Abstract
Background:
In 2021, several professional organizations declared a national state of emergency in child and adolescent mental health. Rising volume and acuity of pediatric mental health emergencies, coupled with reduced access to inpatient psychiatric care, has caused tremendous downstream pressures on EDs resulting in long lengths of stay, or “boarding”, for youth awaiting psychiatric admission. Nationally, boarding times are highly heterogeneous, with medical/surgical patients experiencing much shorter boarding times compared to patients with primary mental health needs. There is little guidance on best practices in the care of the pediatric patient with significant mental health need “boarding” in the hospital setting.
Objective:
There is a significant increase in the practice of “boarding” pediatric patients within emergency departments and inpatient medical floors while awaiting psychiatric admission. This study aims to provide consensus guidelines for the clinical care of this population.
Methods:
Twenty-three panel participants of fifty-five initial participants (response rate 41.8%) committed to completing four successive rounds of questioning using Delphi consensus gathering methodology. Most (70%) were child psychiatrists and represented 17 health systems.
Results:
Thirteen participants (56%) recommended maintaining boarded patients in the emergency department, while 78% indicated a temporal limit on boarding in the emergency department should prompt transfer to an inpatient pediatric floor. Of this group, 65% recommended a 24-hour threshold. Most participants (87%) recommended not caring for pediatric patients in the same space as adults. There was unanimous agreement that emergency medicine or hospitalists maintain primary ownership of patient care, while 91% agreed that child psychiatry should maintain a consultative role. Access to social work was deemed most important for staffing, followed by behavioral health nursing, psychiatrists, child life, rehabilitative services, and lastly, learning specialists. There was unanimous consensus that daily evaluation is necessary with 79% indicating vitals should be obtained every 12 hours. All agreed that if a child psychiatric provider is not available on-site, a virtual consultation is sufficient to provide mental health assessment.
Conclusions:
This study highlights findings of the first national consensus panel regarding the care of youth boarding in hospital-based settings and provides promising beginnings to standardizing clinical practice while informing future research efforts.
Keywords: emergency medicine, emergency psychiatry, child and adolescent psychiatry, consultation-liaison psychiatry, boarding, length of stay, consensus guidelines, consensus best practice, Delphi methodology, mental health crisis, mental health emergency, youth
In 2021, American Academy of Child and Adolescent Psychiatry, American Academy of Pediatrics, and Children’s Hospital Association declared a national state of emergency in child and adolescent mental health.1 The rate of emergency department (ED) visits for medical conditions increased 11.7% from 2006–2014, while the rate of mental health/substance use-related ED visits increased 44.1% during the same period.2 Visits due to suicidal ideation increased by an alarming 414.6%.2 At the same time, there has also been a major decrease in the number of national inpatient psychiatric beds available.3,4 In a study from 2007–2016, pediatric emergency visits for a primary mental health concern rose by 60% with a 300% increase in youth presenting for suicide or self-inflicted injury.5 During the pandemic, the proportion of pediatric patients presenting to the ED with a primary mental health concern, compared to other medical concerns, rose by 20–30% compared to the same period in 2019.6 Among pediatric patients, there has been a statistically significant rise in hospital presentations of suicidal ideation, suicide attempts, depression, anxiety, eating disorders, and substance use in the year following the pandemic compared to the prepandemic period.7 Furthermore, in one study, there was a doubling in psychiatric boarding times for youth with 50% of youth experiencing boarding periods of greater than 2 days following the pandemic.7
Rising volume and acuity of pediatric mental health emergencies, coupled with reduced access to inpatient psychiatric care, have caused tremendous downstream pressures on EDs, resulting in long lengths of stay, or “boarding”, for youth awaiting psychiatric admission.8,9 The Joint Commission recommends boarding time frames not exceeding 4 hours in the interest of patient safety and quality of care.10 However, across hospitals, boarding times are highly heterogeneous, ranging from less than 2 hours up to several weeks, with medical/surgical patients experiencing much shorter boarding times compared to patients with primary mental health needs.10,11
Boarding misaligns patient need to environment and resource allocation resulting in poor outcomes, safety risks, delays in care, workflow inefficiencies, and capacity concerns.12,13 This discrepancy is influenced by limited access to preventative and ambulatory care services, limited care coordination, increased chronic psychosocial stress, lack of intermediate care psychiatric services (such as partial hospitalization and intensive outpatient), lack of diversionary services from inpatient and ED settings, and declining number of inpatient psychiatric beds.14 This study summarizes the findings of a workgroup composed of members from professional organizations in child psychiatry and emergency medicine in the development of consensus guideline recommendations for the care of youth boarding in ED and inpatient pediatric settings.
