Abstract
Idiopathic pulmonary fibrosis (IPF) is a chronic inflammatory and fibrotic response-driven lung disease that is difficult to cure because it manifests excessive profibrotic cytokines (e.g., TGF-β), activated myofibroblasts, and accumulated extracellular matrix (ECM). In an attempt to develop an inhalation formulation with enhanced antifibrotic efficacy, we sought to fabricate unique aerosolizable inhaled microgels (μGel) that contain nintedanib-poly(lactic-co-glycolic acid) (PLGA) nanoparticles (NPs; n-PN) and pirfenidone-liposomes (p-LP). The aero-μGel was ∼12 μm, resisted phagocytosis by alveolar macrophages in vitro and in vivo, and protected inner-entrapped n-PN and p-LP. The n-PN/p-LP@aero-μGel caused enhanced/extended antifibrotic efficacy in a bleomycin-induced pulmonary fibrosis mouse presumably due to prolonged lung residence. Consequently, the results obtained by intratracheal aerosol insufflation of our n-PN/p-LP@aero-μGel twice a week were much better than those by as many as seven doses of single or mixed applications of n-PN or p-LP. The antifibrotic/pharmacokinetic results for the n-PN/p-LP@aero-μGel included reduced fibrosis progression, restored lung physiological functions, deactivated myofibroblasts, inhibited TGF-β progression, and suppressed ECM component production (collagen I and α-SMA) along with prolonged lung retention time. We believe that our n-PN/p-LP@aero-μGel increased the local availability of both nintedanib and pirfenidone due to evasion of alveolar macrophage phagocytosis and prolonged lung retention with reduced systemic distribution. Through this approach, our inhalation formulation subsequently attenuated fibrosis progression and improved lung function. Importantly, these results hold profound implications in the therapeutic potential of our n-PN/p-LP@aero-μGel to serve as a clinically promising platform, providing significant advancements for improved treatment of many respiratory diseases including IFP.
Keywords: Aerosolizable microgel, Lung retention, Extracellular matrix, Pro-inflammatory cytokines, Idiopathic pulmonary fibrosis
Graphical abstract
Highlights
-
•
The 12 μm-sized aerosolizable μGel consists of p-LP and n-PN.
-
•
The μGels evade the phagocytosis by alveolar macrophages.
-
•
The μGels prevent rapid clearance and systemic circulation through alveoli.
-
•
The μGels exhibit inhibitory effect on the EMT process of epithelial cells.
-
•
The μGels show significant anti-fibrotic efficacy in mice with pulmonary fibrosis.
1. Introduction
Idiopathic pulmonary fibrosis (IPF) is a progressive and irreversible fibrotic disorder of the lungs, predominantly associated with advanced age, exposure to tobacco smoke, or genetic predisposition [[1], [2], [3]]. IPF is characterized by activated fibroblast/myofibroblast, severe inflammation, and accumulated extracellular matrix (ECM) [4]. In cases where pneumonia progresses to IPF, a reduction in lung volume occurs, accompanied by dyspnea, persistent and severe coughing, and mucus production [5,6]. This debilitating condition lacks a specific curative treatment and is considered incurable. Notably, in the context of the COVID-19 pandemic, the paramount importance of pulmonary fibrosis has been accentuated. Patients that are seriously affected develop pulmonary fibrotic lesions along with release of pro-inflammatory cytokines within the pulmonary microenvironment, ultimately culminating in the development of severe pulmonary fibrosis [7,8].
Among the drugs clinically applied to IPF, pirfenidone and nintedanib have been most common and are approved by the FDA [9,10]. Pirfenidone treats IPF through its anti-fibrotic and anti-inflammatory properties. Specifically, it inhibits transforming growth factor-beta (TGF-β), a cytokine associated with the activation of fibroblasts that contribute to pulmonary fibrosis, and tumor necrosis factor-alpha (TNF-α) and interleukin-1 (IL-1), which are involved in inflammation within the lungs [11]. Nintedanib acts as a tyrosine kinase inhibitor by inactivating receptors on the cell membrane, such as platelet-derived growth factor receptor (PDGFR), fibroblast growth factor receptor (FGFR) and vascular endothelial growth factor receptor (VEGFR), to prevent the aggravation of pulmonary fibrosis by inhibiting the binding of TGF-β and other factors [[12], [13], [14]]. However, these drugs are currently only available as oral agents that have low bioavailability at high doses [6]. To date, there is no inhaled formulation for IPF, but relevant research has been continuously increasing [[15], [16], [17]]. Nonetheless, its symptomatic relief still relies on oral medications. Combination therapy of existing drugs is in the clinical stages [18,19].
There are two types of macrophages in the lungs: alveolar macrophages, which occur in epithelial cells of alveoli, and interstitial macrophages, which occur in the parenchyma between the microvascular endothelium and alveolar epithelium [20,21]. Alveolar macrophages play a crucial role in defending against pathogens, removing insoluble foreign particles, and preventing lung inflammation [22,23]. The bioavailability of inhaled drug particles or nano/microparticles including drugs relies on the significant phagocytic activity of macrophages, which are abundant in the lungs [21]. In total, 12–14 alveolar macrophages exist in each of the 500 million alveoli in human lungs, and they engulf and digest any insoluble particles deposited in alveoli [23]. Alveolar macrophages are ∼13 and ∼21 μm in size in rats and humans [24,25] and prefer to engulf ∼1 or ∼2 μm particles, respectively [[26], [27], [28], [29], [30], [31]]. Consequently, alveolar macrophages tend to clear particles that are smaller than themselves. This vigorous phagocytosis by alveolar macrophages hinders the long retention and therapeutic effect of particle-based delivery systems including antifibrotic drugs at the target lung site.
Herein, we attempt to introduce nintedanib-loaded PLGA nanoparticles (n-PN) and pirfenidone-loaded liposomes (p-LP) entrapped in aerosolizable microgels for inhalation, hereafter termed n-PN/p-LP@μGel or n-PN/p-LP@aero-μGel, for improved treatment of IPF through prolonged therapeutic effects. First, the hydrophobic and hydrophilic antifibrotic drugs nintedanib and pirfenidone were incorporated into poly(lactic-co-glycolic acid) (PLGA) nanoparticles (NPs) and liposomes, respectively, which are FDA-approved biodegradable materials (PLGA/various lipids) with good biocompatibility and safety. These NPs ensured satisfactory drug incorporation and were the correct size for pulmonary aerosolization. Second, aerosolizable/inhalable microgels consisting of 4-arm PEG and albumin entrapping both NPs were fabricated at a size of ∼12 μm, which significantly slows or evades the phagocytic activity of alveolar macrophages to prolong lung retention time [32,33]. Importantly, we aimed to minimize the dosing frequency and extend the antifibrotic efficacy derived from the NPs protected by outer microgels (Scheme 1). To support this hypothesis, the reduced progression of fibrosis, restored lung physiological functions, deactivated myofibroblasts, inhibited TGF-β progression, and suppressed ECM component production (collagen I and α-smooth muscle actin, α-SMA) were measured in various lung and macrophage cells in vitro and in an IPF mouse model in vivo. In addition, an optimized formulation of n-PN/p-LP@aero-μGels was administered to mice with bleomycin-induced pulmonary fibrosis using a micro-spray aerosolizer.
Scheme 1.
Schematic illustration showing aerosolizable inhaled microgels incorporating nintedanib-PLGA nanoparticles and pirfenidone-liposomes, which are able to evade severe phagocytosis by alveolar macrophages for manifestating improved treatment of pulmonary fibrosis.
2. Results and discussion
2.1. Preparation and characterization of pirfenidone-loaded liposomes (p-LP) and nintedanib-loaded PLGA NPs (n-PN)
We designed and fabricated biocompatible μGel encapsulating pirfenidone-liposomes (p-LP) and nintedanib-PLGA nanoparticles (n-PN) [n-PN/p-LP@μGel] as an inhalation drug delivery system. All the main materials for preparation of n-PN/p-LP@μGel are FDA-approved biodegradable and biocompatible substances with negligible toxicity issues due to the importance of the respiratory route. These materials comprise human serum albumin (HSA), polyethylene glycol (4-arm PEG20k-NHS), PLGA (polylactic-co-glycolic acid: RG502H), and lipids (DSPE-PEG2000 18:0, DOPC 18:1 (Δ9-Cis), and cholesterol) [34]. Owing to these advantages, pulmonary drug delivery carriers using PLGA NPs and liposome/lipid NPs have been extensively pursued [[35], [36], [37]]. In particular, liposomes have gained popularity due to their similar composition to pulmonary surfactants, indicating them as a suitable choice for local lung delivery [38]. Recently, a liposomal Amikacin formulation product for inhalation (Arikayce; DPPC:cholesterol = 2:1) was approved by the FDA and is clinically available for non-tuberculous lung disease caused by the mycobacterium avium complex [39,40].
The first step in the process is to fabricate two individual NPs incorporated into the aero-μGel. The schematic image illustrated in Fig. 1A presents the general process of NP fabrication. Specifically, nintedanib-PLGA NPs (n-PN) were prepared using the nanoprecipitation method to facilitate uniform particle size, forming a water-in-oil (W/O) emulsion. The size and zeta potential of n-PN were 189.7 nm and −23.3 mV, respectively, using dynamic light scattering (DLS) (Fig. 1B and C). For the pirfenidone-liposome (p-LP) formulation, neutrally charged liposomes were prepared using a molar ratio of 32:15:3 of DOPC, cholesterol, and DSPE-PEG2000. The neutral liposomes were considered for their enhanced ability to penetrate mucus versus cationic or negatively charged liposomes, providing an advantage for our intended purposes [36]. The size and zeta potential of p-LP were 89.3 nm and −3.9 mV, respectively (Fig. 1B and C). The photo images in Fig. 1C illustrate n-PN and p-LP in an aqueous solution. Additionally, n-PN and p-LP maintained particle sizes that were very close to their initial sizes over 72 h at room temperature, indicating excellent colloidal physicochemical stability (Fig. 1D). Furthermore, nonsignificant changes in their polydispersity index (PDI) were observed (<0.05 and 0.10, respectively), indicative of particle uniformity (Fig. 1E). These findings indicate that the NPs had robust stability and favorable shelf life under the specified conditions. UV absorbance spectra were used to ascertain the successful encapsulation of drugs within the NPs. The characteristic peaks corresponding to pirfenidone and pirfenidone-liposomes were shown at approximately 310 nm, whereas nintedanib and nintedanib-PLGA NPs exhibited peaks around 390 nm. This corroborates the effective incorporation of drugs within the respective NPs (Fig. 1F). Furthermore, the microgels with incorporated pirfenidone-liposomes and nintedanib-PLGA NPs were found to have very similar UV absorbance characteristics of pirfenidone and nintedanib, respectively (Fig. 1G). Transmission electron microscopy (TEM) and scanning electron microscopy (SEM) images displayed the spherical morphology and notable size homogeneity of both n-PN and p-LP (Fig. 1H). The drug release patterns from each type of NP were monitored over 72 h, showing the sustained release of both drugs without an initial burst-out. Quantification of the loading efficiencies of pirfenidone and nintedanib was conducted using HPLC and UV–visible spectrometry, respectively (Fig. 1I). Additionally, the encapsulation efficiency for pirfenidone and nintedanib was ∼30 % and 54 %, respectively, which were not considered high but sufficient for therapeutic efficacy. Subsequently, physico-chemically stable nintedanib-PLGA NPs and pirfenidone-liposomes were fabricated in homogeneous sizes for the next step of encapsulation into the microgels.
