Abstract
Objective To determine whether taking steam baths was associated with furunculosis and to evaluate possible risk factors for the occurrence of boils during a large outbreak in Alaska. Design A cohort study of village residents, a case-control study, and assessment of environmental cultures taken from steam baths. Setting Village in southwestern Alaska. Participants 1 adult member from 77 of the 92 house-holds in the village was interviewed; 115 residents with at least one boil occurring between January 1 and December 12, 1996 were considered to be cases; 209 residents without a boil acted as the control group. All 459 village residents were included in the cohort study. Main outcome measure Rate of infection among all residents and residents who regularly took steam baths, risk factors for infection, and relative risk of infection. Results 115 people (25%) had had at least one boil. Men were more likely to have had a boil than women (relative risk 1.5; 95% confidence interval 1.1 to 2.2). The highest rate of infection was among people ages 25-34 years (32/76; 42%). No children younger than 2 years had had boils. Boils were associated with using a steam bath (odds ratio 8.1; 3.3 to 20.1). Among those who used a steam bath, the likelihood of developing boils was reduced by routinely sitting on a towel while bathing, which women were more likely to do, and bathing with fewer than 8 people. Of the 93 samples taken from steam baths, one Staphylococcus aureus isolate was obtained from a bench in an outer dressing room. Conclusion Using a steam bath was associated with developing boils in this outbreak in a village in Alaska. People should be advised to sit on towels while using steam baths.
INTRODUCTION
Furunculosis was described in some of the earliest historical accounts of Alaska. Boils were the most prevalent illness among Kodiak Islanders at the beginning of the 18th century.1 During his travels among the natives of the lower Yukon during 1842-1844, Zagoskin ranked abscesses as one of the most commonly occurring conditions.1 More recently, in 1984 an epidemic of staphylococcal disease was described among residents of another village.2,3 Elsewhere, furunculosis and cellulitis have been associated with skin abrasions and bruises among river guides4 and a football team5; an association with local skin injury was not apparent in the 1984 outbreak in a village in Alaska.2
In December 1996, the Alaska Division of Public Health investigated a large outbreak of furunculosis in a village. Healthcare providers were concerned that transmission might be occurring through the residents' use of the 22 steam baths in the community. We sought to determine if transmission was occurring through the use of steam baths and to evaluate possible risk factors associated with the occurrence of boils.
Summary points
In December 1996 the Alaska Division of Public Health investigated a large outbreak of furunculosis
Healthcare providers in the village were concerned that transmission was occurring during the use of the 22 steam baths in the community
Sharing a steam bath with more than 8 people, sharing soap, and being male increased the risk of developing a boil
Those who use steam baths should sit on a towel while bathing to reduce the likelihood of developing boils
Background
The Alaska Native village where the 1996 outbreak occurred is situated on a river in southwestern Alaska. It consists of an area with largely older homes (region 1), a mixed area with both new and older homes (region 2), and an area with only new homes (region 3). Although some homes in region 1 and many homes in regions 2 and 3 have showers, most people bathe at one of the 22 stream baths located in residents' backyards. A typical steam bath consists of an outer dressing room and an inner steam room with benches and a woodburning stove. In general, men and women take steam baths separately. There is one clinic in the village; hospitals and additional clinics are accessible by plane.
In late October 1996, the physician who provided care for the village reported to the Division of Public Health that there had been 80 visits to the clinic for boils during 1996 and that Staphylococcus aureus had been isolated from purulent material from several patients. Six isolates of S aureus were then submitted to the Centers for Disease Control and Prevention for further identification by pulse-field gel electrophoresis, and all had a similar pattern. In early September 1996, healthcare providers in the village distributed fliers urging owners of steam baths to clean their baths with bleach. In addition, people were asked to sit on a towel while bathing and to consider using their own washbasins. (Washbasins are used to pour cool water over the bather while in the steam bath.)
PARTICIPANTS AND METHODS
Identification of population and bathing practices
For the purposes of the study, boils were defined as tender, erythematous, fluctuant skin lesions occurring between January 1 and December 12, 1996. People who had had one or more boils were identified by a review of charts at the village clinic and by interviews during the door to door survey. Clinic personnel provided a list of all current village residents by household. The sex and date of birth of the resident, the region in which they lived, and whether the household had a steam bath were indicated. The rate and the relative risks of infection were determined by the cohort study.
