CBT/Psychotherapy(CBT) | 23/22 | VAS | 8w | ||
| Peng WX | 2015 | not mentioned | not mentioned | Group psychotherapy/Placebo(non-intervention) | 28/28 | IAT | 8w | |
| Gao J | 2012 | not mentioned | not mentioned | Exercise therapy/Placebo(non-intervention) | 35/34 | IAT | 12w | |
| Yao LH | 2012 | not mentioned | not mentioned | Group psychotherapy/Placebo(non-intervention) | 19/19 | IAT | 12w | |
| Duan SL | 2012 | male:7, female:4/male:7, female:4 | not mentioned | Group psychotherapy/Placebo(non-intervention) | 11/11 | IAT | 13w | |
| Zhang W | 2022 | not mentioned | 19.61 ± 1.19/19.39 ± 1.73 | Placebo(non-intervention)/Exercise therapy | 23/23 | IAT | 12w | |
| Yang WJ | 2022 | male:6, female:16/male:7, female:14 | 19.9 ± 0.8/19.5 ± 0.8 | Placebo(non-intervention)/Group psychotherapy | 22/21 | IAT | 1w | |
| Alavi SS | 2021 | male:14, female:4/male:17, female:6 | 21.7 ± 4.2/21.04 ± 3.7 | Group psychotherapy/Psychotherapy(CBT) | 18/23 | IAT | 12w | |
| Peng W | 2021 | male:24, female:12/male:25, female:12/male:24, female:15 | 22.53 ± 2.26/22.41 ± 2.10/21.00 ± 1.97 | Psychotherapy(CBT)/Electro-acupuncture + CBT/Electro-acupuncture | 36/37/39 | IAT | 6w | |
| Yang Y | 2017 | male:13, female:2/male:13, female:1 | 21.13 ± 1.30/21.65 ± 2.36 | Electro-acupuncture/Group psychotherapy | 15/14 | IAT | 6w | |
| Li H | 2017 | not mentioned | 22.5 ± 2.3/21.0 ± 2.0/22.5 ± 2.0 | Psychotherapy(CBT)/Electro-acupuncture/ Electro-acupuncture + CBT | 36/39/37 | IAT | 6w | |
| Sun JJ | 2022 | not mentioned | 17.36 ± 3.98/18.90 ± 4.45 | rTMS/Placebo(non-intervention) | 31/30 | CIAS | 2w | |
| 2022 | not mentioned | 17.36 ± 3.98/18.90 ± 4.45 | rTMS/Placebo(non-intervention) | 31/30 | VAS | 2w | ||
| Chen D | 2021 | male:24, female:12/male:26, female:12 | 16.89 ± 1.43/16.52 ± 1.26 | Health education/Group psychotherapy | 36/38 | CIAS | 8w | |
| Song GY | 2020 | not mentioned | not mentioned | Placebo(non-intervention)/Group psychotherapy | 60/60 | CIAS | 20w | |
| Li R | 2020 | not mentioned | not mentioned | Psychotherapy(CBT)/Group psychotherapy | 12/12 | CIAS | 8w | |
| Chen AW | 2020 | male:35, female:10/male:36, female:9 | 14.83 ± 2.46/14.95 ± 2.51 | Health education/Group psychotherapy | 45/45 | CIAS-R | 8w | |
| Xu ZX | 2018 | male:16, female:4/male:14, female:6 | 13.3 ± 1.3/14.0 ± 1.0 | Health education/Group psychotherapy | 20/20 | CIAS | 4w | |
| Chen SZ | 2018 | male:34, female:18/male:36, female:16 | 16.01 ± 1.45/16.15 ± 1.42 | Psychotherapy(CBT)/Group psychotherapy | 52/52 | CIAS | / | |
| Tang RZH | 2018 | male:18, female:6/male:23, female:4/male:22, female:4 | 22.63 ± 5.23/22.04 ± 7.54/21.54 ± 5.77 | Electro-acupuncture/Psychotherapy(CBT)/ Electro-acupuncture + CBT | 24/27/26 | CIAS-R | 8w | |
| 2018 | male:18, female:6/male:23, female:4/male:22, female:4 | 22.63 ± 5.23/22.04 ± 7.54/21.54 ± 5.77 | Electro-acupuncture/Psychotherapy (CBT)/Electro-acupuncture + CBT | 24/27/26 | VAS | 8w | ||
| Zhao ST | 2016 | male:59, female:6/male:58, female:7 | 16.2 ± 4.1/16.5 ± 3.6 | Health education/Group psychotherapy | 65/65 | CIAS | 16w | |
| Zhou M | 2015 | male:7, female:11/male:8, female:10 | 20.88 ± 1.13/20.38 ± 1.41 | Group psychotherapy/Placebo(non-intervention) | 18/18 | CIAS-R | 8w | |
| Wu ZX | 2015 | not mentioned | not mentioned | Group psychotherapy/Placebo(non-intervention) | 15/15 | CIAS | 8w | |
| Ming LJ | 2014 | not mentioned | not mentioned | Psychotherapy (CBT)/Placebo(non-intervention) | 60/60 | CIAS | 10w | |
| Zhang XF | 2013 | not mentioned | 19.83 ± 1.07/20.1 ± 1.07 | Health education/MBCT | 42/42 | CIAS | 1w | |
| Lv WQ | 2012 | not mentioned | not mentioned | Group psychotherapy/Placebo(non-intervention) | 26/26 | CIAS | 6w | |
| Chen ZZ | 2011 | not mentioned | not mentioned | Group psychotherapy/Placebo(non-intervention) | 14/23 | CIAS-R | 7w | |
| Li G | 2009 | male:35, female:3/male:33, female:5 | 17 ± 4/16 ± 4 | Psychotherapy(CBT)/Placebo(non-intervention) | 38/38 | CIAS | 8-10w | |
| Wang GR | 2008 | not mentioned | not mentioned | Group psychotherapy/Placebo(non-intervention) | 24/24 | CIAS | 12w | |
