Abstract
Background
The number of people aged greater than 65 years per 100 people aged 20–64 years is expected to almost double in The Kingdom of Saudi Arabia (KSA) between 2020 and 2030. We therefore aimed to quantify the growing non-communicable disease (NCD) burden in KSA between 2020 and 2030, and the impact this will have on the national health budget.
Methods
Ten priority NCDs were selected: ischemic heart disease, stroke, type 2 diabetes, chronic obstructive pulmonary disease, chronic kidney disease, dementia, depression, osteoarthritis, colorectal cancer, and breast cancer. Age- and sex-specific prevalence was projected for each priority NCD between 2020 and 2030. Treatment coverage rates were applied to the projected prevalence estimates to calculate the number of patients incurring treatment costs for each condition. For each priority NCD, the average cost-of-illness was estimated based on published literature. The impact of changes to our base-case model in terms of assumed disease prevalence, treatment coverage, and costs of care, coming into effect from 2023 onwards, were explored.
Results
The prevalence estimates for colorectal cancer and stroke were estimated to almost double between 2020 and 2030 (97% and 88% increase, respectively). The only priority NCD prevalence projected to increase by less than 60% between 2020 and 2030 was for depression (22% increase). It is estimated that the total cost of managing priority NCDs in KSA will increase from USD 19.8 billion in 2020 to USD 32.4 billion in 2030 (an increase of USD 12.6 billion or 63%). The largest USD value increases were projected for osteoarthritis (USD 4.3 billion), diabetes (USD 2.4 billion), and dementia (USD 1.9 billion). In scenario analyses, our 2030 projection for the total cost of managing priority NCDs varied between USD 29.2 billion - USD 35.7 billion.
Conclusions
Managing the growing NCD burden in KSA’s aging population will require substantial healthcare spending increases over the coming years.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-023-10309-w.
Keywords: Aging, Non-communicable Disease, Costs, Saudi Arabia
Background
Life expectancy at birth in The Kingdom of Saudi Arabia (KSA) increased from 70.5 years in 2000 to 74.3 years in 2019 [1]. The number of people aged greater than 65 years per 100 people aged 20–64 years is expected to almost double in KSA between 2020 and 2030 (from 5.3 to 9.5 per 100) [2]. The impact of the world’s aging population on healthcare systems is a matter of international concern and a top priority for KSA. KSA’s economy is also dependent on a few key sectors (e.g., crude oil production, petroleum refining) and a large migrant labor workforce, making it vulnerable to shifts within domestic and global economies. It is critical for KSA to consider how population aging will impact the economic demands of its healthcare system in the future.
A key issue is the management of KSA’s growing burden of age-associated non-communicable disease (NCD). In 2019, NCDs accounted for 67.4% of all disability-adjusted life-years lost in KSA [3]. Ischemic heart disease (IHD), stroke, type 2 diabetes, chronic obstructive pulmonary disease (COPD), chronic kidney disease (CKD), dementia, depression, osteoarthritis, colorectal cancer, and breast cancer accounted for 42.9% of this disability-adjusted life-year burden. In 2011, spending on a similar selection of key NCDs was estimated to account for USD 18.3 billion, or 72.8% of the KSAs total health expenditure [4, 5]. This was equivalent to 2.7% of KSAs gross domestic product in the same year.
These NCDs are also likely to be amenable to public health intervention in KSA. The population in KSA exhibits a high prevalence of NCD risk factors including obesity, tobacco use, physical inactivity, and poor diet. For example, a recent World Bank report on NCDs in KSA indicates between 54.1 and 70.2% of adult females and between 57.5 and 68.3% of adult men are overweight [6]. In 2021, it is estimated that 26.5% of adult men in KSA were using tobacco daily [7]. In the 2013 Saudi Health Interview Survey of 10,735 individuals aged ≥ 15 years, dietary guideline recommendations were met by only 5.2% of individuals for fruits, 7.5% for vegetables, 31.4% for nuts, and 44.7% for fish [8]. In the same survey, 46.5% of women reported being physically inactive [9].
