The Second Pandemic
Over the past few years, the perceived level of psychological stress has risen dramatically across the globe due to a combination of events including the long-lasting Covid-19 pandemic, civil unrest, escalation of political instability across the globe, and climate change that has triggered major environmental and economic perturbations. The consequences of this broad-scale increase in stress are only beginning to be appreciated, but evidence suggests that we are facing a second pandemic of mood and anxiety disorders, including major depression, anxiety, and posttraumatic stress disorder (PTSD). This Special Issue entitled “The Neurobiology of Stress: Vulnerability, Resilience, and Major Depression” is intended to ask “How can science help?” Our hope is to initiate a broad discussion on the power of basic and clinical scientific tools to confront these challenges and to offer strategies for treatment and prevention.
Unlike the case of a virus triggering a pandemic where the biomedical scientific strategy for combatting it is relatively clear, brain disorders present significant, complex challenges and involve many unknowns. While depression and related disorders have a strong neurobiological basis (1), our biological insights are not yet sufficiently complete to be fully translated into clinical practice. This starts with their classification—mood and anxiety disorders are clearly heterogeneous and highly interrelated but are currently diagnosed solely on the basis of behavioral abnormalities, with no biological measures to assist diagnosis (2). Yet, the magnitude and impact of these ill-defined mood and anxiety disorders are staggering and the recent increase in their incidence is truly alarming.
Prior to the 2019 Covid-19 pandemic, it was already established that Major Depressive Disorder (MDD) and anxiety disorders are among the leading health burdens globally (3). Within the first year, the pandemic triggered a dramatic rise in these disorders, adding an estimated 53 million cases of MDD and 76 million cases of anxiety disorders globally, representing an approximately 25% increase in the incidence of these disorders (4). The magnitude of increase in mood and anxiety disorders in any given country was highly correlated with the magnitude of the impact of the Covid-10 pandemic on that country. Moreover, younger people and females in particular have been more profoundly impacted by the pandemic than other groups (4). Individuals in certain professions, such as healthcare workers (5), and those confronting economic and social challenges or experiencing racial discrimination were especially affected as well (6).
Hidden behind these statistics are additional sobering facts: Mood and anxiety disorders are typically chronic relapsing disorders that alter the brain in complex ways (1). Their rising incidence in children, adolescents, and young adults is particularly concerning because, if left untreated, they will have consequences for decades. They also increase the risk for other illnesses such as cardiovascular disease and inflammation (7, 8) and have a profound impact on the individual, their family, and society more broadly. It is therefore no exaggeration to conceive of the current mental health crisis as a pandemic—i.e., an instance wherein a disease with significant consequences has spread rapidly across the globe. In addition, while not contagious in the strict viral sense, mood and anxiety disorders are contagious in the societal sense, as evidenced by their dramatic rise in certain communities and specific populations. It is therefore essential to work toward limiting not only the spread but also the duration of this wave of severe distress that so many are experiencing.
What Can Science Do?
While the scope and nature of the challenge of this second pandemic are daunting, there is much that science can offer to alleviate it. This requires a clear vision of what can be achieved in the immediate term, coupled with a thoughtful, strategic, and well-integrated plan for the longer term.
During the last few decades, we have made major strides in our understanding of the biological underpinnings of mood and emotions ranging from genetic to societal factors, with a wealth of knowledge at the molecular, cellular, neurocircuit, and behavioral levels. As importantly, science has reframed the discourse around these illnesses and has debunked many overly simplified ideas about the biology of mood and anxiety disorders—the notion that it is a “chemical imbalance” of a single neurotransmitter system (e.g., serotonin); the notion that a handful of genes will emerge as the cause of these disorders and allow ready treatment targets; and even the idea that the name of any of these disorders—depression, anxiety, PTSD—signifies a single entity. We have begun to confront the complexity and heterogeneity of these disorders and herein lies the hope for dealing with them in a clear-eyed and strategic manner.