| Cao FL | 2007 | not mentioned | not mentioned | Group psychotherapy/Health education | 26/31 | CIAS | 8w | |
| Bai Y | 2007 | male:20, female:4/male:20, female:4 | 19 ± 2/19 ± 2 | Group psychotherapy/Placebo(non-intervention) | 24/24 | CIAS | 4w | |
| Zhao Y | 2022 | male:35, female:15/male:33, female:17 | 15.16 ± 2.18/15.25 ± 2.12 | Health education/Group psychotherapy | 50/50 | CIAS-R | 12w | |
| Liu X | 2021 | male:47, female:14/male:44, female:16 | 15.3 ± 0.8/15.2 ± 0.8 | Health education/MBCT | 61/60 | CIAS | 8w | |
| Deng LY | 2017 | not mentioned | 21.86 ± 1.90/22.05 ± 1.81 | Group psychotherapy/Placebo(non-intervention) | 44/19 | CIAS | 6w | |
| 2017 | not mentioned | 21.86 ± 1.90/22.05 ± 1.81 | Group psychotherapy/Placebo(non-intervention) | 44/19 | VAS | 6w | ||
| Liu D | 2013 | not mentioned | 20.3 ± 0.9/20.3 ± 1.0 | Group psychotherapy/Health education | 16/15 | IAT | 12w | |
| Tang RZH | 2017 | not mentioned | not mentioned | Psychotherapy(CBT)/Electro-acupuncture/ Electro-acupuncture + CBT | 20/23/21 | VAS | 4w | |
| Zhang Y | 2016 | male:25, female:9/male:27, female:7 | 17.21 ± 2.12/16.44 ± 3.53 | Electro-acupuncture/Placebo(non-intervention) | 34/34 | VAS | 6w | |
| Zhang HL | 2011 | not mentioned | not mentioned | Exercise therapy/Placebo(non-intervention) | 18/18 | IAT | 12w | |
| Deng YQ | 2014 | not mentioned | not mentioned | Exercise therapy/Placebo(non-intervention) | 24/24 | CIAS | 10w | |
| Fu YS | 2016 | not mentioned | not mentioned | Exercise therapy/Placebo(non-intervention) | 42/42 | IAT | 16w | |
| Yang CY | 2017 | male:12, female:14/male:13, female:13 | 19.6 ± 1.2/19.7 ± 1.4 | Exercise therapy/Placebo(non-intervention) | 26/26 | CIAS | 16w | |
| Ji W | 2017 | not mentioned | not mentioned | Exercise therapy/Health education | 10/10 | IAT | 12w | |
| Qiu JM | 2022 | male:20, female:20/male:20, female:20 | 15.64 ± 1.68/15.59 ± 1.71 | Drug/Drug + others | 40/40 | CIAS-R | 8w | |
| Zhou XH | 2016 | male:28, female:4/male:29, female:3 | not mentioned | Drug + others/Health education | 32/32 | CIAS-R | 8w | |
| Song HQ | 2017 | not mentioned | 13.90 ± 1.37/14.08 ± 1.49 | Drug/Drug + others | 20/20 | IAT | 16w | |
| Wang DP | 2014 | not mentioned | not mentioned | Psychotherapy (CBT)/Drug + others | 38/36 | CIAS | 8w | |
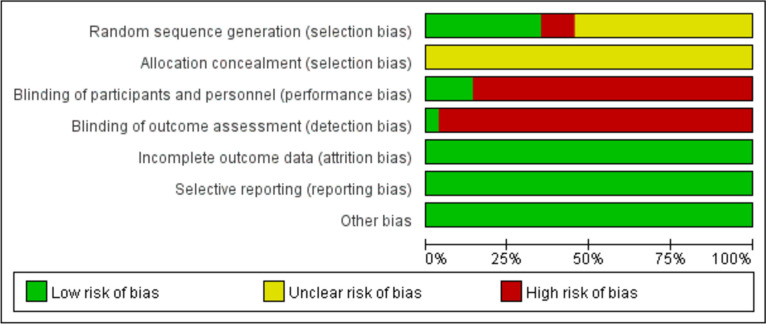
Risk of bias assessment (Fig. 2)
Fig. 2.
Bias risk assessment for included studies
Two reviewers strictly followed the recommended bias risk assessment tools in the Cochrane Handbook to assess the risk of bias for the included studies. For example, in terms of randomization methods, 22 studies were evaluated as "low risk" as they adopted randomized allocation methods such as random number tables, stratified randomization, and drawing lots. Another 28 studies only mentioned "randomization" without reporting specific randomization methods and were evaluated as "unclear risk." The remaining seven studies randomly assigned patients according to the admission order and were rated "high risk." All studies failed to report whether allocation concealment was performed and was rated as “unclear risk." Seven studies involved blinding and were rated as "low risk." All studies had complete data and were rated as "low risk." Other biases were not mentioned and were rated as "low risk."
Network meta-analysis
Network figure
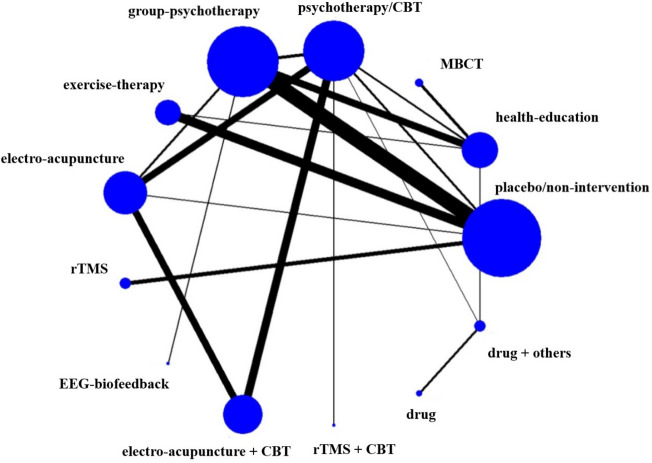
A total of 57 randomized controlled trials (RCTs) reported the effectiveness of different interventions to treat IA, involving 13 interventions. The size of each node in the network diagram (Fig. 3) represents the sample size of the corresponding intervention, and the thickness of the lines that connect different interventions represents the number of studies comparing the two interventions.
Fig. 3.
Network figure about efficient evidence
Analysis result
Network meta-analysis was performed on the included studies, generating 78 pairwise comparisons with 95% confidence intervals for the SMD. Please refer to Table 2 for detailed information.
Table 2.
