Abstract
Objective To evaluate the functional results of patients submitted to a surgical approach for the treatment of the terrible triad of the elbow, analyzing the treatment methods used and associated epidemiological variables.
Methods Patients who underwent surgical treatment for the terrible triad of the elbow from February 2018 to June 2020 at our service were evaluated. The identified sample consisted of 17 patients, but of these, only 13 completed all stages of the study and, therefore, were considered as the universe to be considered. Epidemiological information of interest was collected: age, sex, hand of dominance, affected side, characteristics and classification of injuries, trauma mechanism, time to surgery, type of procedure performed and range of motion. The Mason classification was used for radial head fractures and the Regan and Morrey classification for the coronoid process. In order to perform a functional analysis, the DASH and BRUCE questionnaires were applied.
Results About 77% of the patients were male, 92% of the fracture mechanisms were due to high-energy trauma. Contrary to this, the predominance of the non-dominant side was observed as the most affected. Evaluating the results according to the time to start the treatment, the patients operated within 14 days had statistically better functional results.
Conclusion Surgical treatment of TTIE generates acceptable functional results in most cases. The success of the treatment is related to the time interval between the trauma and the first surgery, in addition to the severity of the injuries.
Keywords: coronoid fracture, elbow dislocation, radial head fracture, terrible triad injury of elbow, elbow joint.
Introduction
Elbow dislocation associated with radial head and coronoid fractures is called the terrible triad injury of the elbow (TTIE). This type of injury is usually related to ligament and capsular involvement of the joint, in addition to the involvement of flexor and extensor tendons. 1 The great structural involvement causes the instability of this joint, often resulting in limitation of range of motion, early arthrosis and joint stiffness. 2
Determined by Hotchkiss (1996), the term terrible triad injury of the elbow started to be used due to the difficulties in managing the injury and which historically presents an unsatisfactory outcome if there is no immediate diagnosis and adequate treatment. The anatomical and biomechanical understanding of the elbow associated with the understanding of the fracture-dislocation mechanism, as well as the development of new implants, have allowed a systematic approach to the treatment of this injury, enabling better functional results. 1 2 3
Regarding epidemiology, this is a rare pathology that usually affects young men. It typically arises from high-energy mechanisms, with one notable scenario being a fall involving an outstretched hand, hyperextended elbow, supination, and valgus stress. 4 5
In view of the scientific relevance of the best approach for treating the terrible triad injury of the elbow, the objective of this study is to evaluate the functional results of patients undergoing surgical intervention for this type of injury, analyzing the treatment methods used and associated epidemiological variables.
Materials and methods
This study was a cross-sectional study evaluating patients with the terrible triad of the elbow who underwent surgical treatment from February 2018 to June 2020 in our service, with a minimum postoperative follow-up of 12 months. The identified sample consisted of 17 patients, but of these only 13 completed all stages of the study and therefore were considered as the universe to be taken into account.
The epidemiological information of interest was collected: age, sex, side of dominance, affected side, characteristics and classifications of injuries, trauma mechanism, time to surgery, type of procedure performed and range of motion. The Mason classification was used for radial head fractures and the Regan and Morrey classification for the coronoid process. In order to perform a functional analysis, the DASH and BRUCE questionnaires were applied at 1, 3, 6, 9 and 12 months after the surgical approach.
The DASH score assesses everyday functional and work capabilities, ranging from no difficulty to totally incapable. It is composed of simple and direct questions answered by the patients themselves.
Among the criteria evaluated by the BRUCE score are the range of motion and cosmetic appearance, evaluation performed by the physician, and the presence of residual pain and impact on activities of daily living, which are considered based on the patients' responses.
Inclusion criteria were patients aged between 16 and 80 years and diagnosed with radial head fracture associated with coronoid fracture and elbow dislocation (terrible triad injury of the elbow). With regard to the exclusion criteria are the existence of other associated fractures in the same limb, active infection, clinical comorbidities that contraindicate surgery and patients younger than 16 years old.