With the growing size of the elderly population, and high prevalence of NCD risk factors, the prevalence of NCDs in KSA will increase leading to a commensurate rise in demand for medical care. We aimed to quantify the growing NCD burden in KSA between 2020 and 2030, and the impact this will have on the national health budget. Our findings will allow KSA to plan for these changes, emphasise the importance of prevention and promotion health policy, and ensure health resources remain adequate into the future.
Methods
Priority non-communicable diseases
IHD, stroke, type 2 diabetes, COPD, CKD, dementia, depression, osteoarthritis, colorectal cancer, and breast cancer were chosen as our priority NCDs based on their large contribution to the disability-adjusted life-year burden in KSA, amenability to public health intervention, and the availability of well-defined cost-of-illness estimates.
Prevalence projections
All priority NCD prevalence projections were based on the population of KSA aged ≥ 15 years. Males and females were split into 5-year age brackets (up to age 85 years with age greater than 85 years considered a single age bracket (i.e., 16–20, 21–25, 26–30, 31–35, 36–40, 41–45, 46–50, 51–55, 56–60, 61–65, 66–70, 71–75, 76–80, 81–85, and > 85 years old). Age- and sex-specific estimates of priority NCD prevalence were taken from the Global Burden of Disease which uses a combination of health data from hospitals, governments, surveys, and other databases around the world and modeling tools to generate estimates for locations and years where data are not available [3]. Prevalence estimates for 2020–2030 were generated using a least squares linear projection of Global Burden of Disease estimates for 2015–2019. Our projected age- and sex-specific prevalence estimates were then multiplied by the age- and sex-specific United Nations population projections [10] for years 2020–2030 to derive the absolute number of people in KSA who may seek care per condition per year.
Treatment coverage
Treatment coverage (i.e., the proportion of people needing treatment for an illness who receive treatment) rates were applied to the projected prevalence estimates for each priority NCD to calculate the number of patients incurring treatment costs for that condition. These were determined based on the severity of the NCD, the ability to detect cases, and the probability that patients with the condition will seek care. Based on these factors, and consistent with previous estimates, [11–18] the following treatment coverage rates were established: 80% for IHD, stroke, diabetes, COPD, dementia, osteoarthritis, colorectal cancer, and breast cancer; 30% for depressive disorders; and 10% for CKD (see Table 1).
Table 1.
Treatment coverage and cost-of-illness estimates for priority non-communicable diseases
| Non-communicable disease | Treatment coverage | Cost of illness, USD (2020) per person treated per year | Cost of illness reference |
|---|---|---|---|
| Ischemic heart disease | 80% | 968 | [21] |
| Stroke | 80% | 2,354 | [21] |
| Diabetes | 80% | 1,955 | [21] |
| Chronic obstructive pulmonary disease | 80% | 5,913 | [20, 27, 28] |
| Chronic kidney disease | 10% | 4,020 | [19, 22, 24] |
| Dementia | 80% | 33,609 | [26] |
| Depression | 30% | 4,097 | [23] |
| Osteoarthritis | 80% | 4,624 | [25] |
| Colorectal cancer | 80% | 2,682 | [21] |
| Breast cancer | 80% | 900 | [21] |
A relatively high treatment coverage target was assigned to IHD, stroke, diabetes, COPD, dementia, osteoarthritis, colorectal cancer, and breast cancer because of the severity of symptoms and ease of detection. On the other hand, people with depression often do not report symptoms or go undiagnosed in primary care settings, [11] and CKD is seriously underdiagnosed in both wealthy and resource-limited countries [12–15]. Therefore, we assigned lower treatment coverage rates for depression and CKD. Treatment coverage rates were assumed to remain constant between 2020 and 2030.
Cost-of-illness
For each priority NCD, the average cost-of-illness (i.e., the value of the resources that are expended as a result of a health problem) was estimated based on published literature [19–28]. Costs were converted to the equivalent USD amount at the time of the study (if not already in USD) using OANDA Currency Converter [29] and then inflated to 2020 USD using the US Bureau of Labor Statistics Consumer Price Index Inflation Calculator [30]. Our final cost-of-illness estimates are shown in Table 1. Cost-of-illness estimates were assumed to remain constant between 2020 and 2030.