Network meta-analysis [SMD (95% CI)]
| Interventions | Drug + others | Drug | rTMS + CBT | Electro-acupuncture + CBT | EEG biofeedback | rTMS | Electro-acupuncture | Exercise therapy | Group psychotherapy | Psychotherapy/CBT | MBCT | Health education |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| drug | -2.12 (-3.53,-0.70) | |||||||||||
| rTMS + CBT | 2.92 (-0.44,6.29) | 5.04 (1.39,8.69) | ||||||||||
| electro-acupuncture + CBT | -1.01 (-3.64,1.62) | 1.11 (-1.88,4.09) | -3.93 (-6.28,-1.58) | |||||||||
| EEG biofeedback | -1.35 (-4.86,2.16) | 0.77 (-3.01,4.55) | -4.27 (-7.58,-0.96) | -0.34 (-2.89,2.21) | ||||||||
| rTMS | -0.89 (-3.92,2.14) | 1.22 (-2.12,4.57) | -3.82 (-6.61,-1.02) | 0.12 (-1.72,1.96) | 0.46 (-1.81,2.72) | |||||||
| electro-acupuncture | -3.42 (-6.87,0.04) | -1.30 (-5.03,2.43) | -6.34 (-9.59,-3.09) | -2.41 (-4.89,0.07) | -2.07 (-4.88,0.74) | -2.52 (-4.71,-0.34) | ||||||
| exercise therapy | -1.54 (-4.47,1.40) | 0.58 (-2.68,3.84) | -4.46 (-7.15,-1.77) | -0.53 (-2.21,1.15) | -0.19 (-2.33,1.95) | -0.65 (-1.84,0.55) | 1.88 (-0.17,3.93) | |||||
| group psychotherapy | -1.93 (-4.84,0.97) | 0.19 (-3.05,3.42) | -4.85 (-7.51,-2.19) | -0.92 (-2.55,0.71) | -0.58 (-2.55,1.38) | -1.04 (-2.16,0.09) | 1.49 (-0.52,3.50) | -0.39 (-1.23,0.45) | ||||
| psychotherapy/CBT | -1.85 (-4.37,0.67) | 0.27 (-2.62,3.16) | -4.77 (-7.00,-2.54) | -0.84 (-1.58,-0.10) | -0.50 (-2.94,1.94) | -0.96 (-2.64,0.73) | 1.57 (-0.80,3.94) | -0.31 (-1.82,1.20) | 0.08 (-1.37,1.54) | |||
| MBCT | -2.36 (-4.74,0.03) | -0.24 (-3.01,2.53) | -5.28 (-8.16,-2.40) | -1.35 (-3.32,0.62) | -1.01 (-4.06,2.04) | -1.46 (-3.95,1.02) | 1.06 (-1.93,4.05) | -0.82 (-3.19,1.55) | -0.43 (-2.76,1.91) | -0.51 (-2.33,1.32) | ||
| health education | -4.25 (-6.34,-2.17) | -2.14 (-4.66,0.39) | -7.17 (-9.82,-4.53) | -3.24 (-4.84,-1.65) | -2.90 (-5.73,-0.08) | -3.36 (-5.56,-1.16) | -0.84 (-3.59,1.92) | -2.71 (-4.78,-0.64) | -2.32 (-4.35,-0.30) | -2.40 (-3.82,-0.99) | -1.90 (-3.05,-0.74) | |
| placebo/non-intervention | -2.26 (-3.26,-1.26) | 0.26 (-1.68,2.20) | -2.05 (-4.52,0.41) | -1.83 (-4.31,0.65) | -1.62 (-2.28,-0.95) | -1.22 (-1.74,-0.71) | -1.16 (-3.02,0.69) | -1.31 (-2.67,0.05) | -0.80 (-3.07,1.48) | 1.10 (-0.86,3.06) | -1.03 (-4.03,1.96) | 0.84 (-1.33,3.02) |
The results of the network meta-analysis showed that compared with the placebo/non-intervention group, drug + others (SMD = -2.26, 95% CI = -3.26 ~ -1.26), EEG biofeedback (SMD = -1.62, 95% CI = -2.28 ~ -0.95), rTMS (SMD = -1.22, 95% CI = -1.74 ~ -0.71) showed statistical significance in the treatment effect of IA. Compared to the health education group, drug + others (SMD = -4.25, 95% CI =—6.34 ~ -2.17), rTMS + CBT (SMD = -7.17, 95% CI = -9.82 ~ -4.53), electro-acupuncture + CBT (SMD = -3.24, 95% CI = -4.84 ~ -1.65), EEG biofeedback (SMD = -2.90, 95% CI = -5.73 ~ -0.08), rTMS (SMD = -3.36, 95% CI = -5.56 ~ -1.16), exercise therapy (SMD = -2.71, 95% CI = -4.78 ~ -0.64), group psychotherapy (SMD = -2.32, 95% CI = -4.35 ~ -0.30), psychotherapy/CBT (SMD = -2.40, 95% CI = -3.82 ~ -0.99), and MBCT (SMD = -1.90, 95% CI = -3.05 ~ -0.74) have been shown to be statistically significant in the treatment of IA. Compared to the psychotherapy/CBT group, rTMS + CBT (SMD = -4.77, 95% CI = -7.00 ~ -2.54), electro-acupuncture + CBT (SMD = -0.84, 95% CI = -1.58 ~ -0.10), reflect the difference in therapeutic effect compared to use CBT alone, combined physical therapy is essential for the curative effect. Similarly, drug + others (SMD = -2.12, 95% CI = -3.53 ~ -0.70) also showed statistically different advantages compared to interventions that only used drugs. Furthermore, compared to MBCT, psychotherapy/CBT group, psychotherapy, exercise therapy, electroacupuncture, rTMS, EEG biofeedback, and electroacupuncture + CBT, therapeutic efficacy in the rTMS + CBT group showed optimal differences, and the results were statistically significant (p < 0.05), which further demonstrating the unique therapeutic effect of rTMS + CBT. This combination of treatment modalities could provide a reference for the treatment of IA in the future.
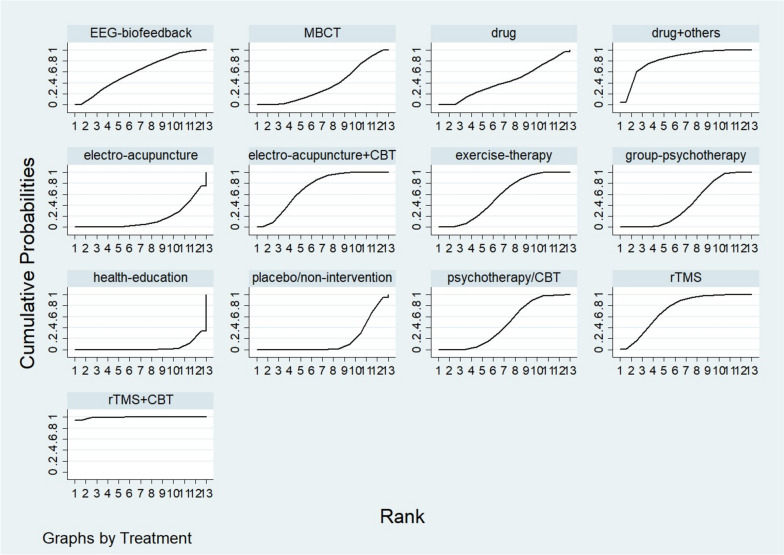
Rank
In terms of efficiency, the ranking was rTMS + CBT > drug + others > rTMS > electro-acupuncture + CBT > EEG-biofeedback > exercise-therapy > psychotherapy/CBT > group-psychotherapy > drug > MBCT > placebo/non-intervention > electro-acupuncture > health-education. The specific rank order is shown in Table 3, and the cumulative probabilities are shown in Fig. 4.
Table 3.