Results
Among the 13 patients studied, 77% were male and only 23% were female. ( Fig. 1A-B ). Different ages were recorded, with a minimum of 27 years old and a maximum of 76 years old. With regard to the injured limb, 77% were in the left elbow and only 23% in the right, of these, 23% of the patients were left-handed and 77% were right-handed. Regarding the motivations for the trauma, although different situations were found, 92% were with a high-energy mechanism ( Table 1 ).
Fig. 1.

A-B AP and lateral radiographs, respectively, demonstrating fracture of the radial head, coronoid fracture, and subluxated elbow after closed reduction of the terrible triad injury of the elbow.
Table 1. Epidemiological data of the terrible triad injury of the elbow.
| Male | 10 (77%) |
| Female | 3 (23%) |
| Average Age | 45 years |
| Dominant side affected | 23% |
| Average time to surgery | 12 days |
Regarding the interval between the date of the trauma and the first surgical intervention, of the 13 cases evaluated, only 4 were operated on in less than 14 days. When analyzing the results obtained according to the time to start treatment, patients operated within 14 days had statistically better functional results than those operated on over 14 days. This longer interval until the surgery is performed among the patients studied may be decisive in the functional results found. In situations of this complexity, the ideal is for hospitalization to take place within 24-48 hours, and among the cases evaluated, the average time was 12 days.
In the present study, Mason's classification was used for fractures of the radial head, with 61% of the cases being type III, another 30% type II and 9% type I. of the coronoid process, the parameters of Regan and Morrey were used, with 38.5% of the cases as type I, 38.5% as type II and only 23% cases as type III. These epidemiological data obtained corroborate with those described in the literature. Conversely, a predominance of the non-dominant side as the most affected (77%) was observed. ( Table 2 ).
Table 2. Clinical data of patients undergoing surgical treatment of the terrible triad injury of the elbow.
| Interval between trauma and hospitalization | Interval between date of trauma and 1st surgical procedure | Mason score | Regan and Morrey classification | Radio Head Technique | Technique for coronoid | |
|---|---|---|---|---|---|---|
| 1 | 8 days | 27 days | III | II | Radial head arthroplasty | Coronoideplasty |
| 2 | 17 days | 23 days | II | II | Osteosynthesis | anchor fixation |
| 3 | 10 days | 22 days | I | I | Radial head arthroplasty | Coronoideplasty |
| 4 | 9 days | 22 days | II | II | Radial head arthroplasty | Coronoideplasty |
| 5 | 10 days | 13 days | III | I | Radial head resection | Coronoideplasty |
| 6 | 12 days | 12 days | II | II | Radial head arthroplasty | Coronoideplasty |
| 7 | 22 days | 34 days | III | III | Radial head arthroplasty | Fixation with Ethibond + External Fixator |
| 8 | 22 days | 24 days | III | III | Radial head arthroplasty | Coronoideplasty + Complex fixation Lateral ligament with anchors |
| 9 | 16 days | 52 days | II | I | Partial radial head resection | Coronoideplasty |
| 10 | 15 days | 44 days | III | I | Radial head resection | Coronoideplasty |
| 11 | 4 days | 11 days | III | I | Radial head arthroplasty | Conservative |
| 12 | 14 days | 26 days | III | II | Radial head arthroplasty | Coronoideplasty |
| 13 | 2 days | 10 days | III | III | Radial head resection | Coronoideplasty |
Initially, the patients underwent closed reduction of the dislocation and immobilization with an axillary plaster splint, until the surgical treatment was performed. Regarding the surgical techniques, radial head arthroplasty (60%), resection (30%) and osteosynthesis (10%) were used in the radial head were. As for the coronoid fracture, coronoidplasty (80%), anchor fixation (20%) and conservative (7.7%) were used. ( Figs. 2 and 3 ).
Fig. 2.

Intraoperative photograph demonstrating lateral access used for coronoid repair, radial head repair/replacement, and common extensor/LCL repair.
Fig. 3.

Intraoperative photography. Bone fragment of the head of the radius resected during a surgical approach.