Budget impact assessment and scenario analyses
Using our projected prevalence, treatment coverage, and cost-of-illness estimates, the budgetary impacts of the ten priority NCDs in KSA were forecast for 2020–2030. The base-case model adopted the assumptions described above. The impact of changes to the base-case model, coming into effect from 2023 onwards, were also explored. These scenarios were designed to depict the consequences of realistic changes in economic or health policy (e.g., drug price changes, healthcare worker salary changes, changes to public/private healthcare ratio, scale up of NCD screening, implementation of tobacco control and healthy eating initiatives). Scenarios evaluated included a 10% reduction in prevalence for priority diseases with a 2023 prevalence > 1% (i.e., IHD, stroke, diabetes, COPD, CKD, depression, and osteoarthritis); a 10% increase in treatment coverage for low treatment coverage priority diseases (i.e., CKD and depression); and a 10% increase or decrease in the costs associated with NCD management. Each scenario was evaluated individually. No combination of scenarios was considered.
Results
Projected prevalence
The projected prevalence of priority NCDs in KSA between 2020 and 2030 is shown in Table 2. Over this period, the largest changes in annual prevalence were for CKD, diabetes, and osteoarthritis with increases of 1.9, 1.5, and 1.2 million cases, respectively. The prevalence estimates for colorectal cancer and stroke were estimated to almost double between 2020 and 2030 (97% and 88% increase, respectively). The only priority NCD prevalence projected to increase by less than 60% between 2020 and 2030 was for depression (22% increase).
Table 2.
Annual prevalence of priority non-communicable diseases among people aged ≥ 15-years, 2020–30
| Non-communicable disease | 2020 | 2021 | 2022 | 2023 | 2024 | 2025 | 2026 | 2027 | 2028 | 2029 | 2030 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Ischemic heart disease | 1,013,588 (3.9%) | 1,077,936 (4.0%) | 1,142,112 (4.2%) | 1,206,115 (4.4%) | 1,269,947 (4.5%) | 1,333,606 (4.7%) | 1,414,888 (4.9%) | 1,495,915 (5.1%) | 1,576,688 (5.3%) | 1,657,207 (5.4%) | 1,737,471 (5.6%) |
| Stroke | 529,102 (2.0%) | 569,356 (2.1%) | 610,422 (2.2%) | 652,300 (2.4%) | 694,989 (2.5%) | 738,491 (2.6%) | 787,472 (2.7%) | 837,331 (2.8%) | 888,068 (3.0%) | 939,683 (3.1%) | 992,177 (3.2%) |
| Diabetes | 2,690,257 (10.3%) | 2,824,930 (10.6%) | 2,961,859 (10.9%) | 3,101,043 (11.2%) | 3,242,481 (11.6%) | 3,386,176 (11.9%) | 3,545,963 (12.2%) | 3,708,341 (12.6%) | 3,873,307 (12.9%) | 4,040,862 (13.2%) | 4,211,007 (13.6%) |
| Chronic obstructive pulmonary disease | 472,947 (1.8%) | 498,917 (1.9%) | 525,197 (1.9%) | 551,786 (2.0%) | 578,685 (2.1%) | 605,893 (2.1%) | 638,371 (2.2%) | 671,273 (2.3%) | 704,600 (2.3%) | 738,352 (2.4%) | 772,528 (2.5%) |