The ordering results of network meta-analysis
| ID and rank | Treatment | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| placebo/non-intervention | health-education | MBCT | psychotherapy/CBT | group-psychotherapy | exercise-therapy | electro-acupuncture | rTMS | EEG-biofeedback | electro-acupuncture + CBT | rTMS + CBT | drug | drug + others | |
| Best | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.2 | 0.4 | 0.0 | 94.6 | 0.0 | 4.8 |
| 2nd | 0.0 | 0.0 | 0.3 | 0.0 | 0.0 | 1.2 | 0.1 | 15.7 | 12.5 | 9.0 | 4.6 | 0.5 | 56.1 |
| 3rd | 0.0 | 0.0 | 2.4 | 0.5 | 0.5 | 5.1 | 0.3 | 24.4 | 15.0 | 22.8 | 0.6 | 13.8 | 14.5 |
| 4th | 0.0 | 0.0 | 4.7 | 4.3 | 2.5 | 12.4 | 0.4 | 22.3 | 12.7 | 24.5 | 0.1 | 8.9 | 7.2 |
| 5th | 0.0 | 0.0 | 6.0 | 10.0 | 6.6 | 18.3 | 0.9 | 16.8 | 10.7 | 18.1 | 0.1 | 7.5 | 5.0 |
| 6th | 0.0 | 0.0 | 7.5 | 15.8 | 13.4 | 20.0 | 1.6 | 10.0 | 9.4 | 11.8 | 0.0 | 6.6 | 3.8 |
| 7th | 0.3 | 0.0 | 8.6 | 19.4 | 18.9 | 17.8 | 2.3 | 5.6 | 9.5 | 8.3 | 0.1 | 5.8 | 3.3 |
| 8th | 1.6 | 0.3 | 10.6 | 22.9 | 22.7 | 12.7 | 4.4 | 2.9 | 8.5 | 3.8 | 0.0 | 7.1 | 2.6 |
| 9th | 8.1 | 0.7 | 15.1 | 16.5 | 20.4 | 8.2 | 7.9 | 1.4 | 7.9 | 1.5 | 0.0 | 10.8 | 1.6 |
| 10th | 19.1 | 1.9 | 20.2 | 8.8 | 12.7 | 3.9 | 10.9 | 0.6 | 7.9 | 0.3 | 0.0 | 13.2 | 0.8 |
| 11th | 39.1 | 9.6 | 13.9 | 1.6 | 2.3 | 0.4 | 19.4 | 0.1 | 3.4 | 0.0 | 0.0 | 10.1 | 0.2 |
| 12th | 26.9 | 21.7 | 10.7 | 0.3 | 0.1 | 0.0 | 26.7 | 0.0 | 1.5 | 0.0 | 0.0 | 12.1 | 0.0 |
| Worst | 4.8 | 65.9 | 0.0 | 0.1 | 0.0 | 0.0 | 25.2 | 0.0 | 0.6 | 0.0 | 0.0 | 3.5 | 0.0 |
Fig. 4.
Cumulative probabilities
Inconsistency test
The consistency of each closed-loop result was tested. Inconsistency factors (IF) showed p = 0.4042, indicating good consistency. All local p > 0.05, indicating good consistency among all groups.
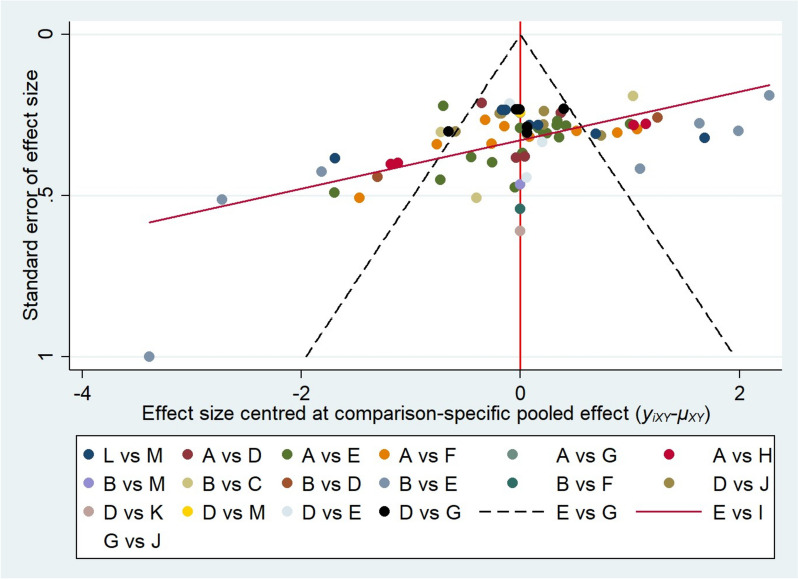
Publication bias
The research was roughly symmetrically distributed on both sides of the midline, indicating that a small sample effect was less likely to exist as shown in Fig. 5.
Fig. 5.
Funnel plot about the 14 interventions in the treatment of IA. A placebo/non-intervention, B health-education, C MBCT, D psychotherapy/CBT, E group-psychotherapy, F exercise-therapy, G electro-acupuncture, H rTMS, I EEG-biofeedback, J electro-acupuncture + CBT, K rTMS + CBT, L drug, M drug + others
Discussion
IA causes serious physical and mental distress and potential harm to people. Many scholars have investigated prevention and intervention measures for IA in recent years, resulting in various interventions. There have been relatively few studies on treating IA, and the effects of most treatments are limited. To investigate the efficacy, advantages, and disadvantages of different treatment methods used alone or in combination, this study conducted a network meta-analysis of the efficacy of 13 intervention methods. The ranking results showed that the top four intervention measures in terms of effectiveness were rTMS combined with CBT, drug combination with other treatments, rTMS, and electro-acupuncture combined with CBT. The rankings of various comprehensive treatments were also high, indicating that combined therapy can effectively improve the effect of IA compared to using a single intervention measure for treatment.
rTMS combined with CBT
Based on the efficacy ranking, both rTMS combined with CBT and rTMS alone achieved optimal treatment effects. Compared with all other interventions except for drug-combined comprehensive treatment, rTMS combined with CBT has shown statistical differences. rTMS is a physical therapy that generates a sequence of repetitive electromagnetic pulses through an electromagnetic coil. It can regulate cortical excitability by acting on specific cortical regions of the brain [71]. Numerous domestic and foreign studies have shown that rTMS has immense potential to treat substance dependence [72]. Studies have shown that rTMS treatment targeting the left or right dorsolateral prefrontal cortex (DLPFC) can fully mobilize the cognitive regulatory capacity of the DLPFC, increase the excitability of cortical areas, and regulate activity by maintaining functional levels of dopamine and other neurotransmitters in various structures of the reward circuit [73]. Thus, people's cravings for the Internet will be reduced, and their addictive behavior will be curtailed. Furthermore, neuroimaging studies have also found that rTMS applied to DLPFC can effectively inhibit brain cortices related to addictive behavior and sensation, reduce the craving of participants with IA, improve their cognitive control and emotional regulation abilities, reward and cognitive control systems, and thereby reduce the craving and behavior in IA [74, 75]. IA can significantly reduce the white matter integrity of DLPFC compared to normal individuals [76], similar to the changes observed in drug addiction. Excessive use of the internet can alter the reward and pleasure centers of the brain, making it difficult to quit addiction. rTMS can help regulate brain activity and reduce cravings related to IA.