Of the 13 patients followed up, 7 (54%) underwent a second surgery. Of these, 4 were performed to remove the external fixator placed at the time of the first surgery, 1 to replace the radial head prosthesis that was subluxated in the immediate postoperative period, 1 patient underwent joint manipulation due to elbow stiffness and 1 for external fixator placement. This last patient underwent a third procedure to remove this fixator. The need to place an external fixator was due to the identification of joint instability during passive movement. Half of the of patients included in this study returned to their professional activities.
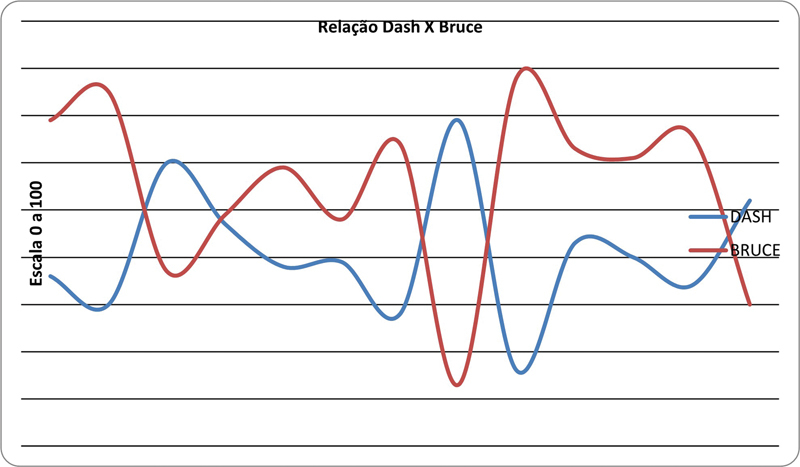
Regarding the DASH score, in which the highest values indicate worse clinical conditions, only 2 patients had a high score. With regard to BRUCE, as expected, a greater number of patients had a high score, ranging from 13 to 78 ( Table 3 ).
Table 3. Classification of the terrible triad injury of the elbow according to the DASH and BRUCE scores.
| FLEX/EXTENSION | PRONE/SUPINATION | DASH | BRUCE | |
|---|---|---|---|---|
| 1 | 15 - 140 | 60 / 10 | 36 | 69 |
| 2 | 20 - 140 | 50 / 50 | 20 | 75 |
| 3 | 70 - 110 | 20 / 10 | 60 | 37 |
| 4 | 30 -70 | 45 / 45 | 47 | 49 |
| 5 | 60 - 120 | 50 / 50 | 38 | 59 |
| 6 | 10 - 130 | 60 / 40 | 39 | 48 |
| 7 | 30 - 120 | 50 / 40 | 28 | 64 |
| 8 | 20 - 30 | 10 / 10 | 69 | 13 |
| 9 | 20 - 130 | 70 / 70 | 16 | 78 |
| 10 | 30 - 110 | 60 / 30 | 43 | 63 |
| 11 | 30 - 110 | 50 / 40 | 40 | 61 |
| 12 | 20 - 120 | 45 / 45 | 34 | 66 |
| 13 | 30 - 70 | 40 / 40 | 52 | 30 |
It is possible to relate the functional results obtained by the scores and by the physical examination with the severity of the injury. It was also observed that among the results obtained in the flexion/extension and prone/supination analysis, and the DASH and BRUCE scores achieved, it can be seen that the patient who presents a good range of motion is the same one who had satisfying DASH and BRUCE's results. Likewise, patients with poor scores were those who had more compromised Flexo/Extension and Prone/Supination results ( Fig. 4 ).
Fig. 4.