METHODS
Study Design
The study aimed to obtain expert consensus regarding the evaluation and management of youth through sequential rounds of surveys utilizing the Delphi method for consensus building (Figure 1). The Delphi method was selected in order to obtain reliable opinion consensus and limit bias by eliciting deidentified input from the participant panel equitably across all participants.15,16 This is done by posing a series of questions to all panel participants with responses being collected, deidentified, and further exploratory questions being asked in follow-up to gather greater nuance, elicit greater reflection, and provide further detailed, iterative responses without contamination of responses by other participants. As such, this methodology limits individual members of the panel from overly influencing the panel’s responses by their expertise, seniority, strength of their opinions, or past experiences. Using this consensus gathering methodology, opinions were elicited from the panel of experts through a series of emailed survey links to provide structured feedback. The study received an institutional review board exemption through the Northwell Health System.
FIGURE 1.
Delphi Consensus Gathering Process
Panel Participants
A convenience sample was obtained from members of the American Academy of Pediatrics, American College of Emergency Physicians Pediatric Subcommittee, American Academy of Child and Adolescent Psychiatry, and American Association of Emergency Psychiatry who were invited to participate in a Pediatric Psychiatry Boarding Consensus Panel in August 2019, at which time initial surveys were disseminated (all surveys available upon request). Participants included pediatric hospitalists, ED physicians, ED psychiatrists, and consultation-liaison psychiatrists with two team members serving as cofacilitators (Table 1). Expertise for inclusion in the consensus panel was defined as any individual with more than one year of experience in the care of youth with mental health emergencies in the emergency department or inpatient medical setting and national experience disseminating research or teaching related to this experience through peer-reviewed publication. All responses from participants were completed by online survey, and responses were deidentified for analysis. No incentivization was utilized to elicit participant engagement. Fifty-five clinicians initially indicated interest in participating in the consensus panel, and the initial round of surveys were distributed on 5/7/21. We had a 41.8% response rate (23/55), and our panel included representation from 17 health systems with 3 adult psychiatrists, 16 child and adolescent psychiatrists, 2 pediatricians, and 2 emergency medicine physicians. The participant response rate is consistent with other survey-based, nonincentivized studies.17,18 Panel participation was consistent throughout the successive rounds of consensus building (Round 1 N = 23, Round 2 N = 23, Round 3 N = 21, Round 4 N = 23).
TABLE 1.
Participant Importance Ranking for Aspects of Care Related to the Pediatric Boarding Patient
| Aspects of care | Ranking along 5-point Likert scale (5 being most important) | |||||
|---|---|---|---|---|---|---|
| Environment | Pediatric-specific space (4.39)* | Bathroom privilege observation (4.00)* | Access to single patient room (3.65) | Access to safe room (3.5) | Access to seclusion room (3.3) | |
| Staffing | Access to social work (4.78)* | Access to behavioral health nursing (4.09)* | Availability of on-site psychiatrist (3.9) | Access to child life/occupational therapy (3.7) | Access to learning specialist (2.6) | |
| Service delivery | ||||||
Indicates consensus threshold was reached.
Survey Dissemination and Data Analysis
The onset of the COVID-19 pandemic in March 2020 delayed study implementation, with resumption of the study in March 2021. The cofacilitators began meeting biweekly in March of 2021. Between May and July of 2021, there were four sequential rounds (5/7, 5/21, 6/4, and 7/21/21) of survey questions using RedCap software 12.2.10 – 2022 Vanderbilt University. Survey questions were utilized to clarify group recommendations related to the following topics: staffing, supervision of patient care, environmental needs, psychiatric services available, the nature of ongoing psychiatric assessment, alternate dispositions, and the impact of COVID on the care of this population. The goal of the survey was to obtain consensus on a variety of aspects of care for youth boarding in the hospital-based setting. No validated survey or tool existed to elicit this information from participants, so questions were developed by the cofacilitators, and responses were clarified over the course of successive rounds of data gathering. Survey validation was then completed using local subject matter experts on the panel to ensure face and content validity and ease of administration. Following each survey round, clarifying questions were posed to the panel in successive rounds for items that did not reach consensus threshold. Surveys were brief (5–10 minutes) with the aim of eliciting recommendations to reach consensus, as opposed to reviewing specific data points from the representative health systems. A virtual panel meeting for preliminary finding review was completed in June 2021, and consensus panel final input was completed in March 2022. Descriptive statistics were utilized to categorize the results, and a 70% cutoff (determined by the panel participants) was used to define the threshold for consensus, which has been modeled after other studies using the Delphi technique.19–22 A 5-point Likert scale was used for questions ranking items by importance with a cutoff score of 4 or above (important to very important) was used to identify best practice recommendations (Table 1). A series of free-text questions were included and analyzed using qualitative analysis for thematic content review, which helped inform iterative clarifications and consensus building.