| Chronic kidney disease | 3,089,066 (11.8%) | 3,245,987 (12.2%) | 3,405,431 (12.5%) | 3,567,398 (12.9%) | 3,731,887 (13.3%) | 3,898,898 (13.7%) | 4,103,037 (14.1%) | 4,310,181 (14.6%) | 4,520,328 (15.1%) | 4,733,478 (15.5%) | 4,949,633 (16.0%) |
| Dementia | 90,854 (0.3%) | 96,567 (0.4%) | 102,299 (0.4%) | 108,052 (0.4%) | 113,825 (0.4%) | 119,617 (0.4%) | 128,207 (0.4%) | 136,827 (0.5%) | 145,475 (0.5%) | 154,153 (0.5%) | 162,861 (0.5%) |
| Depression | 1,130,882 (4.3%) | 1,154,358 (4.3%) | 1,177,957 (4.3%) | 1,201,679 (4.4%) | 1,225,522 (4.4%) | 1,249,488 (4.4%) | 1,274,907 (4.4%) | 1,300,476 (4.4%) | 1,326,195 (4.4%) | 1,352,064 (4.4%) | 1,378,083 (4.4%) |
| Osteoarthritis | 1,744,566 (6.7%) | 1,852,225 (6.9%) | 1,960,589 (7.2%) | 2,069,659 (7.5%) | 2,179,434 (7.8%) | 2,289,914 (8.0%) | 2,411,937 (8.3%) | 2,534,755 (8.6%) | 2,658,371 (8.9%) | 2,782,782 (9.1%) | 2,907,989 (9.4%) |
| Colorectal Cancer | 19,949 (0.1%) | 21,592 (0.1%) | 23,286 (0.1%) | 25,032 (0.1%) | 26,830 (0.1%) | 28,679 (0.1%) | 30,701 (0.1%) | 32,775 (0.1%) | 34,902 (0.1%) | 37,081 (0.1%) | 39,313 (0.1%) |
| Breast cancer | 49,487 (0.2%) | 53,030 (0.2%) | 56,674 (0.2%) | 60,421 (0.2%) | 64,270 (0.2%) | 68,221 (0.2%) | 72,410 (0.2%) | 76,699 (0.3%) | 81,089 (0.3%) | 85,580 (0.3%) | 90,170 (0.3%) |
All values are displayed as absolute prevalence (percentage of population ≥ 15-years-old)
Budget impact assessment
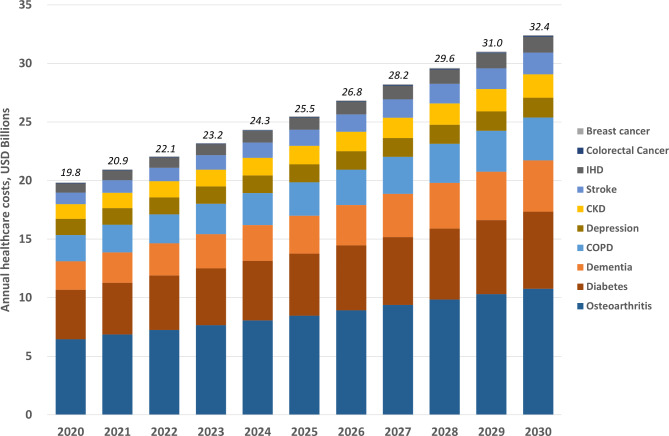
Under our base-case assumptions, it is estimated that the total cost of managing priority NCDs in KSA would increase from USD 19.8 billion in 2020 to USD 32.4 billion in 2030 (an increase of USD 12.6 billion or 63%; Fig. 1 and Supplementary Table 1). The largest USD value increases were projected for osteoarthritis (USD 4.3 billion), diabetes (USD 2.4 billion), and dementia (USD 1.9 billion).
Fig. 1.
Annual healthcare costs for priority non-communicable diseases among people aged ≥ 15-years, 2020–30. Values at top of columns represent the annual sum for all priority non-communicable diseases. IHD, ischemic heart disease; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease
Scenario analyses
With a 10% change in the cost of illness for all priority NCDs, our 2030 projection was estimated to drop to as low as USD 29.2 billion or increase to as much as USD 35.7 billion. A 10% increase in treatment coverage for CKD caused the base-case 2030 cost projection to increase by USD 2.0 billion (to USD 34.4 billion). An equivalent increase in treatment coverage for depression resulted in an increase of USD 0.6 billion (to USD 33.0 billion). Reductions in disease prevalence for osteoarthritis and diabetes had the largest impact on projected costs for 2030 – a 10% reduction in osteoarthritis prevalence equated to a USD 1.1 billion reduction from base-case (to USD 31.3 billion) and a 10% reduction in diabetes equated to a USD 0.7 billion reduction from base-case (to USD 31.8 billion). Table 3 shows the results for all scenarios evaluated.
Table 3.
