ABSTRACT
Chikungunya fever (CHIK) is a neglected tropical disease associated with chronic arthritis. CHIK is usually a self-limiting condition; however, extra-articular manifestations present as atypical illness in a minority of patients. These atypical features may mimic other conditions and potentially distract physicians from the true diagnosis. This review analyzes the evidence of many unusual extra-articular manifestations reported in cases of CHIK. Depending on the affected system, these unusual manifestations include encephalitis, myocarditis, acute interstitial nephritis, cutaneous manifestations, acute anterior uveitis, abdominal pain, and depression. In addition, coinfections and comorbidities may cause atypical illness and obscure the diagnosis. Further studies are required to clarify the pathophysiology and natural history of CHIK, as it remains a burdening condition. Exploring its atypical symptoms may be the missing scientific piece of this puzzle.
Keywords: Chikungunya, Arbovirus infection, Cardiovascular abnormalities, Kidney diseases, Neurologic manifestations, Skin manifestations
INTRODUCTION
The chikungunya virus (CHIKV) is a mosquito-transmitted arthritogenic virus responsible for outbreaks of an acute febrile syndrome called chikungunya fever (CHIK). There are three distinct clades: the West African, Asian, and East/Central/South African (ECSA) genotypes. Most patients develop prominent symptoms of arthritis 1 . CHIK is usually self-limiting; however, some patients may present with atypical symptoms other than fever and arthralgia, potentially leading to fatal outcomes or leave long-term sequelae, such as encephalitis, myocarditis, nephritis, and deforming skin lesions 2 . The frequency of these unusual manifestations varies in the literature, ranging between 5% and 80%. Notably, older patients, pregnant women, and newborns exhibit higher susceptibility to these more severe presentations 3 - 6 .
When faced with atypical symptoms, diagnosing CHIK is more challenging. Given that CHIK is a severely neglected tropical disease, few studies have adequately characterized these atypical cases 1 . The quality and rarity of available data often limit existing reviews. This scarcity of data affects disease management, as physicians lack evidence to support specific treatment strategies and are compelled to treat patients empirically. Complications in the treatment of these unusual CHIK patients are also poorly described, and the impact of comorbidities on disease expression is also not well understood 7 .
In this narrative review, we outline the current knowledge regarding the atypical, often severe, extra-articular presentations of CHIK infection, providing valuable insights into its pathophysiology, clinical picture, and management. Additionally, we discuss the prognoses of these manifestations and highlight the challenges and perspectives in managing possible sequelae.
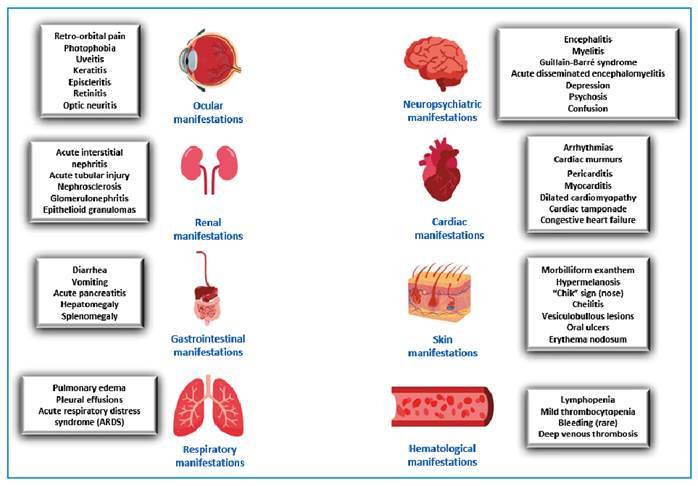
Figure 1 shows the main extra-articular manifestations of CHIK, which will be discussed below.
FIGURE 1: Overview of extra-articular manifestations of Chikungunya fever.
NEUROLOGICAL MANIFESTATIONS
Although CHIKV is not typically considered a neurotropic virus, sporadic cases of nervous system involvement have been reported since the 1960s 8 . The neurovirulence of the Asian genotype is believed to be the highest among the viral strains 9 .
The frequency of nervous system involvement in patients with CHIK ranges from 7 to 33 %. The most frequently observed complication is encephalitis, followed by myelitis, encephalomyelitis, Guillain-Barré syndrome, acute disseminated encephalomyelitis, optic neuropathy, and neuroretinitis. Less frequently reported complications include seizures, sensorineural hearing loss, stroke, cerebellitis, meningism, cranial nerve palsy, carpal tunnel syndrome, ophthalmoplegia, and disorientation 8 , 10 - 14 .
Previous studies have documented that children are more susceptible to neurological disease than adults 8 , 11 , 15 . Maternal-fetal transmission is a major risk factor for the development of neuro-Chikungunya, resulting in neurological symptoms and neurodevelopmental delay in up to 50% of infected neonates 16 .