RESULTS
Of the 23 participants, all defined “boarding” as a status when a disposition decision has been made to admit a pediatric patient to an inpatient psychiatric unit but an inpatient psychiatric bed is not available. 82.6% agreed this terminology may be applied regardless of the patient’s location when boarding, while 78.3% believed it is appropriate to further add the Centers for Medicaid & Medicare Services 4-hour time specifier to the boarding definition. Regarding the physical site for boarding, 56% maintained all boarding patients in the ED, 26% transferred patients to the inpatient floor, and 18% indicated variable practice based on bed availability. Of those who initially boarded patients in the ED, 23% identified that the patient may be moved to the pediatric floor after waiting 24 hours in the ED. Most participants (78%) agreed that a specific amount of time should be used to determine transfer to an inpatient pediatric bed. However, there was a split between the temporal threshold, where 65% identified a 24-hour limit and 35% identified a 48-hour limit.
Environment
The most important aspects of the environment were ranked by participants in Table 1. Most participants (87%) said they would not recommend having pediatric patients in a locked care space with adults. For those who found caring for adults and youth in a shared space was acceptable (13%), they prefaced that this would only be utilized as a last resort factoring patient age and safety of the milieu in this decision. In addition, 95.7% cited access to a private interview space as both highly important and necessary for pediatric patient care.
Staffing
Participants unanimously agreed that ED physicians or pediatric hospitalists should maintain primary care ownership of patients on boarding status, while 91% believed child psychiatry should remain in a consultant role. Elements that weighed heavily into this recommendation included available resources on the psychiatry team, inability to provide 24/7 coverage among child psychiatrists (41%), and inability to appropriately manage the high volume of patients (24%). Consensus was not reached regarding staffing with a split between weekly staffing (31.8%) and daily staffing models (22.7%). However, 90.5% identified that the staffing model utilized could vary as long as there was a consistent model for handoffs to ensure coordination of care. Participants also cited team provider consistency (including advanced practice providers and social workers) as another important factor in facilitating patient care and disposition planning.
Aspects of staffing were also assessed by level of importance (Table 1). Many participants (74%) indicated the location of a patient dictates which (if any) ancillary services are available. However, 70% stated that the relative importance of a service should not depend on the location of the patient. There was unanimous agreement that patients would benefit from child life, occupational therapy, and other milieu therapies made available as a part of standard of care regardless of location. Participants unanimously agreed that a team member not responsible for direct patient care should be assigned the task of locating an inpatient psychiatric bed.
Service Delivery
Participants unanimously identified that daily evaluations should be conducted on the boarding patient, regardless of location. However, the tasks to be completed as part of daily evaluation varied, where 56% believed physical exams should be completed daily, and 44% believed only one initial physical exam was needed at the beginning of the stay. Group discussion was facilitated to clarify the frequency of obtaining vital signs due to lack of consensus between every 8 and every 12 hours. Consensus was reached and that obtaining vital signs every 12-hour was sufficient (79%). Consensus was reached internally among nonpsychiatry providers (n = 4) for once daily physical exams, 12-hour vital signs, and requesting transfer to an inpatient pediatric bed for boarding after 24 hours in the ED. Table 1 summarizes participant importance rankings of child psychiatric service delivery to the boarding patient.
Access to Telepsychiatry
Physician availability on-site, as opposed to remote coverage, was highly variable among participants at their current site of practice. In the context of the COVID-19 pandemic, 5% reported access to telepsychiatry prior to the pandemic, 52% identified new access during the pandemic with 14% reporting expansion of those services over the course of the pandemic, and 28% report still not having access to telepsychiatry. Telephonic access to the child psychiatry team was identified by 65% of participants as being insufficient to meet a minimum standard of psychiatric care for boarding patients, and 76% believed phone backup should not replace daily face-to-face assessment by the child psychiatry team. However, participants all agreed that if a psychiatrist is not available on-site, then formal telepsychiatry consultation is sufficient. Consensus was not fully reached (66.7%) that in-person evaluations should be considered equivalent to telepsychiatry. Among nonpsychiatry participants (n = 4), unanimous consensus was reached that telepsychiatry consultation was equivalent to in-person psychiatry evaluation.