Fig. 1.
(A) Schematic illustration showing aerosolizable microgels (μGel) encapsulating nintedanib-PLGA NPs (n-PN), pirfenidone-liposomes (p-LP), and n-PN/p-LP@aero-μGel. (B) Histograms for the hydrodynamic size of p-LP and n-PN. (C) Zeta potentials of p-LP and n-PN: Insets - photo images for colloidal states of p-LP and n-PN. (D) Physicochemical colloidal stability of p-LP and n-PN over 72 h. (E) Polydispersity index (PDI) profiles for p-LP and n-PN over 72 h. (F) UV-VIS absorption spectra for NT, PF, p-LP, and n-PN. (G) UV-VIS absorption spectra for naïve μGel, n-PN@μGel, and n-PN/p-LP@μGel. (H) Transmission electron microscopy (TEM; top) of p-LP and n-PN and field-emission scanning electron microscopy (FE-SEM; bottom) images of n-PN. (I) Drug release profiles of p-LP and n-PN over 72 h.
2.2. Fabrication and characterization of aerosolizable microgels containing p-LP and n-PN
Our next goal was to prepare aerosolizable microgels (μGel) encapsulating p-LPs and n-PNs. The direct pulmonary application of nanoparticles is subject to rapid clearance, resulting in low bioavailability. In general, inhaled dry nanoparticles <1 μm are prone to be exhaled predominantly through Brownian diffusion (∼80 %) due to their low inertia [41]. However, particles >2.5 μm can deposit in the lungs due to sedimentation and diffusion processes [42]. Furthermore, aerosolized NPs are exposed and trapped in the thick mucus layer (∼5 μm) in airways or alveoli and further subjected to mucociliary clearance. Also, a fraction of inhaled NPs can enter systemic circulation through the alveolar epithelium, which potentially decreases the local bioavailability of antifibrotic drugs [[43], [44], [45]]. Therefore, we sought to achieve an additional microgel system to entrap such nanoparticles and prevent their clearance.
The aerosolizable μGels were prepared by slight modification of a previous method [46] in which the W/O emulsion method was used with a homogenizer. Herein, we used four-arm PEG20k-NHS as a main crosslinker to form a micro-sized gel and tried to minimize the amount of glutaraldehyde (GA) (final concentration: ∼0.01 %), whereas the conventional formulation necessitated at least 0.5–1.0 % GA [46]. At the significantly lower GA concentrations, the molar ratio of PEG:HSA was optimized to show best performance for an aerosolizable μGel formulation in terms of gelation time and gel property: the ratio was determined to be best at 1:2.8, resulting in a soft gel property (Fig. S1 and Supplementary Notes). Consequently, the amount of GA used in this study was 50–100 times lower than in other studies [[46], [47], [48]], and this amount showed negligible toxicity to the cells [49]. Another aim was to optimize the size of the aero-μGel to evade phagocytosis by alveolar macrophages. After considering the size range (13–21 μm) of alveolar macrophages, a series of 6-, 12-, and 18-μm-sized microgels was prepared, and their bypass by alveolar macrophages was evaluated. The fluorescence-guided morphologies of microgels of 6, 12 and 18 μm were examined by using confocal microscopy (CLSM), and the representative μGel of 12 μm was found to be highly homogeneous and spherical (Fig. 2A). The n-PN was dispersed in the water phase, along with HSA and 4-arm PEG20k-NHS and incorporated into the μGel during W/O homogenization. The resulting μGel was subjected to lyophilization to create powder particles, and p-LP was highly permeated into the mesh of well-dispersed μGel suspension in PBS.
Fig. 2.
(A) CLSM images of (a) 6-, (b) 12- and (c) 18-μm sized fluorescent μGels and SEM images of n-PN/p-LP@μGel (12 μm). (B) CLSM images of coumarin 6-n-PN/DiI-p-LP@Ce6-μGel. (C) Photographs of (a) dry powder and (b) dispersed solutions of n-PN/p-LP@μGel (12 μm). (D) High magnification CLSM images of coumarin 6-n-PN/DiI-p-LP@Ce6-μGel (12 μm). (E) FIB-SEM images of (a) naïve μGel, (b) p-LP@μGel, (c) n-PN@μGel, and (d) n-PN/p-LP@μGel.
The CLSM images exhibited a clear incorporation of DiI-doped p-LP (blue) and coumarin-6-loaded n-PN (green) into 12 μm-μGels as well as the HSA (Ce6-tagged) backbone of the μGel (red) (Fig. 2B and D and S2). Fig. 2C showed the physical state of n-PN/p-LP@μGel (12 μm) as its powder and solution forms. The incorporation of n-PN and p-LP was confirmed again through focused ion beam (FIB)-SEM (Fig. 2E). Cross-sectional surface analysis revealed that the water-phase disperse n-PN was embedded within the internal network structure of the μGel, and the permeated p-LP was placed inside and on the surface of the μGel.
2.3. Suppression of TGF-β-induced myofibroblast activation/differentiation
A series of in vitro cell experiments was conducted to investigate the effects of antifibrotic drugs (hereafter termed NT for nintedanib and PF for pirfenidone) and n-PN/p-LP@μGel on inhibiting fibroblast activation and their transformation into myofibroblasts. Specifically, we assessed the inhibitory activities of the fabricated n-PN and p-LP on epithelial-mesenchymal transition (EMT) processes in A549 epithelial cells. In brief, EMT is a biological process that allows polarized epithelial cells interacting with the basement membrane to transform into mesenchymal cell phenotypes and is characterized by greatly increased ECM production, elevated resistance to apoptosis, and enhanced migratory capacity. The reduced expression of E-cadherin in 2D or 3D cells is considered the result of the EMT process [50,51].
Initially, MTT assays were performed after treating both epithelial cells and fibroblast cells with different concentrations of samples (NT, PF, n-PN, and p-LP) to evaluate their effects on cell proliferation (Fig. 3A and S3). At fixed NT doses of 10 or 50 μM, higher levels of PF led to greater inhibition of A549 cells in both groups of free drugs and NPs, which demonstrated the inhibitory activity of antifibrotic drugs released from the NPs. To investigate the expression level of the key epithelial marker E-cadherin, we conducted an immunofluorescence (IF) analysis. As shown in Fig. 3B, the TGF-β-treated groups experienced a substantial progression of the EMT process. However, the progression of EMT was significantly attenuated in A549 cells treated with NT/PF and n-PN/p-LP. The n-PN/p-LP treatment exhibited the most pronounced effect compared to the individual NT/PF treatments. Among these groups, a hierarchical expression pattern of E-cadherin was observed in the order of NT/PF, n-PN/p-LP, NT, n-PN, PF, and p-LP. Notably, the migration assays revealed a slower A549 lung cell differentiation rate in the order of NT/PF, n-PN/p-LP, NT, n-PN, PF, and p-LP. This could be attributed to differentiation induced by TGF-β but which was significantly prevented by NT/PF and n-PN/p-LP (Fig. 3C and D). Protein expression levels were assessed through western blotting, with a focus on the mesenchymal/epithelial characteristic markers of vimentin and E-cadherin, which are the key factors of the EMT process (Fig. 3E and F). The results indicated an increasing trend in the expression level of vimentin in the order of NT/PF, n-PN/p-LP, NT, n-PN, PF, and p-LP. Conversely, the expression of E-cadherin displayed a decreasing trend. While the E-cadherin/vimentin ratio was lowest in the media (+TGF-β alone) group, combined groups of NT/PF and n-PN/p-LP treatment exhibited notably higher values and indicated improved effects (Fig. 3G). In terms of cellular morphology changes, the media (+TGF-β alone) group exhibited the most pronounced alterations (Fig. 3H).
Fig. 3.
(A) Cell growth inhibition of NT, PF, n-PN, and p-LP at various concentrations in A549 cells using an MTT assay. (B) CLSM images of E-cadherin immunostaining in A549 cells after TGF-β (final concentration: 10 ng/mL) stimulation with NT (10 μM), PF (50 μM), n-PN (10 μM), and p-LP (50 μM) for 48 h. (C) Microscope images and (D) determination of cell migration under treatments after 24 h incubation (red dash lines indicate 500 μm gaps). *p < 0.001 over PF. (E) Western blot analysis and (F) EMT progression image. (G) Determination of vimentin and E-cadherin expression in A549 cells after TGF-β (final concentration: 10 ng/mL) and stimulation with NT (10 μM), PF (50 μM), n-PN (10 μM), and p-LP (50 μM). *p < 0.01 over PF and NT; **p < 0.05 over PF and NT. (H) Microscope images of the morphology of A549 cells after TGF-β (final concentration: 10 ng/mL) and stimulation with NT (10 μM), PF (50 μM), n-PN (10 μM), and p-LP (50 μM) for 24 h.
As mentioned previously, the MTT assay was also conducted on NIH/3T3 fibroblast cells. The experiments were carried out using the same drug concentrations as those in A549 cells (10 μM for NT and 50 μM for PF) (Fig. 4A). First, 2D-immunofluorescence was performed to assess the distribution patterns of collagen I and α-SMA, indicative of myofibroblast differentiation (Fig. 4B). Whereas TGF-β treatment critically expressed both collagen I and α-SMA, the NT and PF or n-PN/p-LP remarkably suppressed the expression of both fibrosis markers, indicating that our NP groups had antifibrotic activity. We further tried to confirm the inhibitory effects of sample groups on the activated state of fibroblast cells using NIH/3T3 cell lines in terms of migratory/invasive and contractile properties using Transwell migration assays and collagen gel contraction, respectively. Results revealed that TGF-β stimulation enhanced the migratory (Fig. 4C and D) and contractile (Fig. 4E and F) capacities of the fibroblast cells. Importantly, treatments with n-PN, p-LP, and n-PN/p-LP effectively mitigated those effects induced by TGF-β. Notably, the inhibitory effect caused by n-PN/p-LP treatment was comparable to that of the control or NT/PF group, indicating that the TGF-β activities were critically offset. To mimic the three-dimensional (3D) lung microenvironment, we developed a 3D spheroid model (∼350 μm) comprising epithelial and fibroblast cells (A549, NIH/3T3 cell line). Spheroid construction allowed a comprehensive analysis of the extent of EMT induced by TGF-β and the activation level of fibroblasts (Fig. 4G). In addition, the analysis of z-axis layers (30 μm spacing) of the merged spheroids was shown to provide a more convincing insight into the extent of EMT and activation level of fibroblasts induced by TGF-β (Fig. S4). As a result, we validated the effectiveness of our n-PN/p-LP group as well as free antifibrotic drugs. Similar to the 2D results, the effect of n-PN/p-LP led to significantly reduced expression levels of α-SMA and collagen I on the surface of spheroids compared to the group treated with TGF-β alone.
Fig. 4.
(A) Cell growth inhibition of NT, PF, n-PN, and p-LP at various concentrations in NIH/3T3 fibroblasts using an MTT assay. (B) CLSM images of DAPI (blue), α-SMA (green), and collagen I (red) immunofluorescence staining in NIH/3T3 cells after TGF-β (final concentration: 10 ng/mL) and stimulation with NT (10 μM), PF (50 μM), n-PN (10 μM), and p-LP (50 μM) for 48 h. (C) Microscope images and (D) determination of cell migration of NIH/3T3 fibroblasts using a Transwell migration assay for 24 h: Inset - illustration for transwell-based cell migration. *p < 0.005 over PF and NT. (E) Microscope images and (F) determination of contraction of NIH/3T3 fibroblast gels using a gel contraction assay for 48 h *p < 0.005 over PF and NT. (G) CLSM images of DAPI (blue), α-SMA (green), and collagen I (red) immunostaining in A549/3T3 co-culture spheroids after TGF-β (final concentration: 10 ng/mL) and stimulation with NT (10 μM), PF (50 μM), n-PN (10 μM), and p-LP (50 μM) for 48 h.
