Abstract
Background
CD147, a transmembrane glycoprotein, has been implicated in various cancer-related processes but its role in breast cancer remains poorly understood. Herein, we investigated the expression of CD147 in different breast cancer cell lines and explored its functional roles, including migration, invasion, drug resistance and modulation of key proteins associated with cancer progression.
Methods
The expression of CD147 was assessed in MCF-10 A, BT549, MDA-MB-231 and MCF-7 breast cancer cell lines using qRT-PCR and Western blotting, following which lyposome transfections were performed, leading overexpression of CD147 in BT549 cells and knockdown of CD147 in MCF-7 cells. Scratch assays and Transwell invasion and were performed to evaluate the cells’ migration and invasion abilities. Sensitivity to 5-FU was determined via CCK-8 assays, and the expression of Snail1, E-cadherin, Vimentin, MMP-9 and the MAPK/ERK pathway were analyzed by qRT-PCR and Western blotting.
Results
Compared with normal beast epithelial cells, CD147 was highly expressed in all breast cancer cell lines, with the highest overexpression observed in MCF-7 cells and the lowest overexpression observed in BT549 cells. Overexpression of CD147 in BT549 cells increased, migration, invasion, viability and resistance to 5-FU of BT549 cells, while CD147 knockdown in MCF-7 cells reduced these properties of MCF-7 cells. Furthermore, CD147 influenced the expression of Snail1, Vimentin, E-cadherin, and MMP-9, suggesting its involvement in epithelial-mesenchymal transition (EMT) regulation. The MAPK/ERK pathway was activated by CD147 in BT549 cells, as indicated by increased p-MEK/MEK ratio and p-ERK/ERK ratio. In contrast, CD147 silencing in MCF-7 cells resulted in reduced p-MEK/MEK ratio and p-ERK/ERK ratio.
Conclusion
In summary, our findings suggest CD147 as a potential therapeutic target in breast cancer treatment, particularly in cases where drug resistance and metastasis are concerns, worthy of further explorations.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12885-023-11724-2.
Keywords: CD147, Breast cancer, Drug resistance, Epithelial-mesenchymal transitions (EMT), MAPK/ERK signaling pathway
Introduction
Breast cancer is the most common cause of cancer-related deaths among women worldwide [1]. The incidence of breast cancer has increased steadily in the last few decades [2], with approximately 1.6 million new cases reported in China in 2020 [3]. Although advances in diagnosis and therapeutic strategies have increased the survival rate of breast cancer patients in recent decades, the prognosis of advanced-stage breast cancer remains dismal due to high recurrence rates and drug resistance [4, 5]. Furthermore, the current treatments have poor efficacy in breast cancer patients with distant metastasis. Therefore, there is an urgent need to identify new and effective therapeutic markers against metastatic breast cancer.
Epithelial-mesenchymal transition (EMT) is a process wherein the epithelial cells lose their polarity and intercellular junctions and acquire the characteristics of the highly motile mesenchymal cells [6]. EMT increases the migratory capacity of epithelial cells, which is crucial for cancer invasion and metastasis, immunosuppression, tissue healing and organ fibrosis [7]. Studies have shown that lung cancer cells undergo invasion and distant metastasis through EMT [8]. The MAPK/ERK signaling pathway regulates several cellular processes, and it has been reported that the phosphorylation of ERK triggers an intracellular signaling cascade that culminates in the activation of transcription factors and protein kinases that regulate pro-survival and cell cycle genes. Further, activation of the MAPK/ERK pathway initiates cell proliferation and inhibits apoptosis [9]. Aberrant phosphorylation of ERK is closely associated with the malignant transformation of cells [10], and the MAPK/ERK pathway is frequently dysregulated during the initiation and metastasis of neurological and urinary system tumors [11]. However, further investigations are required to clarify the exact role of the MAPK/ERK pathway in breast cancer invasion and metastasis, especially considering tumor heterogeneity and different responses of patients despite being classified in the same tumor-node-metastasis (TNM) stage [12].
CD147 is a newly discovered cell surface adhesion factor, which is involved in cell-cell and cell-matrix adhesion [13]. It regulates nutrient transport, inflammatory leukocyte migration, inducing MMPs and VEGF production, spermatogenesis, lymphocyte activation, body immunity, tissue repair, nerve conduction activity, monocarboxylate transporter expression, and production of gamma-secretase complex by amyloid beta peptide in Alzheimer’s disease [14]. Furthermore, CD147 is highly expressed in glioma and liver cancer cells [15, 16] and plays a role in tumor occurrence, development, infiltration and metastasis. The high levels of CD147 on tumor cells induce the production of MMPs and vascular endothelial growth factor (VEGF) from both tumor cells and fibroblasts, promoting the degradation of extracellular matrix and tumor neo-angiogenesis, thereby accelerating tumor cell invasion. Su et al. [17] found that silencing CD147 in melanoma cells reduced VEGF production and inhibited their infiltration and metastasis in vitro by down-regulating the glycolytic pathway. Consistent with this, CD147 stimulated tumor angiogenesis, thereby promoting tumor growth, invasion and metastasis [18]. Altering the expression level of CD147 in human breast cancer cells also affected that of VEGF mRNA and protein [19]. In addition, CD147 regulated the expression of VEGF and VEGF-R2 in melanoma cells through the HIF-2α pathway, thereby promoting angiogenesis [20]. Although previous studies have shown that CD147 is upregulated in breast cancer and could lead to drug resistance and tumor invasion [21], its impact on common chemotherapeutic drugs and the underlying mechanisms remains unclear.
In this study, we aimed to determine whether CD147 regulates EMT of breast cancer cells, its effect on a commonly used chemotherapeutic drugs in clinics and to explore the role of the MARK/ERK signaling pathway in CD147-induced breast cancer invasion and metastasis.
Materials and methods
Cell culture
The non-tumorigenic breast epithelial cell line MCF-10 A, the human breast cancer cell lines MCF-7, BT549, and MDA-MB-231 were purchased from ATCC and expanded in DMEM or RPMI 1640 (Gibco, California, USA) supplemented with fetal calf serum (FCS; Institute of Hematology, Hang Zhou, China) and 1% Penicillin-Streptomycin (Gibco, California, USA) within a 5% CO2 incubator. The confluent cultures were homogenized using trypsin (HyClone, Los Angeles, USA). Cells from passages 3 to 6 were used in the experiments.