Scenario analyses for total annual healthcare costs for priority non-communicable diseases among people aged ≥ 15-years, 2023-30
| Scenario | 2023 | 2024 | 2025 | 2026 | 2027 | 2028 | 2029 | 2030 |
|---|---|---|---|---|---|---|---|---|
| Base-case | 23,192,209,970 | 24,333,834,297 | 25,486,341,757 | 26,848,077,253 | 28,222,638,570 | 29,610,025,708 | 31,010,238,665 | 32,423,277,442 |
| Scenarios decreasing costs (in ascending order of 2030 costs) | ||||||||
| 10% reduction in cost of non-communicable disease | 20,872,988,973 | 21,900,450,868 | 22,937,707,581 | 24,163,269,528 | 25,400,374,713 | 26,649,023,137 | 27,909,214,798 | 29,180,949,698 |
| 10% reduction in osteoarthritis prevalence | 22,426,601,814 | 23,527,618,213 | 24,639,256,858 | 25,955,853,696 | 27,284,981,829 | 28,626,641,257 | 29,980,831,980 | 31,347,553,998 |
| 10% reduction in diabetes prevalence | 22,707,206,914 | 23,826,710,195 | 24,956,743,897 | 26,293,488,567 | 27,642,654,109 | 29,004,240,524 | 30,378,247,811 | 31,764,675,970 |
| 10% reduction in chronic obstructive pulmonary disease prevalence | 22,931,193,130 | 24,060,093,340 | 25,199,730,316 | 26,546,102,395 | 27,905,099,466 | 29,276,721,528 | 30,660,968,581 | 32,057,840,626 |
| 10% reduction in chronic kidney disease prevalence | 23,048,800,581 | 24,183,812,459 | 25,329,606,068 | 26,683,135,156 | 28,049,369,313 | 29,428,308,540 | 30,819,952,837 | 32,224,302,203 |
| 10% reduction in stroke prevalence | 23,069,368,905 | 24,202,953,908 | 25,347,269,139 | 26,699,780,578 | 28,064,952,448 | 29,442,784,751 | 30,833,277,485 | 32,236,430,651 |
| 10% reduction in depression prevalence | 23,044,511,659 | 24,183,205,351 | 25,332,767,129 | 26,691,378,419 | 28,062,797,081 | 29,447,023,115 | 30,844,056,522 | 32,253,897,301 |
| 10% reduction in ischemic heart disease prevalence | 23,098,808,407 | 24,235,489,637 | 25,383,067,339 | 26,738,508,356 | 28,106,794,896 | 29,487,926,960 | 30,881,904,548 | 32,288,727,660 |
| Scenarios increasing costs (in descending order of 2030 costs) | ||||||||
| 10% increase in cost of non-communicable disease | 25,511,430,966 | 26,767,217,727 | 28,034,975,932 | 29,532,884,979 | 31,044,902,428 | 32,571,028,278 | 34,111,262,531 | 35,665,605,186 |
| 10% increase in chronic kidney disease treatment coverage | 24,626,303,858 | 25,834,052,684 | 27,053,698,639 | 28,497,498,229 | 29,955,331,143 | 31,427,197,381 | 32,913,096,944 | 34,413,029,832 |
| 10% increase in depression treatment coverage | 23,684,537,671 | 24,835,930,784 | 25,998,257,182 | 27,370,406,703 | 28,755,443,536 | 30,153,367,682 | 31,564,179,140 | 32,987,877,911 |
Scenarios were assumed to begin from 2023. All values are in 2020 USD
Discussion
Managing the growing NCD burden in KSA’s aging population will require substantial increases in healthcare spending over the coming years. We estimated the cost of managing priority NCDs in 2020 was USD 19.8 billion(~ 49% of KSA’s health budget, or 2.7% of KSA’s Gross Domestic Product [4]). This value was projected to increase to USD 32.4 billion by 2030, a 63% increase from costs in 2020. These findings will help KSA plan future health budgets and policy interventions to ensure adequate resources are available to maintain the health of the population.
