STRUCTURED ABSTRACT:
Background:
With increasing complexity of our aging inpatient population, we implemented an interprofessional geriatric and palliative care intervention on a hospitalist service. This study aimed to measure the intervention’s impact on length of stay (LOS), 30-day readmission, and the daily intensity of inpatient services utilization.
Methods:
Using a non-randomized controlled intervention at a 1,000-bed U.S. academic quaternary medical center, we studied 13,941 individuals admitted to a general medicine hospitalist service (of which 5,644 were age >=65 years);1,483 were on intervention teams (576 age >=65 years), 5,413 concurrent controls, and 7,045 historical controls. On 2 of 11 hospitalist teams, a geriatrician, palliative care physician and social worker attended multidisciplinary discharge rounds twice weekly, to recommend inpatient geriatric or palliative care consult (GPCC), post-acute nursing or home care, versus post-discharge outpatient consultation. We measured the difference in improvement over time between intervention and control team patients for the following: (1) LOS adjusted for case-mix index, (2) 30-day readmissions, and (3) intensity of hospital service utilization (mean services provided per patient per day).
Results:
Adjusted LOS (in hospital days) was decreased by 0.36 days (p=0.039) for the 1483 patients in the intervention teams, with greater LOS reduction of 0.55 days per admission (p=0.022) on average among the subset of 576 older patient admissions. Readmissions were unchanged (−1.17%, p=.48 for all patients; 1.91%, p = .46 for older patients). However, the daily Relative Value Unit (RVU) utilization was modestly increased for both the overall and older subgroup, 0.35 RVUs (p=0.041) and 0.74 RVUs (p<0.001) per patient-day on average across the intervention teams, respectively.
Conclusion:
An interprofessional intervention of geriatric and palliative care consultation in collaboration with a hospitalist service may reduce LOS, especially for geriatric patients, without an increase in readmissions. This model may have broader implications for hospital care and should be further studied.
Keywords: geriatric consultation, palliative care consultation, length of stay, readmissions, utilization
INTRODUCTION
Older patients admitted to the hospital for acute medical services are commonly cared for by hospitalists.1,2 With increasing complexity of our aging population, further attention to hospital outcomes such as length of stay, readmissions, and daily resource utilization is paramount. Daily multidisciplinary discharge rounds including physicians, social work, and nursing have been shown to reduce length of stay for older patients.3,4 Furthermore, by routinely involving acute geriatric and palliative care consultation (GPCC) teams in hospitalist discharge rounds, we previously reported that this intervention increased the number of appropriate inpatient referrals to both geriatrics and palliative care, and the delivery of those consultations earlier in the hospital course.5,6 In addition to formal consultation, our previously reported intervention also provided hospitalist teams with interprofessional interchange regarding discharge planning decisions, such as post-acute nursing home versus home care options, home safety, referral to palliative outpatient services, hospice care, geriatric outpatient consultation and establishment of primary care in geriatrics. By facilitating an interdisciplinary partnership between the three services, our intervention reduced barriers for GPCC involvement early in the hospital course, potentially explained by mechanisms described by others7,8 such as fear of threatening patients’ autonomy and negative perceptions around lack of clinical benefit.
Previous research to improve hospital care outcomes using interdisciplinary and interprofessional models of care has focused on specific patient populations, such as palliative care for oncology patients and geriatric consultation for frail older patients.9–15 Our interprofessional model combines the efforts of Geriatric, Palliative Care, and Hospitalist Medicine, applied to a general medical inpatient service population.5,6 This present analysis aims to understand the potential downstream clinical outcomes of that effort: post-discharge readmissions, length of stay, and the daily intensity of inpatient services utilization. We hypothesized that the intervention would reduce all three outcomes through facilitating decisions for discharge planning, communication across care venues, and by substituting more aggressive hospital services with lower-intensity palliative approaches.
METHODS
Study Design and Data
This non-randomized controlled intervention took place during July 1, 2013-June 30, 2014 and included collection of health system data from July 1, 2012-Aug 30, 2014. This research was considered by the University of Michigan Institutional Review Board (HUM00078475) as exempt from human subject research.
Intervention: the enhanced interprofessional discharge meeting
This controlled intervention took place on 2 of 11 hospitalist inpatient teams in a 1000-bed quaternary U.S. academic medical center during July 2013-June 2014 (1483 patients on the intervention teams, 5413 patients on the 9 control teams). However, because this was a pre-post study, the total patients analyzed also included 7045 patients admitted to all 11 teams during the year prior to the intervention from July 2012 to June 2013 (Figure 1), a total of 13,941 patients age 18 and older over the 2-year analysis. The two intervention teams were chosen pragmatically, because both of these teams served general medical admissions and their case management rounds were held consecutively in the same location, so we could conduct the intervention at both meetings. All the hospitalists rotate through these teams, so we reasonably expected that there would be similar provider characteristics overall. Patients are distributed to teams in most cases based on admission cycle and census, rather than to any particular unit or other patient characteristic. The differences between the intervention and control team patients are described in Table 1. We have written more extensively on the patient population characteristics leading to ordering geriatric and/or palliative care consults (GPCC).5,6
Figure 1. Study Design.