Coinfection with other arboviruses, such as Zika and dengue viruses, is associated with more severe neurological disease, necessitating intensive care support and prolonged hospitalization. Additionally, cerebrovascular disease is three times more common in patients with dual infections than in those with mono-infection 11 .
Treatment of CHIK neurological disease is typically symptomatic. The prognosis is variable, although most patients with neurological disease recover without sequelae. During CHIK infection, multiple organ systems can be simultaneously involved with neurological disease; therefore, a multidisciplinary approach is critical 9 .
CARDIOVASCULAR MANIFESTATIONS
Cardiovascular manifestations are one of the most common extra-articular features of CHIK infection, affecting up to 54.2% of the infected patients 17 . The mechanism of cardiac involvement in CHIK remains unclear and may be multifactorial. In some patients, cardiac symptoms are primarily related to CHIK infection; however, in others, cardiovascular disease may be secondary to pre-existing comorbidities 3 . Animal models have revealed active replication of CHIKV in the hearts of immunodeficient mice, and human biopsies have shown CHIKV in the myocardium, suggesting that direct viral infection plays a pathogenic role in CHIK cardiac disease 18 , 19 .
The protean cardiovascular manifestations of CHIK include pericarditis, cardiac tamponade, hypotension, shock, Raynaud’s phenomenon, arrhythmias, cardiac murmurs, myocarditis, dilated cardiomyopathy, congestive insufficiency, and heart failure. Approximately 22% of fatal CHIK cases are caused by cardiovascular diseases, with heart failure being the most common. The most commonly reported abnormality in the electrocardiograms of patients with CHIK is the inversion of T waves in leads DII, III, aVF, V5-V6, and elevation of the ST segment 20 - 22 . Most patients who do not die from acute cardiac involvement completely recover; however, case reports show that cardiovascular compromise can cause subacute and chronic illness, emphasizing the need for longitudinal recognition and management of patients with atypical CHIK 23 - 24 .
As with other arboviral infections, the optimal management of cardiovascular complications in patients with CHIK remains uncertain. The sporadic nature of cardiac CHIK cases limits these studies. Some unanswered questions include the lack of data on whether different CHIK viral strains affect cardiac susceptibility. From a treatment perspective, similar to other forms of viral myocarditis, the role of corticosteroids remains uncertain. The most crucial steps in management involve early monitoring and rapid intervention to prevent sequelae 19 , 20 , 25 , 26 .
HEMATOLOGIC MANIFESTATIONS
CHIKV infection causes milder laboratory abnormalities compared to infection. While mild thrombocytopenia may occur, severe cases are rare, with platelet levels usually above 100,000/µl. Lymphopenia is the most common abnormality, observed in approximately 80% of patients. Hemorrhagic complications are rare in CHIKV infection 27 - 29 . A relationship with deep venous thrombosis has also been proposed, with one study showing increased D-dimer levels in 63.8% of patients 30 .
RENAL MANIFESTATIONS
Renal complications have been reported in 21%-45% of CHIK cases and are more common among severely ill patients. Most of these patients have renal comorbidities, particularly chronic kidney disease, which contributes to high mortality rate 31 . It is still unknown whether the kidneys serve as reservoirs of the virus 32 . However, one study that evaluated patients with post-mortem biopsy-proven kidney injury established after CHIK infection did not detect viral antigens in the kidneys 33 .
Acute interstitial nephritis and tubular injury were the most common renal findings 3 , 31 . Nephrosclerosis, membranoproliferative glomerulonephritis, and epithelioid granulomas have been less frequently reported. Among patients with acute interstitial nephritis, high serum creatinine levels manifest as impaired renal function 34 . In one study that evaluated co-infection with other arboviruses, renal manifestations were uncommon and did not affect prognosis 35 .
Kidney transplant recipients with CHIKV infection have a similar prognosis and clinical course as the general population. Although transitory graft dysfunction has been previously reported, it is usually mild and reversible 34 , 36 , 37 .
The treatment of renal complications is symptomatic. In more severe cases, intensive care and monitoring of renal function may be imperative 38 .
CUTANEOUS MANIFESTATIONS
The most prevalent skin finding in CHIK infection is morbilliform exanthem, which is usually observed between the third and fifth days of febrile acute illness. It commonly starts in the upper limbs, spares the face, is self-limiting, and associated with mild pruritus. Immune complex deposition in the dermal capillaries is believed to be the pathophysiological mechanism underlying these cutaneous manifestations of CHIK. This type III hypersensitivity reaction may be observed in approximately 40-50% of cases 39 .