A good analogy might be the trajectory of cancer research over the last few decades. While “cancer” is an important umbrella term, key to the progress has been fundamental research in cell signaling, growth, and death, and the innumerable ways these mechanisms can become dysregulated. But equally important is the reliance on clinical insights about the nature, heterogeneity, and complexity of multiple types and subtypes of cancer as a framework within which fundamental research questions are articulated. Indeed, it is this marriage of confronting complexity and uncovering fundamental biological mechanisms that has inspired the precision approaches to certain types of cancers and their treatment. However, it is notable that even for cancers, which are far simpler than mental illness—where a tumor can be detected, characterized at the molecular level, excised, and monitored regularly, the journey has been long and arduous. We are more than half a century since the creation of the National Cancer Institute and the “war on cancer,” yet are only now beginning to see advances in precision cancer treatment reach the clinic.
The challenge is much greater for depression and other related disorders where the illness itself is enormously harder to capture. But, as in the case for cancer where cell signaling, growth, and death represent a shared biological framework, mood and anxiety disorders have a common biological underpinning that serves as a starting place for understanding these disorders at a mechanistic level: the stress system, which will be briefly described below. Stress biology also forms a nexus for both immediate action to combat the current mental health crisis and for advancing our fundamental understanding of these disorders in the longer term and arriving at novel, targeted treatment approaches. The partnership between fundamental and clinical research, the recognition of complexity and need for greater specificity and precision, the importance of removing stigma, and forging a strong alliance with the public are all key lessons that must be adapted from cancer research and other fields of medicine to help meet the current mental health challenge.
Role of Science in the Short Term.
First and foremost, clinicians, clinical scientists, and basic scientists need to articulate and communicate a coherent view of mood and anxiety disorders that captures both the reality of these illnesses and our best understanding of their causes, trajectory, and treatment options. In most Western societies, we have made significant strides in diminishing stigma, but there remain numerous misconceptions about the nature of these disorders. This task is daunting because of the huge range of cultural, social, and political differences in views of emotions, mood, and even the ability of the individual to control them. Recently, the World Health Organization (WHO) issued a remarkable report arguing that “mental health and access to mental health care are a basic human right” and defining many strategies for integrating mental health in overall health systems, creating community mental health mechanisms, and confronting the problem in a culturally sensitive and realistic manner (9).
As will be argued in several of the articles in this special issue, the emergence of depression and other mood disorders results from the interplay of biological, developmental, and environmental factors. Moreover, the environment plays a disproportionately greater role in illnesses such as unipolar depression relative to other psychiatric disorders such as autism, schizophrenia, and bipolar disorder (see ref. 1). This presents an opportunity for immediate intervention at the environmental level.
In this context, scientific knowledge can be deployed at multiple levels:
-
a)
National and global level: marshalling the scientific evidence for prioritizing mental health as a target and adopting the notion put forth by the WHO that mental health care is a human right.
-
b)
State, municipal, and local level: guiding public policy for reducing stress and its damaging consequences by creating an integrated infrastructure to address mental health issues within school systems, workplaces, and the broader community.
-
c)
Health care system: increasing awareness about the mental health crisis among physicians, nurses, medical students, residents, and other mental health workers; providing much-needed resources to consider the affective status of patients and their families; and incorporating evidence-based approaches into treatment programs.
-
d)
Individual level: providing scientifically based guidelines to shape “lifestyle” interventions to reduce stress and induce resilience to stress. This includes behavioral interventions, diet, nutrition, exercise, digital hygiene (e.g., safe use of social media), and others.
Critical to this approach for immediate interventions is the dissemination of concepts that are backed by strong scientific evidence. This includes the following broad ideas:
-
(1)
Clinical depression, anxiety, PTSD, and other mood and anxiety disorders are treatable illnesses, and early treatment is highly advisable. There is a wide range of treatment modalities including different classes of psychotherapy, pharmacological approaches, transmagnetic stimulation, and their combination. New treatment strategies (including circuit-based approaches involving deep brain stimulation) are continuously emerging and being validated. Treatment can and should be tailored not only to the nature of the illness but to the age, gender, and health status and cultural context of the individual.
-
(2)
There are multiple paths to depression and other mood disorders, and these represent the start of a precision approach to treatment and prevention. Genetic predisposition is important, but with heritability rates of <35%, it can be superseded by environmental factors, some of which can be highly protective (e.g., a supportive environment especially in early life), while others (e.g., severe or repeated trauma) can trigger depression in the most biologically resilient individuals.