Cell transfection
CD147 siRNA (SiCD147) and CD147 cDNA (cCD147) plasmid constructs were purchased from Sangon Biotech. The cells were seeded into 6-well plates at the density of 2 × 105 cells/well and cultured for 24 h till they were 70–90% confluent. The cells were transfected with 2 µg plasmids using Lipofectamine™ 2000 (Invitrogen, USA), and selected 48 h later with 400 µg/ml G418 (Sigma, USA). Stable BT549, BT549-liposome, BT549-liposome-vector, BT549-liposome-CD147, MCF-7, MCF-7-liposome, MCF-7-liposome-siNC and MCF-7-liposome-si-CD147 clones were obtained after 1 month of continuous selection.
Quantitative real-time polymerase chain reaction (qRT-PCR)
Briefly, Total RNA was extracted from the transfected cells using Trizol (Invitrogen) and reverse transcribed to cDNA using a reverse transcription kit (Takara, Japan). qRT-PCR was performed using SYBR Premix Ex Taq Kit (Takara, Japan) with β-actin as the endogenous control for normalizing gene expression. The primers for CD147 were purchased from Sangon Biotech (Shanghai, China). The forward and reverse primers for CD147 were 5’-CAGCGGTTGGAGGTTGT-3’ and 5’-TTTGAGGGTGGAGGTGG-3’, for β-actin were 5’-AAAGACCTGTACGCCAACAC-3’ and 5’-GTCA TACTCCTGCTTGCTGAT-3’. The PCR cycling conditions were as follows: initial denaturation at 95 °C for 30 s, followed by 40 cycles at 95 °C for 30 s, 60 °C for 30 s, and 72 °C for 30 s. Relative mRNA expression levels were determined by the 2-ΔΔCt method and expressed relative to control cells.
Western blotting (WB)
Here, WB was performed to assess protein expression levels of the cell groups. Briefly, 1 × 106 harvested cells were lysed with ice-cold RIPA buffer for 30 min, and the protein concentration was determined using the BCA method. Equal amounts of protein per sample were separated by 15% SDS-PAGE and transferred onto PVDF membranes. After blocking with 5% bovine serum albumin in Tris-buffer saline (TBST) at 37 °C for 1 h, the membranes were incubated overnight with primary antibodies (Rabbit anti-human CD147, p-ERK, ERK, β-actin, MMP-9, Snail1, E-cadherin and Vimentin antibodies, Abcam, USA) at 4 °C, and thereafter with an HRP-conjugated secondary antibody for 1 h at room temperature. The protein bands were detected using an enhanced chemiluminescence (ECL) detection kit (Beyotime). The density of each band was normalized to β-actin. Fluorescence intensity was quantified via ImageJ software.
Cell counting Kit-8 (CCK-8) assay
The resistance of the different cell lines to 5-FU was determined by the Cell Counting Kit-8 (CCK-8) assay according to the manufacturer’s instructions (Beyotime, Shanghai, China). The cells were seeded in 96-well plates at the density of 1 × 105 cells/well in 100 µl medium and cultured for 24 h. After treating the cells with different concentrations of 5-FU (0, 2, 4, 6, 8, 10 µM) for 48 h, 10 µl CCK-8 reagent was added to each well, and the cells were incubated for 2 h at 37ºC. The absorbance was measured at 450 nm using a microplate reader. The dose-response curves were generated to determine their corresponding IC50 values, representing the 5-FU concentration at which cell viability was reduced by 50% compared to untreated controls.
Scratch wound healing assay
First, the cells were separately seeded and allowed to form a confluent monolayer. Then, a uniform scratch was created across the cell layer using a sterile pipette tip. The cells were then gently washed to remove detached cells and debris, and fresh medium was added. Images of the scratch area were captured at multiple time points post-scratch (e.g., 0, 24 and 48 h). The rate of scratch closure, indicative of cell migration, was quantified by measuring the reduction in scratch width over time to assess the migratory capacity of the different cell groups and the potential impact of CD147 modulation on cell motility.
Transwell invasion assay
In brief, Transwell inserts with Matrigel-coated membranes were placed into wells containing serum-free culture medium, while cells suspended in serum-free medium were added to the upper chamber. The lower chamber contained a culture medium supplemented with a attractant. After incubation, non-invading cells were removed from the upper surface, and invading cells that passed through the Matrigel and membrane were fixed and stained, then counted under a microscope to quantify the invasive potential of each cell group to determine their invasive capacity.
Statistical analysis
Statistical analyses were conducted using SPSS 13.0. The results were expressed as mean ± standard deviation (SD) for continuous variables. Statistical significance was assessed using one-way analysis of variance (ANOVA) followed by post hoc tests such as Tukey’s multiple comparison test for multiple groups. P < 0.05 was considered statistically significant.
Results
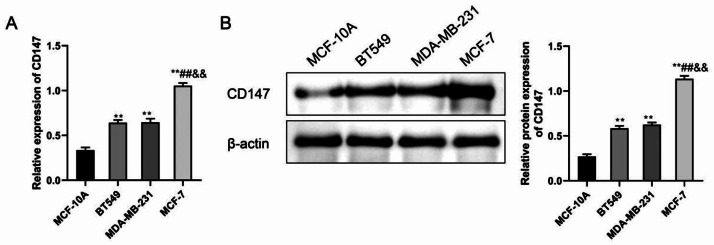
CD147 is highly expressed in breast cancer cell lines
We assessed the expression levels of CD147 mRNA and protein in the MCF-10 A, BT549, MDA-MB-231 and MCF-7 human breast cancer cell lines via qRT-PCR. Comparative analysis revealed that when compared to the MCF-10 A cell group, the BT549, MDA-MB-231, and MCF-7 cell groups exhibited a significant increase in CD147 gene levels (P < 0.01). When compared to the BT549 and MDA-MB-231 cell groups, the MCF-7 cell group demonstrated a significant elevation in CD147 expression (P < 0.01) (Fig. 1A). Besides, the results of WB analysis were consistent with qRT-PCR results (Fig. 1B). BT549 cells and MCF-7 cells were chose for subsequent experiments.
Fig. 1.