A global analysis like ours anticipates similarly large increases in NCD costs over time. In 2011, the World Economic Forum estimated that direct and indirect costs would increase globally between 2010 and 2030 by 58% for cancer (from USD 290 billion to USD 458 billion), 20.5% for cardiovascular disease (from USD 863 billion to USD 1.04 trillion), 129% for COPD (from USD 2.1 trillion to USD 4.8 trillion), 49% for diabetes (from USD 500 billion to USD 745 billion), and 140% for mental illness (from USD 2.5 trillion to USD 6.0 trillion) [31]. Further modelling focusing on the negative impacts of NCDs on labor supply and capital accumulation estimates losses in the order of USD 47 trillion worldwide between 2011 and 2030 for cancer, cardiovascular disease, COPD, diabetes, and mental illness [31–33].
We believe a primary-care focused model and multi-sectoral action are needed to promote NCD prevention in KSA. This is envisioned under the New Model of Care program, which is currently being piloted in several areas of KSA [34]. Multi-sectoral action, including working across ministries outside the health sector (e.g., education, media), is also taking shape under the Public Health Authority’s Master Plan for NCD Prevention [6]. Nevertheless, more government funding for preventive and primary care programs is needed. Further monitoring and evaluation are also necessary to ensure the ongoing effectiveness of the abovementioned programs in reducing NCD burden.
There are several limitations to this analysis. Projections, although useful for health policy planning, rely on assumptions. One key assumption is that the parameter data used are accurate. We have used the best pubished data available, along with reasoned assumptions, in order to establish our model parameters. Our models are based on prevalence, treatment coverage, and cost estimates for priority NCDs. This approach may yield different conclusions than one that attempts to enumerate parameter estimates for every NCD. We used a cost-of-illness approach for our budget impact assessment. While this is a commonly used method that sums direct and indirect costs, it is important to acknowledge that the process of estimating cost-of-illness is vulnerable to double counting associated with comorbidities because data on personal medical care costs rarely divide those costs by condition [31]. Therefore, our budget impact results may be overestimated for some or all priority NCDs.
Conclusion
The number of people aged greater than 65 years per 100 people aged 20–64 years is expected to almost double in KSA between 2020 and 2030. We estimate that KSA will need to substantially increase healthcare spending in the coming years to manage the growing burden of NCDs among its aging population. Planning for future health budgets and policy interventions to maintain the health of the population has to be done now.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The World Bank and The Ministry of Economy and Planning, Saudi Arabia do not guarantee the accuracy of the data included in this work. The findings, interpretations, and conclusions expressed are those of the authors, and do not necessarily reflect the views of The Ministry of Economy and Planning, Saudi Arabia or the World Bank, its Board of Directors, or the governments they represent.
Abbreviations
- KSA
The Kingdom of Saudi Arabia
- NCD
Non-communicable disease
- IHD
Ischemic heart disease
- COPD
Chronic obstructive pulmonary disease
- CKD
Chronic kidney disease
Authors’ contributions
DCB led the study design, conducted the analysis, interpreted the findings, and wrote the manuscript. TKL, MA, MMH, RA, CHH, NA, AA, and FK contributed to the study design, supported the analysis, interpreted the findings, and helped finalize the manuscript.
Funding
This work was supported by The Ministry of Economy and Planning, Saudi Arabia and World Bank. Financing for the analysis was provided by The Ministry of Economy and Planning, Saudi Arabia and the Health, Nutrition and Population Reimbursable Advisory Services Program between the World Bank and the Ministry of Finance in Saudi Arabia (P172148).
Data Availability
The data used for the current study are available from the corresponding author upon reasonable request.
Declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO. : Health data overview for the Kingdom of Saudi Arabia. https://data.who.int/countries/682[08/Nov/2023].
- 2.Organisation for Economic Co-operation and Development (OECD). : Old-age dependency ratio. https://data.oecd.org/pop/old-age-dependency-ratio.htm[22 Feb 2023].
- 3.Institute for Health Metrics and Evaluation. : Global Burden of Disease (GBD). http://www.healthdata.org/gbd/2019[12 May 2022].
- 4.The World Bank. : Current health expenditure (% of GDP) - Saudi Arabia. https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS?locations=SA[12 May 2022].
- 5.United Nation Interagency Task Force on NCDs. : The Investment Case for Noncommunicable Disease Prevention and Control in the Kingdom of Saudi Arabia. https://www.undp.org/[12 May 2022].