2.4. Aero-microgels evading macrophage phagocytosis
As mentioned, an overwhelming number (6–7 billion) of alveolar macrophages exists in the alveolar region of human lungs [23], and these macrophages clear appropriately sized insoluble particles via phagocytosis. This phagocytic clearance alleviates concern regarding inhaled particles consisting of only drugs and some excipients (e.g., inhalation lactose) but can be a critical threaten to inhaled sustained depot systems that deposit in the lungs and release drug for a considerable time over several days. Unfortunately, some particles might be immediately removed and inactivated by engulfment of numerous alveolar macrophages without even manifesting a therapeutic effect. One of the well-established approaches is to modulate the size of inhaled particles to evade or slow the phagocytic activity of macrophages that are unable to engulf a certain size range of particles. Macrophages exhibit immune responses toward particles roughly ranging in size from 0.1 to 10 μm (sometimes 20 μm) [25,52]. Particularly, a size around 1 μm is best for macrophage phagocytosis, exhibiting elevated production of proinflammatory cytokines, whereas lower or negligible responses are observed with other sizes [52]. In another article, particles with diameters of 2–3 μm exhibited maximal phagocytosis and attachment [53]. Therefore, the administration dosage and frequency have to increase due to the phagocytic uptake of nano- or micro-particles by macrophages [54]. This limitation compromises the efficacy of inhaled formulations and causes inconvenience to patients due to the need for repeated administrations. To overcome this challenge, we aimed to achieve an effective sustained-release μGel (∼12 μm) formulation incorporating p-LP and n-PN, allowing significant evasion of alveolar macrophage phagocytosis. Again, this approach can be used to reduce the frequency and/or dosage of drug administrations.
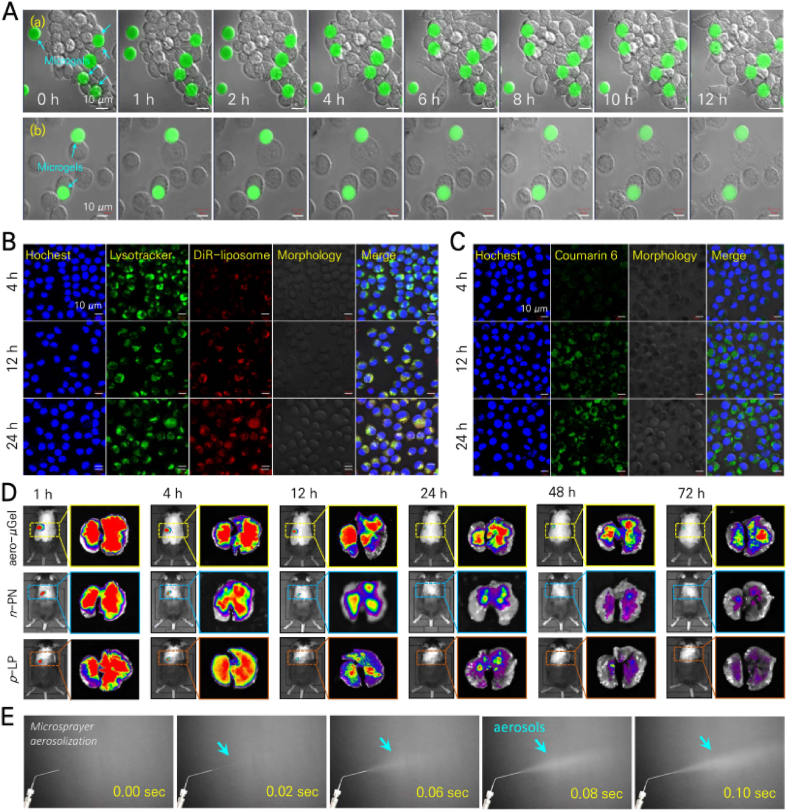
Consequently, n-PN/p-LP@μGel of approximately 6, 12, and 18 μm sizes were individually fabricated to evaluate their ability to evade phagocytosis. As shown in Fig. 5A, S5 and S6, n-PN/p-LP@μGels of the three sizes were treated with RAW 264.7 macrophages, and both μGels and macrophages were monitored over 12 h using a time-lapse video (Supplementary Video 1, 2 and 3). Additionally, the fluorescence of n-PN/p-LP@μGels was determined over 72 h. Over 12 h, macrophages took up very few n-PN/p-LP@μGels of 18 μm, and n-PN/p-LP@μGels of 12 μm were taken up at a much lower rate than n-PN/p-LP@μGels of 6 μm (Fig. 5A, S5 and S6). Similar patterns were obtained when conducting the same treatments with J774A.1 macrophages (Fig. 5A, S5 and S6), and these observations were confirmed through time-lapse videos. In contrast, significant fractions of n-PN and p-LP NPs were readily taken up by RAW 264.7 macrophages even as early as 4 h. After 72 h, a considerable fraction of each NP appeared inside macrophage cells (Fig. 5B and C). The uptake mechanism of colloidal NPs by RAW 264.7 macrophages seldom involves phagocytosis, which is activated usually for large solid particles [55]. Nonetheless, n-PN and p-LP seemed to be very rapidly cleared by RAW 264.7 cells. Separate aliquots (50 μL) of Cy5.5-conjugated n-PN/p-LP@μGel of approximately 6, 12, and 18 μm in size and coumarin 6-n-PN, DiR-p-LP of roughly 90, 190 nm in size (as a control) were aerosolized into the trachea of live C57BL/6 mice to examine their biodistribution and clearance in the lungs (Fig. 5D, S7 and S8). As shown in Fig. 5E, n-PN/p-LP@μGels (12 μm) exhibited good aerosolization performance using a micro-spray aerosolizer, which is considered to appropriate for intratracheal inhalation to mice (Fig. 5E and S9). Additionally, the lung depositions of coumarin 6-labeled n-PN and DiR dye-labeled p-LP were visualized using fluorescence imaging of (i) the whole body including intact lungs of live mice and (ii) the excised lungs from sacrificed mice (Fig. 5D and S7). Notably, the same pattern for fluorescence intensity was obtained in both live and excised lungs for each sample group. Of prime importance, the ∼12-μm-sized PN/p-LP@μGels, closely resembling the size of macrophages, had prolonged retention of up to 3 days within the lungs.
Fig. 5.
(A) CLSM time-lapse images for 12-μm sized μGels showing phagocytotic engulfment by (a) RAW 264.7 and (b) J774A.1 cells for 12 h. (B) CLSM images for uptake of DiR-p-LP by RAW264.7 cells. (C) CLSM images of uptake of coumarin 6-n-PN by RAW264.7 cells. (D) Live mouse whole body/ex vivo fluorescence images for the lungs after intratracheal micro-spraying aerosolization of 12-μm-sized Cy5.5-n-PN/p-LP@aero-μGel, coumarin 6-n-PN, and DiR-p-LP. (E) Photo images for aerosolization of n-PN/p-LP@aero-μGel (12 μm) using micro-spray aerosolizer at the time points of 0, 0.02, 0.06, 0.08 and 0.10 s.
2.5. Antifibrotic efficacy of n-PN/p-LP@aero-μGels in mice with bleomycin-induced pulmonary fibrosis
Based on the significant alleviation of TGF-β-induced fibroblast activation by NT-PLGA NPs (n-PN)/PF-liposomes (p-LP) in vitro, we evaluated the therapeutic efficacy of six groups (G1, PBS only; G2, bleomycin only (non-treated); G3, n-PN; G4, p-LP; G5, n-PN/p-LP; G6, n-PN/p-LP@μGels) in mice. First, we established a pulmonary fibrosis model in C57BL/6 mice by intratracheal administration of bleomycin at a dose of 3.5 mg/kg. After seven days, each mouse was intratracheally administered the appropriate treatment using a micro-spray aerosolizer and doses of PF (15 mg/kg) and NT (4 mg/kg). As mentioned, G6 samples were administered twice over 7 days, on days 1 and 4, whereas all other samples were given daily (Fig. 6A). The weight of the mice was monitored throughout the experiment as a significant indicator of health or recovery from IPF (Fig. 6B). Following bleomycin administrations, the weight of G2 mice rapidly decreased and did not recover due to severe dyspnea, whereas the weight of G1 negative control mice increased continuously. The other test groups showed a rebound in weight after a gradual decrease, Interestingly, the weight of the G6 (n-PN/p-LP@ aero-μGels) mice showed the smallest loss and a rapid recovery, indicating amelioration of pulmonary fibrosis. Only half of the G2 mice survived, whereas the treated groups exhibited increased survival, with no mortality among the G5 and G6 mice (Fig. 6C). After 21 days, the mice were sacrificed for lung analysis. Initially, we evaluated lung sections stained with hematoxylin and eosin (H&E) based on the modified Ashcroft score analysis, following established criteria (Fig. 6D, E and 6F). In comparison to G1 healthy control mice, the lung sections from G2 bleomycin-treated mice exhibited significant structural distortion and an increased extent of fibrosis, confirming successful induction of pulmonary fibrosis. Masson trichrome (MT) staining of lung sections revealed collagen and fibrotic areas, prominently in G2 (Fig. 6D and E), indicative of pulmonary fibrosis. Conversely, the other treatment groups G3–G6 demonstrated reduced collagen levels compared to those of G2, suggesting a mitigating effect on the progression of fibrosis (Fig. 6G). Additionally, a hydroxyproline assay was used to quantify the concentration of hydroxyproline, another well-known marker of fibrosis progression. Significantly, the lungs of mice treated with G6 of n-PN/p-LP@ aero-μGels exhibited a substantial reduction in hydroxyproline concentration, evidence of the in vivo antifibrotic effect of G6 in alleviating bleomycin-induced pulmonary fibrosis (Fig. 6H). Importantly, results of all staining and biomarkers (e.g., H&E, MT, collagen intensity, and hydroxyproline) of G6 treated with n-PN/p-LP@aero-μGels were comparable to those of healthy G1 and daily NP-treated G5 (n-PN/p-LP; 3.5 times greater total doses of NT/PF vs. G6). The G3–G5 mice received a daily dose (4 mg NT/kg/day and/or 15 mg PF/kg/day) for 7 days, whereas G6 mice received the same dose only on days 1 and 4. Such observations indicated the improved potential of inhaled n-PN/p-LP@aero-μGels for treating pulmonary fibrosis in the context of sustained drug release and prolonged lung deposition due to evasion of phagocytosis.
Fig. 6.
(A) Brief animal experiment schedule for anti-fibrosis efficacy in bleomycin-induced pulmonary fibrosis mice. (B) Weight change profiles in mouse groups. G1: PBS; G2: bleomycin (3.5 mg/kg); G3: n-PN (4 mg/kg/day) for 7 days; G4: p-LP (15 mg/kg/day) for 7 days; G5: n-PN/p-LP (4 mg/kg/day+15 mg/kg/day) for 7 days; G6: n-PN/p-LP@μGel (4 mg/kg/day+15 mg/kg/day) on days 1 and 4. *p < 0.05 over G5. (C) Survival rates of mice by group. (D) Representative image of hematoxylin and eosin (H&E) and Masson's trichrome (MT) staining in the lung tissue. (E) High-magnification H&E and MT images for lung tissues of each group. (F) Ashcroft score analysis. *p < 0.01 over G3 and G4. (G) Collagen intensity measurements of lung tissue from MT images by group. **p < 0.05 over G3 and G4. (H) Evaluation of the hydroxyproline (HYP) level by group using an HYP assay. ***p < 0.05 over G3 and G4.