Importantly, some of these paths are related to other aspects of health and can therefore be addressed by the individual and their healthcare providers to decrease the likelihood of becoming depressed in the first instance. A striking example is the well-established correlation between metabolic syndrome and depression (10) and the more recent evidence that insulin resistance (IR) alone, even in the absence of diabetes, greatly increases the risk of subsequent depression (11), strongly suggesting that the increased incidence of obesity is likely one factor contributing to the recent rise in depression. These insights offer an opportunity for interventions that involve changes in diet and exercise and where the impact can be tracked using indices of IR. As importantly, this may define a subtype of metabolic depression with unique biomarker profiles and distinct behavioral and pharmacological treatment approaches that would be consistent with a precision approach to this illness. A parallel, indeed related, argument can be made for the role of inflammatory processes in depression (8), a topic which is addressed in detail in the paper from the Russo group in this issue (12). It is also notable that new treatments are beginning to emerge for specific triggers of mood disorders, such as postpartum depression.
-
(3)
Resilience represents more than the absence of vulnerability. In addition, just as there are multiple types of vulnerability to depression, there are also multiple types of resilience. This is a relatively new emphasis in the neurobiology of emotions that underscores the idea that resilience involves active counter-regulatory mechanisms that oppose susceptibility. This is especially important in uncovering strategies that can enhance resilience even in highly susceptible individuals, and even in the face of strong genetic, developmental, and neurobiological predictors of vulnerability. Many of these approaches involve psychotherapeutic intervention that helps the individuals conceptualize their emotional responses in more adaptive ways and provide cognitive tools that enhance flexibility and adaptability (13).
There is a clear need to identify the conditions under which genetic versus nongenetic mechanisms of resilience play a critical role and to uncover their underlying mechanisms. The contribution by Turner et al. (14) in this issue offers an example of multiple types of vulnerability and resilience to depression before and during the Covid-19 pandemic.
Role of Science in the Longer-Term Discovery and Translation.
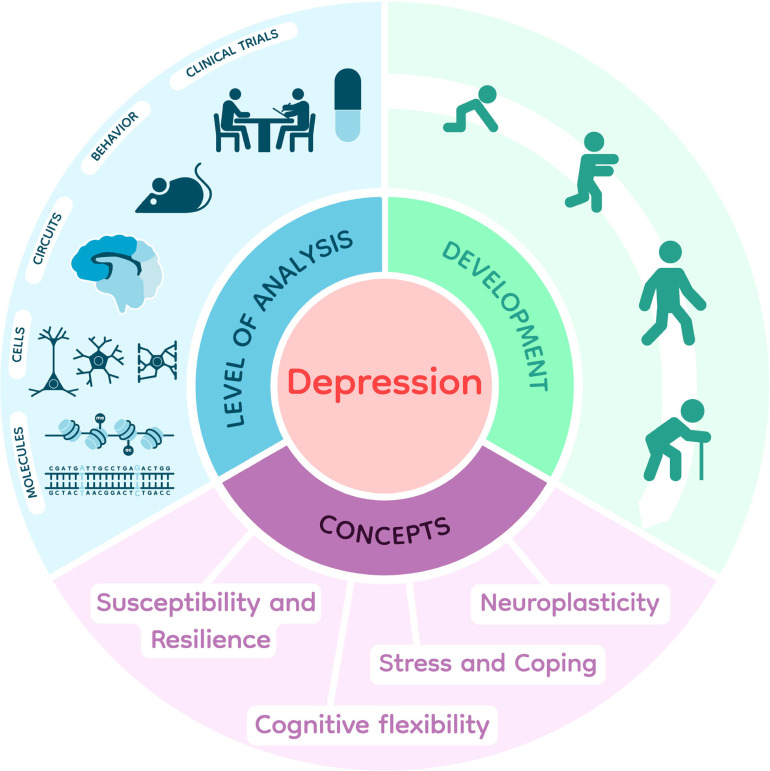
The concepts summarized above that inform the short-term approaches to confronting the mental health crisis also offer a framework for the longer-term scientific questions aimed at achieving a better fundamental understanding that will enable us to target, limit, and ultimately prevent the course of these disorders. Fig. 1 captures some of the key concepts of direct relevance to understanding the neurobiological mechanisms of depression and other mood disorders, highlighting the role of stress biology and the differential responsiveness of individuals to perceived stress, leading to susceptibility or resilience to life events. It points to the interplay of genetics, developmental, gender, and experiential variables in shaping stress responsiveness. It also underscores the importance of utilizing multiple levels of analysis coupled with a range of tools to understand the causes of mood and anxiety disorders, to identify strategies to prevent them and to devise novel and better-targeted approaches for treating them.