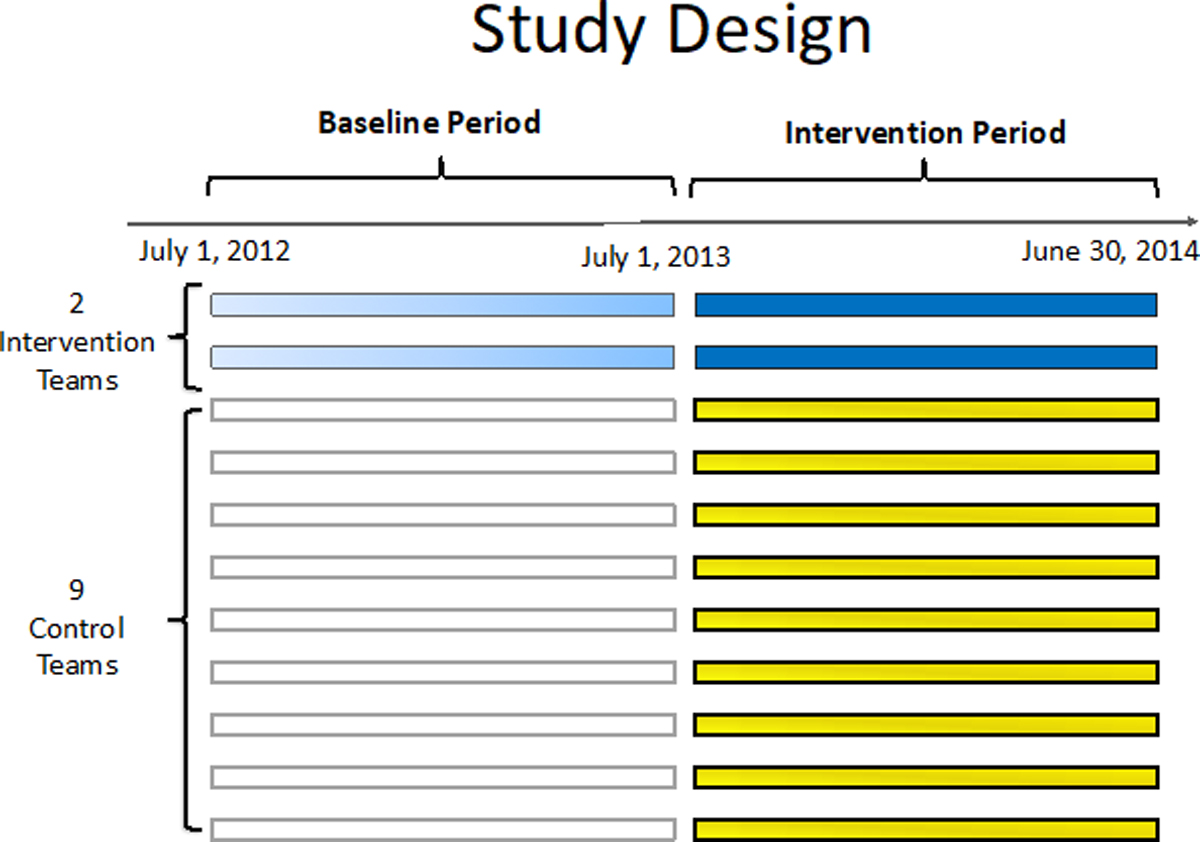
Two years of hospital admissions to 11 acute inpatient teams are depicted in this study design. The dark blue bars represent hospitalizations to two intervention teams, which were compared against two types of control patients: (1) admissions to the intervention team during the prior baseline period (light blue), and (2) non-intervention team admissions (dark and light yellow) during the intervention and baseline periods, respectively.
Table 1:
Sample Characteristics
| Mean or proportion | ||
|---|---|---|
| Overall sample (n=13941) |
Older (Age 65+) subsample (n=5644) |
|
| Age | 58.4 (range 17-104, SD 18.7 years) | 76.5 (range 65-104 SD 8.1 years) |
| Male | 52.2% | 53.6% |
| Any geriatric consult | 2.2% | 5.3% |
| Any palliative care consult | 2.8% | 3.9% |
| Prior hospitalization within 30 days | 18.2% | 17.6% |
| Unadjusted LOS | 5.7 (range 0-154, SD 7.2 days) | 5.7 (range 0-85, SD 6.1 days) |
| Expected LOS* | 5.5 (range 2.1-34.5, SD 2.8 days) | 5.4 (range 2.1-34.5, SD 2.6 days) |
| Adjusted LOS** | 4.3 (range 0-98, SD 3.9 days) | 4.3 (range 0-53, SD 3.6 days) |
| WRVUs per patient-day | 3.6 (range 0-108, SD 4.1 WRVUs per day) | 3.3 (range 0-81, SD 3.5 days) |
| 30-day Readmission | 18.7% | 17.1% |
LOS = Length of Stay
DRG = Diagnosis Related Group
Expected LOS is the mean expected LOS among hospitalizations with the same DRG
Adjusted LOS is the case-mix index adjusted LOS, calculated as unadjusted LOS divided by the case-mix adjustment DRG weight. This weight is greater than 1 for more severe diseases that require more resources on average, less than 1 for diseases that require less than average.