A structured interview with an adult member of each household was attempted at every house in the village during the survey. Two researchers conducted all of the interviews (MGL and BJM). Information was obtained from respondents about their practices while steam bathing and about the practices of all other household members. Respondents provided information about whether they routinely sat on a towel while having a steam bath, whether they routinely had a bath with fewer than 8 people, whether they routinely used their own soap in the steam bath, and whether they bathed daily or less frequently. For the case-control study, a case was defined as a person with a boil. The control group comprised village residents who had not had a boil and who had been interviewed or whose family member had been interviewed about their use of steam baths.
Data analysis
Multivariate analyses using logistic regression were completed for the case-control study using the demographic and general variables and the information on practices while steam bathing. Demographic and general variables analyzed included age, sex, race, whether another household member had had a boil in 1996, whether the person used a steam bath, whether the household had a washing machine, whether clothes were washed with hot water or bleach, whether there was a shower in the house, and the region of residence. Each final model consisted only of those variables that contributed significantly at the P ≤ 0.05 level.
Collection of samples
Environmental cultures were obtained from 9 of the 22 steam baths; six steam baths were cultured before and after use in the evening, and three steam baths were cultured only after use. Surfaces cultured included the bench and wall of the outer dressing rooms and the bench, wall, and floor of the inner steam room. Soap and washbasins were also cultured. All isolates of S aureus from cultures of purulent material from boils were also analyzed. Pulsefield gel electrophoresis testing was completed at the Centers for Disease Control and Prevention on the S aureus isolates obtained.
RESULTS
Interviews were completed at 77 (84%) of 92 households, accounting for 396 (86%) of 459 village residents. Information on whether the participant used a steam bath was available for 320 (81%) of the 396 residents. Demographic and general variables were available for all 320 residents who had provided information about their use of steam baths and an additional four people who had visited the clinic with a boil. Data on practices while bathing were available for the 242 (76%) residents who had taken steam baths.
Incidence
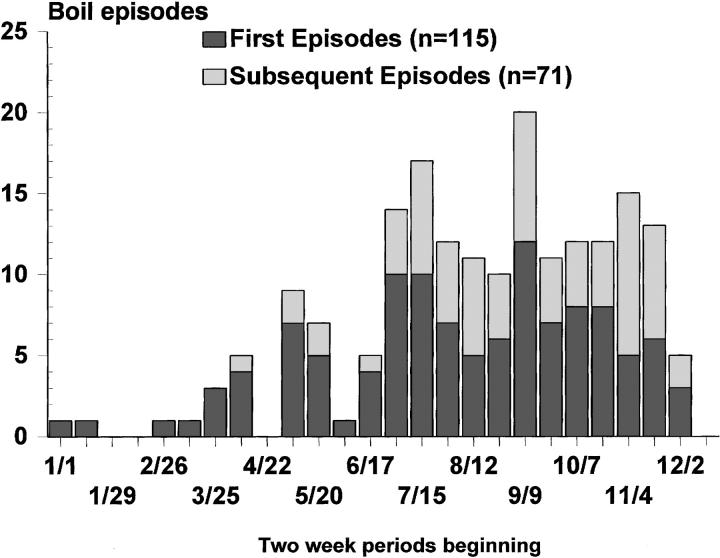
Of the 459 village residents, 115 (25%) had had at least one boil during the period studied; 105 were identified during chart review and 10 others by interview. The outbreak peaked in September (figure). A total of 186 boils were reported. Boils ranged in size from 0.5 cm to 12 cm with a mean of 3.4 cm. Two people had been hospitalized with cellulitis. During 1995, five people (1%) had visited the clinic because they had a boil. During 1996, 74 (30%) of 248 men in the village had had a boil compared with 41 (19%) of 211 women in the village (relative risk 1.5; 95% confidence interval 1.1 to 2.2). Similarly, 26 (37%) of 71 male heads of household had boils compared with 2 (10%) of 21 female heads of household (relative risk 3.9; 1.0 to 14.9). The highest rate of infection was among people aged 25-34 years (32/76; 42%); the lowest was among children 4 years of age and older (8/69; 12%) (table 1). There were no boils among the 23 children who were younger than 2 years. Only one child younger than 2 was known to have had a steam bath. Only one person stated that the boil had occurred after local injury to the skin at the same site.
Figure 1.
Number of people diagnosed with first and subsequent infections with boils during two-week intervals, January 1 through December 12, 1996
Table 1.