Simultaneously, CBT is also a major intervention method for IA in psychotherapy, which is effective in many randomized controlled studies on IA [77, 78]. The essence of CBT is to correct the cognitive dysfunction of patients with IA. Improving cognitive control ability may be the key to solving IA [79]. The results of the network meta-analysis demonstrated that rTMS combined with CBT treatment was more effective than rTMS or CBT alone. When people try to reduce or withdraw from online activities, IA can lead to withdrawal symptoms. Physical therapy interventions can help control these physiological and emotional withdrawal symptoms, making it easier for patients to receive psychological treatment. Therefore, people's desire for the internet will decrease and their addictive behavior will be restricted [80]. This could be attributed to the potential of combined treatment to simultaneously improve the physiological, psychological, and behavioral aspects of IA, thereby producing a cumulative effect for better outcomes.
Combination of medication and other therapies
Medication combined with other intervention measures, as a comprehensive intervention measure, demonstrates excellent efficacy, outperforming single medication therapy. Many experts believe that IA indicates impulse control disorders over the internet. This addictive behavior is classified as compulsive behavior [81]. Researchers suggest that selective serotonin reuptake inhibitors (SSRIs), as first-line drugs for treating obsessive–compulsive disorder, may also have optimal therapeutic effects on patients with IA. The results of our meta-analysis indicated that the efficacy of single drug therapy is only superior to that of the general intervention group, the placebo group, and the single electro-acupuncture group and is comparable to that of a single psychological treatment. However, when combined with psychological or physical treatment, it demonstrates excellent results and is statistically significant compared to single-medication therapy. This may result from medication therapy controlling anxiety and depression to a certain extent in IA patients. For IA patients with poor self-control and resistance to treatment, applying medication first to stabilize the patient's emotions and then using psychological or physical treatment can further improve their depressive and anxious symptoms and cognitive function, thereby reducing their craving for the internet. Additionally, combined therapy can reduce the adverse effects of the long-term use of single medications and improve treatment safety, resulting in better outcomes.
Electro-acupuncture and CBT combined treatment
We also noticed that the combination of electro-acupuncture and CBT treatment had achieved unexpected results. Traditional Chinese medicine has a long history of application in mental illnesses, such as using electro-acupuncture to treat depression and sleep disorders. Studies have demonstrated that electro-acupuncture can promote the recovery of neurons in the affected brain area [82]. The acupoints used in acupuncture can increase blood flow or induce electrical potentials in specific brain regions [83]. As a commonly used treatment in traditional Chinese medicine, Electro-acupuncture therapy has gained recognition in treating modern addictive behaviors. The combination of electro-acupuncture and CBT treatment was shown to significantly reduce the addiction level and related clinical symptoms of IGD patients. fMRI is increasingly being used to study the mechanism of acupuncture. Previous studies have confirmed that acupuncture and moxibustion can regulate the structure and function of the brain regions of drug addicts and can regulate the functional connection between the reward and habit systems of IA [84]. Therefore, the regulatory effect of acupuncture on the brain area of network addiction patients may be a potential mechanism of acupuncture in-network addiction. Both electro-acupuncture and cognitive-behavioral therapy have significant positive effects on network-addicted adolescents. Both treatment methods effectively improve network addiction patients' psychological experience and behavioral expression. However, electro-acupuncture is more effective than psychological therapy regarding impulse control and neuron protection. This advantage may be related to increased NAA and CHO levels in the prefrontal cortex and anterior cingulate cortex [82]. The combination of electro-acupuncture and psychological interventions (cognitive-behavioral therapy, group, psychological therapy combined with individual psychological therapy) can alleviate the mental symptoms, sleep quality, and impulse characteristics of network addiction patients [85]. Its mechanism may be related to increased brain sensory perception gate function. Psychological intervention can help relieve the fear of electro-acupuncture and improve the treatment effect, as acupuncture is an exogenous stimulation that usually accompanies pain. Combining CBT with electro-acupuncture treatment has shown superior results compared to using acupuncture alone, suggesting a synergistic effect between electro-acupuncture and CBT. In summary, combining electro-acupuncture and CBT can achieve optimal therapeutic outcomes.
Other interventions
Compared to comprehensive treatment, we have observed that the following five interventions, namely health education, electro-acupuncture, place/non-intervention, MBCT, and drug treatment, have relatively lower effectiveness. We believe this may be attributed to the following reasons. Health education often focuses on encouragement, comfort, and providing knowledge related to IA, but it fails to address the deep-rooted inner struggles of patients and alleviate their dependency on the internet. Therefore, health education is generally less effective in most cases. As for electroacupuncture treatment, studies have shown that IA patients often experience strong withdrawal reactions during the initial stages of treatment, such as restlessness, palpitations, and irritability. As an acupuncture treatment, electroacupuncture may cause swelling and heaviness at the treatment site, and discomfort may persist for a period of time after the needles are removed and gradually subside. Consequently, the compliance and expectations of most patients are not high, resulting in mediocre therapeutic effects of using electroacupuncture alone.
MBCT, as a mindfulness and meditation-oriented treatment method, has been shown in research to reduce craving for IA by improving the understanding ability of IA patients, improving loneliness in IA, and reducing heart rate and cortisol levels [23]. However, due to the impulsive personality traits of most addiction patients, many individuals are unable to calm their minds and fully engage in the understanding and experience provided by MBCT therapy. Therefore, relying solely on MBCT treatment is ineffective.
The use of drugs alone also fails to achieve better therapeutic effects, mainly because in simple applications of drug therapy, common SSRIs such as sertraline, which selectively inhibit the reuptake of serotonin by central neurons, leading to an increase in serotonin concentration, have slow-acting effects and are associated with side effects such as gastrointestinal discomfort. Consequently, patients have low long-term medication tolerance and poor treatment effectiveness. Moreover, the cognitive function of patients is still insufficient in medication-only treatment [3]. On the other hand, combination therapy and comprehensive treatment can reduce the adverse reactions caused by long-term medication use, enhance treatment safety, and improve treatment effectiveness. Therefore, a single treatment approach may not be able to address all the issues, and personalized comprehensive treatment plans should be developed based on the unique characteristics of each patient during clinical treatment to ensure compliance and treatment effectiveness.
IA is a complex multifactorial disorder with numerous physiological, psychological, and social elements. A single treatment plan can have difficulty addressing all issues, while a comprehensive therapy can integrate the advantages and disadvantages of various treatments and take targeted measures. Although the findings of this study confirm the safety and feasibility of electro-acupuncture + CBT therapy for IA, there are still some limitations. Due to time constraints, the long-term efficacy of the subjects has not been observed, and the effectiveness assessment was based on clinical scales. Therefore, it is possible that subjects may have concealed some information during the measurement.