Soon after the eruptions resolve, post-inflammatory hypermelanosis may occur, which is particularly common in dark-skinned individuals. Case reports have observed this skin condition in the nose, whereas some refer to this finding as a “CHIK sign.” The outer ear and limbs may also have been affected. Hypermelanosis can present as flagellated, freckle-simile, or discrete macules 40 , 41 .
Exacerbation of preexisting dermatological conditions has also been reported in patients with CHIK. Erythroderma and psoriasis are the most common skin comorbidities that worsen during early febrile illness. Cheilitis, skin and mouth ulcers, crusted lesions, vesiculobullous lesions (frequently observed in children and neonates), skin peeling, xerosis, papules, erythema nodosum, and vasculitis-like lesions have also been reported 42 - 44 . CHIKV may also act as a trigger for vitiligo and other autoimmune diseases 45 , 46 . Figures 2 and 3 show examples of cutaneous manifestations of CHIK.
FIGURE 2: A 2-year-old patient with erythematous papules and plaques on the plantar region. (Photo courtesy of dermatologist Dr. Amanda Dantas).

FIGURE 3: An 8-month-old patient with numerous flaccid blisters, some confluent, located on the lower limbs, with areas of exulceration with hematic crusts on the edges of the lesions. (Photo courtesy of dermatologist Dr. Amanda Dantas).

Nail disorders in CHIK occur as red or black lunulae, periungual ulcers, and/or subungual hemorrhage. Periungual desquamation, and diffuse and longitudinal melanonychia have also described 41 .
Treatment of CHIK skin manifestations commonly relies on antibiotics (e.g., erythromycin) and corticosteroids. Although most skin lesions resolve spontaneously, some heal with significant scarring. Drug choices are inconsistent between studies, and there is limited evidence on the efficacy of these strategies, given the self-limiting character of skin findings 40 - 42 .
OCULAR MANIFESTATIONS
Ocular manifestations of CHIK infection include nonspecific conjunctival conditions, retinitis, and occasional exudative retinal detachment 47 . The most common finding is acute nongranulomatous or granulomatous anterior uveitis; however, cases of intermediate, posterior, and panuveitis have also been observed. Episcleritis, optic neuritis, secondary glaucoma, keratitis, and nerve VI palsy are rarer 47 , 48 . It has not been established whether the ocular manifestations of CHIK are immune-mediated or directly caused by viral infection 49 , 50 .
During the acute phase of the disease, retro-orbital pain and photophobia without visual changes are the most prevalent ocular symptoms. Throughout the illness, patients may report decreased visual acuity, which is a symptom that causes most patients to seek ophthalmological evaluation. Unilateral or bilateral uveitis, ocular hypertension, retinal edema, and retinal hemorrhage may cause decreased visual acuity, and more rarely, inflammatory foveal lesions and macular ischemia 47 , 50 , 51 .
The treatment for uveitis generally involves the use of corticosteroids. A favorable response may require 10-12 weeks. The best response is obtained when the diagnosis is promptly made and treatment is immediately initiated 52 .
GASTROINTESTINAL MANIFESTATIONS
Gastrointestinal symptoms, especially abdominal pain and nausea, have been reported in up to 66% of patients 53 . However, the available data vary depending on the study population. Diarrhea, vomiting, acute pancreatitis, hepatomegaly, and splenomegaly have been observed in a minority of patients in some reports 54 , 55 . Patients with the Asian strain of CHIK seem to present more visceral enlargement than other patients; however, the prevalence of other gastrointestinal symptoms is similar 55 . Hepatitis, which manifests as abnormal asymptomatic levels of liver enzymes, is usually mild 56 . In one study, women experienced more nausea and abdominal pain compared to men 54 .
Conclusive information on gastrointestinal symptoms in CHIK remains unattainable because of the low number of publications on the subject and differences in the populations studied and the prevalent strains. There is no consensus regarding the treatment of the gastrointestinal manifestations of CHIK.
PSYCHIATRIC MANIFESTATIONS
In some patients with neurological involvement, there may be psychiatric symptoms such as confusion, delirium, disorientation, and even psychosis 57 . However, few studies have reported specific psychiatric manifestations of acute CHIK, including mania and depression 58 - 60 . Mania has been reported in a patient with acute CHIK who was previously diagnosed with bipolar disorder, although the patient was stabilized with valproic acid 58 . Another study reported a CHIK-induced manic episode in a patient with no psychiatric history 59 .
Depression in acute CHIK affects up to half of the patients. Younger patients and those with severe arthritis and gastrointestinal symptoms are more likely to self-report depression 60 . 61 .