- 6.Alqunaibet A, Herbst CH, El-Saharty S, Algwaizini A. Noncommunicable Diseases in Saudi Arabia - Toward Effective Interventions for Prevention. http://hdl.handle.net/10986/36546[12 May 2022].
- 7.The World Bank. : Health Nutrition and Population Statistics. https://databank.worldbank.org/source/health-nutrition-and-population-statistics[04 May 2021].
- 8.Moradi-Lakeh M, El Bcheraoui C, Afshin A, Daoud F, AlMazroa MA, Al Saeedi M, Basulaiman M, Memish ZA, Al Rabeeah AA, Mokdad AH. Diet in Saudi Arabia: findings from a nationally representative survey. Public Health Nutr. 2017;20:1075–81. doi: 10.1017/S1368980016003141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ministry of Health - Kingdom of Saudi Arabia. : Saudi Health Interview Survey Results. https://www.healthdata.org/sites/default/files/files/Projects/KSA/Saudi-Health-Interview-Survey-Results.pdf[12 May 2022].
- 10.United Nations. : World Population Prospects. https://www.un.org/en/development/desa/population/publications/database/index.asp[12 May 2022].
- 11.Becker SM. Detection of somatization and depression in primary care in Saudi Arabia. Soc Psychiatry Psychiatr Epidemiol. 2004;39:962–6. doi: 10.1007/s00127-004-0835-4. [DOI] [PubMed] [Google Scholar]
- 12.Australian Bureau of Statistics. : Australian Health Survey 2011-12: Biomedical Results for Chronic Diseases. https://www.abs.gov.au/statistics/health/health-conditions-and-risks/australian-health-survey-biomedical-results-chronic-diseases/latest-release[04 May 2021].
- 13.Coresh J, Byrd-Holt D, Astor BC, Briggs JP, Eggers PW, Lacher DA, Hostetter TH. Chronic Kidney Disease awareness, prevalence, and trends among U.S. adults, 1999 to 2000. J Am Soc Nephrol. 2005;16:180–8. doi: 10.1681/ASN.2004070539. [DOI] [PubMed] [Google Scholar]
- 14.Ene-Iordache B, Perico N, Bikbov B, Carminati S, Remuzzi A, Perna A, Islam N, Bravo RF, Aleckovic-Halilovic M, Zou H, et al. Chronic Kidney Disease and cardiovascular risk in six regions of the world (ISN-KDDC): a cross-sectional study. Lancet Glob Health. 2016;4:e307–319. doi: 10.1016/S2214-109X(16)00071-1. [DOI] [PubMed] [Google Scholar]
- 15.George C, Mogueo A, Okpechi I, Echouffo-Tcheugui JB, Kengne AP. Chronic Kidney Disease in low-income to middle-income countries: the case for increased screening. BMJ Glob Health. 2017;2:e000256. doi: 10.1136/bmjgh-2016-000256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chisholm D, Sanderson K, Ayuso-Mateos JL, Saxena S. Reducing the global burden of depression: population-level analysis of intervention cost-effectiveness in 14 world regions. Br J Psychiatry. 2004;184:393–403. doi: 10.1192/bjp.184.5.393. [DOI] [PubMed] [Google Scholar]
- 17.Ortegon M, Lim S, Chisholm D, Mendis S. Cost effectiveness of strategies to combat Cardiovascular Disease, Diabetes, and Tobacco use in sub-saharan Africa and South East Asia: mathematical modelling study. BMJ. 2012;344:e607. doi: 10.1136/bmj.e607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Salomon JA, Carvalho N, Gutierrez-Delgado C, Orozco R, Mancuso A, Hogan DR, Lee D, Murakami Y, Sridharan L, Medina-Mora ME, Gonzalez-Pier E. Intervention strategies to reduce the burden of non-communicable Diseases in Mexico: cost effectiveness analysis. BMJ. 2012;344:e355. doi: 10.1136/bmj.e355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aoun M, Helou E, Sleilaty G, Zeenny RM, Chelala D. Cost of Illness of chronic Kidney Disease in Lebanon: from the societal and third-party payer perspectives. BMC Health Serv Res. 2022;22:586. doi: 10.1186/s12913-022-07936-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dalal AA, Christensen L, Liu F, Riedel AA. Direct costs of Chronic Obstructive Pulmonary Disease among managed care patients. Int J Chron Obstruct Pulmon Dis. 2010;5:341–9. doi: 10.2147/COPD.S13771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ding D, Lawson KD, Kolbe-Alexander TL, Finkelstein EA, Katzmarzyk PT, van Mechelen W, Pratt M. Lancet Physical Activity Series 2 executive C: the economic burden of Physical Inactivity: a global analysis of major non-communicable Diseases. Lancet. 2016;388:1311–24. doi: 10.1016/S0140-6736(16)30383-X. [DOI] [PubMed] [Google Scholar]
