Peripheral vascular disease commonly affects the arteries supplying the leg and is mostly caused by atherosclerosis. Restriction of blood flow due to arterial stenosis or occlusion often leads patients to complain of muscle pain on walking (intermittent claudication). Any further reduction in blood flow causes ischemic pain at rest, which affects the foot. Ulceration and gangrene may then supervene and can result in loss of the limb if not treated. TheFontaine score is useful when classifying the severity of ischemia (see box).
Although many patients with claudication remain stable, about 150 to 200per million of the population progress to critical limb ischemia (Fontaine IIIor IV) each year. Many patients with critical limb ischemia can undergorevascularization, which has a reasonable chance of saving the limb. A recent audit by the Vascular Surgical Society found a success rate of over 70% for these patients. Many patients, however, still require major amputation.Rehabilitation of elderly patients after amputation can prove difficult and costly.
INTERMITTENT CLAUDICATION
History and examination
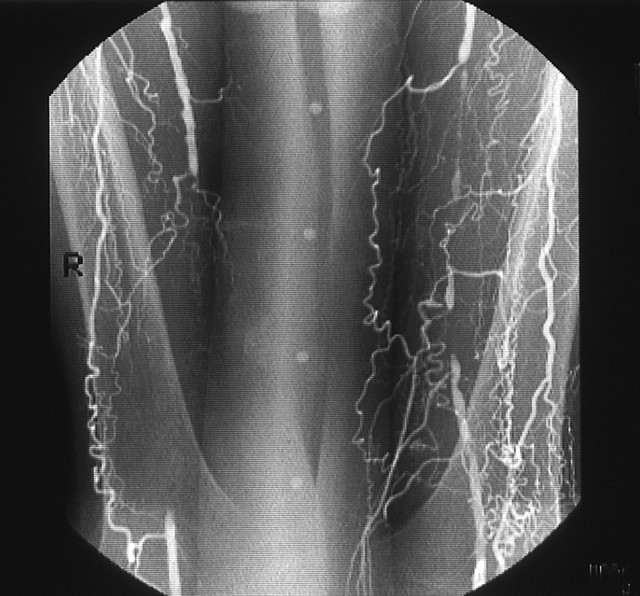
A history of muscular, cramp like pain on walking that is rapidly relieved by resting, together with absent pulses, strongly supports the diagnosis of intermittent claudication. Disease of the superficial femoral artery in the thigh (figure 1) results in absent popliteal and foot pulses and often causes calf claudication. Disease of the aorta or iliac artery results in a weak or absent femoral pulse, often associated with a femoral bruit (figure2). Disease at this level may cause calf, thigh, or buttock claudication.
Figure 1.
Angiogram showing bilateral occlusions of superficial femoral arteries in thighs. Collaterals arising from the profunda femoris artery can functionally bypass this occlusion.
Figure 2.
Method of palpating the femoral pulse in the skin crease of groin.Counterpressure on the lower abdomen pushes the skin crease toward the inguinal ligament and reduces the risk of missing the pulse.
The dorsalis pedis artery lies superficially on the dorsum of the foot, although its position varies considerably(figure3)figure 3. The posterior tibial artery lies deeper behind the medial malleolus. Many healthy people have only one foot pulse. The popliteal pulse can be difficult topalpate in muscular patients (figure4). A prominent popliteal pulse suggests the possibility of apopliteal aneurysm.
Figure 3.
Method of palpating doralis pedis (A) and posterior tibial. Examine pulses from the foot of the bed, keeping the fingers flat for the dorsalis pedis andusing the fingertips for the posterior tibial while applying counter pressure with the thumb.
Figure 3.
Method of palpating doralis pedis (B) pulses. Examine pulses from the foot of the bed, keeping the fingers flat for the dorsalis pedis and using the fingertips for the posterior tibial while applying counter pressure with the thumb.
Figure 4.
