Abstract
Krokodil, the street name for desomorphine, has emerged as a deadly and alarming drug phenomenon in recent years. This report delves into the intricate relationship between krokodil abuse, its adverse effects on the skin and its profound impact on cardiovascular events. Our patient developed a non-healing cutaneous ulceration associated with an acute onset of cardiac arrhythmia, as well as bilateral upper extremity acute deep-vein thrombosis.
LEARNING POINTS
The use of Krokodil can lead to chronic non-healing ulcerations.
It is important to be aware that new cardiac arrhythmias can arise in individuals using krokodil.
Acute bilateral upper extremity thrombosis can occur as a complication in patients using krokodil.
Keywords: Krokodil, morphine, desomorphine, skin ulcer, necrosis
INTRODUCTION
The rise of krokodil abuse serves as a stark reminder of the harsh outcomes that result from the convergence of illicit substance consumption, desperate situations and the manipulation of pharmaceutical chemistry[1]. Emerging in Russia during the early 2000s, krokodil is a synthetic opioid derived from morphine, mixed with accessible and inexpensive additives[1,2]. These additives, which encompass hydrochloric acid, red phosphorus sourced from matchbook striking surfaces, iodine, petrol and paint thinner, are believed to play a role in the profound skin-related consequences associated with krokodil use[1–4].
CASE DESCRIPTION
A 19-year-old male was admitted to our hospital with a non-healing skin ulcer persisting for three weeks, which affected his left hand and extended to the wrist (Fig. 1). The patient had undergone surgical debridement three weeks prior, but the condition showed limited improvement. He admitted a recent history of a suicide attempt and a longstanding pattern of polysubstance abuse, involving krokodil and ethanol. Two days before admission, the patient experienced progressive palpitations. Further evaluation showed supraventricular tachycardia (SVT) (Fig. 2). Physical examination of the ulcer unveiled stage II/III and noticeable purulent discharge (Fig. 1). Furthermore, a grade II tricuspid systolic murmur was detectable. Laboratory investigation and radiographic studies showed no abnormalities except for a slight elevation in leukocyte count, mild transaminitis and increased brain natriuretic peptide (16,500 pg/ml); the ultrasound showed bilateral upper extremity acute deep-vein thrombosis (Fig. 3). The patient’s management comprised cefepime, clindamycin, apixaban (Eliquis) and surgical debridement.
Figure 1.
Krokodil-induced cutaneous ulceration is evident in the form of a stage III ulcer on the right hand, characterised by an irregular margin. This ulcer is accompanied by signs of infection, including purulent discharge. Additionally, there is the presence of granulation tissue and desquamation in the surrounding area of the ulcer.
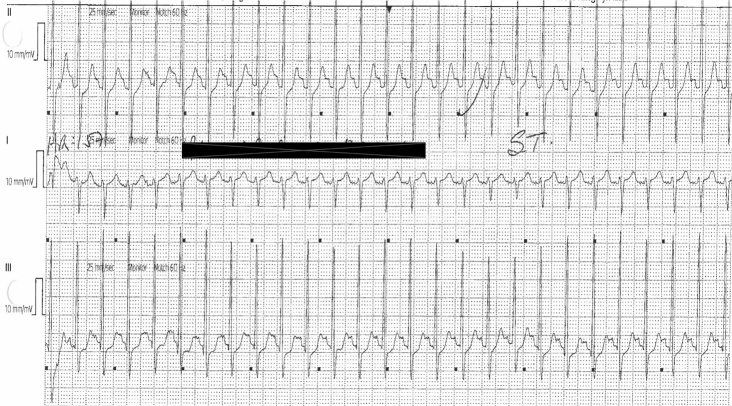
Figure 2.
Electrocardiography reveals the presence of SVT triggered by the use of krokodil.
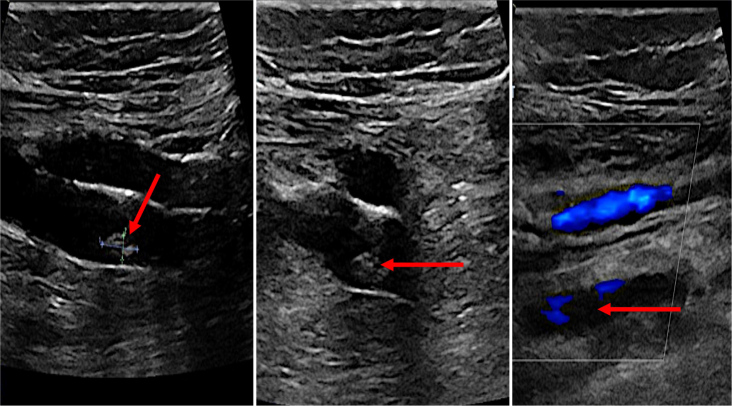
Figure 3.
The venous ultrasound showed bilateral upper extremity deep venous thrombosis (red arrows).
DISCUSSION
The emergence of krokodil abuse has raised significant concerns for public health. Its notorious link to severe skin necrosis and non-healing ulcers is particularly alarming. In our patient, we are reporting two crucial coexisting associations: krokodil leads to both cutaneous manifestations and cardiac arrhythmia.