Further clarifying questions were asked to identify when an in-person child psychiatric evaluation should be completed. Consensus was reached in three patient populations, including those with delirium (96%), catatonia (96%), and psychosis (74%). Consensus was not reached for younger children (65%), disruptive parents (61%), as well as patients with autism (65%), hyperactivity impairing assessment (61%), or exhibiting severe aggression (61%). For youth requiring physical restraint, 52% reported that in-person psychiatry assessment was superior to telepsychiatry in this population.
COVID Impact
The COVID-19 pandemic has greatly influenced national mental health care delivery23–26 which was affirmed by panel participants. Pandemic-related changes reported by panel participants included increased volume and duration of pediatric boarding (87%), and higher acuity of patient needs (35%). Panelists noted increased utilization of ED and hospital resources by youth with subspecialty psychiatric needs, such as youth with autism spectrum disorder and eating disorders (22%). Uniformly, participants reported challenges finding inpatient psychiatric beds for youth who were COVID-positive. Some participants (35%) reported a significant change in workflow secondary to the pandemic including the requirement to wear full personal protective equipment during behavioral code events with resulting challenges to de-escalate patients with comorbid autism spectrum disorder, intellectual disability, or psychosis and impact on response times.
Data Gathering and Monitoring
Lastly, participants were asked about several data items to measure and monitor for pediatric patients boarding in hospital settings (Figure 2). These items were ranked in terms of importance and feasibility of obtaining the data longitudinally. The two items of data that met consensus threshold for importance and feasibility were patient age and volumes.
FIGURE 2.
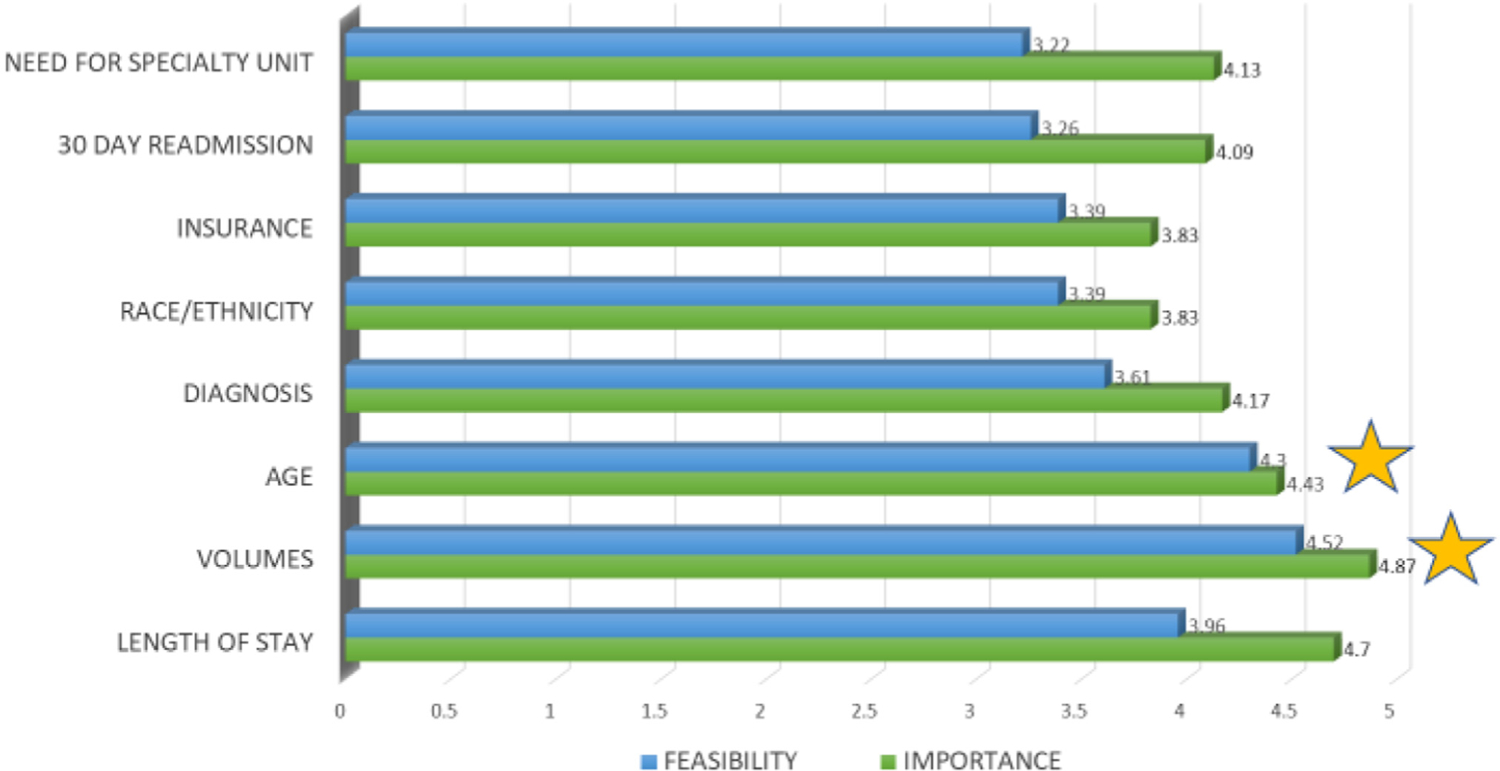
Summary of Importance and Feasibility Rankings for Pediatric Boarding Data Gathering
* Starred areas met consensus for both importance and and feasibility
We explored the feasibility of collecting data specific to patients on boarding status, and 21 participants indicated that they were actively collecting some data on boarding patients. Fifty-two percent of respondents were unsure what data was being collected by their respective health systems. Forty-three percent (43%) reported a willingness to collect data that may be considered both important and feasible.
In summary, consensus was reached on several items to include 1) the definition of boarding, 2) recommendations for the treatment environment, and 3) staffing and service delivery recommendations for the care of pediatric patients with mental health emergencies boarding in hospital-based settings (Table 2).
TABLE 2.
Summary of Best Practice Recommendations for the Care of Youth Boarding in Emergency Department and Hospital Settings
| Definition |
| Boarding is a status when a disposition decision has been made to admit a pediatric patient to an inpatient psychiatric unit, but an inpatient psychiatric bed is not available within a four-hour window, regardless of where the patient is temporarily located. |