Limitation
(1) Most of the studies were conducted by Chinese researchers. (2) The literature on rTMS combined with CBT treatment and drug combinations with other treatments included in this study was limited.
Conclusion
The results of our study show that, although all treatments were slightly more effective than placebo/non-intervention and health education in treating IA patients, rTMS + CBT had the best therapeutic effect in treating IA patients with different interventions, followed by drugs combined with other treatments, followed by rTMS and electro-acupuncture + CBT. This proves the unique role physical therapy, specifically rTMS therapy, plays in treating patients with IA. Comprehensive intervention can achieve better therapeutic effects than using drugs or psychotherapy alone by combining drug therapy, physical therapy, and psychotherapy. Comprehensive intervention improves the physical, psychological, and behavioral aspects of patients with IA by combining the benefits of various methods.
Acknowledgements
Not applicable.
Authors’ contributions
ZYQ and CHH wrote the first draft of the manuscript. LJD interpreted and analyzed the research results, and proposed conclusions and suggestions. MX participates in the literature selection process to ensure the accuracy and completeness of data. WWJ provided critical revision of the manuscript for important intellectual content. All authors read and approved the final manuscript.
Funding
Provincial Education Department Natural Science Key Project (grant number: 2022AH051512), Shanghai Key Laboratory of Psychotic Disorders Open Grant (grant number: 13dz2260500), Bengbu Medical College key Laboratory of Addiction Medicine (29–3).
All funders didn’t interfere in study design, collection, analysis, interpretation, or writing of the manuscript.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
Not applicable (rapid review).
Consent for publication
Not applicable (rapid review).
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yuqiong Zhu and Haihan Chen contributed equally to this work.
References
- 1.Shao YJ, et al. Internet addiction detection rate among college students in the People's Republic of China: a meta-analysis. Child Adolesc Psychiatry Ment Health. 2018;12:25. doi: 10.1186/s13034-018-0231-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Young, K. Internet Addiction : The emergence of a new clinical disorder. in the 104th annual meeting of the American Psychological Association in Toronto, Canada. August 20,1996. 1996.
- 3.Qiu JM, et al. The Intervention Study of EEG Biofeedback Therapy on Internet Addiction of Adolescent Patients with Depression. Chinese Medical Innovations. 2022;19(21):146–149. [Google Scholar]
- 4.Lorenz RC, et al. Cue reactivity and its inhibition in pathological computer game players. Addict Biol. 2013;18(1):134–146. doi: 10.1111/j.1369-1600.2012.00491.x. [DOI] [PubMed] [Google Scholar]
- 5.Gong L, et al. Self-control impacts symptoms defining Internet gaming disorder through dorsal anterior cingulate-ventral striatal pathway. Addict Biol. 2022;27(5):e13210. doi: 10.1111/adb.13210. [DOI] [PubMed] [Google Scholar]
- 6.Cheng H, Liu J. Alterations in Amygdala Connectivity in Internet Addiction Disorder. Sci Rep. 2020;10(1):2370. doi: 10.1038/s41598-020-59195-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weinstein A, Lejoyeux M. Internet addiction or excessive internet use. Am J Drug Alcohol Abuse. 2010;36(5):277–283. doi: 10.3109/00952990.2010.491880. [DOI] [PubMed] [Google Scholar]
- 8.Yen JY, et al. The comorbid psychiatric symptoms of Internet addiction: attention deficit and hyperactivity disorder (ADHD), depression, social phobia, and hostility. J Adolesc Health. 2007;41(1):93–98. doi: 10.1016/j.jadohealth.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 9.Battle DE. Diagnostic and Statistical Manual of Mental Disorders (DSM) Codas. 2013;25(2):191–192. doi: 10.1590/s2317-17822013000200017. [DOI] [PubMed] [Google Scholar]
- 10.YOUNG, S.J.C. Kimberly, and Behavior, Internet Addiction: The Emergence of a New Clinical Disorder. 2009. 1(3): p. 237–244.
- 11.Grohol JM. Caught in the Net: how to recognize the signs of Internet addiction and a winning strategy for recovery. Addiction. 2000;95(1):139–140. [Google Scholar]
- 12.Chen S, et al. Chinese Development of Internet Addiction Scale and Research on Psychometric Characteristics. Chinese Journal of Psychology. 2003;45(3):279–294. [Google Scholar]
- 13.Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 2011;64(2):163–171. doi: 10.1016/j.jclinepi.2010.03.016. [DOI] [PubMed] [Google Scholar]
- 14.Veroniki AA, et al. The rank-heat plot is a novel way to present the results from a network meta-analysis including multiple outcomes. J Clin Epidemiol. 2016;76:193–199. doi: 10.1016/j.jclinepi.2016.02.016. [DOI] [PubMed] [Google Scholar]
- 15.Zhu TM, et al. Intervention on network craving and encephalofluctuogram in patients with internet addiction disorder: a randomized controlled trial. Chinese Acupuncture Moxibustion. 2011;31(05):395–399. [PubMed] [Google Scholar]
- 16.Zhou XH, et al. Double-blind Randomized Controlled Clinical Trial of Sertraline in Adolescents with Internet Addiction Disorder. Chin J Health Psychol. 2016;24(07):965–968. [Google Scholar]
- 17.Zhou M, et al. Research on the intervention effect of group counseling on Internet dependent college students. Beijing: Beihang University Press; 2015. [Google Scholar]
- 18.Zhong YH. Effect of rTMS on decreasing internet addicts' craving for internet. J Gannan Med University. 2020;40(07):727–729. [Google Scholar]
- 19.Zheng WF, et al. Effect Analysis of Group Psychotherapy in College Students with Internet Addiction. Med Soc. 2007;06:28–30. [Google Scholar]
- 20.Zhao Y, Pan Q. Effect of Social-Psychological Intervention on Self-Efficacy, Social Adaptability and Quality of Life of Internet-Addicted Teenagers. Psychiatr Danub. 2022;34(3):490–496. doi: 10.24869/psyd.2022.490. [DOI] [PubMed] [Google Scholar]
- 21.Zhao ST, et al. Control study of curative effect on internet addiction disorder elimination by cognitive-behavioral therapy in groups. Med J Chin PAP. 2016;27(04):392–395. [Google Scholar]
- 22.Zhang Y. Four high school of Hunan Province youth network addiction investigation and electroacupuncture at Baihui, Yintang intervention adolescent Internet addiction randomized, controlled clinical study. Changsha: Hunan University of Chinese Medicine; 2016. [Google Scholar]
- 23.Zhang XF. The Study of Interventions with Naikan Cognitive Therapy to Medical Students with Internet Addiction Disorder. Tianjin: Tianjin Medical University; 2013. [Google Scholar]