Desomorphine, a morphine derivative, stands as a synthetic opioid renowned for its robust analgesic qualities[5]. The process of its synthesis entails readily available and cost-effective precursor chemicals, which adds to its appeal for illicit drug producers[3–5]. The swift commencement of its effects and the profound euphoria it induces render it enticing for individuals in pursuit of a potent high[6].
A hallmark consequence of krokodil abuse is the emergence of severe skin necrosis[6,7]. This phenomenon arises from the toxic by-products generated during the crude synthesis of desomorphine, causing harm to tissues and localised necrosis[5,7]. The drug’s vasoconstrictive attributes, combined with contamination from solvents and chemicals used in the synthesis process, further intensify tissue damage[4,5,7].
The solution injected, comprising petrol and hydrochloric acid, results in discoloured scaling and ulceration[8,9]. Concurrently, iodine inflicts notable harm on muscles and the endocrine system. Additionally, red phosphorous contributes to the deterioration of cartilaginous tissues and bones, extending even to the development of jaw osteomyelitis[4,8,9]. Amid these toxic by-products, substances such as iron, zinc and lead are implicated in a range of adverse effects[1,8,9]. These encompass neurological complications as well as impairments to the liver and kidneys[8,9].
Based on our knowledge, a single instance of fatal endomyocarditis has been linked to krokodil abuse[2]. Our patient exhibited sudden-onset SVT accompanied by thrombi in the upper limbs. While a definitive causal mechanism for these conditions remains elusive, we propose a potential connection to the adverse effects of the additives.
There is no definitive treatment for krokodil-related skin or systemic complications. However, addressing krokodil-induced skin necrosis demands a comprehensive approach, involving wound management, infection control and, in critical scenarios, surgical intervention. In the most severe cases, extensive debridement, skin grafts and even amputation might be necessary[9].
CONCLUSION
In conclusion, krokodil abuse, facilitated by the synthesis of desomorphine and characterised by severe skin necrosis and cardiac complications, presents a multifaceted threat to individual health and public well-being. This report underscores the urgent need for comprehensive research, education and intervention efforts to combat the detrimental effects of krokodil and protect individuals from its devastating consequences.
Footnotes
Conflicts of Interests: The Authors declare that there are no competing interests.
Patient Consent: The patient has provided written informed consent and had no objections or comments regarding the publication of this case report and its content.
REFERENCES
- 1.Grun JPC, Latypov A, Harris M. Breaking worse: the emergence of krokodil and excessive injuries among people who inject drugs in Eurasia. Int J Drug Policy. 2013;24:265–274. doi: 10.1016/j.drugpo.2013.04.007. [DOI] [PubMed] [Google Scholar]
- 2.Sorrentino A, Trotta S, Colucci AP, Aventaggiato L, Marzullo A, Solarino B. Lethal endomyocarditis caused by chronic ‘Krokodil’ intoxication. Forensic Sci Med Pathol. 2018;14:229–235. doi: 10.1007/s12024-018-9967-9. [DOI] [PubMed] [Google Scholar]
- 3.Haskin A, Kim N, Aguh C. A new drug with a nasty bite: a case of krokodil-induced skin necrosis in an intravenous drug user. JAAD Case Rep. 2016;2:174–176. doi: 10.1016/j.jdcr.2016.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Poghosyan YM, Hakobyan KA, Poghosyan AY, Avetisyan EK. Surgical treatment of jaw osteonecrosis in ‘Krokodil’ drug addicted patients. J Craniomaxillofac Surg. 2014;42:1639–1643. doi: 10.1016/j.jcms.2014.05.005. [DOI] [PubMed] [Google Scholar]
- 5.Thekkemuriyi DV, John SG, Pillai U. ‘Krokodil’ – a designer drug from across the Atlantic, with serious consequences. Am J Med. 2014;127:e1–e2. doi: 10.1016/j.amjmed.2013.09.030. [DOI] [PubMed] [Google Scholar]
- 6.Katselou M, Papoutsis I, Nikolaou P, Spiliopoulou C, Athanaselis S. A ‘krokodil’ emerges from the murky waters of addiction. Abuse trends of an old drug. Life Sci. 2014;102:81–87. doi: 10.1016/j.lfs.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 7.Shelton M, Ramirez-Fort MK, Lee KC, Ladizinski B. Krokodil: from Russia with love. JAMA Dermatol. 2015;151:32. doi: 10.1001/jamadermatol.2014.1025. [DOI] [PubMed] [Google Scholar]
- 8.Neves JF, Alves EA, Soares JX, Cravo SM, Silva AMS, Pereira Netto AD, et al. Data analysis of ‘krokodil’ samples obtained by street-like synthesis. Data Brief. 2015;6:83–8. doi: 10.1016/j.dib.2015.11.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Haskin A, Kim N, Aguh C. Reply to: ‘Commentary on “A new drug with a nasty bite: a case of krokodil-induced skin necrosis in an intravenous drug user”’. JAAD Case Rep. 2016;2:424. doi: 10.1016/j.jdcr.2016.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]