Treatment environment
|
Staffing
|
Service delivery
|
DISCUSSION
According to the American Academy of Child and Adolescent Psychiatry, in the current care environment for youth experiencing mental health emergencies, there is a significant lack of access to child psychiatric providers and staff,27 with increasing demand for pediatric mental health services. The result is a significant growth in boarding of youth in medical emergency rooms and inpatient settings. As noted above, this mismatch between access and need has been exacerbated by the COVID-19 pandemic. Many panel participants were initially concerned that developing best practice recommendations for boarding patients may unintentionally perpetuate this practice and allow it to be normalized or accepted. However, given the current crisis in pediatric mental health, the practice of boarding is unlikely to disappear soon, and consensus guidelines on the care of this population are desperately needed (Table 2).
By exploring the areas of unanimous consensus, the guidelines provide a minimum standard for safe, equitable care while providing significant leverage to the end user to provide plasticity in the application of these recommendations. There were several unanimous recommendations from the consensus panel. Access to confidential interview rooms and avoiding scenarios where youth are cohorted in locked adult spaces for care highlight the emphasis panel participants placed on safety and confidentiality in the care of this vulnerable population, two factors that are critical in how clinical operations and space design are dictated. This was further affirmed by full consensus being reached on the need for daily patient evaluations, staffing models that support consistent and safe handoffs, and the importance of having access to a member of the psychiatric care team, whether in person or via telepsychiatry. Other recommendations include ensuring that youth have access to the full spectrum of services available in the pediatric medical setting (such as child life, occupation therapy, physical therapy, etc.) and that a team member not responsible for direct patient care is assigned to complete the psychiatric bed search. Unanimous consensus was also reached regarding the recommendation to identify the emergency department or pediatric hospitalist team as the primary provider for ongoing care in the medical setting rather than adopting a model where the psychiatrist becomes the primary provider. Panel participants cited the nature of the medical care setting and the staff limitations inherent to providing 24/7 on-site psychiatric staffing as the primary reasons that the emergency department or general pediatric team should maintain responsibility for patient care. Furthermore, support for the ongoing role of the child psychiatrist as a consultant also received near unanimous consensus, which highlights the panel’s belief that ongoing psychiatric care is needed even when the emergency department or general pediatric team is managing patients on boarding status. Thus, the combination of psychiatric consultation with ongoing medical oversight in a collaborative model was the predominant agreed-upon model of care delivery for this population in the medical setting.