The damage and roughness of the lungs of each group of mice were visualized three-dimensionally using micro-CT imaging, which can directly associate lung function and fibrotic severity (Fig. 7A and S10). The 3D reconstruction of scanned lung images from micro-CT imaging showed the roughness of the lung surface and the presence of empty spaces in terms of lung damage. Three-dimensionally estimated lung volumes were used as the degree of antifibrotic efficacy for each treatment (Fig. 7B). Moreover, the ratio of lung weight to body weight served as an index of fibrosis severity and aligned with the previous findings (Fig. 7C). Consistently, the estimated lung volumes and lung index demonstrated repair of lungs of G6 mice, similar to those of the G1 healthy control mice, indicating the therapeutic effectiveness of inhaled n-PN/p-LP@aero-μGels. In pulmonary fibrosis, the initial predominance of M1 macrophages due to the inflammatory response transitions to fibroblast activation facilitated by increased M2 macrophages. Interestingly, the flow cytometric result of G6 displayed a much lower level (2.59 %) of M2 macrophages compared with that of G2 (24.9 %) and was comparable to the results of the healthy control (2.03 %) (Fig. 7D and E and S10), indicating inhibition of M2 macrophage polarization.
Fig. 7.
(A) Representative images of micro-computerized tomography (CT), 3D reconstruction, and photographs of the lungs of G1–G6 groups. (B) Lung volume ratio according to the micro-CT images. (C) Lung index (lung weight/body weight) in G1–G6 groups. *p < 0.005 over G3 and G4. (D) Representative flow cytometric plot of M2 macrophage cells and (E) corresponding quantification results of M2 macrophage polarization for G1, G2, and G6 groups. P-value was calculated by the unpaired Student's t-test in (E). *p < 0.05, **p < 0.01, ***p < 0.001.
The lung tissue sections of each group were subjected to immunofluorescence (IF) for collagen I, α-SMA, and immunohistochemistry (IHC) staining of TGF-β to assess the degree of fibrosis or recovery by sample treatment (Fig. 8A). Pronounced levels of collagen I, α-SMA, and TGF-β distribution were observed in the G2 group. The overall expression intensity in G5 and G6 was lower than those of G3 and G4. The total number of cells in the bronchoalveolar lavage fluid (BALF), serving as an indicator of inflammatory cell infiltration, exhibited a significant decrease in all treatment groups (Fig. 8B). Increased total cell counts in BALF are typically associated with elevated cytokine levels. As shown in Fig. 8C, the level of TGF-β in BALF was highest in G2, whereas the level decreased in G5 and G6. Moreover, Western blot analysis was performed using lung tissue samples to evaluate the therapeutic effects through fibrosis-associated indicators, namely fibronectin, collagen I, and α-SMA (Fig. 8D). Unlike the high values found in G2, levels from G6 lungs were similar to those of the healthy control (Fig. 8E). Finally, we sought to evaluate the therapeutic effects of inhaled n-PN/p-LP@aero-μGels on impaired lung function using the precise forced oscillation technique. On day 21 after the treatment, 3 groups were examined: healthy mice, G1; mice with bleomycin-induced pulmonary fibrosis, G2; and mice treated with inhaled n-PN/p-LP@aero-μGel, G6. Key indicators of respiratory resistance (Rrs) and elastance (Ers) exhibited notable increases in mice with fibrosis, providing insights into the extent of lung damage. Additional parameters measuring lung function, such as inspiratory capacity (IC), static compliance (Cst), and compliance (Crs), displayed critical reductions compared with healthy mice, whereas tissue elastance (H) showed a significant increase (Fig. 8F). Remarkably, following the administration of inhaled n-PN/p-LP@aero-μGel, significant improvements were observed in the measured lung parameters, confirming therapeutic efficacy.
Fig. 8.
(A) Representative images of immunofluorescence (IF) of DAPI (blue), α-SMA (green), collagen I (red), and immunohistochemistry (IHC) staining of TGF-β (bottom) in lung tissue of G1–G6. (B) Total cell count in BALF. (C) Evaluation of the TGF-β level in BALF of each group using TGF-β assay. *p < 0.01 and **p < 0.05 over G3/G4 and G4, respectively. (D) Western blot analysis and (E) quantitative determination of α-SMA, collagen I, and fibronectin expression in lung tissues in each group. *p < 0.001 over G3. (F) Quantification of resistance (Rrs), elastance (Ers), inspiratory capacity (IC), static compliance (Cst), compliance (Crs), and tissue elastance (H) in the pulmonary function tests of G1, G2, and G6. P-value was calculated by the unpaired Student's t-test in (F). *p < 0.05, **p < 0.01, ***p < 0.001.
These results demonstrate remarkable antifibrotic efficacy of twice-weekly inhalation formulation of n-PN/p-LP@aero-μGel (total doses: 8 mg NT/kg/week + 30 mg PF/kg/week) in a bleomycin-induced pulmonary fibrosis mouse model. The overall efficacy results of n-PN/p-LP@aero-μGel were very similar to those of once-daily combined nanoparticle formulation of n-PN/p-LP (total doses: 28 mg NT/kg/week + 105 mg PF/kg/week), which was 3.5-time greater than the drug doses. This enhanced efficacy might be attributed to prolonged deposition by evading alveolar macrophage phagocytosis and sustained drug release under μGel protection without rapid clearance and systemic entrance of individual NPs (PLGA NPs + liposomes). This stable elongated local delivery of intratracheally aerosolized n-PN/p-LP@aero-μGel produced enhanced in vivo antifibrotic efficacy with reduced frequency of administration. Furthermore, our inhalation μGel formulation may have a clinical advantage over commercial oral formulations of antifibrotic drugs due to significantly lower dose and reduced dosing frequency. Actual oral doses of NT and PF are 35 mg/kg/week twice daily and 210–700 mg/kg/week thrice daily, respectively [[56], [57], [58], [59]]. To reduce the side effects caused by high-doses and frequency dosing, co-administration of these two drugs is considered to be clinically promising, and this approach has been shown in the clinical phase [18,19,60]. Likewise, the pulmonary co-administration of nintedanib and pirfenidone by using our nanoparticles-containing microgels may reduce the relevant side effects. Despite many other considerations, we believe that our aerosolizable microgels would be a good prototype of long-lasting sustained inhalation formulation with prolonged efficacy for lung diseases. Additionally, there were no signs of in vivo systemic toxicity in the treated mice after inhalation of n-PN/p-LP@aero-μGel: the histologies of liver, spleen, kidney and heart for G6 mice were not significantly different from those of control G1 mice after the entire experiment (21 days) (Fig. S11). Furthermore, all hematology and blood biochemical parameter values, e.g., WBC, AST, ALB, BUN and HGB etc., were not statistically different between G1 and G6, indicating negligible systemic toxicity of our μGel consisting of HSA, PEG, PLGA and lipids, which are FDA-approved materials (Fig. S12). These results might indicate that PN/p-LP@aero-μGel would be considered to be a biocompatible and safe inhalation agent in those contexts.
3. Conclusion
In summary, we successfully fabricated aerosolizable μGels, approximately 12 μm in size, with incorporated NT-loaded PLGA NPs and PF-loaded liposomes for prolonged lung retention and antifibrotic efficacy. Data on in vitro macrophage uptake and in vivo lung deposition demonstrated that our aerosolizable μGels are resistant to engulfment by alveolar macrophages and are retained much longer than other formulations, which significantly protects the inner-entrapped NT and PF as well as PLGA NPs and liposomes. This advantage is attributed to the macrophage phagocytosis-bypassing effect of the μGel size (12 μm), extending the residence time in the lungs and reducing the frequency of drug administration. Interestingly, n-PN/p-LP@aero-μGel significantly attenuated the progression of IPF by promoting TGF-β inhibition and myofibroblast deactivation, leading to lung function restoration and a reduction in the immune cell population. Importantly, we also considered the biocompatibility and biodegradability of the final inhalation formulation of our μGels. Because the respiratory tract and the lungs are involved in breathing and vulnerable to toxicity issues, our μGels consist of FDA-approved clinical materials, such as PEG, albumin, PLGA, and lipids. Taken together, our results validate the prototype of a biocompatible aerosolizable μGel platform as an inhalation delivery system for improved treatment of pulmonary fibrosis.
4. Materials and methods
4.1. Materials
NT and PF were obtained from MedChem Express (Monmouth Junction, NJ, USA). Bleomycin sulfate was obtained from Dong-A Socio Holdings Co., Ltd. (Seoul, Korea). HSA was from Sigma-Aldrich (St. Louis, MO, USA). 1,2-Dioleoyl-sn-Glycero-3-Phosphocholine (DOPC); 1,2-distearoyl-sn-glycero-3-phosphoethanolamine-N-[methoxy(polyethylene glycol)-2000] (DSPE-PEG2000); and cholesterol were from Avanti polar lipids (Alabaster, AL, USA). PLGA (RG502, Mw: 7000–17,000; lactic acid: glycolic acid, 50:50) was from Boehringer-Ingelheim (Ingelheim, Germany). Four-arm PEG succinimidyl ester (4-arm PEG-NHS; Mw 20 kDa) was purchased from NOF Corporation (Tokyo, Japan); and 1,1′-dioctadecyl-3,3,3′,3′-tetramethylindotricarbocyanineiodide (DiR) and 1,1′-dioctadecyl-3,3,3′3′ tetramethylindocarbocyanine perchlorate (DiI) were from Invitrogen (Waltham, MA, USA); Cy5.5 NHS ester dye was from GE Healthcare (Piscataway, NJ, USA). SY-Glyster CR-310 (TGCR) was kindly provided by Sakamoto Yakuhin Kogyo Co. (Osaka, Japan). A549 and J774A.1 cells were obtained from the American Type Culture Collection (ATCC; Rockville, MD, USA). RAW264.7 and NIH/3T3 cells were from the Korean Cell Line Bank (Seoul, Korea). Alexa-Fluor®-488-conjugated goat-anti-rabbit secondary antibodies and Alexa-Fluor®-647-conjugated goat-anti-mouse secondary antibodies were from Abcam (Cambridge, MA, USA). High-glucose Dulbecco's modified Eagle's medium (DMEM), Roswell Park Memorial Institute (RPMI) medium, fetal bovine serum (FBS), were from Capricorn (Ebsdorfergrund, Hesse, Germany); and trypsin-EDTA and penicillin-streptomycin solutions were from Corning (Corning, NY, USA). Antibodies for α-SMA (ab5694), TGF-β (ab215715), E-cadherin (ab231303), and vimentin (ab92547) were from Abcam. Collagenase D and DNase I were from Roche (Basel, Switzerland). GAPDH polyclonal antibody (bs-04591R), goat anti-rabbit IgG antibody (H + L)-HRP conjugated (bs-0295G-HRP), and collagen I (bs-10423R) were obtained from Bioss (MA, USA). APC anti-mouse CD206 (clone C068C2, Catalog: 141708), FITC anti-mouse CD11b (clone M1/70, Catalog: 101206), PE anti-mouse F4/80 (clone: BM8, Catalog: 123110), and TruStain FcX anti-mouse CD16/32 (clone: S17011E, Catalog: 156604) were from BioLegend (San Diego, CA, USA). All other reagents, unless otherwise specified, were purchased from Sigma-Aldrich.