- 22.Jommi C, Armeni P, Battista M, di Procolo P, Conte G, Ronco C, Cozzolino M, Costanzo AM, di Paparatti L, Concas U. The cost of patients with chronic Kidney Failure before Dialysis: results from the IRIDE Observational Study. Pharmacoecon Open. 2018;2:459–67. doi: 10.1007/s41669-017-0062-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Konig H, Konig HH, Konnopka A. The excess costs of depression: a systematic review and meta-analysis. Epidemiol Psychiatr Sci. 2019;29:e30. doi: 10.1017/S2045796019000180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Manns B, Hemmelgarn B, Tonelli M, Au F, So H, Weaver R, Quinn AE, Klarenbach S, for Canadians Seeking S. Innovations to overcome chronic kidney D: the cost of care for people with chronic Kidney Disease. Can J Kidney Health Dis. 2019;6:2054358119835521. doi: 10.1177/2054358119835521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Puig-Junoy J, Ruiz Zamora A. Socio-economic costs of osteoarthritis: a systematic review of cost-of-illness studies. Semin Arthritis Rheum. 2015;44:531–41. doi: 10.1016/j.semarthrit.2014.10.012. [DOI] [PubMed] [Google Scholar]
- 26.Schaller S, Mauskopf J, Kriza C, Wahlster P, Kolominsky-Rabas PL. The main cost drivers in Dementia: a systematic review. Int J Geriatr Psychiatry. 2015;30:111–29. doi: 10.1002/gps.4198. [DOI] [PubMed] [Google Scholar]
- 27.Souliotis K, Kousoulakou H, Hillas G, Tzanakis N, Toumbis M, Vassilakopoulos T. The direct and indirect costs of managing Chronic Obstructive Pulmonary Disease in Greece. Int J Chron Obstruct Pulmon Dis. 2017;12:1395–400. doi: 10.2147/COPD.S132825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wacker ME, Jorres RA, Schulz H, Heinrich J, Karrasch S, Karch A, Koch A, Peters A, Leidl R, Vogelmeier C, et al. Direct and indirect costs of COPD and its comorbidities: results from the German COSYCONET study. Respir Med. 2016;111:39–46. doi: 10.1016/j.rmed.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 29.OANDA. : Currency Converter. www.oanda.com/currency-converter/en/ [22 Jul 2022].
- 30.Bureau of Labor Statistics. : CPI Inflation Calculator. https://www.bls.gov/data/inflation_calculator.htm[12 May 2022].
- 31.World Economic Forum. : The Global Economic Burden of Non-communicable Diseases. https://www3.weforum.org/docs/WEF_Harvard_HE_GlobalEconomicBurdenNonCommunicableDiseases_2011.pdf[23 Feb 2023].
- 32.World Economic Forum and World Health Organization. : From Burden to “Best Buys”: Reducing the Economic Impact of Non-Communicable Diseases in Low- and Middle-Income Countries. https://ncdalliance.org/sites/default/files/resource_files/WHO%20From%20Burden%20to%20Best%20Buys.pdf[23 Feb 2023].
- 33.Institute for the Study of Labor. : The Economic Impact of Non-communicable Disease in China and India: Estimates, Projections, and Comparisons. https://docs.iza.org/dp7563.pdf[23 Feb 2023].
- 34.Chowdhury S, Mok D, Leenen L. Transformation of health care and the new model of care in Saudi Arabia: Kingdom’s Vision 2030. J Med Life. 2021;14:347–54. doi: 10.25122/jml-2021-0070. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used for the current study are available from the corresponding author upon reasonable request.