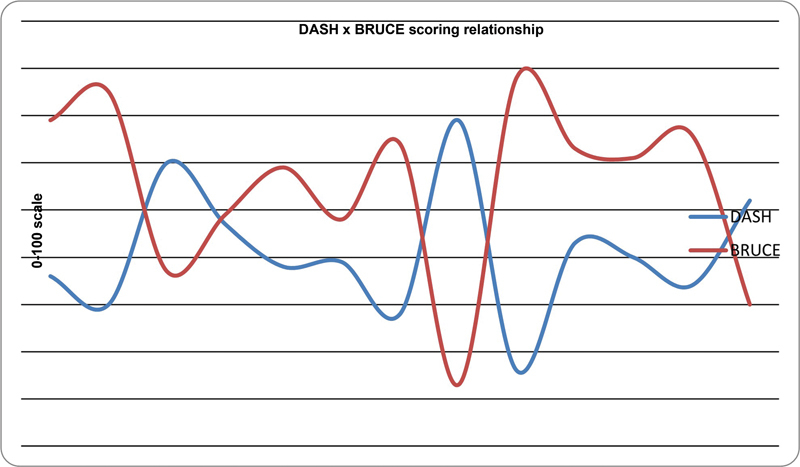
DASH and BRUCE scoring relationship. Relação DASH x BRUCE = DASH x BRUCE scoring relationship, Escala 0 a 100 = 0-100 scale
In addition, when relating the DASH and BRUCE scores of each patient, we observed that those with the lowest DASH scores were also the ones with the highest BRUCE scores. Since these two scores are opposites, while high BRUCE scores are desired, DASH is expected to be low. Thus, the result found in the studied sample is in accordance with the indicators of the area.
Discussion
The terrible triad injury of the elbow is a complex injury with an unfavorable prognosis due to recurrent functional limitations. 6 The main rotatory mechanisms of injury are posterolateral and posteromedial, the displacement force involves supination of the forearm and of the valgus. In cases where rotation is sufficient for the coronoid process and the head of the radius to project below the distal humerus, the dislocation is considered simple. On the other hand, in insufficient rotation, the distal humerus fractures the coronoid process and the radial head, configuring the terrible triad injury of the elbow. The first ligament affected is the lateral collateral (LCL), followed by the medial collateral (LCM). 4 5
The diagnosis is made through standard anteroposterior and lateral radiographs; however, this type of fracture may not be visualized in conventional radiological exams. Thus, it is important that patients who are victims of the aforementioned traumatic mechanism, who have reduced limb mobility, edema, pain on passive and active movement, undergo computed tomography to rule out possible injuries. 7
In the vast majority of cases, surgical treatment is the most indicated since it offers better outcomes. 2 3 Some variants are relevant in obtaining the results of these patients, such as the trauma mechanism, patient age, fracture severity, and time to start treatment. However, even if adequate treatment is used, some complications can be expected, such as range of motion limitation, ligament instability, arthrosis and ulnar neuropathy. 6 8 9
Surgical treatment comprises, in general, reduction and fixation of the coronoid process, repair of fractures of the radial head and of the lateral ligament complex. The medial collateral ligament approach is performed in specific cases of maintenance of residual instability. 10 11
When analyzing the results obtained by Gonçalves et al., 12 in which the DASH score was used to assess treated patients, it is possible to see that they obtained an average score of 12, a result much lower than those achieved in this study, in which the average score was 40 points. This difference in results may be due to the long waiting time for the start of treatment and the severity of these cases of the patients surveyed.
However, in a study by Miyazaki et al., 13 where the BRUCE was used as a parameter for evaluating the results, the scores obtained were much higher than those achieved in this study. Even though most of them were not considered excellent by the researchers, they indicated greater success in the techniques used.
In addition, surgical performance by different professionals may, to some extent, have interfered with the results. Even knowing that all are qualified surgeons, in a study it is important that the sample is submitted to the same parameters for greater reliability and possibility of comparison between cases and results achieved. In a situation where this group of patients went through different parameters in care, it is possible that there are also differences in the results.
Conclusions
Surgical treatment of the terrible triad injury of the elbow generates acceptable functional results in most cases, regardless of the method used. It is also noteworthy that the success of the treatment is related to the time interval between the trauma and the first surgery, in addition to the severity of the injuries. Therefore, the longer this interval and the greater the severity of the injury, the greater the patient's difficulty in restoring elbow functions. Furthermore, due to the reduced sample size, we suggest new studies in order to prove such outcomes.