There were also several items where consensus could not be reached, highlighting the heterogeneity in view-points, local resources, and practice in these areas. Although there was consensus on the need for a time threshold to consider transferring patients from the emergency department to the inpatient medical unit, there was variability as to the number of hours suggested. There was a lack of consensus as to what staffing model was best; however, the need for consistent and clear handoffs was identified as the most important variable for safe care. This same theme was seen with the consensus recommendation that daily assessments should be conducted on all boarding patients, with a lack of consensus on the frequency and what elements of exam should be conducted daily. These consensus recommendations provide flexibility to customize one’s approach based on local resources. However, consensus was reached on the specific aspects of what was more essential for safety, such as which populations required an in-person assessment and the frequency of obtaining vital signs.
Limitations
This study has several limitations worth noting. The consensus guidelines are based on expert panel input, and the risk of overrepresentation of certain sub-specialties or certain types of health systems is openly acknowledged. To address these biases, we utilized blinded responses as outlined in the Delphi methodology. While this survey model reduces bias and allows for ease of implementation, it has several limitations, including a lack of internal validity and reliability, along with the lack of a single methodology, and its inherent outcome of opinion-based information.28 A convenience sample was created using professional listservs. It was difficult to ascertain the number of active members surveyed through these professional listservs, as the listservs may contain members who are retired or not actively practicing in the fields of emergency medicine, emergency psychiatry, or consultation-liaison psychiatry. Therefore, determining the number of active members with expertise in the psychiatric care of youth in mental health crisis was challenging to determine the total number of eligible participants who were initially surveyed. Furthermore, only 23 of 55 participants completed the full survey process, with a modest response rate of 42%. This convenience sampling and limited expert panel size may limit the generalizability of the study’s findings.
Given that the expert panel was a convenience sample elicited from several professional listservs, with an oversampling of psychiatry professional listservs, there was a greater proportion of child psychiatrists among the panel participants when compared to general pediatric or emergency medicine representation. While this may have introduced bias, given the topic of pediatric mental health care delivery, it also reflects the anticipated input necessary to deliver guidance on this topic. Further follow-up study should capture a wider catchment of stakeholders including broader engagement from pediatric emergency medicine physicians, pediatric emergency medicine nursing, pediatric hospitalists, adult emergency medicine physicians and nurses, social workers, and adult emergency psychiatrists. Although we intentionally oversampled emergency psychiatry and child and adolescent psychiatry participants in reaching these consensus guidelines, given the expertise in the delivery of emergency mental health services to this population, we also note the important value of emergency medicine, particularly pediatric emergency medicine, in informing guidance, both due to expertise in the delivery of emergency medical services, as well as serving as frontline providers in the care of youth boarding in the ED.
The response rate was in keeping with a nonincentivized survey study. The survey used in this study only addressed the elements of face validity and content validity. For future studies, any similar surveys would need to go through more rigorous reliability testing (e.g., internal consistency) and validity testing (e.g., criterion validity, construct validity). There are also complex factors that influence boarding including the child’s developmental status, history of past physical or sexual trauma, comorbid medical conditions, family capacity to manage the patient in the home environment, and access to community-based resources. Some of these factors were elicited in the qualitative responses by panel participants but were not specifically elicited in the consensus gathering surveys. It will be important in future studies to explore these factors further to understand how they may impact boarding practices, length of stay, and interventions to address boarding in these unique populations. This study also did not review safety measures taken for youth who were boarding, such as what ligature risk mitigation practices were undertaken, what clothing the youth could wear while boarding, whether youth had access to technology (cell phones, computers, tablets), or what sitter or patient attendant practices were utilized. Partly, these items were not included as they were not specific to boarding patients but more to patients at risk of harm to themselves or others. The study also lacks guidance on what active interventions, both non-pharmacologic and pharmacologic, should be taken in youth while boarding, which is likely partly influenced by staffing models and access to child and adolescent psychiatry. Given the breadth of topics covered in the survey, it was challenge to address all important topics, and these specific safety and management measures in the boarding patient should be addressed in future studies. Additional areas requiring future exploration are included in Table 3.
TABLE 3.
