Abstract
Objective:
Increasing forces threaten the viability of thoracic surgeon–initiated research, a core component of our academic mission. National Institutes of Health funding is a benchmark of research productivity and innovation. This study examined the current status of National Institutes of Health funding for thoracic surgeons.
Methods:
Thoracic surgeon principal investigators on National Institutes of Health– funded grants during June 2010, June 2015, and June 2020 were identified using National Institutes of Health iSearch Grants (version 2.4). American Association of Medical Colleges data were used to identify all surgeons in the United States. Types and total costs of National Institutes of Health–funded grants werecompared relative to other surgical specialties.
Results:
A total of 61 of 4681 (1.3%), 63 of 4484 (1.4%), and 60 of 4497 (1.3%) thoracic surgeons were principal investigators on 79, 76, and 87 National Institutes of Health–funded grants in 2010, 2015, and 2020, respectively; these rates were higher than those for most other surgical specialties (P ≤.0001). Total National Institutes of Health costs for Thoracic Surgeon–initiated grants increased 57% from 2010 to 2020, outpacing the 33% increase in total National Institutes of Health budget. Numbers and types of grants varied among cardiovascular, transplant, and oncology subgroups. Although the majority of grants and costs were cardiovascular related, increased National Institutes of Health expenditures primarily were due to funding for transplant and oncology grants. Per-capita costs were highest for transplant-related grants during both years. Percentages of R01-to-total costs were constant at 55%. Rates and levels of funding for female versus male thoracic surgeons were comparable. Awards to 5 surgeons accounted for 33% of National Institutes of Health costs for thoracic surgeon principal investigators in 2020; a similar phenomenon was observed for 2010 and 2015.
Conclusions:
Long-term structural changes must be implemented to more effectively nurture the next generation of thoracic surgeon scientists.
Keywords: NIH funding, NIH grant, principal investigator, thoracic surgeon
Similar to other medical specialties, research is a core component of the academic mission of thoracic surgery. Pioneering efforts addressing adult cardiovascular (CV) disease, congenital heart anomalies, tuberculosis, and cancer, which established thoracic surgery as a medical discipline,1,2 continue today with thoracic surgeons (TSs) driving major innovations in cardiac surgery, transplantation, and oncology.3–8
In addition to its tremendous societal value, research initiated by TSs has been linked to academic productivity and career trajectories.9–13 Similar for basic scientists, funding from the National Institutes of Health (NIH) has been used as a benchmark of innovation and productivity of surgeon-scientists and is typically essential for senior leadership positions in academic thoracic surgery.9 However, increasing clinical demands, complexity of bench research, a highly competitive funding environment, and paucity of surgeons on study sections pose significant barriers to initiation and sustainment of thoracic surgery research.14–17 These issues may be further exacerbated by fluctuations in yearly NIH budgets.14,17 The present study was performed to examine the current status of NIH funding for TSs.
MATERIALS AND METHODS
Thoracic Surgeon Portfolio Creation
By using iSearch Grants (NIH Office of Portfolio Analysis’ nextgeneration portfolio analysis platform; v2.4), all awarded grants that were active, based on budget timeline, in June of 2010, 2012, 2014, 2016, 2018, and 2020 were extracted. NIH biographical sketches of the PIs were queried for surgeons by using the root word *surg*. We confirmed TS by manually reviewing the biographical sketches and online academic and professional profiles. In an additional analysis, multiple PI grants with 1 or more surgeon as “other PI” were identified and further cross-checked for TS credentials using NIH biographical sketches and online academic and professional profiles. All other PIs and their associated grants were excluded from this analysis. In each year’s database, some TSs were awarded more than 1 grant. Therefore, TSs were only counted once for each analysis to accurately reflect the proportion of NIH-funded TS. The Association of American Medical Colleges (AAMC) Physician Specialty Data Reports for 2010 and 2019 (data for 2020 not yet available) were used to analyze the entire physician workforces, including surgeons and more specifically cardiothoracic surgeons.18 Because AAMC data are not available for general surgeons without subspecialty training, the “General Surgery” category reflects all related subspecialties (surgical oncology, colorectal, and so on). The number of NIH-funded surgeons for all surgical specialties, other than TS, were acquired from existing reports.19
The following grant types were included in this analysis: K-grants (Research Career Programs), P-grants (Research Program Projects and Centers Grants), R-grants (Research Projects), T-grants (Training Programs), and U-grants (Cooperative Agreements). Total costs of grants awarded to TSs were calculated for each year. Grants awarded to TS in 2010, 2015, and 2020 were further stratified into CV, transplant, oncology, benign thoracic, and education.
Statistical Analysis
Exact Wilcoxon rank-sum tests were performed to compare all the costs for each year within the grant types and within the thoracic surgery categories; the “Education” and “Thoracic Benign” categories were excluded because of insufficient sample size. Chi-square and Fisher exact tests were used to compare proportions of funded grants in 2010 and 2020 between 2 categories. A chi-square test was used when there were large numbers of outcomes, and a Fisher exact test was used otherwise. All statistical results should be interpreted as exploratory, including P values that were unadjusted for multiple comparisons.
All results involving the comparison of AAMC TSs and physicians in other specialties in 2010 and 2020 (including male/female analysis) were evaluated with a chi-square test and Fisher exact test.
RESULTS
State of Funding
In June of 2010, 61 of 4681 TSs (1.3%) were principal investigators (PIs) on 79 NIH-funded extramural grants with a total cost of $37.5 M (Table 1). In 2015, this number increased to 63 investigators (1.4%) with 76 grants totaling $41.7 M. By 2019, the TS workforce had decreased to 4479; in June of 2020, 60 TSs (1.3%) were PIs on 87 grants with a total cost of $59 M. When examined on a biennial basis, this apparent upward trend in total NIH funding for TS-PIs held true during this decade (Figure 1, left). The 57% increase in total costs for TS-initiated NIH grants from 2010 to 2020 outpaced the 33% increase in total NIH budget ($31.238B-$41.685 B). After adjusting for inflation, NIH costs for TS-PI grants increased by $14.6 M between 2010 and 2020; this 33% was proportionally more than twice the 13% ($36.9 B) increase in total NIH budget and was not due to indirect costs that remained steady ( 30%) over that decade.
TABLE 1.