- 24.Zhang W, Xu R. Effect of Exercise Intervention on Internet Addiction and Autonomic Nervous Function in College Students. Biomed Res Int. 2022;2022:5935353. doi: 10.1155/2022/5935353. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 25.Zhang LB, et al. Intervention effect of family sandplay therapy on adolescent internet addiction. J Guangdong Med University. 2018;36(3):263–266. [Google Scholar]
- 26.Zhang HL. An Empirical Study on the Intervention Effect of Physical Exercise Prescription on Teenage Internet Addiction. J PLA Inst Phys Educ. 2011;30(4):119–122. [Google Scholar]
- 27.Zhang C.S. A Study on the Sports Intervention of Undergraduates’ Internet Addiction in Kunming City. Sport Sci Technol. 2013;34(04):127–128+133. [Google Scholar]
- 28.Yuan JJ. The Intervention Study of Naikan Therpayon Adolescents with Game Dependence Behavior Disorder. Lanzhou: Northwest Minzu University; 2022. [Google Scholar]
- 29.Yu YG. Research on Influence of College Sports Camps on College students’ Network Addiction. Guangzhou: South China University of Technology; 2017. [Google Scholar]
- 30.Yao ZZ, et al. Evaluation of intervention effect of phased group counseling on college students with Internet addiction. Chin J Sch Health. 2011;32(06):726–728. [Google Scholar]
- 31.Yao LH, Yao F, De Lan Y. Evaluation of intervention effect of group counseling on Internet addiction of college students. Youth Society. 2012;7:219–220. [Google Scholar]
- 32.Yang Y, et al. Electro-acupuncture treatment for internet addiction: Evidence of normalization of impulse control disorder in adolescents. Chin J Integr Med. 2017;23(11):837–844. doi: 10.1007/s11655-017-2765-5. [DOI] [PubMed] [Google Scholar]
- 33.Yang Y. The impact of electro-acupuncture on the impulsive behavior and the change of magnetic resonance spectroscopy(MRS) in patients with internet addiction disorder. Chengdu: Chengdu University of Traditional Chinese Medicine; 2013. [Google Scholar]
- 34.Yang W, et al. Impact of Short-Term Intensive-Type Cognitive Behavioral Therapy Intervention on Internet Addiction among Chinese College Students: A Randomized Controlled Trial. Int J Environ Res Public Health. 2022;19(9):5212. doi: 10.3390/ijerph19095212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yang CY, Zeng GF. The effect of tai chi exercise on college students' Internet addiction. Chin J Sch Health. 2017;38(2):292–294. [Google Scholar]
- 36.Xu ZX, Xu HB. Clinical effect of group psychotherapy on adolescents with Internet addiction. Chin J Clinical Rational Drug Use. 2018;11(36):173–174. [Google Scholar]
- 37.Wu Z. Intervention of Group Training for Vocational Students' Internet Addiction. Changsha: Hunan Normal University; 2015. [Google Scholar]
- 38.Wang QZ. Evaluation of Intervention Effect of Internet Addiction by Cognitive Behavioral Therapy for College Students. J Huangshi Institute Technol. 2012;28(04):49–51. [Google Scholar]
- 39.Wang GR. Study on the effect of group psychological counseling on adolescent Internet dependence. J Shengli College China University Petraoleum. 2008;22(04):64–66. [Google Scholar]
- 40.Wang DP, Shi QW, He QZ. Study on the treatment of children dependent on network game of psychological intervention combined with drug. Chin J Appl Clin Pediatr. 2014;29(15):1170–1173. [Google Scholar]
- 41.Tang Ren ZH, et al. Clinical effect of cognitive behavior therapy combined with electro-acupuncture in the treatment of internet gaming disorder. Clinical Res Practice. 2017;2(35):1–3. [Google Scholar]
- 42.Tang Ren ZH. A randomized, controlled clinical study of cognitive behavioral therapy combined with percutaneous acupoint electrical stimulation in the treatment of online gaming disorder. Changsha: Hunan University of Chinese Medicine; 2018. [Google Scholar]
- 43.Sun JJ, et al. The effect of high 7 frequency repetitive transcranial magnetic stimulation on the left dorsolateral prefrontal cortex in young and adolescent with internet gaming disorders. J Clin Psychiat. 2022;32(4):272–275. [Google Scholar]
- 44.Song QH, Zhu GD, Jin GL. Intervention effect of group psychotherapy on adolescents with internet gaming disorder. J Clin Psychiat. 2017;27(04):263–265. [Google Scholar]
- 45.Song GY, et al. A study on the intervention effect of positive psychology group counseling on the post-00s medical students with Internet addiction. Health Vocational Education. 2020;38(15):154–157. [Google Scholar]
- 46.Qing LW, Zhang BH. The Effects of Group Counseling on Internet-Dependent College Students. Chin J Health Psychol. 2012;20(12):1845–1847. [Google Scholar]
- 47.Peng WX, Li Z. The Effect of group psychotherapy on internet addiction and mental health of secondary school students. J Clin Psychosom Dis. 2015;4:82–84. [Google Scholar]
- 48.Peng W, et al. Effects of Electroacupuncture Combined With Psychological Intervention on Depressive Status and Contingent Negative Variation in Patients With Internet Addiction Disorder: A Randomized Controlled Trial. Front Psychiatry. 2021;12:722422. doi: 10.3389/fpsyt.2021.722422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ming LJ, et al. The effect of cognitive behavioral thepray on the intervention of internet addiction behavior of medical students. J Bengbu Med Coll. 2014;39(02):248–251. [Google Scholar]
- 50.Lu ZJ, Li ZM, Yan WS. Effect of group cognitive therapy on negative emotion and impulsivity of college students with Internet addiction. Chin J Sch Health. 2021;42(06):887–892. [Google Scholar]
- 51.Liu X, Jiang J, Zhang Y. Effects of Logotherapy-Based Mindfulness Intervention on Internet Addiction among Adolescents during the COVID-19 Pandemic. Iran J Public Health. 2021;50(4):789–797. doi: 10.18502/ijph.v50i4.6005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Liu D, et al. Effects of internet addiction group counseling on internet using andstudy management in college students. Chin Ment Health J. 2013;27(07):496–501. [Google Scholar]
- 53.Li R. The Intervention Study of Painting Group Counseling on College Students’ Internet. Suzhou: Soochow University; 2020. [Google Scholar]
- 54.Li M, et al. Current situation and exercise prescription intervention of Internet addiction among middle school students. Chin J Sch Health. 2014;35(12):1847–1848+1852. [Google Scholar]
- 55.Li H, et al. Effect of electro-acupuncture combined with psychological intervention on mental symptoms and P50 of auditory evoked potential in patients with internet addiction disorder. J Tradit Chin Med. 2017;37(1):43–48. doi: 10.1016/S0254-6272(17)30025-0. [DOI] [PubMed] [Google Scholar]