Additional Areas for Future Study and Exploration in Pediatric Boarding
| Issue | Contributing variables |
|---|---|
| Excessive boarding times |
|
| Utilization of nonphysician, multidisciplinary team members (APPs, behavioral health RN, SW, ancillary therapeutic and educational staff) |
|
| Creating therapeutic milieu |
|
| Timely access to intermediate levels of care |
Limited access to:
|
| Reimbursement |
|
| Data collection and analysis |
|
| Advocacy |
|
CONCLUSIONS
This study summarizes the consensus recommendations for the care of youth boarding in medical settings while awaiting inpatient psychiatric care. Although the long-term goals of improving access to timely mental health care while minimizing the need for boarding remain, openly acknowledging that the practice of boarding is a growing and urgent crisis that requires thoughtful guidance to inform standards of care is necessary. This study represents the first step in providing national consensus guidelines on the delivery of care while youth are boarding and provides valuable input on future areas that require improved standardization or further research.
Acknowledgments:
The authors wish to acknowledge Kathleen Samiy for her efforts in the design of Figure 1.
The members of the Pediatric Consensus Boarding Panel are as follows: Arpit Aggarwal MD, University of Missouri Health Care, Aniruddh P. Behere MD, Michigan State University, Khyati Brahmbhatt MD, University of California San Francisco, Beech Burns MD, MCR, Oregon Health Sciences University, Beau Carubia MD, Children’s Hospital of Colorado, Anilla Del Fabbro MD, Carilion Clinic, Mary Lynn Dell MD, Children’s Hospital of New Orleans, Kathleen Donise MD, Warren Alpert Medical School of Brown University, Susan Duffy MD, Warren Alpert Medical School of Brown University, Lisa Giles MD, University of Utah School of Medicine, Kyle Johnson MD, Oregon Health Sciences University, Raj K. Kalapatapu MD, PhD, University of California San Francisco, Marybeth Lardizabal DO, Allina Health, Claudia Moreno MD, Yale School of Medicine, Alba Pergjika MD, MPH Feinberg School of Medicine, Donald Pierce MD, Vanderbilt University Medical Center, Steven Rogers MD, University of Connecticut School of Medicine, Meghan Schott DO, GW School of Medicine and Health Sciences, Richard J. Shaw MD, Stanford Medicine, David Sheridan MD, Oregon Health Sciences University, and Kashmeer Zablan MD, Hartford Healthcare.
Funding:
This research was supported in part by the Intramural Research Program of the National Institutes of Health. Annual report ZIA MH002922-12. Dr. Mooneyham is a medical officer at the National Institutes of Health and receives salary support through the National Institute of Mental Health Intramural Research Program.
Footnotes
Conflicts of Interest: Dr. GenaLynne C. Mooneyham is an employee of the National Institute of Mental Health, Bethesda, MD. The views expressed in this article do not necessarily represent the views of the National Institutes of Health, the Department of Health and Human Services, or the United States Government. All other listed authors have no conflicts of interest to disclose.
Disclosure: The manuscript is not submitted or under review at any other site at this time, and all authors verify that the contents of the manuscript are the original work of the authorship group.
References
- 1.AAP-AACAP-CHA declaration of a national emergency in child and adolescent mental health. Available from: https://www.aap.org/en/advocacy/child-and-adolescent-healthy-mental-development/aap-aacap-cha-declaration-of-a-national-emergency-in-child-and-adolescent-mental-health/
- 2.Moore BJ, Stocks C, Owens PL: Trends in emergency department visits, 2006–2014. Rockville, MD: Agency for Healthcare Research and Quality; 2017 [Google Scholar]
- 3.Currier GW: Psychiatric bed reductions and mortality among persons with mental disorders. Psychiatr Serv 2000; 51:851. [DOI] [PubMed] [Google Scholar]
- 4.Blader JC: Acute inpatient care for psychiatric disorders in the United States, 1996 through 2007. Arch Gen Psychiatry 2011; 68:1276–1283 [DOI] [PubMed] [Google Scholar]
- 5.Lo CB, Bridge JA, Shi J, et al. : Children’s mental health emergency department visits. Pediatrics 2020; 145:e20191536. [DOI] [PubMed] [Google Scholar]