Thoracic surgeon–initiated grants funded by National Institutes of Health
| 2010 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||||
| Cardiovascular | Transplant | Oncology | Benign thoracic | Education | |||||||
|
|
|
|
|
|
|||||||
| No. | % | No. | % | No. | % | No. | % | No. | % | Total | |
| No. of PIs | 42 | 69 | 10 | 16 | 10 | 16 | 0 | 0 | 2 | 3 | 61* |
| No. of grants | 49 | 62 | 16 | 20 | 12 | 15 | 0 | 0 | 2 | 3 | 79 |
| Total cost | $21,611,899 | 58 | $12,410,115 | 33 | $3,041,733 | 8 | $0 | 0 | $391,434 | 1 | $37,455,181 |
|
| |||||||||||
| 2015 | |||||||||||
|
|
|||||||||||
| Cardiovascular | Transplant | Oncology | Benign thoracic | Education | |||||||
|
|
|
|
|
|
|||||||
| No. | % | No. | % | No. | % | No. | % | No. | % | Total | |
|
| |||||||||||
| No. of PIs | 39 | 62 | 12 | 19 | 12 | 19 | 0 | 0 | 3 | 5 | 63† |
| No. of grants | 43 | 57 | 17 | 22 | 13 | 17 | 0 | 0 | 3 | 4 | 76 |
| Total cost | $20,045,710 | 48 | $16,532,769 | 40 | $4,128,401 | 10 | $0 | 0 | $955,543 | 2 | $41,662,423 |
|
| |||||||||||
| 2020 | |||||||||||
|
|
|||||||||||
| Cardiovascular | Transplant | Oncology | Benign thoracic | Education | |||||||
|
|
|
|
|
|
|||||||
| No. | % | No. | % | No. | % | No. | % | No. | % | Total | |
|
| |||||||||||
| No. of PIs | 36 | 60 | 9 | 15 | 13 | 22 | 3 | 5 | 2 | 3 | 60‡ |
| No. of grants | 49 | 56 | 17 | 20 | 16 | 18 | 3 | 3 | 2 | 2 | 87 |
| Total cost | $26,224,105 | 44 | $21,137,967 | 36 | $9,387,010 | 16 | $1,572,114 | 3 | $643,539 | 1 | $58,964,735 |
PI, Principal investigator.
3 TSs had 2 unique grants classified in different categories.
1 TS had 2 and 1 TS had 3 unique grants classified in different categories.
3 TSs had 2 unique grants classified in different categories.
FIGURE 1.
Trends from 2010 to 2020 on a biennial basis. Left: Total costs of TS-initiated NIH grants. Right: Total number of NIH-funded TS PIs. TS, Thoracic surgeon; NIH, National Institutes of Health.
Percentages of NIH-funded TS-PIs were higher than the combination of all other surgical specialties in 2010 and 2020 (P<.01 in 2010, P<.01 in 2020) and statistically exceeded all individual specialties except for neurosurgery in 2010, and neurosurgery, ear, nose, and throat, and vascular surgery in 2020 (Table E1). However, although various other surgical specialties experienced increased proportions of NIH-funded PIs from 2010 to 2020 (P <.03), thoracic surgery was among several that were stagnant in this regard. Biennial analysis revealed minimal fluctuations in the numbers of NIH-funded TS-PIs during this decade (Figure 1, right).
TABLE E1.
Proportion of National Institutes of Health–funded surgeons within different specialties
| 2010 | 2015 | 2020 | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| AAMC total | NIH funded | % Funded | AAMC total | NIH funded | % Funded | AAMC total | NIH funded | % Funded | |
| Cardiothoracic | 4681 | 61 | 1.3 | 4484 | 64 | 1.4 | 4479 | 60 | 1.3 |
| General | 26,296 | 189 | 0.7*† | 25,233 | 228 | 0.9 | 25,544 | 258 | 1.0*† |
| Neurological | 5044 | 73 | 1.4† | 5343 | 90 | 1.7 | 5744 | 125 | 2.2† |
| Obstetrics and oncology | 40,345 | 104 | 0.3*† | 41,466 | 175 | 0.4 | 42,683 | 162 | 0.4*† |
| Ophthalmic | 17,935 | 94 | 0.5* | 18,584 | 162 | 0.9 | 19,302 | 126 | 0.7* |
| Orthopedic | 19,820 | 45 | 0.2* | 19,141 | 56 | 0.3 | 19,064 | 55 | 0.3* |
| Otolaryngology | 9225 | 58 | 0.6*† | 9405 | 104 | 1.1 | 9771 | 109 | 1.1† |
| Plastic and reconstructive | 6819 | 22 | 0.3* | 7017 | 25 | 0.4 | 7314 | 27 | 0.4* |
| Urology | 9824 | 47 | 0.5*† | 9804 | 73 | 0.7 | 10,197 | 72 | 0.7*† |
| Vascular | 2852 | 22 | 0.8* | 3356 | 28 | 0.8 | 3941 | 40 | 1.0 |
AAMC, Association of American Medical Colleges; NIH, National Institutes of Health.
Difference in proportion of NIH-funded surgeons within that subspecialty when compared with TS the same year (P <.05).
Change in proportion of NIH-funded surgeons within that subspecialty from 2010 to 2020 (P <.05).
Funding Within Areas of Thoracic Surgery
Numbers of grants awarded to each major thoracic surgery subspecialty (CV, transplant, oncology) remained relatively stable across the time points analyzed (Table 1), with the notable exception being a 33% increase in the number of oncology-related grants from 2010 to 2020. In contrast, the proportion of total costs pertaining to each TS subspecialty varied somewhat across these time points, once again with the overarching trend being an increase in the proportion of oncology-related costs and a decrease in the proportion of CV-related funding. As shown in Figure 2, the overall distribution patterns of grants differed between 2010 and 2020 (P <.0001).