In acute CHIKV infections, elevated levels of cytokines, including IL-6, are associated with stress susceptibility along with social factors that contribute to post-CHIKV depression. Notably, IL-6, IL-1RA, IL-12, TNF-α, IFN-γ, IL-10, IL-1β, and IL-8/CXCL8 exhibit increased levels in both acute and chronic CHIKV cases, as well as in depression. This suggests the potential of concurrent immunomodulatory interventions targeting these cytokines in comprehensive clinical assessments to mitigate the impact of CHIKV and depressive disorders 62 . 63 .
Manic episodes are treated with antipsychotics such as olanzapine 58 . 59 . The treatment of depression is similar to that used in other settings 60 . 63 . As psychiatric manifestations correlate with pain, analgesics may help treat chronic CHIK infections. Multifactorial and holistic approaches are major elements of optimal care, given that few pharmacological therapies effectively reduce the burden of chronic CHIK 63 .
RESPIRATORY MANIFESTATIONS
Although rare, respiratory manifestations can occur in CHIK patients. CHIKV can infect the lungs and the CHIKV antigen has been isolated from post-mortem biopsies. An intense type I inflammatory response to the virus can lead to acute respiratory distress syndrome (ARDS) 64 . Pulmonary edema and pleural effusion may occur because of endothelial cell dysfunction 65 . Respiratory complications in CHIK patients are strongly associated with higher mortality rates. Pneumonia and respiratory failure are reported as common causes of death in atypical severe CHIK 65 , 66 . Concomitant bacterial infections and pre-existing comorbidities such as emphysema and asthma are believed to increase mortality 66 .
Management of respiratory manifestations is mostly supportive. Noninvasive ventilation may be used successfully in ARDS 67 .
CONCLUSION
Although CHIK infection is usually self-limiting, extra-articular involvement with atypical symptoms may present diagnostic challenges, delay diagnosis, and negatively affect disease outcomes. According to the affected system, the main extra-articular manifestations include encephalitis, myocarditis, acute interstitial nephritis, maculopapular rash, acute anterior uveitis, abdominal pain, and depression. Co-infections, comorbidities, advanced age, pregnancy, and newborns are significant risk factors for unusual and more severe manifestations.
The pathogenesis, clinical features, and management of extra-articular CHIK infections remain unclear. Understanding the pathogenic mechanisms underlying CHIK could also be applicable to other rheumatological and autoimmune diseases, given the role of inflammation and cytokines. An improved understanding of the clinical features of extra-articular manifestations could lead to timely recognition of CHIK, reducing the incidence of its potential complications and long-term sequelae, which represent a high burden to patients. Potential treatments for this neglected tropical disease should be developed and made available in the endemic regions. Such treatments must consider the socioeconomic factors that impact the disease toll. Public health policies in settings where CHIK is prevalent must consider the priorities and values of individuals and their cultural beliefs in order to reduce inequalities, achieve better access to care, and improve the overall quality of life.
Footnotes
Financial Support: None.
REFERENCES
- 1.Suhrbier A. Rheumatic manifestations of chikungunya: emerging concepts and interventions. Nat Rev Rheumatol. 2019;15:597–611. doi: 10.1038/s41584-019-0276-9. [DOI] [PubMed] [Google Scholar]
- 2.Paul BJ, Pannarkady G, Moni SP, Thachil EJ. Clinical profile and long-term sequelae of Chikungunya fever. Indian J Rheumatol. 2011;6(1):12–19. doi: 10.1016/S0973-3698(11)60024-1. [DOI] [Google Scholar]
- 3.Rajapakse S, Rodrigo C, Rajapakse A. Atypical manifestations of chikungunya infection. Trans R Soc Trop Med Hyg. 2010;104(2):89–96. doi: 10.1016/j.trstmh.2009.07.031. [DOI] [PubMed] [Google Scholar]