The expression of CD147 in different breast cancer cell lines. (A) qRT-PCR analysis of CD147 mRNA levels in MCF-10 A, BT549, MDA-MB-231, and MCF-7 cells. (B) Western blot analysis of CD147 protein expression in these cell lines, showing substantial upregulation in BT549, MDA-MB-231, and MCF-7 cells relative to MCF-10 A. **P < 0.01, vs. MCF-10 A; ##P < 0.01, vs. BT549; &&P < 0.01, vs. MDA-MB-231
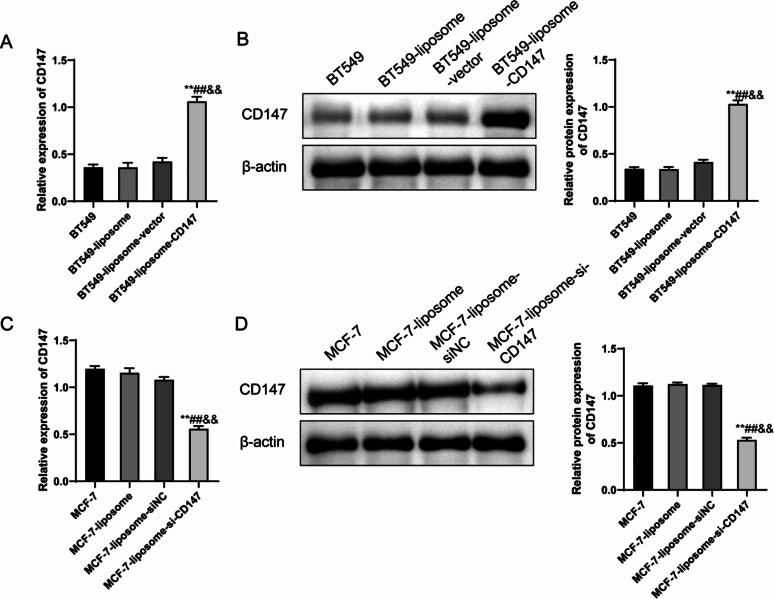
Modulating CD147 expression in breast cancer cell lines
Considering that there was a significantly greater expression of CD147 in the MCF-7 cell group than in the BT549 group, further experiments were performed to overexpress the CD147 levels in BT549 cells and knockdown CD147 expression levels in the MCF-7 cells. The qRT-PCR results indicated that CD147 levels remained relatively consistent across BT549, BT549-liposome and BT549-liposome-vector cell groups, with no significant differences observed (P > 0.05), and a successful upregulation of CD147 in the BT549-liposome-CD147 group compared to the BT549 control groups (P < 0.01), which was then confirmed in WB experiments (Fig. 2B). In addition, we also successfully knocked down the CD147 expression in the MCF-7-liposome-si-CD147 group, which had significant lower CD147 level than MCF-7, MCF-7-liposome and MCF-7-liposome-siNC cell groups (P < 0.01) (Fig. 2C–D).
Fig. 2.
Transfection efficiency of the different constructs in BT549 and MCF-7 cells. (A) qRT-PCR results show consistent CD147 expression in BT549, BT549-liposome, and BT549-liposome-vector cells, with successful upregulation in BT549-liposome-CD147. (B) Western blot confirms increased CD147 protein expression in BT549-liposome-CD147. (C) qRT-PCR demonstrates CD147 knockdown in MCF-7-liposome-si-CD147. (D) Western blot confirms reduced CD147 protein expression in MCF-7-liposome-si-CD147. **P < 0.01, vs. BT549/MCF-7; ##P < 0.01, vs. BT549-liposome/MCF-7-liposome; &&P < 0.01, vs. BT549-liposome-CD147/MCF-7-liposome-siNC
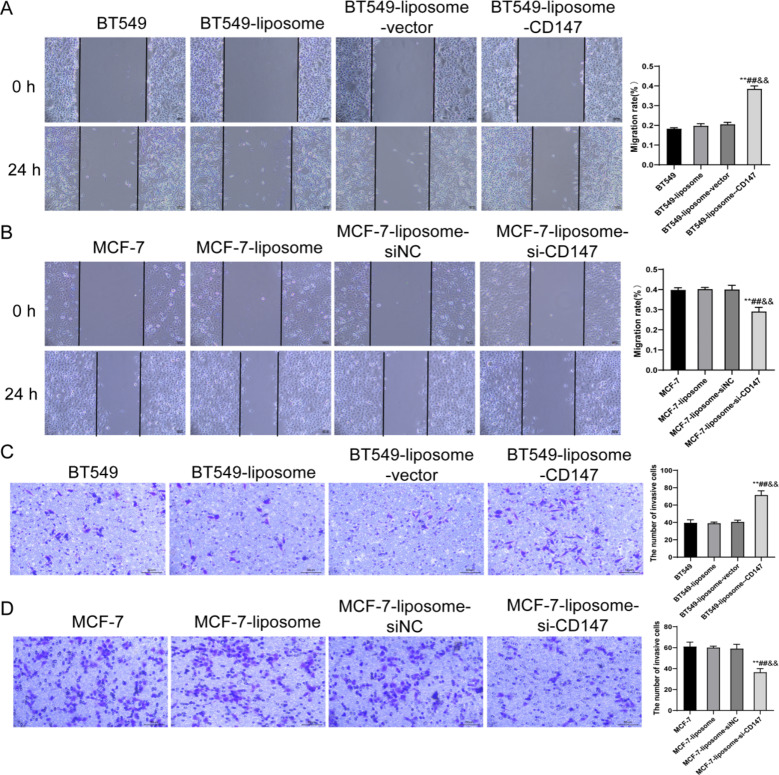
CD147 impact on breast cancer cell migration and invasion
In this experiment, we examined the migratory and invasive capabilities of BT549 and MCF-7 cell groups. Within the BT549 cell-based groups, no significant differences in invasion abilities were observed between the BT549, BT549-liposome and BT549-liposome-vector groups, while the BT549-liposome-CD147 group exhibited a significant increase in migratory capacity (P < 0.01) (Fig. 3A). Comparatively, the MCF-7-liposome-si-CD147 group displayed a significant decrease in migratory abilities compared to the MCF-7, MCF-7-liposome and MCF-7-liposome-siNC groups (P < 0.01) (Fig. 3B). Same as the migration capacity, the BT549-liposome-CD147 group showed a significant increase in the invasion capability of BT549 cells (P < 0.01) and the MCF-7-liposome-si-CD147 group was significantly reduced the invasive potential of MCF-7 cells (Fig. 3C–D). Overall, these findings indicate a potential role of CD147 in promoting cell migration and invasion in the BT549 and MCF-7 cell lines.
Fig. 3.