4.2. Cell cultures and animals
NIH/3T3 fibroblast cells were incubated in a high-glucose DMEM medium containing 10 % bovine calf serum (BCS) and 1 % antibiotics (penicillin−streptomycin, 10,000 U/mL) in a humidified atmosphere of 5 % CO2 at 37 °C. RAW264.7 and J774A.1 cells were incubated in high-glucose DMEM medium containing 10 % FBS and 1 % antibiotics (penicillin−streptomycin, 10,000 U/mL) in a humidified atmosphere containing 5 % CO2 at 37 °C. A549 epithelial cells were incubated in RPMI medium containing 10 % FBS and 1 % antibiotics (penicillin−streptomycin, 10,000 U/mL) in a humidified atmosphere containing 5 % CO2 at 37 °C. The C57BL/6 mice (male, 7 weeks old) were purchased from Orient Bio (Seongnam, Korea). Animal care strictly followed the guidelines issued by the National Institute of Health (NIH publication 80−23, revised in 1996). Mice were maintained in a controlled 12-h/12-h light/dark cycle (lights on at 8:00 a.m.). All animal experiments were conducted under complete review and approval of the Institutional Animal Care and Use Committee (IACUC) of Sungkyunkwan University (IACUC No. 202206021 and 202305041, approval dates - 22 July 2022 and 12 May 2023).
4.3. Preparation of nintedanib-loaded PLGA NPs and pirfenidone-loaded liposomes
Nintedanib-loaded PLGA NPs (n-PN) were prepared by a modified nanoprecipitation method [61,62]. Briefly, PLGA (90 mg) and NT (2 mg) were dissolved in 4 mL acetone in an ultrasonic bath for 15 min. The polymer/drug solution was injected into 60 mL of 1 % PVA solution at a flow rate of 0.5 mL/min using an autoinjector (KDS 200, KD Scientific, Korea). A simple magnetic stirrer was used during the injection at 600 rpm. Residual solvent was removed using magnetic stirring under a fume hood for 24 h. The resulting NPs were collected by centrifugation at 10,000 rpm for 5 min and washed three times with distilled water [61]. To prepare PF-loaded liposomes (p-LP), the thin-film hydration method was chosen. The p-LP were prepared using DOPC:cholesterol:DSPE-PEG2000 (mass ratio of 32:15:3) dissolved in chloroform. Chloroform and methanol were mixed at a volume ratio of 3:1 and evaporated with a rotary evaporator at room temperature for 3 h. The dried thin film was hydrated with PF in phosphate buffer (pH 7.4) and sonicated at 25 °C for 10 min to produce a clear liposome solution. The liposome solution was further centrifuged at 16,000×g for 15 min at 4 °C to remove any uncontained drug. After centrifugation, the liposome sample was extruded by filter membranes in the order of 400 nm, 200 nm, and 100 nm to achieve unilamellar liposomes. The prepared liposomes were stored at 4 °C for further experiments.
4.4. Characterization of n-PN and p-LP
The hydrodynamic sizes and the zeta potentials of the p-LP and n-PN were measured using DLS (Zetasizer Nano ZS90, Malvern Instruments, Worcestershire, UK) with a 633 nm He–Ne laser beam and a fixed 90° scattering angle. The surface morphology of the NPs was observed by TEM with a JEM-3010 (JEOL, Tokyo, Japan) and field-emission (FE)-SEM using a JSM7000F (JEOL). The physical stability of the NPs was evaluated at room temperature considering the stability of the particle size. Briefly, the particle sizes of the p-LP and n-PN were monitored for 72 h using the DLS method described above.
4.5. Release profile and encapsulation efficiency of n-PN and p-LP
For measuring the amounts of PF and NT in p-LP and n-PN, respectively, lyophilized liposomes were dissolved in acetonitrile (ACN). Loading efficiency and capacity of PF were measured by reverse-phase high-performance liquid chromatography (RP-HPLC) using a PLRP-S Zorbax 100 RP-18 column (150 × 4.6 mm, 8 μm/300 Å; Agilent Technologies, Palo Alto, CA, USA). The isocratic elution method was conducted at a flow rate of 1.0 mL/min using a mixed solution (DW:ACN = 70:30). The NT loading efficiency and capacity were measured by UV-Vis-NIR using a Synergy™ NEO microplate reader (Bio Tek, Winooski, VT, USA). Drug loading efficiency was calculated as follows: Drug loading efficiency = mass of drugs in liposomes or PLGA NPs/mass of drugs used in formulation × 100 %.
The drug release experiment was conducted with a dialysis tube at 37 °C and pH 7.4, with only 0.02 % (v/v) Tween 80 added to the liposome release beaker. The amount of drug released was measured at 0, 1, 2, 4, 8, 12, 18, 24, 48, and 72 h with HPLC/UV-absorbance.
4.6. Preparation of inhalable n-PN/p-LP@μGel
Human serum albumin (HSA)-based μGels were fabricated by a slight modification of a previous method using a homogenizer W/O emulsification [46]. Briefly, dispersed and continuous phases were 0.5 mL mixture solutions of HSA, n-PN, and 4-arm PEG-NHS (80, 8, and 8.5 mg, respectively) and of 25 mL kerosene with 2 % TGCR. Specifically, HSA and n-PN were thoroughly dispersed in 0.5 mL of 10 mM PBS (pH 7.4), and the dispersed solution was then allowed to mix with 4-arm PEG-NHS before the emulsification. The mixing sequence was kept to enhance the n-PN incorporation into the μGel, preventing rapid gelation before entrapping n-PN.
The mixture was emulsified using a homogenizer at 8500 rpm, 37 °C, 5 min. The resulting W/O emulsion containing HSA, n-PN, and 4-arm PEG-NHS liquid microdroplets was mixed with 5.2 μL 50 % glutaraldehyde solution (final concentration of 0.01 v/v%) and stirred at 600 rpm for 3 h for cross-linking. The reaction was quenched by milled glycine (final concentration, 0.05 M) for 30 min. The resulting mixture was centrifuged at 6108×g and washed 3 times with 10 mM PBS containing 0.02 % Tween 80 and 50 % ethanol. Pellets were finally washed with DW, and the resulting microgel solution was briefly filtered through a 10–15 μm mesh strainer to remove μGels of the incorrect size and further lyophilized with 3 % d-(+)-trehalose dihydrate to prevent aggregation during the lyophilization step. To immerse the p-LP, a portion (30 mg) of the freeze-dried microgels was dispersed in the p-LP solution at 250 rpm for 2 h. The resulting n-PN/p-LP@μGel was briefly centrifuged at 4000 rpm for 2 min. The supernatant was removed, and the μGels were washed 3 times with PBS and stored at 4 °C for further experiments.
4.7. Characterization of inhalable n-PN/p-LP@μGel
The μGels were characterized using various analytical instruments [46]. The following materials were used for visualization by confocal microscopy (CLSM; LSM510, Carl Zeiss, Jena, Germany). HSA-Chlorin e6 (excitation/emission wavelengths of 683/703 nm) was used instead of HSA when making μGel; in the case of PLGA and liposome, Coumarine-6 (360/447 nm) and DiI (549/565 nm) were used, respectively. Surface morphology was examined by FE-SEM (JSM7500F, JEOL Ltd.). Cross-sectional naïve μGel, p-LP@μGel, n-PN@μGel, and n-PN/p-LP@μGel samples were prepared by focused ion beam (FIB) (JIB-4601 F, JEOL Ltd.) and analyzed by FE-SEM. All μGel samples were lyophilized for 2 days before analysis.
4.8. Cell viability
Cytotoxic effects of drugs and NPs against A549 (lung epithelial cell line) and NIH/3T3 cells (fibroblast cell line) were assessed using a 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT)-based assay. Both cell lines were seeded at 1 × 104 cells/well in 96-well plates and incubated overnight. After replacing the cell culture medium with TGF-β (final concentration: 10 ng/mL), cells were treated with NT, PF, p-LP, and n-PN at different concentrations for 48 h. Cells without NT, PF, or p-LP and n-PN treatment were used as a control. After 48 h, free drug and NP solutions were removed from the plates by washing with d-PBS. Cell viability was analyzed using an MTT assay.
4.9. Wound healing assay
A549 cells were seeded onto an SPLScar™ Block at a concentration of 1 × 105 cells per well [63]. After incubation for 2–3 h, the blocks were removed to produce 500 μm gaps to simulate wounds. Serum-free media was used for 12 h. Then, after incubation with a complete medium containing TGF-β (final concentration: 10 ng/mL) for 1 h, each treatment (final concentration: NT 10 μM, PF 50 μM) was applied. Images of cells invading the gaps were captured at predetermined time points using microscopy.
4.10. Cell morphology
A549 cells were seeded onto 8-well plates at a concentration of 1.5 × 104 cells per well. After incubation overnight, serum-free media was used for 12 h. Next, after induction with a complete medium containing TGF-β (final concentration: 10 ng/mL) for 1 h, each treatment (final concentration: NT 10 μM, PF 50 μM) was applied. After incubating for 48 h, the cells were imaged using a microscope to capture changes in cell morphology.
4.11. Cell migration assay in a transwell system
The migration ability of fibroblasts was determined using Boyden chamber assays. NIH/3T3 fibroblast cells were seeded into 6-well culture plates. When the cells were ∼50 % confluent, they were starved for 24 h in serum-free medium. TGF-β (final concentration: 10 ng/mL) and then each treatment (final concentration: NT 10 μM, PF 50 μM) was added to the culture media. Cells were incubated at 37 °C for 24 h and washed with PBS 3 times. The cells were then detached using 0.25 % trypsin-EDTA, pelleted at 400×g for 5 min, and resuspended at a density of 2.5 × 105 cells/mL using serum-free culture media. Then, 200 μL of the cell suspensions (5 × 104 cells) was added to the Transwell insert, and 800 μL of complete culture media was added to the lower chamber. After an 8 h incubation period, the cells were fixed in methanol and stained for 30 min at room temperature with a 1 % crystal violet solution. Cotton swabs were used to remove non-migratory cells. Migratory cells from three non-overlapping fields per membrane were photographed and counted.
4.12. Gel contraction assay
The 3T3 cells were harvested and resuspended in a complete medium at 2 × 106 cells/mL. The cell contraction matrix was prepared by mixing 2 parts of the cell suspension with 8 parts of cold collagen gel working solution. Then, 0.5 mL of the cell contraction matrix was added to each well of the 24-well cell contraction plate. The plate was incubated at 37 °C and 5 % CO2 for 1 h. After collagen polymerization, 1 mL of culture medium was added to the top of each collagen gel lattice. TGF-β (final concentration: 10 ng/mL) and each treatment (final concentration: NT 10 μM, PF 50 μM) were added to the culture medium. The wells were monitored for contraction over 2 days at 37 °C and 5 % CO2. Media was changed daily by removing 0.5 mL and replacing it with 0.5 mL of fresh media. The collagen gel size change was measured over time and at set endpoints.
