Abstract
Remedies are not useless because they fall short of their full scope. It is better to keep a man on the edge of a precipice, if you cannot pluck him away from it, than to let him fall over. And many diabetic patients are kept in this predicament of dangerous safety.
Lectures on the Principles and Practice of Physic, 1836-1837 SirThomas Watson
Among the remarkable medical accomplishments of the past century, insulin's introduction in 1922 appears miraculous. Emaciated youngsters with diabetes mellitus, kept barely alive through “starvation diets” were resurrected within weeks of starting an insulin regimen. The 1923 Nobel prize awarded to Banting and Mcleod expressed only partially the prevailing enthusiasm and gratitude.1 Yet, as ensuing decades have taught, the legacy of insulin has had a blackened lining. Delayed diabetic sequelae include damage to the eyes, kidneys, and blood vessels, and the daily burden of living with a chronic illness often weighs heavily on patients.2,3,4
This central tension—between exultation over therapeutic success and concern for dreaded complications—underwrites the modern story of diabetes. Indeed, a similar tension of “dangerous safety” exists for many health care technologies, from neonatal intensive care to bone marrow transplantation to the care of human immuno-deficiency viral disease. In each instance, patients' perspectives on their condition and health care, adopted early in the course of illness, can over time lead to long-term emotional and ethical predicaments.
To explore this process, I use a historical case study to describe one patient's experiences with both diabetes and the style of care provided by the renowned Joslin Diabetes Clinic in Boston. From the mid-1910s until his death in 1962, Elliott P Joslin, MD, was an international leader in diabetic care ;his protégée,Priscilla White, MD (1900-1989), became an expert on children and pregnant women with diabetes (figure 1).Joslin's vision of ideal diabetic management—marked by a strongProtestant work ethic, a zealous attention to detail, and high regard forself-control—permeated his clinic. Although some patients rebuked his vision, others accepted his philosophy and, unwittingly, the predicaments entailed by his outlook on illness and care.
Figure 1.
Drs Joslin (front row, center), White (front row, right), and the JoslinDiabetes Clinic staff
Summary points
Insulin and other modern therapeutic innovations have changed type 1diabetes mellitus (formerly juvenile diabetes) from an acutely lethal disease into a chronic and often debilitating condition
This process of therapeutic change—which has altered many diseases over the past century—generates states of “dangeroussafety”
For some patients, the attitudes adopted early in their illness toward this dangerous safety can lead to emotional and ethical predicaments
These predicaments frequently involve issues of control, stigma, risk, and responsibility
As diagnostic and therapeutic technologies advance further, such predicaments may increase, compelling a reevaluation of fundamental attitudes toward illness and death
VIRTUOUS VERSUS PROFLIGATE PATIENTHOOD
In the winter of 1940, 15-year-old John Hansen (a pseudonym) began to lose weight and feel poorly. His physician recognized the classic symptoms and, finding glucose in the young man's urine, referred him immediately to Joslin.John was seen the next day in Joslin's office and then sent to DeaconessHospital in Boston.5 The week-longhospitalization marked the beginning of John's career as a diabetic, as he learned about his disease and how to adjust his diet and to administer insulin. 6 In addition, his physicians inculcated values that would prove defining throughout John's life.
Two weeks after discharge, John's mother wrote to White that her son's“attitude remains excellent, with a continued desire to follow his diet rigidly.... We are not discouraged because we realize that there is much to be thankful for, especially since we have you to guide us in the right direction.” 5White replied graciously, emphasizing that John's combination of attitude, cooperation, and knowledge—cardinal virtues in the mortal and moralstruggle with diabetes—would ultimately determine his outcome.