Rate of infection by age group during an outbreak of furunculosis among residents in a village in southwestern Alaska, 1996
| Age (years) | Number of people | Number of people with boils | Rate of infection (%) | Relative risk (95% CI) |
|---|---|---|---|---|
| ≤4 | 69 | 8 | 12 | 1.0 |
| 5-14 | 118 | 32 | 27 | 2.3 (1.1 to 4.8) |
| 15-24 | 65 | 12 | 18 | 1.6 (0.7 to 3.6) |
| 25-34 | 76 | 32 | 42 | 3.6 (1.8 to 7.3) |
| 35-44 | 54 | 8 | 15 | 1.3 (0.5 to 3.2) |
| 45-54 | 39 | 11 | 28 | 2.4 (1.1 to 5.5) |
| 55-64 | 22 | 9 | 41 | 3.5 (1.6 to 8.0) |
| ≥65 | 16 | 3 | 19 | 1.6 (0.5 to 5.4) |
| Total | 459 | 115 | 25 |
The incidence of boils in different regions of the village varied from 30% (31/102) in region 1 to 21% (25/120) in region 2, and 25% (59/237) in region 3. The relative risk of having a boil among those living in region 1 compared with those living in other regions was 1.3 (0.9 to 1.8). The number of steam baths also varied by region with 6 (5.9/100 people) in region 1, 4 (3.3/100 people) in region 2, and 12 (5.1/100 people) in region 3. Rates of infection did not vary according to the presence of a household steam bath (relative risk 1.0; 0.7 to 1.5).
The case-control study compared 115 residents with boils with 209 residents without boils and showed that having one or more boils was associated with taking steam baths (odds ratio 5.7; 95% confidence interval 2.4 to 14.4), having another household member with a boil (3.5; 2.0 to 6.4), and being male (1.9; 1.2 to 3.2). Seven people who had never used the steam baths had had a boil. Being a case was not significantly associated with washing clothes with hot water (odds ratio 0.9; 0.5 to 1.5), washing clothes with bleach (0.6; 0.3 to 1.2), having a washing machine (0.7; 0.4 to 1.1), or the presence of a shower in the house (0.7; 0.4 to 1.2).
Among those who used steam baths, those who routinely bathed with fewer than 8 people were less likely to have a boil than those who bathed with more than 8 people (odds ratio 0.3; 0.1 to 0.6). Having a steam bath less often than once a day protected people against getting boils (odds ratio 0.5; 0.3 to 1.0). Using personal soap instead of sharing soap also protected people (0.3; 0.1 to 0.6) as did routinely sitting on a towel on the bench in the steam bath (0.3; 0.2 to 0.6). Women were more likely than men to sit on a towel (76/91 (84%) vs 28/96 (29%); P < 0.0001) and use personal soap (39/91 (43%) vs 19/96 (20%); P = 0.001). Showering less than twice a week did not significantly increase the likelihood of developing a boil (1.8; 0.5 to 6.1) among those who used steam baths. Boils were significantly associated with using two particular steam baths in the village (P < 0.05) and one at a fishing camp outside of the village (P < 0.05). Those who used another particular steam bath were protected against getting boils.
Sites of boils
Boils were most commonly found on the buttocks and posterior thigh (81/186; 44%), abdomen (25/186; 13%), and arms (18/186; 10%). Sixty-two of the 115 (54%) people with boils had a boil on their buttocks or posterior thigh. Of the seven people who had boils but did not use the steam baths, only one (14%) had a boil on the buttocks or posterior thigh. Having a boil on the buttocks or posterior thigh was associated with steam bathing (odds ratio 19.5; 3.2 to 796.9), with not routinely sitting on a towel (4.0; 1.9 to 8.8), and with having another member of the family with a boil (2.0; 1.0 to 3.9).
Multivariate analysis
Multivariate analysis of demographic and general variables resulted in a model that included four variables (table 2). Taking steam baths remained strongly associated with having a boil (odds ratio 8.1; 3.3 to 20.1). In a multivariate analysis of steam bathing practices, routinely sitting on a towel and bathing with fewer than 8 people remained the only significant factors that protected people against developing boils (table 3). In the univariate analysis, bathers who used their own soap were protected against developing boils (table 3).
Table 2.
Demographic and general variables identified by logistic regression as being most strongly associated with developing boils among 324 residents of a village in southwestern Alaska, 1996
| Variable | Odds ratio (95% CI) |
|---|---|
| Uses a village steam bath | 8.1 (3.3 to 20.1) |
| Other household member has a boil | 4.6 (2.4 to 8.9) |
| Male sex | 2.3 (1.3 to 3.9) |
| Household doesn't wash clothes with bleach | 1.5 (0.8 to 2.9) |
Table 3.
Steam bathing practices of 242 village residents*
| Practice | Odds ratio (95% CI) |
|---|---|
| Usually sits on towel while steam bathing | 0.3 (0.1 to 0.8) |
| Uses own soap while steam bathing | 0.4 (0.2 to 1.1) |
| Usually steam bathes with <8 people | 0.3 (0.2 to 0.8) |
Identified by logistic regression as being most significant in protecting people against developing boils, southwestern Alaska, 1996.