4.13. Immunofluorescence
The 3T3 and A549 cells were cultured in DMEM and RPMI media, respectively, containing 10 % (v/v) FBS or 10 % (v/v) BCS 1 % penicillin/streptomycin in a 5 % CO2, 95 % RH incubator at 37 °C. The 3T3 and A549 cells (both 1500 cells per well) were seeded into v-bottom cell plates (Shimadzu, Kyoto, Japan) designed to induce the formation of 3D multicellular spheroids. Spheroids were transferred to 96-well plates with a flat bottom. TGF-β (final concentration: 10 ng/mL) and each treatment (final concentration: NT 10 μM, PF 50 μM) were added. After 48 h, spheroids were washed with PBS and plated in each well of an 8-well chamber (Ibidi, Martinsried, Germany). The spheroids were fixed with 4 % formaldehyde for 10 min and allowed to incubate for 5 min with 0.1 % Triton x-100 and then washed 3 times with PBS. The resulting cell spheroids were incubated with a blocking solution (1 % BSA, 22.52 mg/mL glycine in PBST [PBS containing 0.1 % Tween 20]) for 0.5 h. Next, anti-α-SMA and anti-collagen type I primary antibodies (diluted 3:500, 1:99, respectively, in PBST with 1 % BSA) were added, and the mixtures were incubated overnight in a humidified chamber at room temperature. The spheroids were washed three times in PBS and incubated with both Alexa-Fluor®-488 (anti-rabbit)/-647 (anti-mouse)-conjugated secondary antibodies (diluted 1:600 in 1 % BSA) at room temperature in the dark for 2 h. The secondary antibody solution was removed, and the spheroids were washed 3 times with PBS. After incubation with DAPI (to stain DNA) for 2 h and rinsing with PBS, the spheroids were visualized using CLSM (Carl Zeiss, Jena, Germany). The experiments also were conducted in 2D using E-cadherin primary antibodies (E-cadherin diluted 1:200) and secondary antibodies (Alexa-488 diluted 1:400).
4.14. Cellular uptake of nanoparticles and microgels
RAW264.7 and J774A.1 cells (1.0 × 104 cells) were seeded into an 8-well chamber (Ibidi, Martinsried, Germany) and incubated overnight. Then, cells were incubated with three sizes of μGels for time-lapse at 37 °C and 5 % CO2 for 12 h. The other DiR-liposome, Coumarine-6 PLGA, was also incubated. After a predetermined time, the cells were washed twice to remove extracellular NPs, and the nuclei were stained for 30 min using Hoechst. The time-lapse videos for μGels of 6, 12 and 18 μm were obtained by confocal laser scanning microscopy (Carl Zeiss).
4.15. In vivo biodistribution and ex vivo fluorescent imaging
The in vivo localization of our manufactured n-PN/p-LP@μGel, p-LP, and n-PN in mice and the images of lungs dissected from mice were visualized using an in vivo imaging system (FOBI in vivo imaging system, NeoScience, Korea, and IVIS Lumina XR Spectrum, PerkinElmer, Waltham, MA, USA). To evaluate the lung deposition of n-PN/p-LP@μGel, p-LP, and n-PN, 50 μL aliquots of different sized Cy5.5-conjugated μGels (5 mg), DiR-loaded liposomes (5 mg), and coumarin 6-loaded PLGA NPs (5 mg) were directly aerosolized into the trachea of C57BL/6 mice using a model IA-1C-M micro-spray aerosolizer (Penn-Century, Inc., Philadelphia, PA, USA). At predetermined times after inhalation (0, 1, 2, 4, 8, 12, 18, 24, 48, and 72 h), mice were sacrificed and their lungs were excised.
4.16. Anti-fibrosis efficacy using a bleomycin-induced pulmonary fibrosis mouse model
Pulmonary fibrosis was induced using a slight modification of bleomycin-induction protocols published previously [3,35]. Aliquots (25 μL) of bleomycin sulfate solution in saline were individually sprayed into the trachea of 8-week-old C57BL/6 male mice weighing 3.5 mg/kg. Mice were anesthetized with a single intraperitoneal (i.p.) injection of pentobarbital (7.5 mg/kg) or Avertin (200 mg/kg). Control mice received 25 μL of saline; G1, negative control-PBS; G2, positive control-bleomycin (3.5 mg/kg); G3, NT-loaded PLGA NPs (n-PN; 4 mg/kg/day) for 7 days; G4, PF-loaded liposomes (p-LP; 15 mg/kg/day) for 7 days; G5, NT-loaded PLGA NP + PF-loaded liposomes (n-PN/p-LP; 4 mg/kg/day+15 mg/kg/day) for 7 days; G6, NT-loaded PLGA NP + PF-loaded liposome@ μGel (n-PN/p-LP@μGel, 4 mg/kg/day+15 mg/kg/day) for 2 days. To confirm the antifibrotic efficacy of our formulations, we carried out the following measurements and experiments: mouse body weight, survival rate, histology (H&E, MT assay), Ashcroft score, hydroxyproline assay, Micro-CT scanning, lung index, FACS analysis for M2 macrophages, immunofluorescence visualization for α-SMA/collagen I, BALF cell counting, TGF-β assay, western blotting, Flexivent™ lung function, hematology analysis, and blood biochemical assay. The methods for the respective experiments are described elsewhere in detail.
4.17. Histology
The lungs were inflated through the trachea with 4 % paraformaldehyde for a few minutes before fixing with 4 % paraformaldehyde for 24 h at room temperature. Fixed lung tissues and major organs (liver, kidney heart, and spleen) were embedded in paraffin and cut into 4 μm sections for H&E and MT staining. Based on the histology, the severity of pulmonary fibrosis in each group was rated from 0 to 8 according to the Ashcroft scale: 0, normal lung; 1, minimal fibrous thickening of alveolar or bronchiolar walls; 3, moderate thickening of walls without obvious damage to lung architecture; 5, increased fibrosis with definite damage to lung structure and formation of fibrous bands or small fibrous masses; 7, severe distortion of structure and large fibrous areas, including “honeycomb lung”; 8, total fibrous obliteration of the field [64].
4.18. Hydroxyproline assay
Lung tissues from the IPF-induced mouse group were homogenized to measure collagen content using a hydroxyproline (HYP) assay kit (BioVision Inc., Milpitas, CA, USA) with slight modification of method described previously [3]. Briefly, the right side of the lung was homogenized in DW (10 mg lung tissue/200 μL DW). Then, 100 μL of homogenized solution was mixed with 12 N 100 μL of HCl and hydrolyzed at 120 °C for 3 h. The resultant solutions were centrifuged at 14,500 rpm for 20 min, and supernatant (10 μL) was transferred to a 96-well plate. Chloramine-T reagent (100 μL) was added to each sample and incubated at room temperature for 5 min. Then, dimethyl aminobenzaldehyde (DMAB) reagent (100 μL) was mixed into each sample and incubated at 60 °C for 90 min. The absorbance of each sample was measured at a 560 nm wavelength using a microplate reader.
4.19. Micro-CT
A micro-CT scan was conducted using a Quantum GX2 micro-CT Imaging System (PerkinElmer) using the following parameters: 90 kV, 88 μA, and pixel size of 72 μm. The volume was calculated with Analyze 12.0 software (PerkinElmer). To minimize inter-specimen variations, identical settings were used for the analysis of all images.
4.20. Flow cytometry
The collected fresh lung tissues were cut into pieces, digested with collagenase D (1.5 mg/mL) and DNase 1 (0.1 mg/mL) at 37 °C for 20 min, and treated with red blood cell (RBC) lysis buffer at 4 °C for 5 min to remove the RBCs. To block nonspecific binding, cell suspensions were stained by anti-mouse CD16/CD32 (1 μg/mL) and then co-stained with the corresponding antibody for quantitative evaluation of M2 macrophages by flow cytometry. The described experiment was conducted exclusively in the G1, G2, and G6 groups.
4.21. Bronchoalveolar lavage fluid
A 21G catheter was inserted into the mouse trachea, and the lung was filled and aspirated three times with 0.5 mL of EDTA containing PBS. This step was repeated 3 times to obtain 1.5–1.7 mL of BALF. The merged bronchoalveolar lavage fluids were centrifuged at 400×g for 8 min at 4 °C, and the supernatants were collected and frozen for further TGF-β ELISA. The remaining BALF cell precipitates were resuspended in 1 mL PBS for total cell counting.
4.22. SDS-PAGE and Western blot analysis
Cells from in vivo lung tissues and in vitro monolayer were lysed with RIPA buffer (89900; Thermo Fisher Scientific, Waltham, MA, USA) and 1 mM of PMSF at 2–8 °C. Total protein concentration was determined using a BCA protein assay kit (Thermo Fisher Scientific). Protein samples were separated by SDS-PAGE in 12 % acrylamide gel at a voltage of 100 mV and were transferred to PVDF membranes at 110 mV for 2 h. All SDS-PAGE and transfer processes were performed with a Mini-PROTEAN Tetra Vertical Electrophoresis Cell (Bio-Rad, Hercules, CA, USA). To block the membranes, 2.5 g of skim milk powder was dissolved in 50 ml of 0.1 % TBS-T to produce a 5 % blocking solution, and then the membranes were incubated with this solution for 1 h at room temperature. Then, the membranes were washed 5 times for 10 min each using 0.1 % TBS-T and were incubated with the corresponding primary antibody overnight at 4 °C. Antibodies were diluted in blocking solution as per the manufacturer's instructions. After washing the primary antibody in the same way as the blocking solution, the secondary antibody was incubated with the membrane for 1 h at room temperature. Finally, the membrane was processed using a mixture of peroxide solution and luminol/enhancer solution for 5 min to analyze in a ChemiDoc™ Imaging System (Bio-Rad).
4.23. Pulmonary function test
The experimental animals were anesthetized by intraperitoneal injection of pentobarbital and were intubated with a 21G cannula. The test was performed using a FlexiVent system (SCIREQ, Canada). The described experiment was exclusively conducted in the G1, G2, and G6 groups.
4.24. Hematology analysis and blood biochemical assay
A dose (25 μL) of n-PN/p-LP@μGel was intratracheally injected into mice (n = 3). Blood was collected on day 21 for hematology analysis and blood biochemical assays. Each biological marker provided physiological information. Albumin (ALB) is a protein in blood plasma made by the liver, and aspartate aminotransferase (AST) is an enzyme mainly present in the heart and liver. Both ALB and AST are used to detect liver damage. Blood urea nitrogen (BUN) is produced when protein breaks down in the body. A healthy kidney removes >90 % of BUN produced in the body; thus, the urea nitrogen concentration in the blood shows how well the kidney is functioning. Creatinine (CREA) is a waste product produced by muscle from the decomposition of creatine. Since almost all CREA is excreted through the kidneys, its blood level is a good indicator of kidney function. Total bilirubin (TBIL) is a purple pigment in bile that is used to screen and monitor liver disease. White blood cell count (WBC) measures the number of white blood cells in whole blood, an RBC count measures the number of RBCs in whole blood, and hematocrit (HCT) is a measure of the ratio of RBCs in the blood. Platelets (PLT) are used as an indication of bleeding disease or bone marrow disease. Hemoglobin (HGB) is an indication of anemia or erythropoiesis. Mean corpuscular volume (MCV) is the average volume of 1 RBC, mean corpuscular HGB (MCH) is the average amount of HGB contained in 1 RBC, and mean corpuscular HGB concentration (MCHC) is the average concentration of HGB in RBCs. MCV, MCH, and MCHC are used for diagnosis of anemia.