WRVU = Work relative value units
On the two intervention teams, a geriatrician, palliative care physician and social worker attended multidisciplinary discharge rounds twice weekly (every Monday and Thursday). The scope of the intervention rounds was enhanced with in-depth interprofessional discussions of patients with identified geriatric and/or palliative care needs. The consultants offered informal recommendations ranging from pursuing formal inpatient GPCC, post-acute care location, and/or post-discharge outpatient consultation. The hospitalists made the final decision about whether to request an inpatient consult. One palliative team member (JF) attended all intervention meetings and collected all descriptive information.
Usual care on control teams consisted of multidisciplinary discharge rounds with the hospitalist and case manager daily (Monday through Friday) to discuss patients and their discharge needs, lasting 15–30 minutes per team. Hospitalists rotate on a weekly basis to various teams. We previously reported that the intervention did not have a statistically lasting effect within specific hospitalists rotating in and out of the intervention teams, suggesting that any learning effect would not be expected to contaminate the intervention assignment.6 Details about our model are described in full elsewhere.5,6
Outcome Measures
Readmissions were defined as an admission to our institution within 30 days after the date of discharge. Length of stay (LOS) was adjusted for case-mix index, which decreases LOS for more resource-intensive conditions using Diagnosis Related Group (DRG) weights. Admissions without a DRG weight (e.g., “outpatient observation” admissions) were assigned the mean LOS for observation admissions as the DRG weight (0.55 days). Intensity of hospital service utilization was calculated as a daily average of all Common Procedural Terminology (CPT) codes for evaluation and management (e.g., new patient evaluation, follow up hospital visits), tests, and procedures over the inpatient stay. Each CPT was linked to corresponding Work Relative Value Units (WRVU),16 with each unit roughly equivalent to 1 hour of work, adjusted for associated risk and additional resource utilization. We divided total WRVUs by the number of hospital days to obtain the daily utilization intensity measure.
Analysis
Difference-in-differences (DID) analysis
We used a difference-in-differences (DID) analysis to test the effect of being on an intervention team during the intervention period compared to concurrent controls and historic control teams (baseline period). We tested the significance of the interaction term between intervention versus control and intervention versus baseline period (p<.05). This model was necessary to control for secular time trends that may have also occurred concurrently in the outcomes. Moreover, during this study, palliative care doubled its clinical capacity on July 1, 2013. Third, there was also a concurrent, increasing awareness regarding palliative care among hospitalists, including two hospitalists who became palliative care specialty board-certified (RK and DS who served on both intervention and control hospitalist teams).
For each outcome, we tested transformations that would result in the most normal distribution to select the appropriate link for use in generalized linear model regression (glm routine in STATA). The predictors were the main effect of intervention versus control, intervention versus baseline period, the interaction term, and a random effect for patients (to account for patients who might be in the data set multiple times). There was no clustering of GPCC ordering within specific hospitalists,5,6 therefore physician-level clustering was not included in this analysis of outcomes of the GPCC.
The resulting difference-in-difference (DID) for an intervention versus control admission was calculated based on the difference from the intervention period (denoted as T2) minus baseline period (denoted T1):
Because the average DID per patient was difficult to interpret clinically (i.e., a fraction of a hospital day or readmission per patient), we converted the results into the overall effect on the patient population served by the intervention teams. For two outcomes, length of stay and readmissions, we multiplied the DID by the number of patients admitted to the intervention teams during the year of the intervention. The third outcome was a rate, the intensity of RVUs provided per patient-day, so we multiplied this DID by cumulative hospital days of patient care provided by the intervention teams during the intervention year, then divided by 365 days. For the statistically significant associations (p<.05 that the DID was zero), we bootstrapped the results with replacement 1000 times to obtain the 95% confidence intervals around the DID. Because geriatric consults are relevant only in older patients, but palliative care can be ordered in patients of all ages, the results were obtained in the overall sample as well as only in the subgroup of patients age 65 and older. We felt that it was analytically impossible to separate the effect of geriatric versus palliative care consults because both were considered at every enhanced discharge planning meeting, and older patients could potentially receive both consults. To account for this in our design, we studied the full sample of all ages first, then specifically studied only the older patients. We then applied a propensity score analysis which stratifies patients into likelihood of needing consultation because of the prevailing practice pattern of ordering consults for geriatrics and palliative care as a response to the patient (1) being in the hospital for longer than expected (2) being readmitted, and (3) using excessive resources, the outcomes are confounded by indication.