- 6.Leeb RT, Bitsko RH, Radhakrishnan L, et al. : Mental health-related emergency department visits among children aged, 18 Years during the COVID-19 pandemic - United States, January 1-October 17, 2020. MMWR Morb Mortal Wkly Rep 2020; 69:1675–1680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ibeziako P, Kaufman K, Scheer KN, et al. : Pediatric mental health presentations and boarding: first year of the COVID-19 pandemic. Pediatrics 2022; 12:751–760 [DOI] [PubMed] [Google Scholar]
- 8.Gallagher KAS, Bujoreanu IS, Cheung P, et al. : Psychiatric boarding in the pediatric inpatient medical setting: a retro-spective analysis. Hosp Pediatr 2017; 7:444–450 [DOI] [PubMed] [Google Scholar]
- 9.The “patient flow standard” and the 4-hour recommendation. Jt Comm Perspect 2013; 33:3–4 [PubMed] [Google Scholar]
- 10.American College of Emergency Physicians: ACEP psychiatric and substance abuse survey 2008. 2008. Available from: http://newsroom.acep.org/statistics_and_reports?o=25
- 11.Bender D, Pande N, Ludwig M: A literature review: Psychiatric Boarding. Washington, DC: US Department of Health and Human Services; 2008 [Google Scholar]
- 12.Claudius I, Donofrio JJ, Lam CN, Santillanes G: Impact of boarding pediatric psychiatric patients on a medical ward. Hosp Pediatr 2014; 4:125–132 [DOI] [PubMed] [Google Scholar]
- 13.Leyenaar JK, Freyleue SD, Bordogna A, et al. : Frequency and duration of boarding for pediatric mental health conditions at Acute care hospitals in the US. JAMA 2021; 326:2326–2328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salehi L, Phalpher P, Valani R, et al. : Emergency department boarding: a descriptive analysis and measurement of impact on outcomes. CJEM 2018; 20:929–937 [DOI] [PubMed] [Google Scholar]
- 15.Dalkey N, Helmer O: “An experimental application of the DELPHI method to the use of experts”. Manage Sci 1963; 9:458–467 [Google Scholar]
- 16.Murphy MK, Black NA, Lamping DL, et al. : Consensus development methods, and their use in clinical guideline development. Health Technol Assess 1998; 2:i–iv [PubMed] [Google Scholar]
- 17.Nulty DD: “The adequacy of response rates to online and paper surveys: what can be done?”. Assess Eval High Educ 2008; 33:301–314 [Google Scholar]
- 18.Fincham JE: Response rates and responsiveness for surveys, standards, and the Journal. Am J Pharm Educ 2008; 72:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vogel C, Zwolinsky S, Griffiths C, et al. : A Delphi study to build consensus on the definition and use of big data in obesity research. Int J Obes 2019; 43:2573–2586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Slade SC, Dionne CE, Underwood M, Buchbinder R: Standardised method for reporting exercise programmes: protocol for a modified Delphi study. BMJ Open 2014; 4: e006682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Henderson EJ, Rubin GP: Development of a community-based model for respiratory care services. BMC Health Serv Res 2012; 12:193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Diamond IR, Grant RC, Feldman BM, et al. : Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol 2014; 67:401–409 [DOI] [PubMed] [Google Scholar]
- 23.Brahmbhatt K, Mournet AM, Malas N, et al. : Adaptations made to pediatric consultation-liaison psychiatry service delivery during the early months of the COVID-19 pandemic: a North American multisite survey. J Acad Consult Liaison Psychiatry 2021; 62:511–521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Monroe KK, Rappaport LG, Oesch J, Kullgren KA, Malas N: The Epidemic within the pandemic: pediatric mental health demands in the setting of COVID-19. Clin Pediatr (Phila) 2022; 61:228–231 [DOI] [PubMed] [Google Scholar]
- 25.Leith T, Brieger K, Malas N, et al. : Increased prevalence and severity of psychiatric illness in hospitalized youth during COVID-19. Clin Child Psychol Psychiatry 2022; 27:804–812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Radhakrishnan L, Carey K, Hartnett KP, et al. : Pediatric emergency department visits before and during the COVID-19 pandemic - United States, January 2019-January 2022. MMWR Morb Mortal Wkly Rep 2022; 71:313–318 [DOI] [PubMed] [Google Scholar]
- 27.American Academy of Child and Adolescent Psychiatry: Workforce issues. Available from: https://www.aacap.org/aacap/Resources_for_Primary_Care/Workforce_Issues.aspx Last
- 28.Nasa P, Jain R, Juneja D: Delphi methodology in healthcare research: how to decide its appropriateness. World J Methodol 2021; 11:116–129 [DOI] [PMC free article] [PubMed] [Google Scholar]