Ethics approval and consent to participate
Animals were cared for in accordance with the National Institutes of Health's Guide for the Care and Use of Laboratory Animals. Protocols were also approved by the Institutional Animal Care and Use Committee (IACUC) of Sungkyunkwan University (IACUC No. 202206021 and 202305041, approval date - 22 July 2022 and 12 May 2023). All animal experiments were conducted under the complete review.
CRediT authorship contribution statement
Woo Tak Lee: Data curation, Formal analysis, Methodology, Validation, Writing – original draft, Writing – review & editing. Hyunjun Lee: Data curation, Formal analysis, Methodology, Validation. Juho Kim: Data curation, Formal analysis, Methodology, Validation. Yujin Jung: Investigation. Eojin Choi: Investigation. Ji Hoon Jeong: Project administration. Jee-Heon Jeong: Project administration. Jung Heon Lee: Project administration. Yu Seok Youn: Conceptualization, Data curation, Funding acquisition, Supervision, Writing – original draft, Writing – review & editing, Project administration.
Declaration of competing interest
The authors declare that they have no competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT; No. NRF-2019R1A5A2027340) and by the Bio & Medical Technology Development Program of the NRF funded by the Korean government (MSIT; No. NRF-2022M3A9G8017220). Some parts of the schematic illustrations in Scheme1, Figs. 1, 3, 4 and 6 were created with BioRender.com.
Footnotes
Peer review under responsibility of KeAi Communications Co., Ltd.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bioactmat.2023.11.005.
Appendix A. Supplementary data
The following are the Supplementary data to this article.
References
- 1.Kim D.S., Collard H.R., King T.E., Jr. Classification and natural history of the idiopathic interstitial pneumonias. Proc. Am. Thorac. Soc. 2006;3(4):285–292. doi: 10.1513/pats.200601-005TK. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moore B.B., Hogaboam C.M. Murine models of pulmonary fibrosis. Am. J. Physiol. Lung Cell Mol. Physiol. 2008;294(2):L152–L160. doi: 10.1152/ajplung.00313.2007. [DOI] [PubMed] [Google Scholar]
- 3.Seo J., Lee C., Hwang H.S., Kim B., Thao L.Q., Lee E.S., Oh K.T., Lim J.-L., Choi H.-G., Youn Y.S. Therapeutic advantage of inhaled tacrolimus-bound albumin nanoparticles in a bleomycin-induced pulmonary fibrosis mouse model. Pulm. Pharmacol. Ther. 2016;36:53–61. doi: 10.1016/j.pupt.2016.01.001. [DOI] [PubMed] [Google Scholar]
- 4.Wijsenbeek M. Progress in the treatment of pulmonary fibrosis. Lancet Respir. Med. 2020;8(5):424–425. doi: 10.1016/S2213-2600(20)30062-X. [DOI] [PubMed] [Google Scholar]
- 5.Mann J., Goh N.S.L., Holland A.E., Khor Y.H. Cough in idiopathic pulmonary fibrosis. Front. Rehabil. Sci. 2021;2:1–12. doi: 10.3389/fresc.2021.751798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.U.S. Food and Drug Administration . Food and Drug Administration's (FDA's) Patient-Focused Drug Development Initiative for Idiopathic Pulmonary Fibrosis. 2015. Center for drug evaluation and research (cder), the voice of the patient: a series of reports from the U.S.www.fda.gov/downloads/ForIndustry/UserFees/PrescriptionDrugUserFee/UCM440829.pdf accessed March 2015. [Google Scholar]
- 7.Amin B.J.H., Kakamad F.H., Ahmed G.S., Ahmed S.F., Abdulla B.A., Mohammed S.H., Mikael T.M., Salih R.Q., Ali R.K., Salh A.M., Hussein D.A. Post COVID-19 pulmonary fibrosis; a meta-analysis study. Ann. Med. Surg. (Lond.) 2022;77 doi: 10.1016/j.amsu.2022.103590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.John A.E., Joseph C., Jenkins G., Tatler A.L. COVID-19 and pulmonary fibrosis: a potential role for lung epithelial cells and fibroblasts. Immunol. Rev. 2021;302(1):228–240. doi: 10.1111/imr.12977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rivera-Ortega P., Hayton C., Blaikley J., Leonard C., Chaudhuri N. Nintedanib in the management of idiopathic pulmonary fibrosis: clinical trial evidence and real-world experience. Ther. Adv. Respir. Dis. 2018;12:1–13. doi: 10.1177/1753466618800618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shah P.V., Balani P., Lopez A.R., Nobleza C.M.N., Siddiqui M., Khan S. A review of pirfenidone as an anti-fibrotic in idiopathic pulmonary fibrosis and its probable role in other diseases. Cureus. 2021;13(1):1–8. doi: 10.7759/cureus.12482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Takeda Y., Tsujino K., Kijima T., Kumanogoh A. Efficacy and safety of pirfenidone for idiopathic pulmonary fibrosis. Patient Prefer. Adherence. 2014;8:361–370. doi: 10.2147/PPA.S37233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grimminger F., Gunther A., Vancheri C. The role of tyrosine kinases in the pathogenesis of idiopathic pulmonary fibrosis. Eur. Respir. J. 2015;45(5):1426–1433. doi: 10.1183/09031936.00149614. [DOI] [PubMed] [Google Scholar]
- 13.Wollin L., Wex E., Pautsch A., Schnapp G., Hostettler K.E., Stowasser S., Kolb M. Mode of action of nintedanib in the treatment of idiopathic pulmonary fibrosis. Eur. Respir. J. 2015;45(5):1434–1445. doi: 10.1183/09031936.00174914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Surber M.W., Pham S. 2019. https://patents.justia.com/patent/11123290/ (Specially Formulated Compositions of Inhaled Nintedanib and Nintedanib Salts). [Google Scholar]
- 15.Montgomery A., Otto K., Khoo J., Glaspole I. Late Breaking Abstract - Phase 1 dose escalation study of aerosolized pirfenidone in normal healthy volunteers (NHV), smokers, and IPF patients. 2018;52(suppl 62):OA266. doi: 10.1183/13993003.congress-2018.OA266. [DOI] [Google Scholar]
- 16.Andrade da Silva L.H., Vieira J.B., Cabral M.R., Antunes M.A., Lee D., Cruz F.F., Hanes J., Rocco P.R.M., Morales M.M., Suk J.S. Development of nintedanib nanosuspension for inhaled treatment of experimental silicosis. Bioeng. Transl. Med. 2023;8(2) doi: 10.1002/btm2.10401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kaminskas L.M., Landersdorfer C.B., Bischof R.J., Leong N., Ibrahim J., Davies A.N., Pham S., Beck S., Montgomery A.B., Surber M.W. Aerosol pirfenidone pharmacokinetics after inhaled delivery in sheep: a viable approach to treating idiopathic pulmonary fibrosis. Pharm. Res. (N. Y.) 2019;37(1):3. doi: 10.1007/s11095-019-2732-2. [DOI] [PubMed] [Google Scholar]
- 18.Flaherty K.R., Fell C.D., Huggins J.T., Nunes H., Sussman R., Valenzuela C., Petzinger U., Stauffer J.L., Gilberg F., Bengus M., Wijsenbeek M. Safety of nintedanib added to pirfenidone treatment for idiopathic pulmonary fibrosis. Eur. Respir. J. 2018;52(2) doi: 10.1183/13993003.00230-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vancheri C., Kreuter M., Richeldi L., Ryerson C.J., Valeyre D., Grutters J.C., Wiebe S., Stansen W., Quaresma M., Stowasser S., Wuyts W.A. Nintedanib with add-on pirfenidone in idiopathic pulmonary fibrosis. Results of the INJOURNEY trial. Am. J. Respir. Crit. Care Med. 2018;197(3):356–363. doi: 10.1164/rccm.201706-1301OC. [DOI] [PubMed] [Google Scholar]
- 20.Hu G., Christman J.W. Editorial: alveolar macrophages in lung inflammation and resolution. Front. Immunol. 2019;10:1–3. doi: 10.3389/fimmu.2019.02275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee J.W., Chun W., Lee H.J., Min J.-H., Kim S.-M., Seo J.-Y., Ahn K.-S., Oh S.-R. The role of macrophages in the development of acute and chronic inflammatory lung diseases. Cells. 2021;10(4):897. doi: 10.3390/cells10040897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Joshi N., Walter J.M., Misharin A.V. Alveolar macrophages. Cell. Immunol. 2018;330:86–90. doi: 10.1016/j.cellimm.2018.01.005. [DOI] [PubMed] [Google Scholar]
- 23.Patton J.S., Byron P.R. Inhaling medicines: delivering drugs to the body through the lungs. Nat. Rev. Drug Discov. 2007;6(1):67–74. doi: 10.1038/nrd2153. [DOI] [PubMed] [Google Scholar]
- 24.Crapo J.D., Young S.L., Fram E.K., Pinkerton K.E., Barry B.E., Crapo R.O. Morphometric characteristics of cells in the alveolar region of mammalian lungs. Am. Rev. Respir. Dis. 1983;128(2 Pt 2):S42–S46. doi: 10.1164/arrd.1983.128.2P2.S42. [DOI] [PubMed] [Google Scholar]
- 25.Krombach F., Münzing S., Allmeling A.M., Gerlach J.T., Behr J., Dörger M. Cell size of alveolar macrophages: an interspecies comparison. Environ. Health Perspect. 1997;105(suppl 5):1261–1263. doi: 10.1289/ehp.97105s51261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Edwards D.A., Jebria A.B., Langer R. Recent advances in pulmonary drug delivery using large, porous inhaled particles. J. Appl. Physiol. 1998;85(2):379–385. doi: 10.1152/jappl.1998.85.2.379. [DOI] [PubMed] [Google Scholar]
- 27.Edwards D.A., Hanes J., Caponetti G., Hrkach J., Jebria A.B., Eskew M.L., Mintzes J., Deaver D., Lotan N., Langer R. Large porous particles for pulmonary drug delivery. Science. 1997;276(5320):1868–1872. doi: 10.1126/science.276.5320.1868. [DOI] [PubMed] [Google Scholar]
- 28.Patton J.S., Fishburn C.S., Weers J.G. The lungs as a portal of entry for systemic drug delivery. Proc. Am. Thorac. Soc. 2004;1(4):338–344. doi: 10.1513/pats.200409-049TA. [DOI] [PubMed] [Google Scholar]
- 29.Kim H., Park H., Lee J., Kim T.H., Lee E.S., Oh K.T., Lee K.C., Youn Y.S. Highly porous large poly (lactic-co-glycolic acid) microspheres adsorbed with palmityl-acylated exendin-4 as a long-acting inhalation system for treating diabetes. Biomaterials. 2011;32(6):1685–1693. doi: 10.1016/j.biomaterials.2010.10.045. [DOI] [PubMed] [Google Scholar]
- 30.Kim I., Byeon H.J., Kim T.H., Lee E.S., Oh K.T., Shin B.S., Lee K.C., Youn Y.S. Doxorubicin-loaded porous PLGA microparticles with surface attached TRAIL for the inhalation treatment of metastatic lung cancer. Biomaterials. 2013;34(27):6444–6453. doi: 10.1016/j.biomaterials.2013.05.018. [DOI] [PubMed] [Google Scholar]