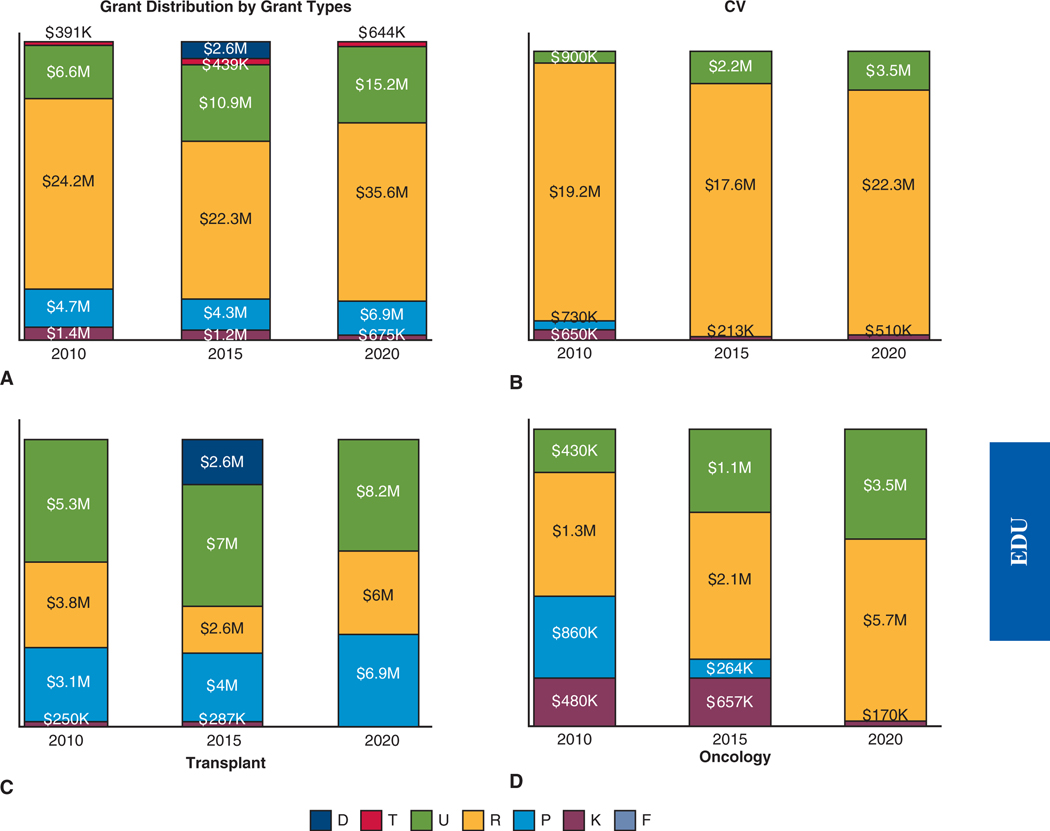
FIGURE 2.
Distribution of grant costs with percentages and relative amounts for thoracic surgery subspecialties in 2010, 2015, and 2020. CV, Cardiovascular.
Most of the NIH funding for TS-initiated grants in 2010, 2015, and 2020 came from the National Heart, Lung, and Blood Institute (NHLBI), followed by the National Institute of Allergy and Infectious Diseases (NIAID), and the National Cancer Institute (NCI) (Table E2). Although total dollar obligations for TS-initiated grants increased for all 3 institutes from 2010 to 2020, the percentage of total costs steadily decreased for NHLBI, while nearly doubling for NIAID and NCI.
TABLE E2.
National Institutes of Health funding institutes for thoracic surgeon principal investigator grants
| 2010 | 2015 | 2020 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||||
| NIH institute | No. of grants | Cost | % of cost | NIH institute | No. of grants | Cost | % of cost | NIH institute | No. of grants | Cost | % of cost |
| NHLBI | 58 | $28,357,438 | 75.7 | NHLBI | 54 | $27,439,999 | 65.9 | NHLBI | 59 | $34,391,768 | 58.3 |
| NIAID | 5 | $4,907,610 | 13.1 | NIAID | 6 | $6,998,927 | 16.8 | NIAID | 8 | $13,880,085 | 23.5 |
| NCI | 10 | $3,032,867 | 8.1 | NCI | 12 | $4,048,401 | 9.7 | NCI | 15 | $8,982,427 | 15.2 |
| NICHD | 2 | $1,063,793 | 2.8 | OD | 1 | $2,613,250 | 6.3 | NCATS | 1 | $513,078 | 0.9 |
| NIDDK | 1 | $53,810 | 0.1 | NIA | 1 | $293,303 | 0.7 | NIBIB | 2 | $485,583 | 0.8 |
| NIAAA | 1 | $30,797 | 0.1 | NIBIB | 2 | $268,543 | 0.6 | NICHD | 1 | $424,178 | 0.7 |
| NCRR | 2 | $8866 | 0.0 | NIAMS | 1 | $287,616 | 0.5 | ||||
| 79 | $37,455,181 | 76 | $41,662,423 | 87 | $58,964,735 | ||||||
NIH, National Institutes of Health; NHLBI, National Heart, Lung, and Blood Institute; NIAID, National Institute of Allergy and Infectious Diseases; NCI, National Cancer Institute; NICHD, National Institute of Child Health and Human Development; OD, Office of the Director; NCATS, National Center for Advancing Translational Sciences; NIDDK, National Institute of Diabetes and Digestive and Kidney Diseases; NIA, National Institute on Aging; NIBIB, National Institute of Biomedical Imaging and Bioengineering; NIAAA, National Institute of Alcohol Abuse and Alcoholism; NCRR, National Center for Research Resources; NIAMS, National Institute of Arthritis and Musculoskeletal and Skin Diseases.
Grant Types
R grants support specific investigator-initiated research projects in the interest/expertise of the named investigator and are considered the true measure of scientific independence. U grants foster collaboration and provide coordination/facilitation between extramural investigators and NIH staff. They provide support for projects such as the Cardiothoracic Surgical Trials Network. P grants support program projects and centers focusing on interdisciplinary disease-specific translational research, such as the Specialized Programs of Research Excellence initiative established by the NCI. K grants support mentored career development for junior faculty, and T and F grants support training and fellowship programs.
In 2010, the most frequently awarded grant types to TS-PIs included 49 R grants (accounting for 64.7% of total costs), of which 40 were R01 grants (total cost: $20.1 M) and 9 were U grants (17.7% of total costs), of which 7 were U01 grants ($4.3 M) and 8 P grants (12.7% of total costs), including 5 P01 grants ($4.3 M) and 9 K grants (3.7% of total costs), of which 8 were K08 grants ($1.1 M). Grant types and respective costs are summarized in (Figures 3, A, and E1).
FIGURE 3.
Distribution of costs with relative amounts based on grant types for 2010, 2015, and 2020. A, All TS-initiated grants. B, CV-related grants. C, Transplant-related grants. D, Oncology-related grants. CV, Cardiovascular.
FIGURE E1.
A, Total cost of each activity code for TS-PI grants in 2010, 2015, and 2020. B, Total number of grants within each activity code for TS-PIs in 2010, 2015, and 2020. TS, Thoracic surgeon.
In 2015, the most frequently awarded grant types were R grants (n = 48, comprising 53.6% of total costs), U grants (n = 13, totaling 26.1% of costs), K grants (n = 8, totaling 2.8% of costs), and P grants (n = 4, totaling 10.3% of total costs). Within each grant type, the most frequently awarded activity codes were 41 R01 grants ($20.4 M), 7 UM1 grants ($4.4 M), 3 U01 grants ($3.4 M), 5 K23 grants ($710 K), and 4 P01 grants ($4.3 M).