For the next 2 uneventful years, according to White's notes, the results ofJohn's periodic examinations and blood glucose tests were“perfect,” and he remained “really in fine condition,”even soliciting her counsel on choosing a college. Then, when he was 18 years old, John failed to live up to the Joslin clinic's strict standard. As White stated curtly, John's test result 3 days earlier was “not as good a test as you should have and I don't think you have been trying quite as hard as you should.” White instructed him to increase his insulin dose and added,“I shall want to see you in a month and with better tests.”5
Notably, John soon penned 2 letters that reestablished his credentials as a“good patient.” In the first, written in December 1942, he toldWhite that he had recently disclosed his diabetes on a draft questionnaire and that he needed a letter attesting to his diagnosis. A week later, John again wrote that “due to the current food shortages, my Mother has had difficulty in obtaining meat and butter as required on my diet.” He asked White to suggest substitute foods. White responded first with a note to the draft board, reassuring John that, with this in hand, “I am sure they will send you home at once.” Several days later, she sent instructions on substituting margarine for butter, fish or nuts for meat, and entrusted him to figure the vegetables and fruits exchanges according to rule she had been taught.5
A year passed, and John, attending his college of choice, returned toBoston to be examined. “You are doing splendidly,” White enthused subsequently. “Take no chances with yourself,” she continued,“but keep on as you are doing. I do think it advisable for you to be checked up at least every 3 to 4 months. It does not take very long. You can bring a book with you if you need to wait.”5
SAFETY VERSUS DISTANT DANGER
In the summer of 1945, John married. Two years later, he informed White of plans to pursue a doctorate in chemistry before broaching some harrowing questions. Noting that he would not complete the doctorate until his late 20s,he wondered whether his “life expectancy is long enough to warrant my spending another 4 years in school [or would it] seem wiser for me to accept a position now, and thus be able to provide my wife with a home and family for a maximum length of time.” He also sought advice regarding “myhaving children. That is, what is the probability of a child of mine being diabetic (there is no record of diabetes in my wife's family) ?”Finally, he requested some medical writing on diabetes because his current knowledge was “limited to what I've gained from Dr Joslin's DiabeticManual,” He was particularly keen “to gain a more technical knowledge, especially concerning what parts of my body will be most likely to fail in later life, and the detrimental (if any) effects of prolonged use of insulin.”5
White retorted that John's “life expectancy is certainly long enough to warrant your spending another 4 years in school.” She stated that the life span of a person with diabetes was three-fourths the normal length,“and of course treatment will be improving during the next few years.” She also offered reassurance that “there is no probability of diabetes in your children providing your wife's family history is absolutely correct [that is, `untainted by diabetes'].” Finally, she recommended the most recent textbook that Joslin and colleagues had written on diabetes.5,7
NORMAL VERSUS ABNORMAL PERSONHOOD
After his first year of graduate school, John worked the summer of 1948 at a manufacturing plant to learn how his research was applied in industry. On arrival, he had a physical examination. “A doctor (of questionable mentality),” he told White, “placed a stethoscope in the center of my chest for fully 3 seconds, and then after checking me for hernia was about to pronounce me a perfect physical specimen until I was naive enough to tell him I was diabetic. Visibly shaken, the doctor made several hurried phone calls while watching me to see when I would fall into coma.” John was told that company policy forbid hiring diabetics. After hasty negotiation, he was retained, but instead of working throughout the plant, he “would be confined within the safe walls of the laboratory.”5
John fumed : he was “not ashamed to be a diabetic, and until now I have never hesitated to admit it....My health is perfect, I feel fine.... Yet, because some moron employed by the mill has gone into coma several times, they believe that all diabetics will do likewise.” He asked White to send the company physician a letter to clear up his misconceptions and thus “make it possible for capable and intelligent diabetics to secure jobs in the future—jobs that they have no right to be denied.” Mentioning a newspaper article that advocated prohibiting diabetic persons from obtaining driver's licenses, he summed up his feelings : “This type of hog-wash makes my blood boil ! I see no reason for the thousands of sensible diabetics to be looked upon as `industrial hazards' merely because of the mistakes of a few, too idiotic to care properly for themselves.”5
White replied evenhandedly, explaining why such discrimination existed but was no longer appropriate. She enclosed a letter to the company physician, telling him that antibiotic treatment of infection in patients with diabetes was effective, “so that no longer do we fear infection as we did formerly.” White further testified that John “is an extremely intelligent and cooperative patient, recognizes his insulin reactions, and I think the hazards from this point of view [are] also very slight.”5
This exchange of letters bespoke a deep mutual understanding, dating back to John's first hospital stay, of the key principles of diabetic management—knowledge, attitude, and adherence—preached by theJoslin staff and believed by John. Having built his diabetic identity as an intelligent and conscientious patient, John took knowledge to be a talisman, attitude a defensive weapon, and adherence to regimen his protective armor.Yet, for John, like so many others, the final stages of his life were fraught with difficulty.