Effects of CD147 on cellular migration and invasion in BT549 and MCF-7 cells. (A) Scratch assay reveals enhanced migration in BT549-liposome-CD147. (B) Scratch assay shows reduced migration in MCF-7-liposome-si-CD147. (C) Transwell invasion assay for BT549 cell groups shows increased invasion in BT549-liposome-CD147. (D) Transwell invasion assay for MCF-7 cell groups displays reduced invasion in MCF-7-liposome-si-CD147. **P < 0.01, vs. BT549/MCF-7; ##P < 0.01, vs. BT549-liposome/MCF-7-liposome; &&P < 0.01, vs. BT549-liposome-CD147/MCF-7-liposome-siNC
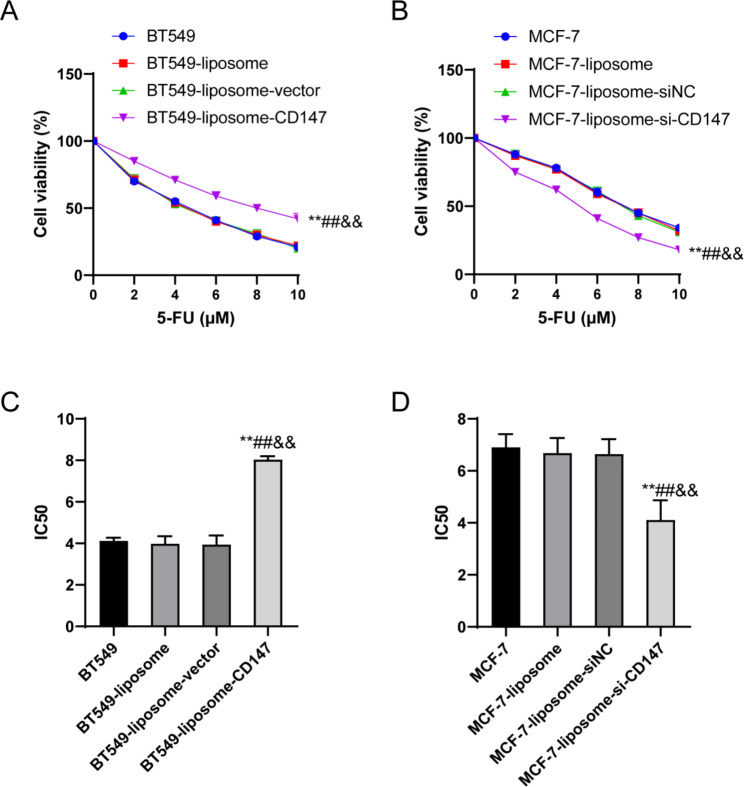
CD147 enhanced the 5-FU resistance of breast cancer cells
The sensitivity of the different breast cancer cell lines to 5-FU was determined by evaluating the cells viability using CCK-8 assay in the BT549 and MCF-7 cell groups following treatment with different concentrations of 5-FU. In both BT549 cell groups and MCF-7 cell groups, there were no significant differences in cell viability at a 5-FU concentration of 0 µM among groups, when the 5-FU concentration increased from 2 µM to 10 µM, the cells viability gradually decreased (Fig. 4A–B). Notably, compared with the BT549 group, BT549-liposome group and BT549-liposome-vector group, the BT549-liposome-CD147 group displayed a significant increase in cell viability (P < 0.01) (Fig. 4A), while the MCF-7-liposome-si-CD147 group exhibited a significant lower cell viability than the MCF-7 group, MCF-7-liposome group and MCF-7-liposome-siNC group (P < 0.01) (Fig. 4B).
Fig. 4.
Effects of CD147 on 5-FU resistance in breast cancer cells. (A) CCK-8 assay indicates increased cell viability in BT549-liposome-CD147 at higher 5-FU concentrations. (B) CCK-8 assay demonstrates reduced cell viability in MCF-7-liposome-si-CD147 at higher 5-FU concentrations. (C) Increased IC50 value in BT549-liposome-CD147 cells. (D) Reduced IC50 value in MCF-7-liposome-si-CD147. **P < 0.01, vs. BT549/MCF-7; ##P < 0.01, vs. BT549-liposome/MCF-7-liposome; &&P < 0.01, vs. BT549-liposome-CD147/MCF-7-liposome-siNC.
Furthermore, when assessing the half-maximal inhibitory concentration (IC50) for 5-FU, there were no significant differences among the BT549 group, BT549-liposome group, and BT549-liposome-vector group, but when compared with these groups, the IC50 value for BT549 cells in the BT549-liposome-CD147 group significantly increased (P < 0.01) (Fig. 4C). For the MCF-7 cells,, the IC50 value for MCF-7 cells in the MCF-7-liposome-si-CD147 group significantly decreased compared to the MCF-7 group, MCF-7-liposome group, and MCF-7-liposome-siNC group (P < 0.01) (Fig. 4D). These results indicated that CD147 could regulate the 5-FU resistance in breast cancer cells.
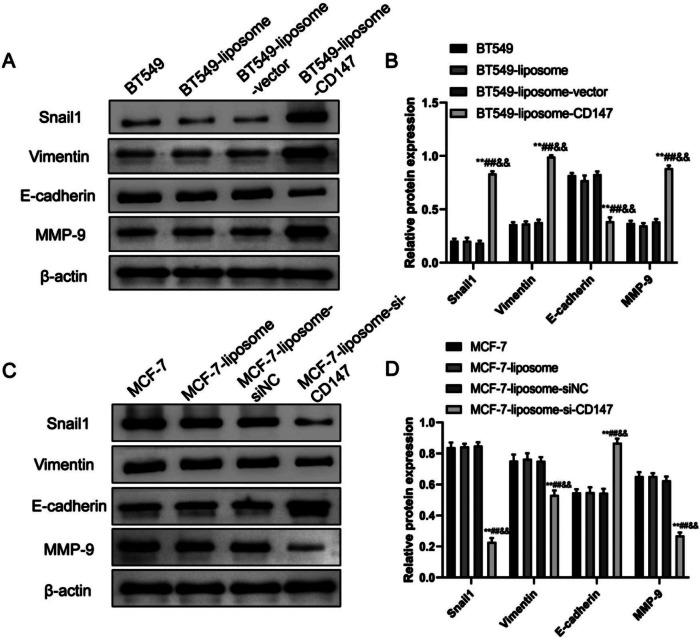
CD147 induced EMT in breast cancer cells
Here, we examined the expression of Vimentin, MMP-9 and E-cadherin and the impact of CD147 in different cell line variants of the BT549 and MCF-7 cells (Fig. 5). For the BT549, BT549-liposome and BT549-liposome-vector groups, The WB results showed no significant differences in Snail1, Vimentin, E-cadherin and MMP-9 expression levels, however, when compared to these groups, the BT549-liposome-CD147 group displayed a noteworthy increase in Snail1, Vimentin and MMP-9 expression as well as a significant decrease in E-cadherin (P < 0.01) (Fig. 5A–B). Similarly, for the MCF-7, MCF-7-liposome, and MCF-7-liposome-siNC groups, there were no significant differences in Snail1, Vimentin, E-cadherin and MMP-9 expression levels, while the MCF-7-liposome-si-CD147 group exhibited a significant increase in E-cadherin expression as well as a significant decrease in Snail1, Vimentin and MMP-9 expression (P < 0.01) (Fig. 5C–D). Collectively, both cell lines showed similar results within their respective groups, emphasizing the notable impact of CD147 on the expression of these critical proteins in cellular processes.