These trends held true for 2020. TS-PIs held 64 R grants comprising 60.4% of total costs, as well as 14 U grants, 3 P grants, and 4 K grants (accounting for 25.7%, 11.6%, and 1.2% of total costs, respectively). In 2020, the most awarded grant activity codes were R01 (55 grants totaling $31.6 M) and UM1 (5 grants with total cost $2.9 M). Additionally, there were 3 K08 grants totaling $508 K and 3 P01 grants totaling $6.9 M. Notably, the number of R01 grants increased from 40 in 2010 to 41 in 2015 and 55 in 2020. Despite this 57% increase, funding for R01s as a percent of total costs of TS-PI grants remained steady at 50% to 55%. The remaining grant activity codes for the years analyzed each comprised less than 4% of the total distributions.
Figure 3, B-D, summarizes results of additional analyses examining grant distributions across the 3 major thoracic surgery subspecialties. The majority of costs (89.1%, 87.8%, and 84.9%) for all CV grants in 2010, 2015, and 2020, respectively, were associated with R grants; costs associated with U grants for CV-related research increased from 4.1% in 2010 to 11.1% in 2015 and 13.2% in 2020, consistent with modest changes in distributions despite essentially no change in the total number of grants. Relative costs associated with R grants for transplant-related research ranged from 16% to 30% of total costs for this subspecialty at all 3 time points, and thus were considerably less than for CV-related investigations; in contrast, relative costs associated with transplant-related U grants were higher than for similar CV-related grants and remained relatively stable at approximately 40%. These data suggest a stable landscape of grant support with relatively proportionate increases in funding for the major grant categories pertaining to transplant-related research despite no appreciable changes in the number of PIs or number of grants in this discipline across the decade. In contrast, relative costs of oncology R grants increased from 42% to 61% from 2010 to 2020, and costs associated with oncology U grants more than doubled (14.2%−37.2%) during this period; these changes coincided with a modest increase in the total number of oncology grants.
Diversity of Funded Principal Investigators
Review of NIH biographical sketches and online academic and professional profiles indicated that women accounted for 6.6%, 7.9%, and 10% of NIH-funded TS in 2010, 2015, and 2020, respectively (Table 2). According to the AAMC workforce database, women comprised 4.6% to 8% of the thoracic surgery workforce in 2010, 2015, and 2019. As such, proportions of NIH-funded female TS were 1.8% in 2010, 1.8% in 2015, and 1.7% in 2020 (Table 2). Meanwhile, 1.3% to 1.4% of male TSs were NIH funded in all 3 years. In comparison, women accounted for 15.4%, 19%, and 22% of the general surgery workforce in 2010, 2015, and 2020, respectively. Proportions of NIH-funded male and female general surgeons were 0.7% and 0.9% in 2010 (P = .16), 0.9% and 1% in 2015, and 1% for both in 2020 (P = .76). Collectively, these findings reflected overall trends in nonthoracic surgical specialties. Relative to other surgical specialties, proportionally more female TSs were NIH-funded PIs in 2010 (P = .02), 2015 (P = .03), and 2020 (P = .02) (Table 2).
TABLE 2.
Proportion of funded principal investigators based on gender
| 2010 | 2015 | 2020 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||||
| Thoracic surgery | NIH-funded TSs | Funded % | Thoracic surgery | NIH-funded TSs | Funded % | Thoracic surgery | NIH-funded TSs | Funded % | |||
| Male | 4464 | 57 | 1.3 | Male | 4213 | 58 | 1.4 | Male | 4119 | 54 | 1.3 |
| Female | 217 | 4 | 1.8* | Female | 271 | 5 | 1.8* | Female | 360 | 6 | 1.7* |
| Total | 4681 | 61 | 1.3 | Total | 4484 | 63 | 1.4 | Total | 4479 | 60 | 1.3 |
|
| |||||||||||
| General surgery | NIH-funded general surgeons | Funded % | General surgery | NIH-funded general surgeons | Funded % | General surgery | NIH-funded general surgeons | Funded % | |||
|
| |||||||||||
| Male | 22,255 | 153 | 0.7 | Male | 20,398 | 179 | 0.9 | Male | 19,915 | 199 | 1 |
| Female | 4041 | 36 | 0.9 | Female | 4835 | 49 | 1.0 | Female | 5629 | 59 | 1 |
| Total | 26,296 | 189 | 0.7 | Total | 25,233 | 228 | 0.9 | Total | 25,544 | 258 | 1 |
|
| |||||||||||
| All non-TS combined | NIH-funded non-TS surgeons | Funded % | All non-TS combined | NIH-funded non-TS surgeons | Funded % | All non-TS combined | NIH-funded non-TS surgeons | Funded % | |||
|
| |||||||||||
| Male | 107,428 | 522 | 0.5 | Male | 102,410 | 716 | 0.7 | Male | 101,398 | 718 | 0.7 |
| Female | 30,732 | 132 | 0.4* | Female | 36,920 | 225 | 0.6* | Female | 42,162 | 256 | 0.6* |
| Total | 138,160 | 654 | 0.5 | Total | 139,330 | 941 | 0.7 | Total | 143,560 | 974 | 0.7 |
NIH, National Institutes of Health; TS, thoracic surgeon.
P values < .05 for the proportion of funded female TSs compared with funded female surgeons in other sugical specialties.
Total costs of female TS-initiated grants were $1.1 M, $1.5 M, and $4.2 M, in 2010, 2015, and 2020, respectively, which corresponded respectively to 3%, 3.5%, and 7.1% of NIH funding for TS-PIs for these 3 years (Table E3). Because per-capita analysis based on total costs of male versus female PI grants would be skewed by the large U and P grants awarded to male TS-PIs, and because levels of funding for the same types of grants vary among CV, transplant, and oncology (Table 3), we directly compared funding for male and female TSs with R01s in the same clinical subgroups. For CV grants, R01 per capita funding for female TS-PIs was $326 K versus $608 K for male TS-PIs in 2010, $396 K versus $605 K in 2015, and $799 K versus $821 K in 2020. Although there were no female TSs with transplant R01s in 2010 or 2015, per capita costs for transplant R01 grants were $871 K for women and $863 K for men in 2020. Last, per capita costs for oncology R01 grants were $361 K for women versus $303 K for men in 2010, compared with $405 K and $728 K, respectively, in 2020. Comparisons for 2015 could not be performed because there were no female R01 oncology grants that year. Whereas the limited number of female TS-PIs precluded formal statistical analysis, these data suggest no obvious gender disparities regarding overall NIH funding for TS-PIs. The database did not allow any verifiable analysis of races/ethnicities of the funded TS relative to the overall thoracic surgery workforce.
TABLE E3.
National Institutes of Health funding for female thoracic surgeons
| No. of surgeons | No. of grants | Cost | |
|---|---|---|---|
| 2010 | 4 | 4 | $1,141,972 |
| 2015 | 5 | 5 | $1,466,421 |
| 2020 | 6 | 7 | $4,181,073 |
TABLE 3.