SUCCESS VERSUS THERAPEUTIC FAILURE
After returning to graduate school, John was healthy for a decade. In 1959,his fortunes changed drastically for the worse. He wrote Joslin “toobtain any possible advice or help from your clinic which may help prevent my becoming blind.” He had suffered a “massive hemorrhage” in 1eye, followed shortly by hemorrhage in the other. He told Joslin that he“would greatly appreciate your advice or comments as to anything I can possibly do to save what sight I have left.” Drawing his letter to a close, John added “some personal comments.” As a chemical engineering professor, he fully appreciated “the tremendous research problem involved in this blood vessel damage.” What shocked John, however, was his “ownnaïveté about this problem. From the meager statistics I now can find, I should have expected this development.” Pointing a recriminating finger, he asserted that “I do not fear the truth, but I do fear ignorance, and therefore I resent very deeply not being informed truthfully.” Contemplating“the personal hell I have gone through trying to rationalize my coming blindness,” John was “horrified to think of all the others having to face the same problem with no warning. Yet, I hasten to add, I have been grateful for every day of life I have had since first becoming diabetic. I've always regarded each day as a sort of bonus.”5
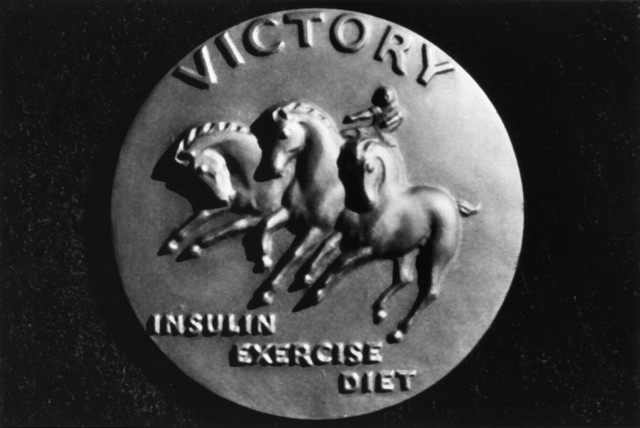
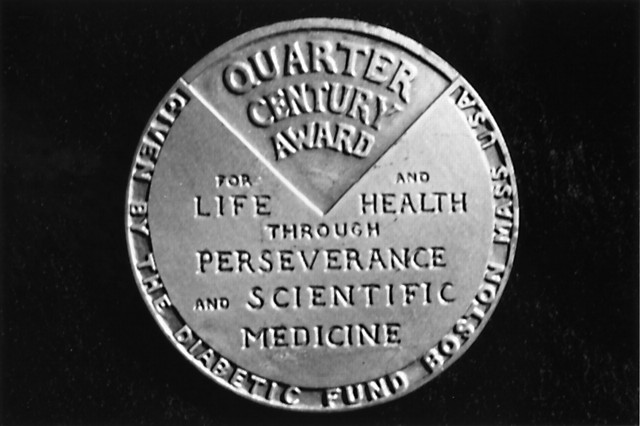
Joslin, who for decades had warned about the endangerment of vision by long-standing diabetes,8 responded to John,“although what I write will not restore your eye-sight, I think you willbe thankful to learn what is going on.” He informed John that the JoslinDiabetes Center had recently “spent over $200,000 on research for a single year” and that the center cared for “90 patients who have been awarded our Quarter Century Victory Medal because their eyes were certified perfect by [an] expert ophthalmologist.” The medal(figure2)figure 2,established in 1947 and rewarded to patients who remained free of diabetic complications 25 years after diagnosis, was intended by Joslin to symbolize scientific progress. Joslin reiterated his caveat that “what I write does not bring back your eye-sight, but it shows we are not idle, and I feel reassured that our patients are living 3 times as long as formerly and the children... have lived some 24 years compared with 1 year at the beginning of the century,” He ended by offering his advice to John's physicians regarding how best to manage his diabetes and eye disease.5
Figure 2.
The Quarter Century Victory Medal
Figure 2.