Sensitivity analyses
GPCC-related services (formal consults as well as interprofessional discussion) were differentially provided to patients based on clinical appropriateness, rather than as a randomized intervention. Therefore, we controlled for clinical and demographic differences in the distribution of patients that might have GPCC-relevant issues in the intervention and control groups. To predict patients more likely to have GPCC-relevant issues, we first performed a first-order propensity model using variables that were significant predictors for formal GPCC consultation in prior analyses5,6 or related to one of the outcomes: age (in years), gender, cancer-related admission, admission within the past 30 days, Charlson Comorbidity Score,17 discharge disposition (home, facility, hospice, or hospital death), a weight determined by Elixhauser comorbidity (designed to risk-adjust for readmissions),18–20 and a DRG-assigned weight (designed to adjust for length of stay). The propensity score, which was calculated in the overall sample separately from the age ≥65 sample, was used to divide the sample into 10 equally sized strata, then the analysis repeated within strata and the propensity adjusted DIDs obtained as a sum across the 10 groups. To display smoothed effects graphically, the propensity-adjusted marginal DIDs (triple interaction of intervention*time*decile, all pairs and main effects, with bootstrapped confidence intervals around the effects) are displayed graphically as a function of increasing deciles of propensity to receive GPCC (i.e., as if all the patients were at that varying level of propensity). Second, we clustered by physician instead of by patient. Third, we tested whether the outcomes were plausibly explained by mechanism of increased mortality (i.e., GPCC facilitating more decisions to pursue hospice care), thereby reducing opportunity to realize the outcomes. All analyses were conducted using Stata 14 (College Station, Texas). 21
RESULTS:
Demographics and clinical descriptors
Our analytic sample during the intervention phase was composed of 13941 patients age ≥ 18 and 5644 patients in the age ≥65 years subsample (Table 1), with a mean age of 58 and 77 years, respectively. The older subsample had more geriatric and palliative consultation than the overall sample. Hospital mortality was 1.78% in the overall sample, 2.45% in the older subsample. The mean unadjusted LOS was 5.7 days (range 0–154, SD 7.2 days); the mean adjusted LOS was 4.3 days (range 0–98, SD 3.9 days, Table 2). Each team on the hospitalist service cared for a mean of 12.5 patients per day during the intervention period (SD 1.30), of which 5.09 (SD 0.75) were age >=65 years.
Table 2:
Difference in outcomes associated with the intervention teams
| Outcome | Sample | Estimated DID per patient * | Estimated DID for all patients on the 2 Intervention Teams over the intervention year | ||
|---|---|---|---|---|---|
| Effect | p-value | DID | 95% CI | ||
| Adjusted** Length of Stay (in days) | All patientsa | −0.39 | 0.039 | 528.5 days saved | 112.1 to 1072.7 days saved |
| Age 65+ years b | −0.55 | 0.022 | 315.4 days saved | 76.3 to 605.8 days saved | |
| Readmission within 30 days | All patientsa | −1.17% | 0.482 | 17.4 readmissions saved | −30.8 to + 63.8 readmissions |
| Age 65+ years b | 1.91% | 0.459 | 11.0 additional readmissions | −39.2 to + 17.6 readmissions | |
| Utilization (daily RVUs) | All patientsa | 0.35 | 0.041 | 8.1 additional RVUs generated per day | 0.8 to 15.5 RVUs |
| Age 65+ years b | 0.74 | <0.001 | 6.8 additional RVUs generated per day | 2.9 to 10.7 RVUs | |
DID = Difference in Differences, which is the difference in the outcome over time (from year 1 to year 2) between the intervention and control teams. Outcomes with DIDs associated with statistically significant intervention effect different from zero (p<.05) are bolded.
Length of stay was adjusted for the expected length of stay for that hospital stay diagnosis-related group.
N=1483 hospitalizations of all patients in the overall study
N=subsample of 576 older patients
RVU = Relative Value Units
DRG = Diagnosis Related Groups
The population had a prior hospitalization at this hospital within the past 30 days in 18% and next 30 days after discharge in 18%. The mean intensity of RVUs per day was 3.6 RVUs (SD 4.1). The top 50 most common CPT codes captured in this study are displayed on Table 3. The top CPT code associated with an RVU was a level-3 follow up visit.
Table 3:
Top 50 Clinical Procedure Terminology (CPT) codes used in the utilization outcome whole sample of patients (13941 patients, average LOS 5.7 days)
| Short description | CPT code | RVUs assigned | Total number of times | Percent of all CPT codes |
|---|---|---|---|---|
| Glucose blood test | 82962 | 0 | 107641 | 79.8% |
| Subsequent hospital care (high complexity) | 99233 | 2 | 67861 | 50.3% |
| Complete blood count with white blood count differential | 85025 | 0 | 66506 | 49.3% |
| Complete blood count | 85027 | 0 | 65365 | 48.5% |
| Assay of phosphorus | 84100 | 0 | 64972 | 48.2% |
| Metabolic panel total | 80048 | 0 | 50638 | 37.5% |
| Comprehensive metabolic panel | 80053 | 0 | 40302 | 29.9% |
| Blood gas | 82803 | 0 | 31907 | 23.7% |