- 56.Li G, Xiu YD. Control Study of Cognitive-Behavior Therapy in Adolescents with Internet Addiction Disorder. Chin Ment Health J. 2009;23(07):457–460. [Google Scholar]
- 57.Ji W. The study of the physical intervention of the "Internet Addiction Syndrome" in college students. Mudanjiang: Mudanjiang Normal University; 2017. p. 55. [Google Scholar]
- 58.Gao J, Sun JH, Xiao KP. Influence of Sport Interference on University Students’Network Addiction. J Shenyang Sport University. 2012;31(4):55–59. [Google Scholar]
- 59.Fu YS, Yang L. The situation of Internet addiction among Korean college students and the effect of intervention in football training. Chin J Sch Health. 2016;37(12):1890–1892. [Google Scholar]
- 60.Duan SL, Ye ML. Psychological intervention in college students’ intervent dependence and its effect: Based on the control test in Hunan Police Academy. J Hunan Agricultural University (Social Sciences) 2012;6:63–67. [Google Scholar]
- 61.Deng YQI. Study on the intervention of physical exercise on Internet addiction of vocational college students. Vocational Tech Educ Forum. 2014;35:35–38. [Google Scholar]
- 62.Deng LY, et al. Craving Behavior Intervention in Ameliorating College Students' Internet Game Disorder: A Longitudinal Study. Front Psychol. 2017;8:526. doi: 10.3389/fpsyg.2017.00526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cheng Geng J.S, Luo J.H. Intervention effect of electroencephalogram biological feedback on adolescents with Internet addiction. Chin J Sch Health. 2017;38(11):1648–1650. [Google Scholar]
- 64.Chen SZ, Wu SY. Effects of group cognitive behavioral therapy on adolescent patients with Internet addiction. Chinese Foreign Medic Res. 2018;16(15):172–173. [Google Scholar]
- 65.Chen J, Lu J.X, Su M. Repetitive high-frequency transcranial magnetic stimulation can safely relieve the symptoms of internet addiction. Chinese Journal of Physical Medicine and Rehabilitation. Chin J Phys Med Rehabil. 2022;44(2):153–156. [Google Scholar]
- 66.Chen D, Liang CS, Liu R. Application value of cognitive-behavior-oriented group psychotherapy in patients with Internet addiction. Clin Med. 2021;41(11):71–73. [Google Scholar]
- 67.Chen AW. Analysis of clinical effect of group psychotherapy on adolescents with Internet addiction. Psychologies Magazine. 2020;15(14):53. [Google Scholar]
- 68.Cao FL, et al. Control Study of Group Psychotherapy on Middle School Students with Internet Overuse. Chin Ment Health J. 2007;21(05):346–349+358.
- 69.Bai Y, Fu MF. The Effects of Group Counseling on Internet-Dependent College Students. Chin Ment Health J. 2007;04:247–250. [Google Scholar]
- 70.Alavi SS, et al. The effects of cognitive-behavioral group therapy for reducing symptoms of internet addiction disorder and promoting quality of life and mental health. Trends Psychiatry Psychother. 2021;43(1):47–56. doi: 10.47626/2237-6089-2020-0010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lewis G. Transcranial magnetic stimulation for depression. Lancet. 2018;391(10131):1639–1640. doi: 10.1016/S0140-6736(18)30863-8. [DOI] [PubMed] [Google Scholar]
- 72.Steele VR. Transcranial Magnetic Stimulation as an Interventional Tool for Addiction. Front Neurosci. 2020;14:592343. doi: 10.3389/fnins.2020.592343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Seidel K, et al. Postoperative navigated transcranial magnetic stimulation to predict motor recovery after surgery of tumors in motor eloquent areas. Clin Neurophysiol. 2019;130(6):952–959. doi: 10.1016/j.clinph.2019.03.015. [DOI] [PubMed] [Google Scholar]
- 74.Moretti J, Poh EZ, Rodger J. rTMS-Induced Changes in Glutamatergic and Dopaminergic Systems: Relevance to Cocaine and Methamphetamine Use Disorders. Front Neurosci. 2020;14:137. doi: 10.3389/fnins.2020.00137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gay A, et al. Repetitive Transcranial Magnetic Stimulation (rTMS) as a Promising Treatment for Craving in Stimulant Drugs and Behavioral Addiction: A Meta-Analysis. J Clin Med. 2022;11(3):624. doi: 10.3390/jcm11030624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Li S, et al. Exercise-Based Interventions for Internet Addiction: Neurobiological and Neuropsychological Evidence. Front Psychol. 2020;11:1296. doi: 10.3389/fpsyg.2020.01296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wölfling K, et al. Efficacy of Short-term Treatment of Internet and Computer Game Addiction: A Randomized Clinical Trial. JAMA Psychiat. 2019;76(10):1018–1025. doi: 10.1001/jamapsychiatry.2019.1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Young KS. Treatment outcomes using CBT-IA with Internet-addicted patients. J Behav Addict. 2013;2(4):209–215. doi: 10.1556/JBA.2.2013.4.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zhou ZH, et al. An event-related potential investigation of deficient inhibitory control in individuals with pathological Internet use. Acta Neuropsychiatr. 2010;22(5):228–236. doi: 10.1111/j.1601-5215.2010.00444.x. [DOI] [PubMed] [Google Scholar]
- 80.Liu J, Nie J, Wang Y. Effects of Group Counseling Programs, Cognitive Behavioral Therapy, and Sports Intervention on Internet Addiction in East Asia: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2017;14(12):1470. doi: 10.3390/ijerph14121470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Alavi SS, et al. Behavioral Addiction versus Substance Addiction: Correspondence of Psychiatric and Psychological Views. Int J Prev Med. 2012;3(4):290–294. [PMC free article] [PubMed] [Google Scholar]
- 82.Yang Y, et al. Electro-acupuncture treatment for internet addiction: Evidence of normalization of impulse control disorder in adolescents. Chin J Integr Med. 2017;23(11):837–844. doi: 10.1007/s11655-017-2765-5. [DOI] [PubMed] [Google Scholar]
- 83.Huang Y, et al. Effects of needling in Baihui (DU20), Shuigou (DU26) and Shenmen (HT7) on glucose metabolism in the lentiform nuclus in patients with vascular dementia. Di Yi Jun Yi Da Xue Xue Bao. 2005;25(11):1405–7. [PubMed] [Google Scholar]
- 84.Wang Y, et al. The Modulation of Reward and Habit Systems by Acupuncture in Adolescents with Internet Addiction. Neural Plast. 2020;2020:7409417. [DOI] [PMC free article] [PubMed]
- 85.Dai Y, et al. The modulation of mRNA levels of MAOA by electroacupuncture and psychotherapy in patients with pathological internet use. Front Psychiatry. 2022;13:918729. doi: 10.3389/fpsyt.2022.918729. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analysed during this study are included in this published article.