- 4.Godaert L, Najioullah F, Bartholet S, Colas S, Yactayo S, Cabié A, et al. Atypical Clinical Presentations of Acute Phase Chikungunya Virus Infection in Older Adults. J Am Geriatr Soc. 2017;65(11):2510–2515. doi: 10.1111/jgs.15004. [DOI] [PubMed] [Google Scholar]
- 5.Deeba IM, Hasan MM, Al Mosabbir A, Siam MHB, Islam MS, Raheem E, et al. Manifestations of Atypical Symptoms of Chikungunya during the Dhaka Outbreak (2017) in Bangladesh. Am J Trop Med Hyg. 2019;100(6):1545–1548. doi: 10.4269/ajtmh.19-0122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beserra FLCN, Oliveira GM, Marques TMA, Farias LABG, Santos JRD, Daher EF, et al. Clinical and laboratory profiles of children with severe chikungunya infection. Rev Soc Bras Med Trop. 2019;52:e20180232. doi: 10.1590/0037-8682-0232-2018. [DOI] [PubMed] [Google Scholar]
- 7.Tandale BV, Sathe PS, Arankalle VA, Wadia RS, Kulkarni R, Shah SV, et al. Systemic involvements and fatalities during Chikungunya epidemic in India, 2006. J Clin Virol. 2009;46(2):145–149. doi: 10.1016/j.jcv.2009.06.027. [DOI] [PubMed] [Google Scholar]
- 8.Arpino C, Curatolo P, Rezza G. Chikungunya and the nervous system: what we do and do not know. Rev Med Virol. 2009;19(3):121–129. doi: 10.1002/rmv.606. [DOI] [PubMed] [Google Scholar]
- 9.Wei Chiam C, Fun Chan Y, Chai Ong K, Thong Wong K, Sam IC. Neurovirulence comparison of chikungunya virus isolates of the Asian and East/Central/South African genotypes from Malaysia. J Gen Virol. 2015;96(11):3243–3254. doi: 10.1099/jgv.0.000263. [DOI] [PubMed] [Google Scholar]
- 10.Mehta R, Gerardin P, de Brito CAA, Soares CN, Ferreira MLB, Solomon T. The neurological complications of chikungunya virus: A systematic review. Rev Med Virol. 2018;28(3):e1978. doi: 10.1002/rmv.1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Singh A, Jain R. Neurological Manifestations of Chikungunya in Children. Indian Pediatr. 2017;54(3):249–249. doi: 10.1007/s13312-017-1040-3. [DOI] [PubMed] [Google Scholar]
- 12.Brito Ferreira ML, Militão de Albuquerque MFP, de Brito CAA, de Oliveira França RF, Porto Moreira ÁJ, de Morais Machado MÍ, et al. Neurological disease in adults with Zika and chikungunya virus infection in Northeast Brazil: a prospective observational study. Lancet Neurol. 2020;19(10):826–839. doi: 10.1016/S1474-4422(20)30232-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Farias LABG, Ferragut JM, Pires RDJ., Neto Encephalitis and transverse myelitis in dengue and chikungunya coinfection. Rev Soc Bras Med Trop. 2018;51(3):403–403. doi: 10.1590/0037-8682-0259-2017. [DOI] [PubMed] [Google Scholar]
- 14.Pinheiro TJ, Guimarães LF, Silva MT, Soares CN. Neurological manifestations of Chikungunya and Zika infections. Arq Neuropsiquiatr. 2016;74(11):937–943. doi: 10.1590/0004-282X20160138. [DOI] [PubMed] [Google Scholar]
- 15.Ward CE, Chapman JI. Chikungunya in Children: A Clinical Review. Pediatr Emerg Care. 2018;34(7):510–515. doi: 10.1097/PEC.0000000000001529. [DOI] [PubMed] [Google Scholar]
- 16.Cerny T, Schwarz M, Schwarz U, Lemant J, Gérardin P, Keller E. The Range of Neurological Complications in Chikungunya Fever. Neurocrit Care. 2017;27(3):447–457. doi: 10.1007/s12028-017-0413-8. [DOI] [PubMed] [Google Scholar]
- 17.Cotella JI, Sauce AL, Saldarriaga CI, Perez GE, Farina JM, Wyss F, et al. Chikungunya and the Heart. Cardiology. 2021;146(3):324–334. doi: 10.1159/000514206. [DOI] [PubMed] [Google Scholar]
- 18.Langsjoen RM, Zhou Y, Holcomb RJ, Routh AL. Chikungunya Virus Infects the Heart and Induces Heart-Specific Transcriptional Changes in an Immunodeficient Mouse Model of Infection. Am J Trop Med Hyg. 2021;106(1):99–104. doi: 10.4269/ajtmh.21-0719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Obeyesekere I, Hermon Y. Arbovirus heart disease: myocarditis and cardiomyopathy following dengue and chikungunya fever--a follow-up study. Am Heart J. 1973;85(2):186–194. doi: 10.1016/0002-8703(73)90459-6. [DOI] [PubMed] [Google Scholar]