Distribution of R01 grants based on gender
| 2010 CV–R01 grants | 2015 CV–R01 grants | 2020 CV–R01 grants | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| No. of TS | Cost | Average | No. of TS | Cost | Average | No. of TS | Cost | Average | |
| Male | 25 | $15,195,874 | $607,835 | 26 | $15,724,605 | $604,793 | 21 | $17,245,745 | $821,226 |
| Female | 2 | $652,250 | $326,125 | 3 | $1,187,308 | $395,769 | 3 | $2,395,861 | $798,620 |
| Total | 27 | $15,848,124 | $586,968 | 29 | $16,911,913 | $583,169 | 24 | $19,641,606 | $818,400 |
|
| |||||||||
| 2010 Transplant–R01 grants | 2015 Transplant–R01 grants | 2020 Transplant–R01 grants | |||||||
|
| |||||||||
| Male | 5 | $3,006,073 | $601,215 | 4 | $2,406,227 | $601,557 | 6 | $5,180,791 | $863,465 |
| Female | 0 | $0 | $0 | 0 | $0 | $0 | 1 | $870,551 | $870,551 |
| Total | 5 | $3,006,073 | $601,215 | 4 | $2,406,227 | $601,557 | 7 | $6,051,342 | $864,477 |
|
| |||||||||
| 2010 Oncology–R01 grants | 2015 Oncology–R01 grants | 2020 Oncology–R01 grants | |||||||
|
| |||||||||
| Male | 3 | $909,530 | $303,177 | 3 | $1,073,710 | $357,903 | 6 | $4,366,645 | $727,774 |
| Female | 1 | $360,905 | $360,905 | 0 | $0 | $0 | 1 | $404,583 | $404,583 |
| Total | 4 | $1,270,435 | $317,609 | 3 | $1,073,710 | $357,903 | 7 | $4,771,228 | $681,604 |
CV, Cardiovascular.
Additional Funding
To capture all TSs who received NIH funding during our study time points, further data mining was performed to identify TS who were listed as other PIs rather than PIs of record. Unfortunately, for 2010 and 2015, this information was not reliably recorded for all awards. However, for 2020, this analysis identified 21 TS other PIs on 27 additional grants with a total cost of $17.6 M (Figure 4, A). Six of these 21 TS other PIs had not been previously identified in our analysis, whereas the remaining 15 surgeons had already been captured as PIs of record on other grants.
FIGURE 4.
A, Distributions of grant costs with percentages and relative amounts of thoracic surgery subspecialties for awards given to TS Other PIs during 2020. B, Breakdown of costs with percentages and relative amounts of different grant types awarded to TS Other PIs in 2020. CV, Cardiovascular.
Types and costs of these 27 grants are summarized in Figure 4, B. In contrast to TS-PI grants that were predominantly CV related, oncology grants were the most common ones linked to TS multiple PI grants. Consistent with what was observed for TS-PIs, R grants with TS other PIs accounted for the majority of costs. Specifically, 18 grants were R01s totaling $9.9 M. The NCI, NHLBI, and NIAID provided the majority of funding for these grants (Table E4).
TABLE E4.
National Institutes of Health funding institutes for grants of thoracic surgeons listed as “other principal investigator”
| 2020 | ||||
|---|---|---|---|---|
|
| ||||
| No. of PIs | No. of grants | Cost | % of cost | |
| NCI | 6 | 10 | $8,811,576 | 50.0 |
| NHLBI | 12 | 14 | $7,568,873 | 43.0 |
| NIAID | 1 | 1 | $418,750 | 2.4 |
| NIAMS | 1 | 1 | $408,978 | 2.3 |
| NIBIB | 1 | 1 | $402,750 | 2.3 |
| Total | 21 | 27 | $17,610,927 | |
NCI, National Cancer Institute; NHLBI, National Heart, Lung, and Blood Institute; NIAID, National Institute of Allergy and Infectious Diseases; NIAMS, National Institute of Arthritis and Musculoskeletal and Skin Diseases; NIBIB, National Institute of Biomedical Imaging and Bioengineering; PI, principal investigator.
Distribution of Funding Based on Institution
A total of 55 of 79 grants in 2010, 52 of 76 grants in 2015, and 74 of 87 grants in 2020, which accounted for 73.6%, 77.3%, and 84.2% of total costs, respectively, were held by TS PIs who were affiliated with one of the top 50 NIH-funded (elite) institutions in the United States. Awards to 5 senior surgeons accounted for 32% to 33% of total NIH costs for TS-PIs in 2010, 2015, and 2020. Although only 1 surgeon ranked among these top 5 across all 3 years, 3 were the same in 2015 and 2020 (Table E5). Eight of these most highly funded surgeons were affiliated with elite institutions. Likewise, 21 of 27 grants with TS other PIs including 5 of the 6 grants with TS Other PIs who were not captured as PIs on other grants were awarded to investigators at medical centers ranking among the top 50 NIH-funded institutions in the United States.
TABLE E5.
Grant distribution of top 5 funded thoracic surgeon principal investigator grants
| 2010 | |||
|---|---|---|---|
|
| |||
| No. of grants | Cost | % of cost | |
| R grants | 7 | $5,352,368 | 44.6 |
| P grants | 1 | $2,658,462 | 22.2 |
| U grants | 3 | $3,986,090 | 33.2 |
| Transplant | 6 | $8,483,325 | 70.7 |
| CV | 5 | $3,513,595 | 29.3 |
| Total | 11 | $11,996,920 | |
|
| |||
| 2015 | |||
|
| |||
| No. of grants | Cost | % of cost | |
|
| |||
| R grants | 5 | $2,689,118 | 20.4 |
| P grants | 3 | $4,010,688 | 30.4 |
| U grants | 2 | $3,888,548 | 29.4 |
| DP2 grants | 1 | $2,613,250 | 19.8 |
| Transplant | 8 | $11,279,472 | 85.4 |
| CV | 3 | $1,922,132 | 14.6 |
| Total | 11 | $13,201,604 | |
|
| |||
| 2020 | |||
|
| |||
| No. of grants | Cost | % of cost | |
|
| |||
| R grants | 5 | $3,359,984 | 17.2 |
| P grants | 3 | $6,862,654 | 35.1 |
| U grants | 4 | $9,335,411 | 47.7 |
| Transplant | 8 | $15,554,874 | 79.5 |
| CV | 3 | $2,162,610 | 11.1 |
| Oncology | 1 | $1,840,565 | 9.4 |
| Total | 12 | $19,558,049 | |
CV, Cardiovascular.