The Quarter Century Victory Medal
Three years later, John sought to save his vision through an experimental operation that removed part of his pituitary gland.9 Although this dubious surgical intervention was soon discredited, his eyesight afterward seemed to improve. John's overall condition, however, continued to deteriorate, and when he died a few years later, among the factors cited as leading to his death was the diabetes insipid us that the operation had caused.5
THE PREDICAMENTS OF DANGEROUS SAFETY
Being mortal, we all live in states of dangerous safety, our lives distinguished by the degree of hazard, our awarencess of potential peril, and our attitude toward risk. John's engagement with his illness highlights 4challenges—involving control, stigma, risk, and responsibility—that arise when living in the shadow of a threat. First, how can a patient live with a danger that eludes full control, and how can a sense of safety be enhanced without lapsing into false reassurances, magical thinking, or judgmental moralizing ? Second, how can health care mitigate the stigma that accompanies life-threatening conditions, reducing its detrimental effects on self-concept and preventing social injustice ? Third, how can risk assessment be incorporated into a vibrant care plan, allowing patients to move ahead joyously with life while addressing the threat of future dangers ?Finally, how should responsibility for the sequelae of chronic disease be apportioned between patients and physicians, fostering patient empowerment while avoiding antagonism, blame, or inappropriate abdication of professional responsibility ?
These predicaments, which occurred throughout John's life, intensified when his eyesight was threatened. For John, the crisis prompted his protest—not fully supported by his medical record—that he had been left uninformed. Nevertheless, he continued to look to his physicians for guidance and hope, striving poignantly in the final sentences of his last letter to strike a balance between outrage and obligation, gratitude and grief. Joslin's response, on the other hand, bespoke his abiding faith :taking the longer view, he accepted the painful misfortunes of 1 patient by focusing on the trend toward better outcomes for many people with diabetes and by working devotedly to improve clinical care for all.
Recounting how this patient and physicians struggled to make sense of a threatening chronic illness at a personal level illuminates our collective struggle with the frustration associated with chronic debilitating conditions.Reacting to this frustration, out culture has typically sought further technical innovation, desiring to remove the root causes of suffering and death. Yet, given advances in diagnostics, we are likely to become more aware of the specific diseases that threaten us. Advances in medical therapy will keep us living longer in states of dangerous safety. Perhaps, then, we pursue a goal that guarantees frustration, as technology shifts but never eradicates the predicaments of our mortality. If so, our fundamental perspective on health needs to change, accommodating the inescapable threats of illness and death into the concept of a well-lived life.10,11
Acknowledgments
This study was approved by the human subjects review committee of theJoslin Diabetes Center, Boston, and all primary historical materials are from their archives. My enduring thanks to Jim and Susan Warram, who pointed me in the right direction and graciously helped with all that followed. I am solely responsible for the facts and views presented in this article.
Funding : This research was supported by Dissertation AwardHS07476-01 and National Research Service Award grant T32 HS00009 from theAgency for Healthcare Research and Quality and the Robert Wood JohnsonClinical Scholars Program.
Competiting interests : None declared
West J Med 2000 ; 173 : 64-67
References
- 1.Bliss M. The Discovery of Insulin. Chicago: University of Chicago Press ; 1982.
- 2.Charmaz K. Good Days, Bad Days : The Self in ChronicIllness and Time. New Brunswick, NJ : Rutgers Univ. Press ;1991.
- 3.Feudtner C. The want of control : ideas, innovations, and ideals in the modern management of diabetes mellitus. Bull HistMed 1995. ; 69 :66-90. [PubMed] [Google Scholar]
- 4.Feudtner C. A disease in motion : diabetes history and the new paradigm of transmuted disease. Perspect Biol Med 1996. ; 39 :158-170. [DOI] [PubMed] [Google Scholar]
- 5.Archival Record 18899, 1960 1940.Boston : Joslin Diabetes Center Archives.
- 6.Corbin J, Strauss A. Managing chronic illness at home : three lines of work. In : Conrad P, Kern R, eds. The Sociology of Health andIllness : Critical Perspectives. 3rd ed. New York : St Martin'sPress ; 1990. : 122-135.
- 7.Joslin EP, Root HF, White P, et al. The treatment of diabetes mellitus. Philadelphia : Lea & Febiger ;1946.
- 8.Joslin EP. The Treatment of DiabetesMellitus. 3rd ed. Philadelphia : Lea & Febiger ;1923.
- 9.Poulsen JE. Diabetes and anterior pituitary insufficiency : final course and postmortem study of a diabetic patient with Sheehan's syndrome.Diabetes 1966. ; 15: 73-77. [DOI] [PubMed] [Google Scholar]
- 10.Dubos R. Mirage of Health : Utopias, Progress, andBiological Change. New Brunswick : Rutgers University Press ;1987.
- 11.Callahan D. The Troubled Dream of Life : In Search of aPeaceful Death. New York : Touchstone ;1993.