- 20.Alvarez MF, Bolívar-Mejía A, Rodriguez-Morales AJ, Ramirez-Vallejo E. Cardiovascular involvement and manifestations of systemic Chikungunya virus infection: A systematic review. F1000Res. 2017;6:390–390. doi: 10.12688/f1000research.11078.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Farias LABG, Beserra FLCN, Fernandes L, Teixeira AAR, Ferragut JM, Girão ES, et al. Myocarditis Following Recent Chikungunya and Dengue Virus Coinfection: A Case Report. Arq Bras Cardiol. 2019;113(4):783–786. doi: 10.5935/abc.20190187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shah AB, Parmar YJ, Mangla A, Lasic Z, Coplan N. Dengue fever as a cause of perimyocarditis and low-pressure cardiac tamponade. Proc (Bayl Univ Med Cent) 2018;31(4):487–489. doi: 10.1080/08998280.2018.1482519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Simon F, Paule P, Oliver M. Chikungunya virus-induced myopericarditis: toward an increase of dilated cardiomyopathy in countries with epidemics? Am J Trop Med Hyg. 2008;78(2):212–213. [PubMed] [Google Scholar]
- 24.Traverse EM, Hopkins HK, Vaidhyanathan V, Barr KL. Cardiomyopathy and Death Following Chikungunya Infection: An Increasingly Common Outcome. Trop Med Infect Dis. 2021;6(3):108–108. doi: 10.3390/tropicalmed6030108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wiwanitkit V. Dengue myocarditis, rare but not fatal manifestation. Int J Cardiol. 2006;112(1):122–122. doi: 10.1016/j.ijcard.2005.09.027. [DOI] [PubMed] [Google Scholar]
- 26.Scatularo CE, Ballesteros OA, Saldarriaga C, Mendoza I, Wyss F, Liprandi AS, et al. Zika & heart: A systematic review. Trends Cardiovasc Med. 2022;32(1):52–58. doi: 10.1016/j.tcm.2020.11.003. [DOI] [PubMed] [Google Scholar]
- 27.Anwar S, Taslem Mourosi J, Khan MF, Ullah MO, Vanakker OM, Hosen MJ. Chikungunya outbreak in Bangladesh (2017): Clinical and hematological findings. PLoS Negl Trop Dis. 2020;14(2):e0007466. doi: 10.1371/journal.pntd.0007466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Borgherini G, Poubeau P, Staikowsky F, Lory M, Le Moullec N, Becquart JP, et al. Outbreak of chikungunya on Reunion Island: early clinical and laboratory features in 157 adult patients. Clin Infect Dis. 2007;44(11):1401–1407. doi: 10.1086/517537. [DOI] [PubMed] [Google Scholar]
- 29.Lee VJ, Chow A, Zheng X, Carrasco LR, Cook AR, Lye DC, et al. Simple clinical and laboratory predictors of Chikungunya versus dengue infections in adults. PLoS Negl Trop Dis. 2012;6(9):e1786. doi: 10.1371/journal.pntd.0001786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ramacciotti E, Agati LB, Aguiar VCR, Wolosker N, Guerra JC, de Almeida RP, et al. Zika and Chikungunya Virus and Risk for Venous Thromboembolism. Clin Appl Thromb Hemost. 2019;25:1076029618821184–1076029618821184. doi: 10.1177/1076029618821184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Costa DMDN, Gouveia PADC, Silva GEB, Neves PDMM, Vajgel G, Cavalcante MAGM, et al. The relationship between chikungunya virus and the kidneys: A scoping review. Rev Med Virol. 2023;33(1):e2357. doi: 10.1002/rmv.2357. [DOI] [PubMed] [Google Scholar]
- 32.do Nascimento Costa DM, Machado CE, Neves PD, Brito DJ, Oi S, Barros FH, et al. Chikungunya virus as a trigger for different renal disorders: an exploratory study. J Nephrol. 2022;35(5):1437–1447. doi: 10.1007/s40620-022-01256-6. [DOI] [PubMed] [Google Scholar]
- 33.Mercado M, Acosta-Reyes J, Parra E, Guzmán L, Beltrán M, Gasque P, et al. Renal involvement in fatal cases of chikungunya virus infection. J Clin Virol. 2018;103:16–18. doi: 10.1016/j.jcv.2018.03.009. [DOI] [PubMed] [Google Scholar]
- 34.Aurore AC, Couderc T, Dueymes JM, Deligny C, Lecuit M, Molinié V, et al. The Clinicopathological Spectrum of Kidney Lesions in Chikungunya Fever: A Report of 5 Cases With Kidney Biopsy. Am J Kidney Dis. 2021;78(6):902–906. doi: 10.1053/j.ajkd.2021.04.012. [DOI] [PubMed] [Google Scholar]
- 35.da Justa Pires R, Neto, Bezerra G., da Silva Junior . In: Tropical Nephrology. 1st ed. Bezerra G da Silva Junior, De Francesco Daher E, Barros E, editors. Springer International Publishing; 2020. Renal Involvement in Patients with Arbovirus Infections; pp. 91–103. [Google Scholar]
- 36.Tavares BM, Fernandes PF, Oliveira CMC, Silva SL, Mota MU, Andrade TH, et al. Chikungunya on Kidney Transplant Recipients: Is It the Same? Transplantation. 2019;103(2):441–445. doi: 10.1097/TP.0000000000002363. [DOI] [PubMed] [Google Scholar]