DISCUSSION
Because of conflicting reports, it is difficult to accurately assess NIH funding for surgeon-scientists over the past 2 decades. Several studies have highlighted increased numbers of grant applications, as well as decreased numbers of awarded grants including lower funding rates for surgeons, which collectively have made an already competitive environment even more challenging for aspiring surgeon-scientists.14,16,17,20,21 In contrast, other studies have portrayed a more favorable funding environment for surgeon-scientists. For instance, Demblowski and colleagues19 recently noted that numbers of surgeon-scientists increased as did NIH funding for these PIs between 2010 and 2020. Discrepancies regarding NIH funding for surgeons described in these various reports could be related, at least in part, to dates of publications, time windows evaluated, and types of data analyzed.
Although the present study does not fully depict the status of funding for TS-scientists because it focused primarily on only 3 time points (2010, 2015, 2020), it does provide a reasonably complete picture of the NIH funding landscape for our discipline. On the surface, our data suggest a favorable funding environment. TSs were funded proportionately higher than the mean for all other surgical specialties, exceeding most individual specialties in 2010, 2015, and 2020. Additionally, total costs of TS-initiated grants increased at rates that outpaced expansions in total yearly NIH budgets. Furthermore, numbers of NIH-funded female TS-PIs were reflective of the percentages of women comprising the thoracic surgery workforce during all 3 years.18 Whereas limited numbers prevented any formal statistical analysis, overall levels of funding for male and female TSs with comparable grant types did not appear to differ.
From an opposing perspective, thoracic surgery was among the few specialties with no increase in the number of NIH-funded PIs between 2010 and 2020 (Figure 5). Furthermore, 5 senior surgeons accounted for 33% of total NIH funding for TS-PIs at all 3 time points. These funds are not truly reflective of individual investigator-initiated research grants because more than half of the costs associated with these surgeons were due to U or P grants. The total costs for U grants increased 155% from 2010 to 2020. As such, increased costs due to expansion of U and P grants could create a false impression of a robust increase in NIH funding for TS-initiated research. Consistent with this notion, R01s constituted the predominant grant type awarded to TSs during all 3 years, whereas numbers and costs of these grants increased, the rise in R01 grants was relatively modest, and the proportion of R01 costs-to-total costs for TS-PI grants did not change over the decade. These observations are particularly concerning for future academic vitality of thoracic surgery.
FIGURE 5.
Graphical Abstract depicting the number of NIH-funded TS PIs and total grant numbers and associated costs from 2010 to 2020. NIH, National Institutes of Health; TS, thoracic surgeon; PI, principal investigator.
Our analysis indicated that TS-PIs conducting transplant-related research had the highest per capita grant costs ($1.2 M in 2010; $1.4 M in 2015; $2.3 M in 2020) as well as the highest proportion of P and U grant funding. TS-PIs conducting CV-related research had the second highest per capita funding ($515 K in 2010; $514 K in 2015; $728 K in 2020) and oncology-related research had the least ($304 K in 2010; $344 K in 2015; $722 K in 2020). However, if only R01 grants are considered, the per capita costs for each subspecialty were closer (2010: transplant $601 K, CV $587 K, and oncology $318 K; 2015: transplant $602 K, CV $583 K, and oncology $358 K; 2020: transplant $864 K, CV $818 K, and oncology $682 K).
K08 (career development) grants have correlated with academic productivity and progression to R01 grant acquisition.17,22,23 K grants are designed to provide time for junior surgeon-scientists to hone their research skills under dedicated mentorship, thereby making them more competitive for extramural funding.21–23 Several studies have demonstrated that the rates with which surgeons, including TSs, convert K08 grants to R01 grants are comparable to other clinician-investigators (40%−50%) within a 5- to 10-year period.11,17,22,23 Despite a high conversion rate (all TS-PIs with K08 grants in 2010 secured R01 grants by 2020), the total number of K08 grants and the proportion of costs for these grants relative to total costs decreased from 2010 to 2020. This reduction may be related to several factors including the $100,000 cap on NIH contributions to the investigator’s salary in exchange for 75% dedicated research time, leaving the remainder of the surgeon’s salary to be covered at the departmental level despite reduced overall clinical productivity.14,17,24 Additionally, selecting a strong mentor with experience in the proposed research field supported by R01 grant funding is crucial for recipients of K08 awards, and with only 39 TS-PIs with R01 grants in 2020, the options for junior TS-scientists to be mentored by established TS-PIs may be limited.13,14,23–25
Dedicated time for research during training has been shown to be beneficial to TSs because it has been linked to higher career-long academic productivity, increased rates of NIH funding, accelerated promotions, and a higher number of ongoing publications.12,13,22,26–28 Furthermore, dedicated time for research has a positive effect on career selection, with one study noting that trainees supported by a thoracic surgery T32 grant were more likely to pursue thoracic surgery after residency (40% vs 7%).26–28 We observed no change in the numbers of T32 grants from 2010 to 2020, with only 2 thoracic surgery T32 grants at all 3 time points. Admittedly, our analysis did not capture T32 grants that were awarded to non-TSs that could be supporting TS trainees; therefore, our data may underestimate the number of T32 grants. Nevertheless, our results raise concerns that decreased investment in the development of surgeon-scientists will lead to further academic stagnation in thoracic surgery.
Study Limitations
Potential limitations of our study include that we focused primarily on 3 time points. As such, we may have not fully captured various nuances pertaining to NIH funding for TSs from 2010 to 2020. Furthermore, the database did not allow us to ascertain total numbers of grant applications submitted by TS, which would have enabled a better assessment of whether the lack of expansion of TS-initiated research reflects insurmountable barriers to entry or instead is indicative of an overall decrease in engagement of TS in the highly competitive process of NIH-funded investigation. Additionally, whereas our analysis did identify some TSs who were engaged as other PIs but not PIs of record on NIH-funded grants, a potentially positive sign of ongoing academic productivity, we were unable to gather full data pertaining to this activity, including specific roles of these other PIs on their respective grants. Last, our analysis did not include any assessment of non-NIH funding (ie, Department of Defense, pharma, biomedical companies, or private donations), which in some cases could be substantial and reflect the ability of TS to creatively adapt to limited opportunities for NIH-funding to support long-term research endeavors. Despite these limitations, our comprehensive analysis provides potentially important insight into the status of NIH funding for TSs, which continues to be the metric of personal and institutional productivity in biomedical research.