| Assay of magnesium | 83735 | 0 | 30982 | 23.0% |
| Assay of lactic acid | 83605 | 0 | 30471 | 22.6% |
| Assay of serum potassium | 84132 | 0 | 25090 | 18.6% |
| Thromboplastin time partial | 85730 | 0 | 24402 | 18.1% |
| Chest x-ray 2 views | 71020 | 0.22 | 23909 | 17.7% |
| Assay of blood chloride | 82435 | 0 | 21899 | 16.2% |
| Prothrombin time | 85610 | 0 | 21882 | 16.2% |
| Assay glucose blood quant | 82947 | 0 | 19368 | 14.4% |
| Assay of calcium | 82330 | 0 | 18485 | 13.7% |
| Emergency department visit | 99285 | 3.8 | 18466 | 13.7% |
| Subsequent hospital care (moderate complexity) | 99232 | 1.39 | 18122 | 13.4% |
| Blood gases oxygen saturation only | 82810 | 0 | 16562 | 12.3% |
| Electrocardiogram report | 93010 | 0.17 | 16038 | 11.9% |
| Therapeutic activities | 97530 | 0.44 | 15761 | 11.7% |
| Urinalysis | 81003 | 0 | 15574 | 11.5% |
| Blood culture for bacteria | 87040 | 0 | 15554 | 11.5% |
| Measure blood oxygen level | 94762 | 0 | 14094 | 10.5% |
| Assay of serum sodium | 84295 | 0 | 13913 | 10.3% |
| RBC antibody screen | 86850 | 0 | 12757 | 9.5% |
| Blood typing rh (d) | 86901 | 0 | 12004 | 8.9% |
| Airway inhalation treatment | 94640 | 0 | 11673 | 8.7% |
| Assay of creatine kinase | 82550 | 0 | 11452 | 8.5% |
| Chest x-ray 1 view | 71010 | 0.18 | 9691 | 7.2% |
| Smear gram stain | 87205 | 0 | 9105 | 6.8% |
| Microscopic exam of urine | 81015 | 0 | 8886 | 6.6% |
| Hospital discharge day | 99239 | 1.9 | 8460 | 6.3% |
| Pulmonary service/procedure | 94799 | 0 | 8297 | 6.2% |
| Assay of lipase | 83690 | 0 | 7671 | 5.7% |
| Urine bacteria culture | 87088 | 0 | 7320 | 5.4% |
| Tissue exam by pathologist | 88305 | 0.75 | 7041 | 5.2% |
| Assay of amylase | 82150 | 0 | 6772 | 5.0% |
| Renal function panel | 80069 | 0 | 6644 | 4.9% |
| Initial hospital care | 99223 | 3.86 | 6305 | 4.7% |
| New physical therapy evaluation | 97001 | 1.2 | 6292 | 4.7% |
| Therapeutic, prophylactic or diagnostic injection | 96375 | 0.1 | 6085 | 4.5% |
| Critical care first hour | 99291 | 4.5 | 5872 | 4.4% |
| Hemoglobin | 85018 | 0 | 5819 | 4.3% |
| Therapeutic exercises | 97110 | 0.45 | 5783 | 4.3% |
| Measure blood oxygen level | 94761 | 0 | 5613 | 4.2% |
| Computed tomography abdomen and pelvis with contrast | 74177 | 1.82 | 5395 | 4.0% |
| Computed tomography head/brain without dye | 70450 | 0.85 | 4836 | 3.6% |
Within 30 days after discharge, 60 patients had an outpatient encounter in geriatric primary care (54 in the older subgroup, or 0.96%) and only 1 patient in an outpatient palliative clinic. Deaths after live discharges within 30 days were recorded in 459 (3.29% of the overall sample), of which 302 (5.35%) were among the older subsample.
The transformations that best normalized the continuous outcomes were logarithmic for adjusted LOS and inverse square root for RVU per day.
Associated outcomes related to intervention
The intervention was associated with two of the three outcomes we studied (Table 2). Adjusted hospital days were saved at 0.36 days per admission (p=.039), for a net savings of 528.5 days [95% CI 112.1–1072.7 days] of hospital care for 1483 patients in the intervention teams during the intervention period. Greater benefit was found for the older subgroup, at 0.55 days per admission, p=.022, or a net savings of 315.4 days [95% CI 76.3 to 605.8 days] of hospital care saved over the 576 older patient admissions during the intervention period. There was no difference in 30-day readmissions: −1.17% (p=.48) for all patients, 1.91% (p = .46) for older patients. Daily resource utilization increased, rather than decreased, for both the overall and the older subgroup, .35 (p<.041) and .74 RVUs (p<.001) per patient-day respectively, resulting in a net utilization of 8.2 RVUs [95% CI .8 to 15.5 RVUs] provided on an average day to intervention team patients and 6.8 RVUs [95% 2.9–10.7 RVUs] for the older subgroup. To put the additional RVUs into clinical context of professional hospital visits, this difference is about equal to 6 extra moderately-complex follow-up hospital care visits (Level 2 99232, worth ~1.4 RVUs) per day for the overall sample, or 5 visits for the older subsample provided between the two teams.
In the sensitivity analyses applied to the statistically significant outcomes, the intervention effects were attenuated after controlling for propensity to receive a GPCC. Adjusted length of stay provided by intervention teams was attenuated from 315 to 253 days for the older subgroup but unaffected in the overall sample (529 to 530 days). The increase in daily RVUs on the intervention teams was adjusted downwards from an additional 8.2 to 7.5 daily RVUs; for the older subgroup, from 6.8 to 6.5 RVUs. Plotted across deciles of propensity for the older subgroup (Figure 2A), a higher propensity for GPCC was associated with reduced adjusted LOS (all patients and older patients), with the confidence intervals departing from zero at propensity in the top (5th decile or higher). Utilization increases, however, reaching significance above the 3rd decile of the propensity scale for the older subgroup (Figure 2B).
Figure 2. Estimated Intervention Effect for Older Patients of Increasing Propensity to Receive Palliative or Geriatric Consultation.