- 37.Pierrotti LC, Lopes MIBF, Nascimento APD, Caiaffa-Filho H, Lemos FBC, Reusing JO, Jr, et al. Chikungunya in kidney transplant recipients: A series of cases. Int J Infect Dis. 2017;64:96–99. doi: 10.4269/ajtmh.19-0926. [DOI] [PubMed] [Google Scholar]
- 38.Gupta A, Juneja D, Singh O, Garg SK, Arora V, Deepak D. Clinical Profile, Intensive Care Unit Course, and Outcome of Patients Admitted in Intensive Care Unit with Chikungunya. Indian J Crit Care Med. 2018;22(1):5–9. doi: 10.4103/ijccm.IJCCM_336_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Benjamanukul S, Chansaenroj J, Chirathaworn C, Poovorawan Y. Atypical skin manifestation in severe acute chikungunya infection in a pregnant woman: a case report. J Med Case Rep. 2022;16(1):5–5. doi: 10.1186/s13256-021-03197-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bothra A, Maheswari A, Singh M, Pawar M, Jodhani K. Cutaneous manifestations of viral outbreaks. Australas J Dermatol. 2021;62(1):27–36. doi: 10.1111/ajd.13421. [DOI] [PubMed] [Google Scholar]
- 41.Kumar R, Sharma MK, Jain SK, Yadav SK, Singhal AK. Cutaneous Manifestations of Chikungunya Fever: Observations from an Outbreak at a Tertiary Care Hospital in Southeast Rajasthan, India. Indian Dermatol Online J. 2017;8(5):336–342. doi: 10.4103/idoj.IDOJ_429_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kaleem S, Ghafoor R, Khan S. Mucocutaneous manifestations of Chikungunya fever, an experience of tertiary care hospital. J Pak Med Assoc. 2021;71(2(B)):619–623. doi: 10.47391/JPMA.693. [DOI] [PubMed] [Google Scholar]
- 43.Robin S, Ramful D, Zettor J, Benhamou L, Jaffar-Bandjee MC, Rivière JP, et al. Severe bullous skin lesions associated with Chikungunya virus infection in small infants. Eur J Pediatr. 2010;169(1):67–72. doi: 10.1007/s00431-009-0986-0. [DOI] [PubMed] [Google Scholar]
- 44.Farias LABG, Pires RDJ, Neto, Leite RD. Extensive vesiculobullous exanthema following chikungunya fever in a 13-year-old patient. Rev Soc Bras Med Trop. 2019 Jun 27;52:e20190015. doi: 10.1590/0037-8682-0015-2019. [DOI] [PubMed] [Google Scholar]
- 45.Farias LABG, Bezerra KRF, Albuquerque MMS, Pires RDJ, Neto, Accioly JW., Filho Association between vitiligo lesions and acute chikungunya infection: is there a causal relationship? Rev Soc Bras Med Trop. 2019;52:e20190238. doi: 10.1590/0037-8682-0238-2019. [DOI] [PubMed] [Google Scholar]
- 46.Tanay A. Chikungunya virus and autoimmunity. Curr Opin Rheumatol. 2017;29(4):389–393. doi: 10.1097/BOR.0000000000000396. [DOI] [PubMed] [Google Scholar]
- 47.Esporcatte LPG, Portes AJF. Ocular manifestations of Chikungunya fever in the chronic phase. Arq Bras Oftalmol. 2021;84(6):549–553. doi: 10.5935/0004-2749.20210081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mahendradas P, Ranganna SK, Shetty R, Balu R, Narayana KM, Babu RB, et al. Ocular manifestations associated with chikungunya. Ophthalmology. 2008;115(2):287–291. doi: 10.1016/j.ophtha.2007.03.085. [DOI] [PubMed] [Google Scholar]
- 49.Mittal A, Mittal S, Bharati MJ, Ramakrishnan R, Saravanan S, Sathe PS. Optic neuritis associated with chikungunya virus infection in South India. Arch Ophthalmol. 2007;125(10):1381–1386. doi: 10.1001/archopht.125.10.1381. [DOI] [PubMed] [Google Scholar]
- 50.Mahendradas P, Avadhani K, Shetty R. Chikungunya and the eye: a review. J Ophthalmic Inflamm Infect. 2013;3(1):35–35. doi: 10.1186/1869-5760-3-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mahesh G, Giridhar A, Shedbele A, Kumar R, Saikumar SJ. A case of bilateral presumed chikungunya neuroretinitis. Indian J Ophthalmol. 2009;57(2):148–150. doi: 10.4103/0301-4738.45508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Oliver GF, Carr JM, Smith JR. Emerging infectious uveitis: Chikungunya, dengue, Zika and Ebola: A review. Clin Exp Ophthalmol. 2019;47(3):372–380. doi: 10.1111/ceo.13450. [DOI] [PubMed] [Google Scholar]