Funding Statement
Suporte Financeiro O presente estudo não recebeu nenhum suporte financeiro de fontes públicas, comerciais ou sem fins lucrativos.
Financial Support This study did not receive any financial support from public, commercial, or non-profit sources.
Conflito de Interesses Os autores declaram não haver conflito de interesses.
Estudo desenvolvido no Departamento de Ortopedia e Traumatologia do Hospital do Oeste, BA, Brasil.
Study developed at the Orthopaedics and Traumatology Department of the Hospital do Oeste, BA, Brazil.
Referências
- 1.Kani K K, Chew F S. Terrible triad injuries of the elbow. Emerg Radiol. 2019;26(03):341–347. doi: 10.1007/s10140-019-01676-1. [DOI] [PubMed] [Google Scholar]
- 2.Ohl X, Siboni R.Surgical treatment of terrible triad of the elbow Orthop Traumatol Surg Res 2021107(1S):102784. [DOI] [PubMed] [Google Scholar]
- 3.Rodriguez-Martin J, Pretell-Mazzini J, Andres-Esteban E M, Larrainzar-Garijo R. Outcomes after terrible triads of the elbow treated with the current surgical protocols. A review. Int Orthop. 2011;35(06):851–860. doi: 10.1007/s00264-010-1024-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rhyou I H, Lee J H, Cho C H, Park S G, Lee J H, Kim K C. Patterns of injury mechanism observed in terrible triad. J Shoulder Elbow Surg. 2021;30(09):e583–e593. doi: 10.1016/j.jse.2020.12.015. [DOI] [PubMed] [Google Scholar]
- 5.Reichert I L, Ganeshamoorthy S, Aggarwal S, Arya A, Sinha J.Dislocations of the elbow - An instructional review[published correction appears in J Clin Orthop Trauma 2021;20:101539]J Clin Orthop Trauma 202121101484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Giannicola G, Calella P, Piccioli A, Scacchi M, Gumina S. Terrible triad of the elbow: is it still a troublesome injury? Injury. 2015;46 08:S68–S76. doi: 10.1016/S0020-1383(15)30058-9. [DOI] [PubMed] [Google Scholar]
- 7.Zeiders G J, Patel M K. Management of unstable elbows following complex fracture-dislocations–the “terrible triad” injury. J Bone Joint Surg Am. 2008;90 04:75–84. doi: 10.2106/JBJS.H.00893. [DOI] [PubMed] [Google Scholar]
- 8.Egol K A, Immerman I, Paksima N, Tejwani N, Koval K J. Fracture-dislocation of the elbow functional outcome following treatment with a standardized protocol. Bull NYU Hosp Jt Dis. 2007;65(04):263–270. [PubMed] [Google Scholar]
- 9.Ring D, Jupiter J B, Zilberfarb J. Posterior dislocation of the elbow with fractures of the radial head and coronoid. J Bone Joint Surg Am. 2002;84(04):547–551. doi: 10.2106/00004623-200204000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Gomide L C, Campos DdeO, Ribeiro de Sá J M, Pamfílio de Sousa M R, do Carmo T C, Brandão Andrada F. Terrible triad of the elbow: evaluation of surgical treatment. Rev Bras Ortop. 2015;46(04):374–379. doi: 10.1016/S2255-4971(15)30248-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Seijas R, Ares-Rodriguez O, Orellana A, Albareda D, Collado D, Llusa M. Terrible triad of the elbow. J Orthop Surg (Hong Kong) 2009;17(03):335–339. doi: 10.1177/230949900901700319. [DOI] [PubMed] [Google Scholar]
- 12.Gonçalves L B, Neto JdeA, Correa Filho M R et al. Terrible triad of the elbow: influence of radial head treatment. Rev Bras Ortop. 2014;49(04):328–333. doi: 10.1016/j.rboe.2014.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miyazaki A N, Santos Checchia C, Fagotti L et al. Evaluation of the results from surgical treatment of the terrible triad of the elbow. Rev Bras Ortop. 2014;49(03):271–278. doi: 10.1016/j.rboe.2014.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]