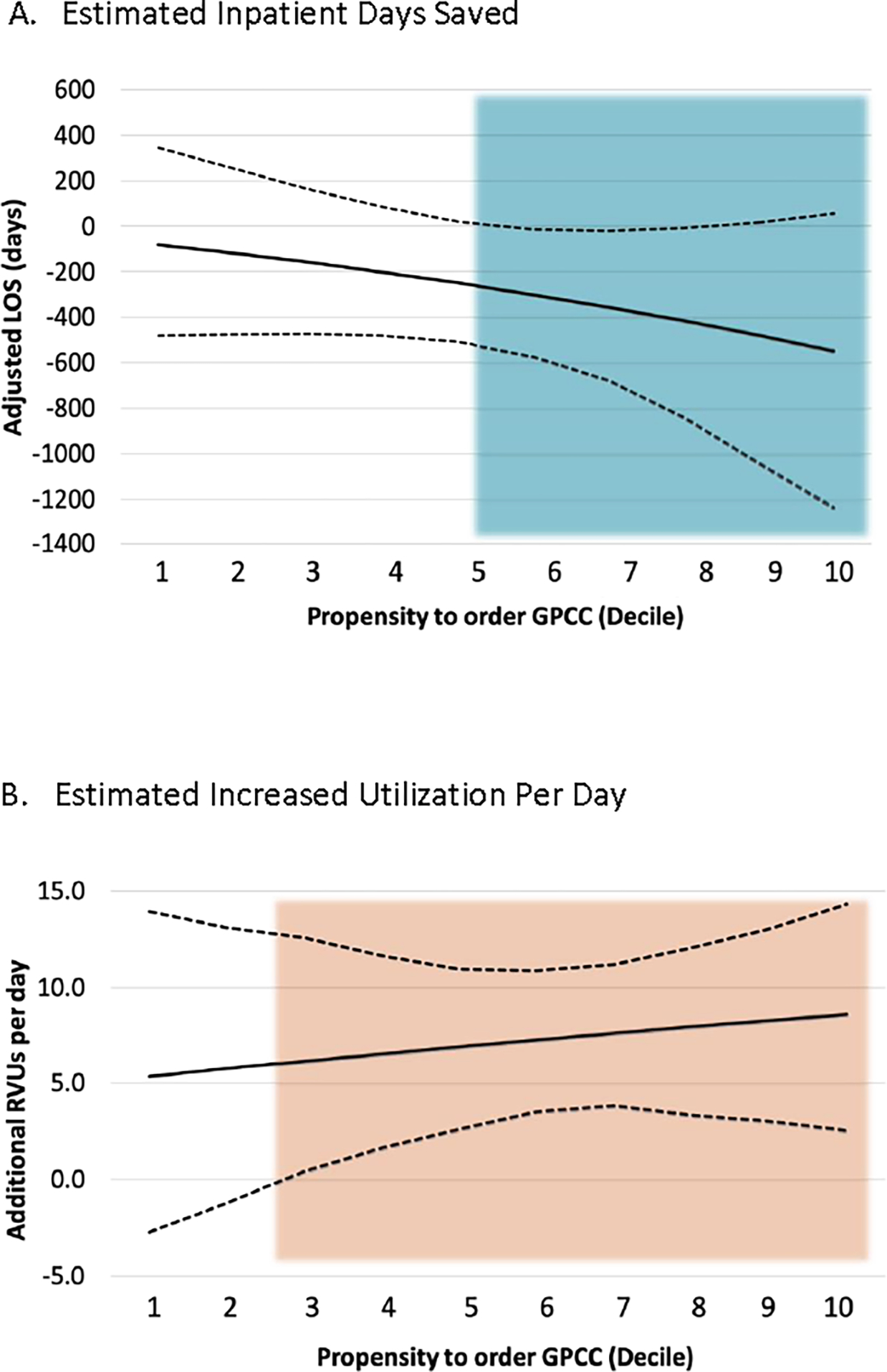
The estimated net effect of the intervention experienced by the two intervention teams for their older patients during the 1-year intervention, by increasing propensity to receive geriatric or palliative care consults (GPCC). Solid line = point estimate for that decile. Dotted line = Bootstrapped 95% confidence interval (percentile method). For length of stay, the annual benefit increased more among the patients in the top half (above 5th decile) of likelihood to receive GPCC. The additional utilization associated with the intervention group increased with increased propensity, statistically different from zero above the 3rd decile.
LOS = length of stay in days
RVU = relative value units
For both the overall and older subgroup, we found no substantive nor statistical modification of the intervention effect by mortality or when clustering by physician instead of by patient.
DISCUSSION:
We found that our intervention was associated with a decreased adjusted length of stay and a small increase in resource utilization, with greater effect among the older patients, those with greater propensity for receiving GPCC, and those more complex based on illness severity, comorbidity, age, and other complexity measures consistent with prior research in older adults. In 2010 Kuo et al found that admissions and reductions in length of stay were greater in older patients and patients with a higher DRG weight.2 As readmission and length of stay are intimately connected, the desire to decrease length of stay by quickly discharging patients from the hospital could increase readmission risk for patients if prematurely discharged, as could poor discharge planning or lack of care coordination.22,23 In our study we did not find such an unintended effect, although we did find a greater utilization of services. For certain conditions, particularly those experienced by older patients receiving geriatric and/or palliative care services, longer length of stays and/or readmission optimization may be preferable to protracted outpatient management.24
While we had hypothesized that involvement of geriatrics and/or palliative care would lead to a decrease in RVUs, the tradeoff of increased net utilization of 8.2 RVUs per average day to intervention team patients and 6.8 RVUs for the older subgroup may be accounted for in part by the GPCC professional visit charges. This is a modest utilization increase when considering that the total patient census on any hospitalist service team would typically range between 11 to 13 patients per day (i.e., 22 to 26 total for the two intervention teams).