Fig. 5.
The expression of snail1, vimentin, E-cadherin and MMP-9 in BT549 and MCF-7 cells. (A–B) Western blot images (A) and semi-quantification (B) of Snail1, Vimentin, E-cadherin and MMP-9 proteins in BT549, BT549-liposome, BT549-liposome-vector and BT549-liposome-CD147. (C-D) Western blot images (C) and semi-quantification (D) of Snail1, Vimentin, E-cadherin and MMP-9 proteins in MCF-7, MCF-7-liposome, MCF-7-liposome-vector and MCF-7-liposome-siCD147 cell lines. Data were represented as the mean ± SD. **P < 0.01, vs. BT549/MCF-7; ##P < 0.01, vs. BT549-liposome/MCF-7-liposome; &&P < 0.01, vs. BT549-liposome-CD147/MCF-7-liposome-siNC
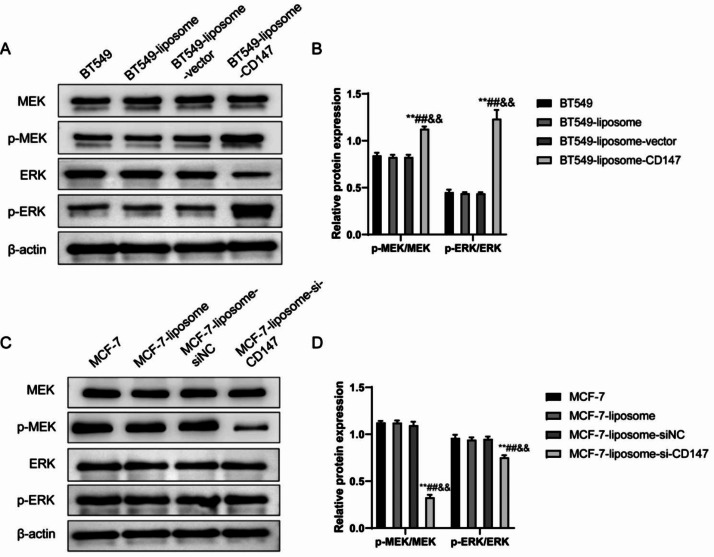
CD147 activated the MAPK/ERK pathway in breast cancer cells
Among the BT549, BT549-liposome and BT549-liposome-vector, no significant differences were observed between them in regards to MEK, p-MEK, ERK and p-ERK protein levels, while the BT549-liposome-CD147 group, showed a significant increase in p-MEK/MEK ratio and p-ERK/ERK ratio (P < 0.01) (Fig. 6A–B). Conversely, the MCF-7-liposome-si-CD147 group showed a significant reduction in p-MEK/MEK ratio and p-ERK/ERK ratio compared with the MCF-7, MCF-7-liposome, and MCF-7-liposome-siNC groups (P < 0.01) (Fig. 6C–D). These findings indicated that CD147 activated the MAPK/ERK pathway both in BT549 and MCF-7 cell lines.
Fig. 6.
The expression of pERK and tERK in BT549 and MCF-7 cells. (A) Western blot analysis of MEK, p-MEK, ERK, and p-ERK protein levels in BT549 cell groups, indicating increased p-MEK and p-ERK in BT549-liposome-CD147. (B) Ratios of p-MEK/MEK and p-ERK/ERK significantly increase in BT549-liposome-CD147. (C) Western blot displays reduced p-MEK and p-ERK levels in MCF-7-liposome-si-CD147. (D) Decreased p-MEK/MEK and p-ERK/ERK ratios in MCF-7-liposome-si-CD147 indicate MAPK/ERK pathway modulation. **P < 0.01, vs. BT549/MCF-7; ##P < 0.01, vs. BT549-liposome/MCF-7-liposome; &&P < 0.01, vs. BT549-liposome-CD147/MCF-7-liposome-siNC
Discussion
Drug resistance and tumor metastasis are the two important causes of treatment failure and mortality in cancer patients [22]. Tumor metastasis is a complex process involving multiple pathways and factors. EMT of the tumor cells increases their ability to migrate and invade nearby tissues, eventually resulting in the formation of new metastatic foci [23]. Several studies have shown that CD147 is closely involved in cancer metastasis [24–26]. The results of our study reveal significant insights into the role of CD147 in breast cancer cell behavior and its potential impact on various cellular processes. We initially observed high levels of CD147 expression in multiple breast cancer cell lines compared with normal breast epithelial cells, including BT549, MDA-MB-231 and MCF-7, with differential expression patterns among them, indicating its potential as a promising therapeutic target for breast cancer treatment. Additionally, the successful manipulation of CD147 levels in BT549 and MCF-7 cells demonstrates the feasibility of controlling CD147 expression, opening avenues for potential treatment strategies [27]. From a clinical standpoint, CD147’s differential expression among cell lines, especially its significant elevation in MCF-7 cells, hints at its relevance for prognosis and treatment response prediction. Investigating CD147 as a potential prognostic marker in breast cancer patient samples could provide valuable insights.
CD147 has also been implicated in chemoresistance, which is the main cause of treatment failure [28]. The choice of 5-FU in breast cancer cell lines for this study holds historical significance, reflects progress in cancer research, and offers valuable clinical implications. 5-FU is a chemotherapy drug with a long history of use in cancer treatment, including breast cancer [29]. It inhibits DNA synthesis, making it effective against rapidly dividing cancer cells [30]. Here, we intended to determine whether CD147 mediated the chemoresistance of metastatic breast cancer cells. We found that CD147 overexpression decreased the sensitivity of breast cancer cells to 5-FU. The reason may be that CD147 stimulates hyaluronic acid production and upregulates HER-2, which interacts with the cell surface receptor CD44 and indirectly induces multidrug resistance [31]. In terms of clinical implications, our findings regarding CD147’s role in mediating 5-FU resistance have potential relevance for breast cancer patients because understanding the molecular mechanisms behind resistance can inform treatment strategies and the development of combination therapies that target CD147 alongside 5-FU may enhance treatment efficacy and overcome resistance. Furthermore, these insights contribute to the ongoing evolution of breast cancer treatment, emphasizing the need for personalized, targeted approaches to improve patient outcomes.