CONCLUSIONS
Because of an aging TS workforce and diminishing numbers of trainees, it is predicted that there will be a shortage of TSs in the United States by 2035.29–31 In light of the decreasing workforce, an increasingly competitive environment, and a stagnant funding landscape, we must question whether the future of TS-initiated research is in jeopardy. Although the Thoracic Surgery Foundation for Research and Education and other AATS funding initiatives have fostered the development of junior and mid-level TSs,22,32,33 such efforts may be insufficient to maintain current numbers of TS-PIs and preserve the academic vitality of our specialty. Structural changes must be implemented to more effectively nurture the next generation of TS-scientists. The traditional model of taking 2 or 3 years out of general surgery residency for dedicated research and subsequently reengaging in these activities once clinical training has been completed is inefficient, unrealistic, and unsustainable in the current era, particularly given the ongoing shift to integrated residencies that may further limit flexibilities for dedicated research time. Structured research (clinical or lab-based) should be fully integrated into the academic mission of residency training and tracked as a metric of program performance; there is already evidence that such efforts can significantly enhance academic productivity and accelerate career trajectories of aspiring TSs.34 Furthermore, irrespective of research experience gained during residency training, protected time, dedicated mentorship, and sustained financial support are essential for junior attending surgeons to fully mature and to successfully compete for external funding. Such “R and D” efforts are challenging and costly. Although the recently established NCI Early-stage Surgeon Scientist Program (https://www.cancer.gov/grants-training/training/funding/nci-essp) could serve as a model for academic development of clinician-investigators, this initiative alone cannot cover all costs required to train the next generation of TS-scientists. Ultimately, we are responsible for ensuring our academic survival. There are already programs with cultures in which research endeavors are fully valued as core components of their academic missions.13,14,35,36 The path to increased NIH funding for TSs has been illuminated; it is up to us to follow the light.
CENTRAL MESSAGE.

In light of a decreasing workforce, increasingly competitive funding climate, and stagnant funding landscape, we must consider structural changes to foster the next generation of TS scientists.
The number of NIH-funded TS-PIs has remained unchanged in the past decade.
PERSPECTIVE.
NIH funding has been used as a benchmark of research productivity. We analyzed TS-PIs on NIH-funded grants in 2010, 2015, and 2020. Despite increases in total grant numbers and associated costs, numbers of TS-PIs, proportion of R01 costs-to-total costs, and training/development grants were stagnant.
Acknowledgments
This work was supported by National Institutes of Health intramural grant (ZIA BC 011115; DSS) and the Stephen J. Solarz Memorial Fund at the Foundation for the National Institutes of Health.
The authors thank Jan Pappas for administrative assistance.
Abbreviations and Acronyms
- AAMC
Association of American Medical Colleges
- CV
cardiovascular
- NCI
National Cancer Institute
- NHLBI
National Heart Lung and Blood Institute
- NIAID
National Institute of Allergy and Infectious Diseases
- NIH
National Institutes of Health
- PI
principal investigator
- TS
thoracic surgeon
Footnotes
Scanning this QR code will take you to the table of contents to access supplementary information.
Conflict of Interest Statement
The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
References
- 1.Khaitan PG, D’Amico TA. Milestones in thoracic surgery. J Thorac Cardiovasc Surg. 2018;155:2779–89. 10.1016/j.jtcvs.2017.12.149 [DOI] [PubMed] [Google Scholar]
- 2.Tesler UF. A History of Cardiac Surgery: An Adventurous Voyage from Antiquity to the Artificial Heart. UK Cambridge Scholars Publishing; 2020. [Google Scholar]
- 3.Altorki NK, Borczuk AC, Harrison S, Groner LK, Bhinder B, Mittal V, et al. Global evolution of the tumor microenvironment associated with progression from preinvasive invasive to invasive human lung adenocarcinoma. Cell Rep. 2022;39:110639. 10.1016/j.celrep.2022.110639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Awad MA, Shah A, Griffith BP. Current status and outcomes in heart transplantation: a narrative review. Rev Cardiovasc Med. 2022;23:11. 10.31083/j.rcm2301011 [DOI] [PubMed] [Google Scholar]
- 5.Bueno R, Stawiski EW, Goldstein LD, Durinck S, De Rienzo A, Modrusan Z, et al. Comprehensive genomic analysis of malignant pleural mesothelioma identifies recurrent mutations, gene fusions and splicing alterations. Nat Genet. 2016; 48:407–16. 10.1038/ng.3520 [DOI] [PubMed] [Google Scholar]
- 6.Selzman CH, Feller ED, Walker JC, Sheridan BC, Silvestry SC, Daly RC, et al. The Jarvik 2000 left ventricular assist device: results of the United States Bridge to Transplant Trial. ASAIO J. April 13, 2022. [Epub ahead of print]. 10.1097/MAT.0000000000001750 [DOI] [PubMed] [Google Scholar]
- 7.Testa JR, Cheung M, Pei J, Below JE, Tan Y, Sementino E, et al. Germline BAP1 mutations predispose to malignant mesothelioma. Nat Genet. 2011;43:1022–5. 10.1038/ng.912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yuan G, Flores NM, Hausmann S, Lofgren SM, Kharchenko V, Angulo-Ibanez M, et al. Elevated NSD3 histone methylation activity drives squamous cell lung cancer. Nature. 2021;590:504–8. 10.1038/s41586-020-03170-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bajaj SS, Wang H, Williams KM, Pickering JM, Heiler JC, Manjunatha K, et al. National Institutes of Health R01 grant funding is associated with enhanced research productivity and career advancement among academic cardiothoracic surgeons. Semin Thorac Cardiovasc Surg. 2021;33:1047–56. 10.1053/j.semtcvs.2020.12.002 [DOI] [PubMed] [Google Scholar]
- 10.Narahari AK, Charles EJ, Mehaffey JH, Hawkins RB, Sharma AK, Laubach VE, et al. Can lung transplant surgeons still be scientists? High productivity despite competitive funding. Heart Surg Forum. 2019;22:E001–7. 10.1532/hsf.2024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Narahari AK, Mehaffey JH, Chandrabhatla AS, Hawkins RB, Charles EJ, Roeser ME, et al. Longitudinal analysis of National Institutes of Health funding for academic thoracic surgeons. J Thorac Cardiovasc Surg. 2022;163:872–9.e2. 10.1016/j.jtcvs.2021.01.088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosati CM, Valsangkar NP, Gaudino M, Blitzer D, Vardas PN, Girardi LN, et al. Training patterns and lifetime career achievements of us academic cardiothoracic surgeons. World J Surg. 2017;41:748–57. 10.1007/s00268-016-3760-2 [DOI] [PubMed] [Google Scholar]