Various models of integrating Palliative Care consultation into inpatient oncology care have shown improvement in hospital outcomes including length of stay, readmissions, costs and/or hospice referrals.9–13 In addition, Geriatric interprofessional care can reduce length of stay and costs.14,15
Our study is distinct in evaluating an interprofessional model of both Geriatric and Palliative Care for a heterogeneous inpatient population of all ages and various conditions on a hospitalist service, making it more widely applicable. While data for this study was captured between 2013 and 2015, the Palliative and Geriatric consult team member roles and scope of practice have been stable since then. To accommodate the increase in volume, our health system has developed new service lines for general medical inpatient care (inpatient or observation status). The new teams have the same structure with a case management discharge planning rounds. In response to the COVID-19 crisis, discharge planning rounds are now conducted virtually. Despite this, we believe our findings to still be applicable as functionally the teams remain the same.
Strengths and Limitations
While this analysis benefits from a large sample size and robust, well-developed geriatric and palliative care clinical programs, we recognize limitations including a single-center and a twice weekly intervention to allow for multidisciplinary geriatric and palliative care staff participation, meaning that patients admitted and discharged between meetings could not directly receive the intervention. Additionally, admissions to other hospitals during this period were not captured by this study. Actual readmission rates may have been higher than what was observed, however, we do not expect that the missingness of this outcome differed by intervention team.
By chance, the intervention teams were more likely to have oncology patients. Therefore, we included this as a control variable. As providers on the team rotate every week and overlap between the intervention and control teams, we do not think that physician characteristics were confounding our results. In fact, the rotating nature of the physician between the different teams (which would bias the results toward null), strengthens our findings. Furthermore, adding clustering by physician did not change our results.
Older patients in our study could have received either multidisciplinary geriatric and/or palliative care consultation, thus in this age group we are unable to disentangle which intervention resulted in the identified associations. We believe that the decrease in LOS was facilitated by the multiple components combined, including the interprofessional discussions during rounds and reduced barriers among hospitalists to working with GPCC earlier in the hospital course. These results may not generalize to hospitals without geriatric or palliative care clinical programs, however, virtual attendance by geriatric and palliative care experts may provide similar benefits and would warrant further study.
Finally, because this was not a randomized intervention, the intervention teams may have been more receptive to the intervention, including the individual discharge planners (case managers) who were permanent team members of the teams. In prior research,5,6 we previously demonstrated that increased provision of GPCC was detected even between admissions within providers, i.e., who rotated between and in and out of the intervention and control teams. Thus, to the extent that the schedule was distributed among individual providers, the intervention likely exerted its effect directly as a reminder to order appropriate GPCC and may have had little spillover effect, i.e., when the physicians rotated onto the non-intervention teams. Therefore, we expect that this intervention would not produce sustained outcomes after stopping the intervention.
Clinical Implications
Outcomes measures, while appealing for their ease of being understood by providers, payors, and patients, are challenging to study and interpret, as clear causal links between the care rendered and the outcome achieved are difficult to establish or, subsequently, modify.17 The intervention in our study presents an opportunity for improving LOS for older adults. However, implementation requires assessment of, and possibly restructuring, staffing ratios for geriatric and palliative care consultation services, as well as potential tradeoffs in the form of minor increases in utilization.
Potential future directions would be to apply this model intermittently as new hospitalists are hired/turned over, to apply to other services, and to other types of inpatient hospital teams such as within community hospital settings. As Centers for Medicare and Medicaid Services (CMS) transitions into bundled hospital payment for Medicare beneficiaries, further exploration of costs associated with additional tests, medications and other interventions during the hospitalization is of interest, as is inclusion of available Medicare claims data to ensure that all readmissions are captured in the analyses. Measuring the adherence to consultation recommendations and specific aspects of high-quality transitions of care for the patients who did receive a consultation were beyond the scope of this study but are also of interest for future exploration. Lastly, the COVID-19 pandemic has given rise to new virtual interprofessional rounding opportunities which would facilitate adaptation of this model to a virtual format and allow for further study and dissemination of this model of care.
Conclusion
An interprofessional intervention of geriatric and palliative care consultation in collaboration with a hospitalist service may reduce LOS, especially for geriatric patients. This model may have broader implications for hospital care and should be further studied.
Key Points:
Interprofessional intervention of geriatric and palliative care consultation in collaboration with a hospitalist service during discharge planning rounds decreased adjusted length of stay in adult patients without increasing 30-day readmissions.
The intervention was associated with a minor increase in utilization, a fraction of one relative-value unit per patient per day on average.
Why does this matter?
Reduced length of stay is desired by both patients and healthcare systems and may be facilitated by this interprofessional intervention to enhance delivery of geriatric and palliative care consultation in inpatient hospital care.
ACKNOWLEDGEMENTS:
Funding:
BCBSM-15-PAF07639 01/2016–3/2017/Blue Cross Blue Shield of Michigan Foundation/International. This research was presented as an abstract at the 2019 American Geriatric Society Annual Scientific Meeting.
Footnotes
Conflict of Interest: LM, JW are faculty geriatricians, JF, RK and DS serve on the palliative care service, and RK, DS, and RC are faculty hospitalists; all served intermittently on the inpatient geriatric or palliative care consultation team during this study.