EMT is a crucial process in cancer metastasis, allowing cancer cells to become more invasive and mobile, and has been closely related to poor prognosis [31, 32]. Therefore, studies are increasingly focusing on the regulatory pathways of EMT in tumor metastasis to identify novel therapeutic targets [33]. EMT is the process of epithelial cells into mesenchymal cells. During the process of EMT, the expression of marker proteins of epithelial cells (such as E-cadherin and Cytokeratin) is reduced, while the expression of marker proteins of mesenchymal cells (such as MMPs and Vimentin) is increased [34, 35]. Snail1 is an EMT regulator, belonging to the Snail superfamily of transcriptional repressors, which represses E-cadherin expression by binding to E-boxes in the promoter region of the proximal E-cadherin gene and induces EMT, plays a critical role in tumor metastasis [36]. In this study, the observed increase in Snail1, Vimentin and MMP-9 expression as well as the reduction in E-cadherin expression in the BT549-liposome-CD147 group suggests that CD147 may contribute to EMT and facilitate tumor invasiveness in certain breast cancer cases. Conversely, the reduction in Snail1, Vimentin and MMP-9 expression as well as the increase in E-cadherin expression in the MCF-7-liposome-si-CD147 group indicate that targeting CD147 could potentially reverse EMT in breast cancer cells. Overall, these findings imply that CD147 may serve as a potential therapeutic target for modulating the EMT behavior of breast cancer cells. In this regard, our findings were concordant with existing literature as CD147 has previously been shown to stimulate the production and secretion of MMPs [37] that facilitate tumor invasion and metastasis by breaking down the extracellular matrix [38].
Further research and clinical investigations are warranted to assess the feasibility of targeting CD147 in breast cancer treatment and its potential to impact patient outcomes.
Previous studies have shown that the MAPK/ERK pathway is involved in cancer metastasis and drug resistance [9, 39]. Kim et al. reported that CD147 induces the expression of MMP-9 in macrophages through ERK and NF-κB [40]. Our findings in regard to the MAPK/ERK pathway may have some credible clinical implications for breast cancer treatment. The activation of the MAPK/ERK pathway by CD147, as demonstrated in this study, suggests CD147 is a potentially considerable target for therapeutic intervention of breast cancer. Given that the MAPK/ERK pathway is known to be involved in cancer metastasis and drug resistance, inhibiting this pathway may hold promise for mitigating these critical aspects of breast cancer progression [41, 42]. Previous studies have revealed various different pathways by which CD147 promotes tumor metastasis and invasion. Zhang et al. reported that silencing of CD147 inhibited the migration and invasion of lung adenocarcinoma cells through blocking the Rap1 signaling pathway [24]. Dana et al’s data indicated that CD147 promotes the migration and invasion of cholangiocarcinoma cells by activating the Akt-FoxO3-NF-κB-MCT-1/4 axis [25]. The study of wang et al. demonstrated that CD147 promotes hepatocellular carcinoma cells collective invasion via upregulating cathepsin B expression [26]. It’s no doubt that CD147, as an extracellular matrix metalloproteinase inducer, can promote migration and invasion of the different tumors, but its mechanism is not fully confirmed. Our study’s results suggest that targeting CD147 could represent a novel approach to suppress the MAPK/ERK pathway and thereby potentially reduce the invasive behavior of breast cancer cells and inhibit EMT. Such therapeutic strategies, if validated in further studies and clinical trials, could offer new avenues for improving the management of breast cancer, particularly in cases where CD147-mediated pathway activation contributes to disease aggressiveness and resistance to standard treatments.
In future experiments, researchers could use preclinical studies in animal models to assess the therapeutic potential of CD147 inhibition in breast cancer. The successful manipulation of CD147 levels in BT549 and MCF-7 cells suggests promising treatment strategies, such as the development of targeted therapies, potentially through monoclonal antibodies or small molecule inhibitors aimed at reducing CD147 expression. RNA interference (RNAi) approaches could also be explored utilizing siRNA or other delivery methods. Furthermore, combination therapies involving CD147-targeted agents alongside standard chemotherapy drugs, immunotherapeutic strategies, and the initiation of clinical trials to evaluate the safety and efficacy of these approaches in breast cancer patients are all potential avenues for further investigation. These strategies aim to mitigate CD147-mediated effects, including drug resistance and enhanced invasive behavior, aiming to improve breast cancer treatment outcomes.
Conclusion
In summary, our study provides compelling evidence for the significant influence of CD147 on breast cancer cell behavior, including invasion, migration, cell viability, drug resistance and EMT process. Additionally, our findings suggest a potential mechanistic link between CD147 and the MAPK/ERK pathway in mediating these effects. These insights contribute to a better understanding of CD147’s role in breast cancer progression and may hav e implications for the development of targeted therapies aimed at modulating CD147-related pathways in breast cancer treatment.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1: The full-length gels and blots of Western blotting in the article
Acknowledgements
Not applicable.
List of abbreviations
- EMT
epithelial-mesenchymal transition
- TNM
tumor-node-metastasis
- VEGF
vascular endothelial growth factor
- FCS
fetal calf serum
- WB
Western blotting
- TBST
Tris-buffer saline
- ECL
enhanced chemiluminescence
- CCK-8
Cell Counting Kit-8
- SD
standard deviation
- ANOVA
analysis of variance
- IC50
inhibitory concentration
- RNAi
RNA interference
Author contributions
Study concept and design: FL, JW; Analysis and interpretation of data: YY, CB, JG; Drafting of the manuscript: FL, JW; Critical revision of the manuscript for important intellectual content: FL, JW; Statistical analysis: YY, CB, JG; Study supervision: all authors; all authors have read and approved the manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (No. 82201722), the Basic Research Program (Free Exploration) of Shanxi Province, China (No. 20210302123491), Four “Batches” Innovation Project of Invigorating Medical through Science and Technology of Shanxi Province (No. 2022XM58), the Basic Research Program of Shanxi Province, China (No. 20210302124277), the scientific research project of Shanxi Province Health Commission (No. 2020007), the scientific research fund of Shanxi Bethune Hospital (No. 2021YJ06).
Data Availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study did not involve humans or animals and therefore did not require ethical approval.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Fang Li and Jing Wang contributed equally to this work as Co-first author.