Method of palpating popliteal artery with patient's knee slightly flexed.Use thumbs to apply counter pressure while palpating the artery, which lies deep in the popliteal fossa, with fingers.
Differential diagnosis
The pain of nerve root compression can be mistaken for vascularclaudication. A careful history can usually distinguish nerve root compression, especially sciatica due to compression of the lumbosacral root.Compression of the cauda equina due to spinal stenosis, however, can be more difficult to diagnose. This condition usually causes pain that radiates down both legs. Although the pain is made worse by walking, it also comes on after prolonged standing and is not rapidly relieved by rest, unlike vascularclaudication.
Investigation
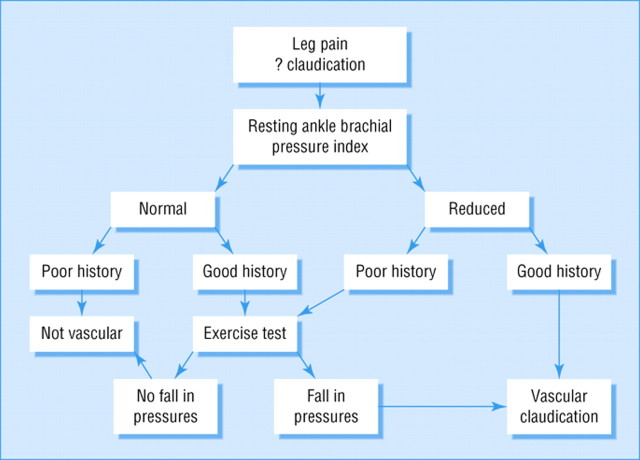
Many causes of leg pain can occur in the presence of asymptomatic peripheral vascular disease. Therefore, the absence of pulses does not necessarily imply a causal link. Furthermore, the presence of pulses at rest does not exclude symptomatic peripheral vascular disease, A good history together with an ankle branchial systolic pressure index of less than 0.9confirms the diagnosis (figure5).
Figure 5.
Algorithm for investigation of suspected intermittent claudication
Exercise testing provides an objective measurement of walking distance and highlights other exercise limiting conditions, such as arthritis and breathlessness. Exercise testing takes time, however, and many patients find it difficult or impossible to walk on a treadmill. Only those with a good history of claudication and normal resting ankle brachial systolic pressure indices require an exercise test.
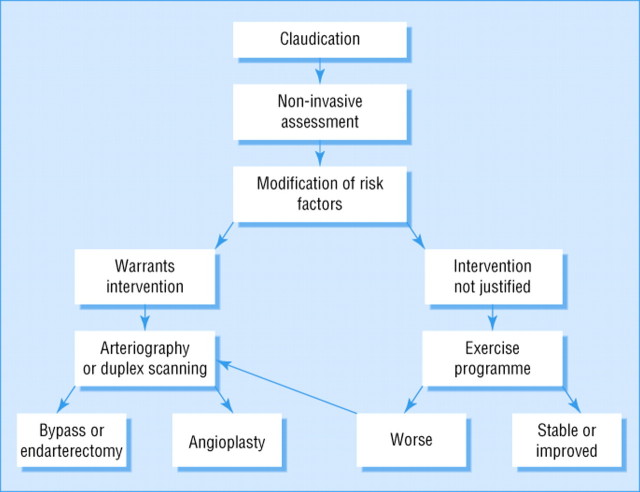
Duplex ultrasound scanning is useful for delineating the anatomic site of disease in the lower limb (figure6). Many hospitals still use arteriography for this purpose or when the results of duplex scanning are equivocal. This invasive and expensive investigation should not be requested unless there is a plan to proceed with revascularization, if possible.
Figure 6.