- 31.Kim I., Byeon H.J., Kim T.H., Lee E.S., Oh K.T., Shin B.S., Lee K.C., Youn Y.S. Doxorubicin-loaded highly porous large PLGA microparticles as a sustained-release inhalation system for the treatment of metastatic lung cancer. Biomaterials. 2012;33(22):5574–5583. doi: 10.1016/j.biomaterials.2012.04.018. [DOI] [PubMed] [Google Scholar]
- 32.Lü J.-M., Wang X., Muller C.M., Wang H., Lin P.H., Yao Q., Chen C. Current advances in research and clinical applications of PLGA-based nanotechnology. Expert Rev. Mol. Diagn. 2009;9(4):325–341. doi: 10.1016/10.1586/erm.09.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Swierczewska M., Lee K.C., Lee S. What is the future of PEGylated therapies? Expet Opin. Emerg. Drugs. 2015;20(4):531–536. doi: 10.1517/14728214.2015.1113254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Surassmo S., Saengkrit N., Ruktanonchai U.R., Suktham K., Woramongkolchai N., Wutikhun T., Puttipipatkhachorn S. Surface modification of PLGA nanoparticles by carbopol to enhance mucoadhesion and cell internalization. Colloids Surf. B Biointerfaces. 2015;130:229–236. doi: 10.1016/j.colsurfb.2015.04.015. [DOI] [PubMed] [Google Scholar]
- 35.Lee C., Seo J., Hwang H.S., Thao L.Q., Lee S., Lee E.S., Lee E.H., Choi H.-G., Youn Y.S. Treatment of bleomycin-induced pulmonary fibrosis by inhaled tacrolimus-loaded chitosan-coated poly(lactic-co-glycolic acid) nanoparticles. Biomed. Pharmacother. 2016;78:226–233. doi: 10.1016/j.biopha.2016.01.027. [DOI] [PubMed] [Google Scholar]
- 36.Li D., Zhao A., Zhu J., Wang C., Shen J., Zheng Z., Pan F., Liu Z., Chen Q., Yang Y. Inhaled lipid nanoparticles alleviate established pulmonary fibrosis. Small. 2023;19(30) doi: 10.1002/smll.202300545. [DOI] [PubMed] [Google Scholar]
- 37.Park S., Park J.Y., Nahm J.H., Kim G., Cho Y.L., Kang W.J., Key J. Systemic delivery of nintedanib using PLGA-based discoidal polymeric particles for idiopathic pulmonary fibrosis treatment. Mater. Today Chem. 2022;26 doi: 10.1016/j.mtchem.2022.101181. [DOI] [Google Scholar]
- 38.Bhagya N., Chandrashekar K.R. Liposome encapsulated anticancer drugs on autophagy in cancer cells – current and future perspective. Int. J. Pharmacol. 2023;642 doi: 10.1016/j.ijpharm.2023.123105. [DOI] [PubMed] [Google Scholar]
- 39.Li Z., Zhang Y., Wurtz W., Lee J.K., Malinin V.S., Durwas-Krishnan S., Meers P., Perkins W.R. Characterization of nebulized liposomal amikacin (Arikace™) as a function of droplet size. J. Aerosol Med. Pulm. Drug Deliv. 2008;21(3):245–254. doi: 10.1089/jamp.2008.0686. [DOI] [PubMed] [Google Scholar]
- 40.Li Z., Perkins W., Cipolla D. Robustness of aerosol delivery of amikacin liposome inhalation suspension using the eFlow® Technology. Eur. J. Pharm. Biopharm. 2021;166:10–18. doi: 10.1016/j.ejpb.2021.05.021. [DOI] [PubMed] [Google Scholar]
- 41.Heyder J., Gebhart J., Rudolf G., Schiller C.F., Stahlhofen W. Deposition of particles in the human respiratory tract in the size range 0.005–15 μm. J. Aerosol Sci. 1986;17(5):811–825. doi: 10.1016/0021-8502(86)90035-2. [DOI] [Google Scholar]
- 42.Praphawatvet T., Peters J.I., Williams R.O., 3rd Inhaled nanoparticles-An updated review. Int. J. Pharm. 2020;587 doi: 10.1016/j.ijpharm.2020.119671. [DOI] [PubMed] [Google Scholar]
- 43.Husain M., Wu D., Saber A.T., Decan N., Jacobsen N.R., Williams A., Yauk C.L., Wallin H., Vogel U., Halappanavar S. Intratracheally instilled titanium dioxide nanoparticles translocate to heart and liver and activate complement cascade in the heart of C57BL/6 mice. Nanotoxicology. 2015;9(8):1013–1022. doi: 10.3109/17435390.2014.996192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Miller M.R., Raftis J.B., Langrish J.P., McLean S.G., Samutrtai P., Connell S.P., Wilson S., Vesey A.T., Fokkens P.H.B., Boere A.J.F., Krystek P., Campbell C.J., Hadoke P.W.F., Donaldson K., Cassee F.R., Newby D.E., Duffin R., Mills N.L. Inhaled nanoparticles accumulate at sites of vascular disease. ACS Nano. 2017;11(5):4542–4552. doi: 10.1021/acsnano.6b08551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mills N.L., Donaldson K., Hadoke P.W., Boon N.A., MacNee W., Cassee F.R., Sandström T., Blomberg A., Newby D.E. Adverse cardiovascular effects of air pollution. Nat. Clin. Pract. Cardiovasc. Med. 2009;6(1):36–44. doi: 10.1038/ncpcardio1399. [DOI] [PubMed] [Google Scholar]
- 46.Kim H., Yoon J., Kim H.K., Lee W.T., Nguyen N.T., Le X.T., Lee E.-H., Lee E.S., Oh K.T., Choi H.-G., Youn Y.S. Upconverting nanoparticle-containing erythrocyte-sized hemoglobin microgels that generate heat, oxygen and reactive oxygen species for suppressing hypoxic tumors. Bioact. Mater. 2023;22:112–126. doi: 10.1016/j.bioactmat.2022.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lai Y.-T., Sato M., Ohta S., Akamatsu K., Nakao S.-i., Sakai Y., Ito T. Preparation of uniform-sized hemoglobin–albumin microspheres as oxygen carriers by Shirasu porous glass membrane emulsification technique. Colloids Surf. B Biointerfaces. 2015;127:1–7. doi: 10.1016/j.colsurfb.2015.01.018. [DOI] [PubMed] [Google Scholar]
- 48.Ohta S., Hashimoto K., Fu X., Kamihira M., Sakai Y., Ito T. Development of human-derived hemoglobin–albumin microspheres as oxygen carriers using Shirasu porous glass membrane emulsification. J. Biosci. Bioeng. 2018;126(4):533–539. doi: 10.1016/j.jbiosc.2018.04.017. [DOI] [PubMed] [Google Scholar]
- 49.Sun H.W., Feigal R.J., Messer H.H. Cytotoxicity of glutaraldehyde and formaldehyde in relation to time of exposure and concentration. Pediatr. Dent. 1990;12(5):303–307. [PubMed] [Google Scholar]
- 50.Kalluri R., Weinberg R.A. The basics of epithelial-mesenchymal transition. J. Clin. Investig. 2009;119(6):1420–1428. doi: 10.1172/JCI39104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Radisky D.C. Epithelial-mesenchymal transition. J. Cell Sci. 2005;118(19):4325–4326. doi: 10.1242/jcs.02552. [DOI] [PubMed] [Google Scholar]
- 52.Chikaura H., Nakashima Y., Fujiwara Y., Komohara Y., Takeya M., Nakanishi Y. Effect of particle size on biological response by human monocyte-derived macrophages. Biosurf. Biotribol. 2016;2(1):18–25. doi: 10.1016/j.bsbt.2016.02.003. [DOI] [Google Scholar]
- 53.Champion J.A., Walker A., Mitragotri S. Role of particle size in phagocytosis of polymeric microspheres. Pharm. Res. (N. Y.) 2008;25:1815–1821. doi: 10.1007/s11095-008-9562-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Evren E., Ringqvist E., Willinger T. Origin and ontogeny of lung macrophages: from mice to humans. Immunology. 2020;160(2):126–138. doi: 10.1111/imm.13154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Petros R.A., DeSimone J.M. Strategies in the design of nanoparticles for therapeutic applications. Nat. Rev. Drug Discov. 2010;9(8):615–627. doi: 10.1038/nrd2591. [DOI] [PubMed] [Google Scholar]
- 56.Epstein-Shochet G., Pham S., Beck S., Naiel S., Mekhael O., Revill S., Hayat A., Vierhout M., Bardestein-Wald B., Shitrit D. Inhalation: a means to explore and optimize nintedanib's pharmacokinetic/pharmacodynamic relationship. Pulm. Pharmacol. Ther. 2020;63 doi: 10.1016/j.pupt.2020.101933. [DOI] [PubMed] [Google Scholar]
- 57.Wollin L., Maillet I., Quesniaux V., Holweg A., Ryffel B. Antifibrotic and anti-inflammatory activity of the tyrosine kinase inhibitor nintedanib in experimental models of lung fibrosis. J. Pharmacol. Exp. Therapeut. 2014;349(2):209–220. doi: 10.1124/jpet.113.208223. [DOI] [PubMed] [Google Scholar]
- 58.Inomata M., Kamio K., Azuma A., Matsuda K., Kokuho N., Miura Y., Hayashi H., Nei T., Fujita K., Saito Y., Gemma A. Pirfenidone inhibits fibrocyte accumulation in the lungs in bleomycin-induced murine pulmonary fibrosis. Respir. Res. 2014;15(1):1–14. doi: 10.1186/1465-9921-15-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Oku H., Shimizu T., Kawabata T., Nagira M., Hikita I., Ueyama A., Matsushima S., Torii M., Arimura A. Antifibrotic action of pirfenidone and prednisolone: different effects on pulmonary cytokines and growth factors in bleomycin-induced murine pulmonary fibrosis. Eur. J. Pharmacol. 2008;590(1–3):400–408. doi: 10.1016/j.ejphar.2008.06.046. [DOI] [PubMed] [Google Scholar]
- 60.Wan Q., Zhang X., Zhou D., Xie R., Cai Y., Zhang K., Sun X. Inhaled nano-based therapeutics for pulmonary fibrosis: recent advances and future prospects. J. Nanobiotechnol. 2023;21(1):215. doi: 10.1186/s12951-023-01971-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Choi J.-S., Cao J., Naeem M., Noh J., Hasan N., Choi H.-K., Yoo J.-W. Size-controlled biodegradable nanoparticles: preparation and size-dependent cellular uptake and tumor cell growth inhibition. Colloids Surf., B. 2014;122:545–551. doi: 10.1016/j.colsurfb.2014.07.030. [DOI] [PubMed] [Google Scholar]
- 62.Lee C., Choi J.S., Kim I., Oh K.T., Lee E.S., Park E.S., Lee K.C., Youn Y.S. Long-acting inhalable chitosan-coated poly(lactic-co-glycolic acid) nanoparticles containing hydrophobically modified exendin-4 for treating type 2 diabetes. Int. J. Nanomed. 2013;8:2975–2983. doi: 10.2147/IJN.S48197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Le X.T., Lee J., Nguyen N.T., Lee W.T., Lee E.S., Oh K.T., Choi H.-G., Shin B.S., Youn Y.S. Combined phototherapy with metabolic reprogramming-targeted albumin nanoparticles for treating breast cancer. Biomater. Sci. 2022;10(24):7117–7132. doi: 10.1039/D2BM01281B. [DOI] [PubMed] [Google Scholar]
- 64.Ashcroft T., Simpson J.M., Timbrell V. Simple method of estimating severity of pulmonary fibrosis on a numerical scale. J. Clin. Pathol. 1988;41(4):467–470. doi: 10.1136/jcp.41.4.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.