- 53.Pathak S, Chaudhary N, Dhakal P, Yadav SR, Gupta BK, Kurmi OP. Comparative Study of Chikungunya Only and Chikungunya-Scrub Typhus Coinfection in Children: Findings from a Hospital-Based Observational Study from Central Nepal. Int J Pediatr. 2021;2021:6613564–6613564. doi: 10.1155/2021/6613564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Monteiro JD, Valverde JG, Morais IC, Souza CRM, Fagundes JC, Neto, Melo MF, et al. Epidemiologic and clinical investigations during a chikungunya outbreak in Rio Grande do Norte State, Brazil. PLoS One. 2020;15(11):e0241799. doi: 10.1371/journal.pone.0241799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bonifay T, Prince C, Neyra C, Demar M, Rousset D, Kallel H, et al. Atypical and severe manifestations of chikungunya virus infection in French Guiana: A hospital-based study. PLoS One. 2018;13(12):e0207406. doi: 10.1371/journal.pone.0207406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Srikirin P, Siripoon T, Charoenpong L, Soonthornworasiri N, Matsee W, Kittitrakul C, et al. Prevalence, Risk Factors, and Prognosis of Liver Involvement in Adult Patients with Chikungunya in Thailand. Am J Trop Med Hyg. 2022;107(5):1107–1113. doi: 10.4269/ajtmh.22-0339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rampal Sharda M, Meena H. Neurological complications in Chikungunya fever. J Assoc Physicians India. 2007;55:765–769. [PubMed] [Google Scholar]
- 58.Figueiredo T, Dias da Costa M, Segenreich D. Manic Episode After a Chikungunya Virus Infection in a Bipolar Patient Previously Stabilized With Valproic Acid. J Clin Psychopharmacol. 2018;38(4):395–397. doi: 10.1097/JCP.0000000000000887. [DOI] [PubMed] [Google Scholar]
- 59.Soares DS, Fortaleza LY, Melo MC. Chikungunya-induced manic episode in a patient with no psychiatric history: a case report. Braz J Psychiatry. 2020;42(6):687–687. doi: 10.1590/1516-4446-2020-0892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Murillo-Zamora E, Mendoza-Cano O, Trujillo-Hernández B, Trujillo X, Huerta M, Guzmán-Esquivel J, et al. Screening for Depressive Mood During Acute Chikungunya Infection in Primary Healthcare Settings. Int J Environ Res Public Health. 2018;15(11):2552–2552. doi: 10.3390/ijerph15112552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ninla-Aesong P, Mitarnun W, Noipha K. Long-Term Persistence of Chikungunya Virus-Associated Manifestations and Anti-Chikungunya Virus Antibody in Southern Thailand: 5 Years After an Outbreak in 2008-2009. Viral Immunol. 2020;33(2):86–93. doi: 10.1089/vim.2019.0168. [DOI] [PubMed] [Google Scholar]
- 62.Rodriguez-Morales AJ, Hoyos-Guapacha KL, Vargas-Zapata SL, Meneses-Quintero OM, Gutiérrez-Segura JC. Would be IL-6 a missing link between chronic inflammatory rheumatism and depression after chikungunya infection? Rheumatol Int. 2017;37(7):1149–1151. doi: 10.1007/s00296-017-3747-9. [DOI] [PubMed] [Google Scholar]
- 63.Rodríguez-Morales AJ, Hernández-Moncada ÁM, Hoyos-Guapacha KL, et al. Potential relationships between chikungunya and depression: Solving the puzzle with key cytokines. Cytokine. 2018;102:161–162. doi: 10.1016/j.cyto.2017.08.011. [DOI] [PubMed] [Google Scholar]
- 64.Traverse EM, Millsapps EM, Underwood EC, Hopkins HK, Young M, Barr KL. Chikungunya Immunopathology as It Presents in Different Organ Systems. Viruses. 2022;14(8):1786–1786. doi: 10.3390/v14081786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sharp TM, Keating MK, Shieh WJ, Bhatnagar J, Bollweg BC, Levine R, et al. Clinical Characteristics, Histopathology, and Tissue Immunolocalization of Chikungunya Virus Antigen in Fatal Cases. Clin Infect Dis. 2021;73(2):e345-e354. doi: 10.1093/cid/ciaa837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Freitas ARR, Donalisio MR, Alarcón-Elbal PM. Excess Mortality and Causes Associated with Chikungunya, Puerto Rico, 2014-2015. Emerg Infect Dis. 2018;24(12):2352–2355. doi: 10.3201/eid2412.170639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Singh A. Acute Respiratory Distress Syndrome: An Unusual Presentation of Chikungunya Fever Viral Infection. J Glob Infect Dis. 2017;9(1):33–34. doi: 10.4103/0974-777X.194374. [DOI] [PMC free article] [PubMed] [Google Scholar]