Algorithm for treatment of intermittent claudication
Principles of treatment
Intermittent claudication seems a relatively benign condition, although severe claudication may preclude patients from manual work (see box). The risk of generalized vascular disease is probably more important. Patients with claudication have three times higher risk of death compared with age matched controls. Modification of risk factors is therefore vital to reduce death from myocardial infarction and stroke. All patients should be advised to stopsmoking and participate in regular exercise. They should also be screened for hyperlipidemia and diabetes. Patients with peripheral vascular disease benefit from regular podiatric care, and those with diabetes should be seen in a foot clinic. Obesity reduces exercise capacity, and losing weight will improve the walking distance.
Drug treatment
All patients with peripheral vascular disease benefit from taking aspirin(75 to 300 mg/day) because this reduces the risk of cardio-vascular events.Patients who are intolerant of aspirin should take dipyridamole (200 mg twice daily) or clopidrogrel bisulfate (75 mg/day). Naftidrofuryl, currently available in the United Kingdom, may improve the walking distance of patients with moderate claudication (<500 m [<550 yd]), but evidence to support its use is controversial, and its effect on the outcome of the disease is not known.
Exercise programs
A recent meta-analysis of 21 supervised exercise programs showed that training for at least 6 months, by walking to near-maximum pain tolerance, significantly improved pain free and maximum walking distance(figure 7). The only controlled trial comparing an exercise program with percutaneous transluminal angioplasty found that exercise was better. Exercise programs are cheaper than percutaneous transluminal angioplasty or surgery, although long-term compliance seems poor.
Figure 7.
Treadmills can be used for objective measurement of walking distance and for exercise training
Endovascular techniques
The number of percutaneous transluminal angioplasties performed for claudication has risen steeply in recent years. In some situations, endovascular techniques have virtually replaced conventional surgery.Percutaneous transluminal angioplasty seems best suited for stenoses or shortocclusions of the iliac and superficial femoral vessels, with 1-year patency rates of 90% and 80% respectively (figure8)figure8figure 8.Angioplasty carries a small but definite risk of losing the limb because of thrombosis or embolization, and patients should be informed of this risk.
Figure 8.

Short occlusion of left popliteal artery (A), treated by percutaneoustransluminal angioplasty.
Figure 8.

Short occlusion of left popliteal artery. The balloon catheter is passed through the occlusion over a guidewire and inflated (B).
Figure 8.

Short occlusion of left popliteal artery. The balloon catheter is passedthrough the occlusion over a guidewire and inflated (B).
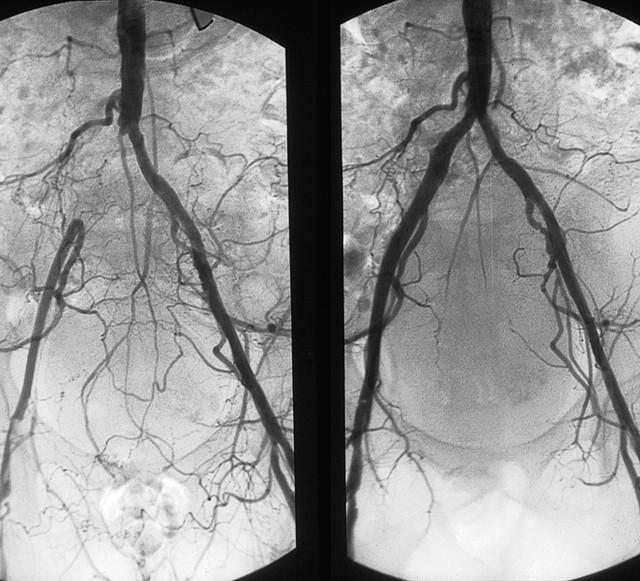
Metallic stents push back the atheroma and improve on the initial lumengain after angioplasty alone (figure9). The indications for iliac stents include a residual stenosisor dissection after angioplasty and long occlusions, but there seems little evidence to justify their routine use. Deployment of stents more distally has produced disappointing results due to high restenosis rates.
Figure 9.