REFERENCES
- 1.Kuo Y-F, Sharma G, Freeman JL, Goodwin JS. Growth in the Care of Older Patients by Hospitalists in the United States. N Engl J Med. 2009;360(11):1102–1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kuo Y-F, Goodwin JS. Effect of hospitalists on length of stay in the medicare population: variation according to hospital and patient characteristics. J Am Geriatr Soc. 2010;58(9):1649–1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gonçalves-Bradley DC, Lannin NA, Clemson LM, Cameron ID, Shepperd S. Discharge planning from hospital. Cochrane Database of Systematic Reviews. 2016(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ortiga B, Salazar A, Jovell A, Escarrabill J, Marca G, Corbella X. Standardizing admission and discharge processes to improve patient flow: A cross sectional study. BMC Health Serv Res. 2012;12(1):180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Puelle M, Wiggins J, Khateeb R, et al. Interprofessional Intervention to Improve Geriatric Consultation Timing on an Acute Medical Service. J Am Geriatr Soc. 2018;66(12):2372–2376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khateeb R, Puelle MR, Firn J, Saul DA, Chang R, Min L. Interprofessional Rounds Improve Timing of Appropriate Palliative Care Consultation on a Hospitalist Service. Am J Med Qual. 2018;33(6):569–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rodriguez KL, Barnato AE, Arnold RM. Perceptions and utilization of palliative care services in acute care hospitals. J Palliat Med. 2007;10(1):99–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kennedy R, Abdullah N, Bhadra R, Bonsu NO, Fayezizadeh M, Ickes H. Barriers to Effective use of Palliative Care Services in the Acute Care Setting with Emphasis on Terminal Noncancer Diseases. Indian J Palliat Care. 2019;25(2):203–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.DiMartino LD, Weiner BJ, Hanson LC, et al. Inpatient Palliative Care Consultation and 30-Day Readmissions in Oncology. J Palliat Med. 2018;21(1):62–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DiMartino LD, Weiner BJ, Hanson LC, et al. The impact of two triggered palliative care consultation approaches on consult implementation in oncology. Healthc (Amst). 2019;7(1):38–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Woodrell CD, Goldstein NE, Moreno JR, Schiano TD, Schwartz ME, Garrido MM. Inpatient Specialty-Level Palliative Care Is Delivered Late in the Course of Hepatocellular Carcinoma and Associated With Lower Hazard of Hospital Readmission. J Pain Symptom Manage. 2021;61(5):940–947.e943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chang S, May P, Goldstein NE, et al. A Palliative Radiation Oncology Consult Service Reduces Total Costs During Hospitalization. J Pain Symptom Manage. 2018;55(6):1452–1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bell CL, Kuriya M, Fischberg D. Hospice referrals and code status: outcomes of inpatient palliative care consultations among Asian Americans and Pacific Islanders with cancer. J Pain Symptom Manage. 2011;42(4):557–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fox MT, Persaud M, Maimets I, et al. Effectiveness of Acute Geriatric Unit Care Using Acute Care for Elders Components: A Systematic Review and Meta-Analysis. J Am Geriatr Soc. 2012;60(12):2237–2245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yoo JW, Kim S, Seol H, et al. Effects of an internal medicine floor interdisciplinary team on hospital and clinical outcomes of seniors with acute medical illness. Geriatr Gerontol Int. 2013;13(4):942–948. [DOI] [PubMed] [Google Scholar]
- 16.Centers for Medicare and Medicaid Services. National Physician Fee Schedule and Relative Value Files. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/PFS-Relative-Value-Files-Items/RVU13A. Published 2013. Accessed 16 December 2020.
- 17.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. [DOI] [PubMed] [Google Scholar]
- 18.Payment of Chronic Care Management Services Under CY 2015 Medicare [press release]. 2015–02-18 2015. [Google Scholar]
- 19.Centers for Medicare and Medicaid Services. CMS DRG weights from 2013, “Table 5: List of final MS-DRGs, Relative Weighting Factors and Geometric and Arithmetic Mean Length of Stay”. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Acute-Inpatient-Files-for-Download-Items/FY2013-FinalRule-CorrectionNotice-Files.html. Published 2013. Accessed 26 April 2019.
- 20.User’s guide APS-DRGs. All Payer Severity-Adjusted DRGS (APS-DRGS®) Normalized Charge, LOS, and Mortality Weights Version 22, healthcare utilization project, AHRQ. https://www.hcup-us.ahrq.gov/db/nation/nis/APS-DRGs%20V22%20Weights%20Manual.pdf. Published 2013. Accessed 26 April 2019.
- 21.StataCorp. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP; 2015. [Google Scholar]
- 22.Jweinat JJ. Hospital readmissions under the spotlight. J Healthc Manag. 2010;55(4):252–264. [PubMed] [Google Scholar]
- 23.Ludke RL, Booth BM, Lewis-Beck JA. Relationship between early readmission and hospital quality of care indicators. Inquiry. 1993;30(1):95–103. [PubMed] [Google Scholar]
- 24.Lane-Fall MB, Neuman MD. Outcomes measures and risk adjustment. Int Anesthesiol Clin. 2013;51(4):10–21. [DOI] [PMC free article] [PubMed] [Google Scholar]