References
- 1.Viens L, Perin D, Senkomago V, Neri A, Saraiya M. Questions about cervical and Breast Cancer screening knowledge, practice, and outcomes: a review of demographic and health surveys. J Womens Health (Larchmt) 2017;26(5):403–12. doi: 10.1089/jwh.2017.6441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li S, Wang Y, Feng C, Wu G, Ye Y, Tian J. Calycosin inhibits the Migration and Invasion of human Breast Cancer cells by down-regulation of Foxp3 expression. Cell Physiol Biochem. 2017;44(5):1775–84. doi: 10.1159/000485784. [DOI] [PubMed] [Google Scholar]
- 3.Zhang Z, Lin M, Wang J, Yang F, Yang P, Liu Y, Chen Z, Zheng Y. Calycosin inhibits Breast cancer cell migration and invasion by suppressing EMT via BATF/TGF-beta1. Aging. 2021;13(12):16009–23. doi: 10.18632/aging.203093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cheng YJ, Nie XY, Ji CC, Lin XX, Liu LJ, Chen XM, Yao H, Wu SH. Long-Term Cardiovascular Risk after Radiotherapy in Women with Breast Cancer. J Am Heart Assoc. 2017;6(5). [DOI] [PMC free article] [PubMed]
- 5.Corona SP, Sobhani N, Ianza A, Roviello G, Mustacchi G, Bortul M, Zanconati F, Generali D. Advances in systemic therapy for metastatic Breast cancer: future perspectives. Med Oncol. 2017;34(7):119. doi: 10.1007/s12032-017-0975-5. [DOI] [PubMed] [Google Scholar]
- 6.Chen T, You Y, Jiang H, Wang ZZ. Epithelial-mesenchymal transition (EMT): a biological process in the development, stem cell differentiation, and tumorigenesis. J Cell Physiol. 2017;232(12):3261–72. doi: 10.1002/jcp.25797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pan QZ, Li K, Yang ZD, Gao M, Shi JH, Ren SP, Zhao GQ. Dexmedetomidine attenuates high glucose-induced HK-2 epithelial-mesenchymal transition by inhibiting AKT and ERK. Biomed Environ Sci. 2020;33(5):323–30. doi: 10.3967/bes2020.044. [DOI] [PubMed] [Google Scholar]
- 8.Pastushenko I, Blanpain C. EMT Transition States during Tumor Progression and Metastasis. Trends Cell Biol. 2019;29(3):212–26. doi: 10.1016/j.tcb.2018.12.001. [DOI] [PubMed] [Google Scholar]
- 9.Pereira SS, Monteiro MP, Costa MM, Ferreira J, Alves MG, Oliveira PF, Jarak I, Pignatelli D. MAPK/ERK pathway inhibition is a promising treatment target for adrenocortical tumors. J Cell Biochem. 2019;120(1):894–906. doi: 10.1002/jcb.27451. [DOI] [PubMed] [Google Scholar]
- 10.Murai Y, Jo U, Murai J, Jenkins LM, Huang SN, Chakka S, Chen L, Cheng K, Fukuda S, Takebe N, et al. SLFN11 inactivation induces proteotoxic stress and sensitizes Cancer cells to Ubiquitin activating enzyme inhibitor TAK-243. Cancer Res. 2021;81(11):3067–78. doi: 10.1158/0008-5472.CAN-20-2694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Noi M, Mukaisho KI, Murakami S, Koshinuma S, Machida Y, Yamori M, Nakayama T, Ogawa T, Nakata Y, Shimizu T, et al. Expressions of ezrin, ERK, STAT3, and AKT in tongue cancer and association with Tumor characteristics and patient survival. Clin Exp Dent Res. 2020;6(4):420–7. doi: 10.1002/cre2.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.El-Sayes N, Vito A, Mossman K. Tumor heterogeneity: a great barrier in the age of cancer immunotherapy. Cancers (Basel). 2021;13(4). [DOI] [PMC free article] [PubMed]
- 13.Asgari R, Vaisi-Raygani A, Aleagha MSE, Mohammadi P, Bakhtiari M, Arghiani N. CD147 and MMPs as key factors in physiological and pathological processes. Biomed Pharmacother. 2023;157:113983. doi: 10.1016/j.biopha.2022.113983. [DOI] [PubMed] [Google Scholar]
- 14.Wang N, Jiang X, Zhang S, Zhu A, Yuan Y, Xu H, Lei J, Yan C. Structural basis of human monocarboxylate transporter 1 inhibition by anti-cancer drug candidates. Cell. 2021;184(2):370–383e313. doi: 10.1016/j.cell.2020.11.043. [DOI] [PubMed] [Google Scholar]
- 15.Guo N, Miao R, Gao X, Huang D, Hu Z, Ji N, Nan Y, Jiang F, Gou X. Shikonin inhibits proliferation and induces apoptosis in glioma cells via downregulation of CD147. Mol Med Rep. 2019;19(5):4335–43. doi: 10.3892/mmr.2019.10101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shi WP, Ju D, Li H, Yuan L, Cui J, Luo D, Chen ZN, Bian H. CD147 promotes CXCL1 expression and modulates liver fibrogenesis. Int J Mol Sci 2018, 19(4). [DOI] [PMC free article] [PubMed]
- 17.Su J, Gao T, Jiang M, Wu L, Zeng W, Zhao S, Peng C, Chen X. CD147 silencing inhibits Tumor growth by suppressing glucose transport in Melanoma. Oncotarget. 2016;7(40):64778–84. doi: 10.18632/oncotarget.11415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lian C, Guo Y, Zhang J, Chen X, Peng C. Targeting CD147 is a Novel Strategy for Antitumor Therapy. Curr Pharm Des. 2017;23(29):4410–21. doi: 10.2174/1381612823666170710144759. [DOI] [PubMed] [Google Scholar]
- 19.Amit-Cohen BC, Rahat MM, Rahat MA. Tumor cell-macrophage interactions increase angiogenesis through secretion of EMMPRIN. Front Physiol. 2013;4:178. doi: 10.3389/fphys.2013.00178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hatanaka M, Higashi Y, Kawai K, Su J, Zeng W, Chen X, Kanekura T. CD147-targeted siRNA in A375 malignant Melanoma cells induces the phosphorylation of EGFR and downregulates cdc25C and MEK phosphorylation. Oncol Lett. 2016;11(4):2424–8. doi: 10.3892/ol.2016.4267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li F, Zhang J, Guo J, Jia Y, Han Y, Wang Z. RNA interference targeting CD147 inhibits Metastasis and invasion of human Breast cancer MCF-7 cells by downregulating MMP-9/VEGF expression. Acta Biochim Biophys Sin (Shanghai) 2018;50(7):676–84. doi: 10.1093/abbs/gmy062. [DOI] [PubMed] [Google Scholar]