Occlusion of the right common iliac artery before (left) and after (right) insertion of stent
Surgery
The role of surgical bypass grafting for longer arterial occlusions remains poorly defined because of a lack of proper trials comparing it with percutaneous transluminal angioplasty and conservative treatment. Polyester(Dacron) aortobifemoral bypass grafts have 5-year patency rates of over 90%but are associated with a mortality of up to 5%. Complications include graft infection and postoperative impotence. Femoropoliteal bypass grafting, using autologous long saphenous vein, polyester, or polytetrafluoroethylene(Gore-Tex) yields patency rates of less than 70% at 5 years. The early patency of prosthetic grafts seems similar to that of vein grafts, although the long-term results seem less good. Femoropopliteal bypass grafts should rarely be used for patients with claudication.
CRITICAL LIMB ISCHEMIA
History and examination
Patients with critical limb ischemia often describe a history of deteriorating claudication, progressing to nocturnal rest pain. Ulceration or gangrene commonly results from minor trauma. Nocturnal rest pain often occurs just after the patient has fallen asleep, when the systemic blood pressure falls, further reducing perfusion to the foot. Hanging the foot out of bed increases perfusion and produces the typical dusky red hue due to loss of capillary tone (figure 10).Elevation causes pallor and venous guttering. Inspect the foot carefully for ulceration under the heel and between the toes. Swelling suggests deep infection. If you can palpate foot pulses, consider an alternative cause of pain, such as gout. Patients with critical limb ischemia require urgent referral to a vascular surgeon.
Figure 10.

Critically ischemic foot displaying typical dusky red hue on dependency (ischemic rubor)
Investigation
The ankle brachial systolic pressure index is usually less than 0.5.Arterial calcification may result in falsely increased pressures, and caution is needed when relying on Doppler pressures alone, especially in patients with diabetes. All patients with critical limb ischemia should ideally have arteriography with a view to endovascular treatment, if feasible. Duplex scanning may be used instead of angiography and for mapping of the longsaphenous vein before distal bypass surgery. Department Doppler or pulse-generated runoff can help to determine the most suitable artery to receive a distal bypass graft if these cannot be identified by angiography.
Principles of treatment
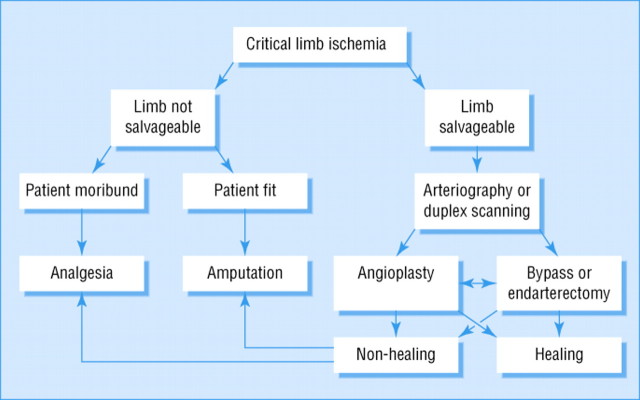
The same principles and techniques used to treat claudication also apply to critical limb ischemia. Critical limb ischemia, however, is usually caused by multilevel disease involvement, which means that success rates are lower.Treatment focuses on saving the limb(figure 11), although modification of risk factors remains important.
Figure 11.
Algorithm for treatment of critical limb ischemia
Endovascular treatment
Percutaneous transluminal angioplasty or stenting of proximal diseaseinvolvement may relieve ischemic rest pain, but healing of ulceration or gangrene usually requires restoration of foot pulses. This may necessitate extensive angioplasty of the superficial femoral, popliteal, and tibialarteries. Good results have been reported using subintimal angioplasty.Endovascular treatment can also reduce the magnitude of subsequent surgery.