- 13.Wang H, Bajaj SS, Krishnan A, Heiler JC, Williams KM, Pickering JM, et al. Characterization of cardiothoracic surgeons actively leading basic science research. J Surg Res. 2021;268:371–80. 10.1016/j.jss.2021.06.065 [DOI] [PubMed] [Google Scholar]
- 14.Ikonomidis JS, Menasche P, Kreisel D, Sellke FW, Woo YJ, Colson YL. Attrition of the cardiothoracic surgeon-scientist: definition of the problem and remedial strategies. J Thorac Cardiovasc Surg. 2019;158:504–8. 10.1016/j.jtcvs.2019.03.057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Keswani SG, Moles CM, Morowitz M, Zeh H, Kuo JS, Levine MH, et al. The future of basic science in academic surgery: identifying barriers to success for surgeon-scientists. Ann Surg. 2017;265:1053–9. 10.1097/SLA.0000000000002009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mann M, Tendulkar A, Birger N, Howard C, Ratcliffe MB. National institutes of health funding for surgical research. Ann Surg. 2008;247:217–21. 10.1097/SLA.0b013e3181568e26 [DOI] [PubMed] [Google Scholar]
- 17.Narahari AK, Mehaffey JH, Hawkins RB, Charles EJ, Baderdinni PK, Chandrabhatla AS, et al. Surgeon scientists are disproportionately affected by declining NIH funding rates. J Am Coll Surg. 2018;226:474–81. 10.1016/j.jamcollsurg.2017.12.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Colleges AoAM. Physician specialty data report. Washington, DC, US: 2010–2020. Accessed December 28, 2021. https://www.aamc.org/data-reports/workforce/report/physician-specialty-data-report [Google Scholar]
- 19.Demblowski LA, Busse B, Santangelo G, Blakely AM, Turner PL, Hoyt DB, et al. NIH funding for surgeon-scientists in the US: what is the current status? J Am Coll Surg. 2021;232:265–74.e2. 10.1016/j.jamcollsurg.2020.12.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rangel SJ, Moss RL. Recent trends in the funding and utilization of NIH career development awards by surgical faculty. Surgery. 2004;136:232–9. 10.1016/j.surg.2004.04.025 [DOI] [PubMed] [Google Scholar]
- 21.Ratcliffe MB, Howard C, Mann M, del Nido P. National Institutes of Health funding for cardiothoracic surgical research. J Thorac Cardiovasc Surg. 2008;136: 392–7; discussion 398–9. 10.1016/j.jtcvs.2008.04.009 [DOI] [PubMed] [Google Scholar]
- 22.Jones DR, Mack MJ, Patterson GA, Cohn LH. A positive return on investment: research funding by the Thoracic Surgery Foundation for Research and Education (TSFRE). J Thorac Cardiovasc Surg. 2011;141:1103–6. 10.1016/j.jtcvs.2011.03.010 [DOI] [PubMed] [Google Scholar]
- 23.Narahari AK, Mehaffey JH, Hawkins RB, Baderdinni PK, Chandrabhatla AS, Tribble CG, et al. Cardiothoracic and vascular surgeons achieve high rates of K award conversion into R01 funding. Ann Thorac Surg. 2018;106:602–7. 10.1016/j.athoracsur.2018.02.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brock MV, Bouvet M. Writing a successful NIH Mentored Career Development Grant (K award): hints for the junior faculty surgeon. Ann Surg. 2010;251: 1013–7. 10.1097/SLA.0b013e3181deb4ef [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Scott JD, Carlson DE. K08 and K99 cardiovascular training: comparisons and trends among current awardees. Circ Res. 2012;110:910–4. 10.1161/RES.0b013e3182533291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ko CY, Whang EE, Longmire WP Jr, McFadden DW. Improving the surgeon’s participation in research: is it a problem of training or priority? J Surg Res. 2000;91:5–8. 10.1006/jsre.2000.5855 [DOI] [PubMed] [Google Scholar]
- 27.Narahari AK, Charles EJ, Mehaffey JH, Hawkins RB, Schubert SA, Tribble CG, et al. Cardiothoracic surgery training grants provide protected research time vital to the development of academic surgeons. J Thorac Cardiovasc Surg. 2018;155: 2050–6. 10.1016/j.jtcvs.2017.12.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang H, Bajaj SS, Williams KM, Heiler JC, Pickering JM, Manjunatha K, et al. Early engagement in cardiothoracic surgery research enhances future academic productivity. Ann Thorac Surg. 2021;112:1664–71. 10.1016/j.athoracsur.2020.10.013 [DOI] [PubMed] [Google Scholar]
- 29.Byrd CT, Williams KM, Backhus LM. A brief overview of thoracic surgery in the United States. J Thorac Dis. 2022;14:218–26. 10.21037/jtd-21-1504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ikonomidis JS, Boden N, Atluri P. The Society of Thoracic Surgeons Thoracic Surgery practice and access task force-2019 workforce report. Ann Thorac Surg. 2020;110:1082–90. 10.1016/j.athoracsur.2020.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shemin RJ, Ikonomidis JS. Thoracic surgery workforce: report of STS/AATS Thoracic Surgery practice and access task force–snapshot 2010. J Thorac Cardiovasc Surg. 2012;143:39–46. 46.e1–6. 10.1016/j.jtcvs.2011.10.022 [DOI] [PubMed] [Google Scholar]
- 32.Aranda-Michel E, Arnaoutakis G, Kilic A, Bavaria J, Szeto WY, Yousef S, et al. Thoracic surgery foundation research awards: leading the way to excellence. Ann Thorac Surg. 2022;113:1015–20. 10.1016/j.athoracsur.2021.04.012 [DOI] [PubMed] [Google Scholar]
- 33.Mehaffey JH, Wang H, Narahari AK, Bajaj SS, Chandrabhatla AS, Krupnick AS, et al. The impact of the American Association for Thoracic Surgery on National Institutes of Health grant funding for cardiothoracic surgeons. J Thorac Cardiovasc Surg. October 28, 2021 [Epub ahead of print]. 10.1016/j.jtcvs.2021.10.031 [DOI] [PubMed] [Google Scholar]
- 34.Coyan GN, Sultan I, Seese LM, Chu D, Schuchert MJ, Kinnunen A, et al. Implementation of a protocol to increase the academic productivity of cardiothoracic surgery resident physicians. J Thorac Cardiovasc Surg. 2022; 163:739–45. 10.1016/j.jtcvs.2020.09.122 [DOI] [PubMed] [Google Scholar]
- 35.Schutz A, LeMaire SA, Trautner BW, Rosengart TK. Commentary: building an academic cardiothoracic surgical program: the Baylor experience. J Thorac Cardiovasc Surg. 2022;163:1435–6. 10.1016/j.jtcvs.2021.04.081 [DOI] [PubMed] [Google Scholar]
- 36.Yarboro LT, Mehaffey JH, Charles EJ, Kron IL. How to build and sustain an academic cardiothoracic surgery program. J Thorac Cardiovasc Surg. 2022;163: 1431–4. 10.1016/j.jtcvs.2021.03.129 [DOI] [PubMed] [Google Scholar]