Gel electrophoresis
Pulse-field gel electrophoresis was completed on 18 S aureus isolates obtained from boils. Fourteen isolates (78%) had the same pattern; the other four each had a different pattern. The one S aureus isolate from the 93 cultures taken from the steam baths was obtained from a bench in the outer dressing room; it had the same pattern on gel electrophoresis as one of the four isolates without the majority pattern from the boils. Resistance to methicillin was found among all six isolates from boils tested for antibiotic sensitivity in December 1996; further testing was unnecessary once resistance was identified.
DISCUSSION
Boils resulting from infection with S aureus were associated with the use of steam baths in this village in Alaska. Controlling the outbreak was problematic. Health education notices, which recommended cleaning steam baths regularly and sitting on towels while bathing, were posted during the peak and subsequent decline in the number of cases (September-December 1996). However, people continued to develop boils during the spring of 1997. Temporarily closing the steam baths was not an option since use of the steam baths is a social activity and a means of bathing. The residents rejected the idea of placing portable showers at the steam baths to be used before and after bathing. Instead, healthcare providers tried to provide additional health education messages through their distribution of fliers. People with boils were asked not to use steam baths. Residents were asked to sit on towels in the steam baths, to use their own soap, and to wash their hands before and after each bath. Those who owned the steam baths were asked to clean them with a dilute solution of chlorine bleach. Healthcare providers were asked to avoid using antibiotics unless severe cellulitis or systemic infection was present and to treat the boils with incision and drainage instead.
In the outbreaks of furunculosis that occurred among river guides4 and a football team,5 the boils were most commonly located on the extremities and were associated with injury to the skin. In the 1984 outbreak in another village in Alaska2 and in the outbreak in this village, the boils were most commonly located on the buttocks and posterior thighs and were rarely associated with local skin injury. During the 1984 outbreak it was suspected that a recently opened public sauna might have facilitated transmission; however, an association was not established.2 Among the river guides, no new cases were reported after the use of hexachlorophene to scrub the skin became routine, surveillance for cases was improved, prompt medical treatment was provided, and those with boils were isolated. In the 1984 outbreak, the rate of infection among residents remained above 25% 1 year later despite a health education program emphasizing the need for prompt medical treatment and improved personal hygiene.2
In outbreaks of infections with methicillin-resistant S aureus in hospitals, mupirocin and isolation have been used successfully to eliminate nasal carriage and establish control.6 Neither treatment with mupirocin nor isolation was believed to be an option in this outbreak, since some residents with boils continued to use a steam bath although they had received consistent and repeated health education messages not to do so.
Large outbreaks of furunculosis in villages in Alaska have probably occurred periodically. The outbreak described here was associated with steam bathing and steam bathing likely contributed to the 1984 village outbreak. Ideally, protective practices, including sitting on a towel on the steam bench, should be encouraged so that outbreaks may be reduced in size and frequency. When an outbreak occurs, medical treatment should be limited to incision and drainage and local wound care. The use of antibiotics should be restricted only to those patients who have severe cellulitis or systemic illness.
Acknowledgments
Annie Chocknok and Richard Ascher assisted us in investigating the outbreak by helping to decide which strategies would be most effective; Gary Hancock performed the pulse-field gel electrophoresis testing; Michael Beller and Ronald L Moolenaar constructively reviewed the manuscript; and Elizabeth Funk offered valuable general advice.
Funding: None
Competing interests: None declared
References
- 1.Fortuine R. Chills and fever. Fairbanks: University of Alaska Press, 1989.
- 2.Cartter M. Hyperendemic furunculosis in residents of an Alaskan Eskimo village. Paper presented at: the Epidemic Intelligence Service. Regional Conference; March 15, 1985; Ann Arbor.
- 3.DeParle J. Lacking plumbing villages in Alaska face health crisis. New York Times Nov 28, 1992: A1.
- 4.Centers for Disease Control and Prevention. Staphylococcal infections among river guides - Tennessee, South Carolina, and North Carolina. MMWR Morb Mortal Wkly Rep 1982;31: 605-607. [PubMed] [Google Scholar]
- 5.Bartlett PC, Martin RJ, Cahill BR. Furunculosis in a high school football team. Am J Sports Med 1982;10: 371-374. [DOI] [PubMed] [Google Scholar]
- 6.Hill RLR, Duckworth GJ, Casewell MW. Elimination of nasal carriage of methicillin-resistant Staphylococcus aureus with mupirocin during a hospital outbreak. J Antimicrob Chemother 1988;22: 377-384. [DOI] [PubMed] [Google Scholar]