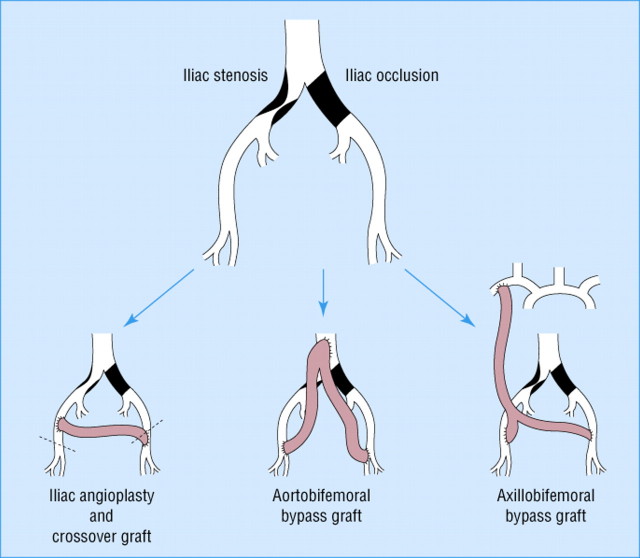
Surgery
Patients with a pattern of arterial disease considered unsuitable for endovascular treatment will usually require surgery(figure 12). Fit patients with proximal disease involvement benefit greatly from aortobifemoral bypass grafting. In unfit patients, the options include cross-femoral bypass for unilateral disease or axillobifemoral bypass for bilateral disease. These extra-anatomic procedures have lower patency rates. Many patients with distal disease will require bypass grafting to the popliteal or crural arteries below the knee. Autologous vein grafts give the best patency rates (70% at 1 year).Postoperative duplex surveillance may improve patency by permitting the detection and treatment of vein graft stenoses before occlusion occurs.
Figure 12.
Surgical treatment options for aortoiliac disease
Amputation
Patients with unreconstructable peripheral vascular disease, fixed flexiondeformities, or extensive tissue loss usually require a major amputation.Preservation of the knee joint has enormous advantages for wearing artificial limbs and subsequent mobility. There is little point in risking a non healing, below-the-knee amputation, however, if the patient seems unlikely to walk again. Similarly, a patient with good prospects of wearing an artificial limb will fare better with an above-the-knee amputation, if below-the-knee amputation seems unachievable. Local amputation of ulcerated or gangrenous toes will not heal without revascularization.
Pain relief
Critical limb ischemia causes severe pain that requires narcotic analgesia to provide relief (see box). A slow-release opiate such as morphine seems a good option. Opiates can be supplemented by nonsteroidal anti-inflammatory drugs if these are not contraindicated. Apart from rehydration, adequate analgesia alone may be the best treatment for patients with dementia or other severe comorbidity. If opiate analgesia remains inadequate, then lumbarsympathectomy (surgical or chemical) or spinal cord stimulation may help.
About 20% to 30% of patients with critical limb ischemia have unreconstructable disease. A meta-analysis of 6 randomized trials of a stableprostacyclin analogue found that infusion of this drug reduced the death and amputation rate. Phantom limb pain may complicate major amputation.Amitriptyline hydrochloride, carbamazepine, transcutaneous nerve stimulation, and acupuncture can help in this situation.
Table 1.
Fontaine classification of chronic leg ischemia
| Stage I | Asymptomatic |
| Stage II | Intermittent claudication |
| Stage III | Ischemic rest pain |
| Stage IV | Ulceration or gangrene, or both |
Table 2.
Factors that may influence the decision to treat claudication
| For | Against |
|---|---|
| Severe symptoms | Short history |
| Job affected | Continued smoking |
| No better after exercise training | Severe angina or chronic obstructive airway disease |
| Stenosis or short occlusion | Long occlusion |
| Proximal disease | Distal disease |
| Unilateral disease | Multilevel disease |
Methods of pain relief for critical limb ischemia
Slow-release opiate analgesia-for example, morphine sulfate
Prostacyclin analogues-for example, iloprost or prostaglandin E1(alprostadil)
Chemical or surgical lumbar sympathectomy
Dorsal column spinal stimulation
This article was previously published in BMJ 2000 ; 320 :854-857