- 22.Yang JM, Xu Z, Wu H, Zhu H, Wu X, Hait WN. Overexpression of extracellular matrix metalloproteinase inducer in multidrug resistant cancer cells. Mol Cancer Res. 2003;1(6):420–7. [PubMed] [Google Scholar]
- 23.Puram SV, Tirosh I, Parikh AS, Patel AP, Yizhak K, Gillespie S, Rodman C, Luo CL, Mroz EA, Emerick KS, et al. Single-cell transcriptomic analysis of primary and metastatic Tumor ecosystems in Head and Neck Cancer. Cell. 2017;171(7):1611–1624e1624. doi: 10.1016/j.cell.2017.10.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang N, Liu Z, Lai X, Liu S, Wang Y. Silencing of CD147 inhibits cell proliferation, migration, invasion, lipid metabolism dysregulation and promotes apoptosis in lung adenocarcinoma via blocking the Rap1 signaling pathway. Respir Res. 2023;24(1):253. doi: 10.1186/s12931-023-02532-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dana P, Saisomboon S, Kariya R, et al. CD147 augmented monocarboxylate transporter-1/4 expression through modulation of the Akt-FoxO3-NF-κB pathway promotes cholangiocarcinoma migration and invasion. Cell Oncol (Dordr) 2020;43(2):211–22. doi: 10.1007/s13402-019-00479-3. [DOI] [PubMed] [Google Scholar]
- 26.Wang SJ, Chao D, Wei W, et al. CD147 promotes collective invasion through cathepsin B in hepatocellular carcinoma. J Exp Clin Cancer Res. 2020;39(1):145. doi: 10.1186/s13046-020-01647-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bhushan A, Gonsalves A, Menon JU. Current state of Breast Cancer diagnosis, treatment, and Theranostics. Pharmaceutics 2021, 13(5). [DOI] [PMC free article] [PubMed]
- 28.Grass GD, Dai L, Qin Z, Parsons C, Toole BP. CD147: regulator of hyaluronan signaling in invasiveness and chemoresistance. Adv Cancer Res. 2014;123:351–73. doi: 10.1016/B978-0-12-800092-2.00013-7. [DOI] [PubMed] [Google Scholar]
- 29.Amjad MT, Chidharla A, Kasi A. Cancer Chemotherapy. In: StatPearls, editor. Treasure Island (FL) ineligible companies. Disclosure: Anusha Chidharla declares no relevant financial relationships with ineligible companies. Disclosure: Anup Kasi declares no relevant financial relationships with ineligible companies; 2023. [Google Scholar]
- 30.Liang GB, Wei JH, Jiang H, Huang RZ, Qin JT, Wang HL, Wang HS, Zhang Y. Design, synthesis and antitumor evaluation of new 1,8-naphthalimide derivatives targeting nuclear DNA. Eur J Med Chem. 2021;210:112951. doi: 10.1016/j.ejmech.2020.112951. [DOI] [PubMed] [Google Scholar]
- 31.Xiong L, Ding L, Ning H, Wu C, Fu K, Wang Y, Zhang Y, Liu Y, Zhou L. CD147 knockdown improves the antitumor efficacy of trastuzumab in HER2-positive Breast cancer cells. Oncotarget. 2016;7(36):57737–51. doi: 10.18632/oncotarget.10252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mittal V. Epithelial mesenchymal transition in Tumor Metastasis. Annu Rev Pathol. 2018;13:395–412. doi: 10.1146/annurev-pathol-020117-043854. [DOI] [PubMed] [Google Scholar]
- 33.Kaszak I, Witkowska-Pilaszewicz O, Niewiadomska Z, Dworecka-Kaszak B, Ngosa Toka F, Jurka P. Role of cadherins in Cancer-A Review. Int J Mol Sci 2020, 21(20). [DOI] [PMC free article] [PubMed]
- 34.Lamouille S, Xu J, Derynck R. Molecular mechanisms of epithelial-mesenchymal transition. Nat Rev Mol Cell Biol. 2014;15(3):178–96. doi: 10.1038/nrm3758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Scheau C, Badarau IA, Costache R, Caruntu C, Mihai GL, Didilescu AC, Constantin C, Neagu M. The Role of Matrix Metalloproteinases in the Epithelial-Mesenchymal Transition of Hepatocellular Carcinoma. Anal Cell Pathol (Amst) 2019, 2019:9423907. [DOI] [PMC free article] [PubMed]
- 36.Tang X, Sui X, Weng L, Liu Y. SNAIL1: linking Tumor Metastasis to Immune Evasion. Front Immunol. 2021;12:724200. doi: 10.3389/fimmu.2021.724200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Patrizz A, Doran SJ, Chauhan A, Ahnstedt H, Roy-O’Reilly M, Lai YJ, Weston G, Tarabishy S, Patel AR, Verma R, et al. EMMPRIN/CD147 plays a detrimental role in clinical and experimental ischemic Stroke. Aging. 2020;12(6):5121–39. doi: 10.18632/aging.102935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rahat MA, Safieh M, Simanovich E, Pasand E, Gazitt T, Haddad A, Elias M, Zisman D. The role of EMMPRIN/CD147 in regulating angiogenesis in patients with psoriatic arthritis. Arthritis Res Ther. 2020;22(1):240. doi: 10.1186/s13075-020-02333-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Xu T, Zhou M, Peng L, Kong S, Miao R, Shi Y, Sheng H, Li L. Upregulation of CD147 promotes cell invasion, epithelial-to-mesenchymal transition and activates MAPK/ERK signaling pathway in Colorectal cancer. Int J Clin Exp Pathol. 2014;7(11):7432–41. [PMC free article] [PubMed] [Google Scholar]
- 40.Kim JY, Kim WJ, Kim H, Suk K, Lee WH. The stimulation of CD147 induces MMP-9 expression through ERK and NF-kappaB in macrophages: implication for Atherosclerosis. Immune Netw. 2009;9(3):90–7. doi: 10.4110/in.2009.9.3.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Guo YJ, Pan WW, Liu SB, Shen ZF, Xu Y, Hu LL. ERK/MAPK signalling pathway and tumorigenesis. Exp Ther Med. 2020;19(3):1997–2007. doi: 10.3892/etm.2020.8454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lee S, Rauch J, Kolch W. Targeting MAPK signaling in Cancer: mechanisms of Drug Resistance and Sensitivity. Int J Mol Sci 2020, 21(3). [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material 1: The full-length gels and blots of Western blotting in the article
Data Availability Statement
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.