Fig. 1.
Framework for studying stress, depression, and other mood disorders. The figure highlights the importance of utilizing broad-based experimental approaches across several levels of analysis, across the lifespan, and across species (rodents, nonhuman primates, and humans) to delineate the biological basis of stress susceptibility vs. resilience and of human stress disorders. Courtesy of Elisabeth Binder, Max Planck.
The Basic Science of Mood and Anxiety Disorders: Stress Biology and Stress Responsiveness
Stress biology represents the interface between an organism and its environment. The stress system, which is highly conserved, has evolved to enable an organism to respond to its environmental context to optimize coping with current conditions and to enhance survival. It therefore needs to be both highly reactive and capable of long-term adaptation. The popular view of “stress” as a negative force is incomplete and rather misleading. Responding to the environment and learning from experience is highly adaptive and critical for survival. It is only when environmental demands exceed the individual’s capacity to adapt, either because of the magnitude or duration of the stressors or the inherent susceptibility of the individual, that coping comes at a high biological cost, resulting in both psychologically and physiologically adverse consequences. Thus, stress biology is not simply an alarm system, but rather an ongoing monitoring process that optimizes functioning in various environments. In addition, as is the case for any essential biological process, its dysregulation can lead to significant consequences, including mood and anxiety disorders.
Basic Physiology of the Stress System.
The concept of stress as a subject of biological research took shape over a hundred years ago, with Walter Cannon focusing on acute stress responses and first identifying the role of the autonomic nervous system in “flight or fight” (15), followed by Hans Selye who focused on the impact of chronic stress, defining “a Syndrome Produced by Diverse Nocuous Agents”, and implicating the pituitary and the adrenal glands in the physiological response (16). The role of the brain in controlling the stress response emerged in the 1950s and 1960s with the birth of neuroendocrinology. Since then, much has been learned about the major physiological stress response cascade otherwise known as the hypothalamic–pituitary–adrenal axis (HPA axis). Key molecular players in the stress cascade include the hypothalamic corticotropin-releasing factor (CRF) which represents the final common path of brain signals that trigger the peripheral endocrine stress response; adrenocorticotropic (ACTH) which, upon CRF stimulation, is released from the anterior lobe of the pituitary gland into the general circulation, targets the adrenal cortex and stimulates the synthesis and release of the glucocorticoid stress hormones, cortisol in humans and corticosterone in rodents (17). Circulating glucocorticoids exert their actions through two major steroid hormone receptors, the glucocorticoid receptor (GR) and the mineralocorticoid receptor (MR). These ligand-activated transcription factors are expressed in the cells of most organs to regulate glucose utilization, energy consumption, and the overall physiological response to stress. Importantly, GR and MR are also present in the brain, with especially high expression levels in the hippocampus, and act through both classic genomic effects as well as nongenomic plasma membrane mechanisms to modify neural activity (18). At the broad physiological level, GR activation in the hippocampus and cortex signals the presence of high levels of circulating stress steroids and triggers mechanisms of negative feedback that terminate the endocrine stress response (19, 20). Each one of these molecules and associated genes is part of complex signaling mechanisms that have been implicated in depression and other mood disorders. An example from the Binder group (21) in this issue focuses on the relationship between the molecular regulation of GR and associated genes and stress-related disorders including depression and ways to mine these discoveries for novel therapeutics.
While we are using stress as a general term, there are many distinct classes of stressors—i.e., stimuli that trigger the physiological stress response, including physical stressors, metabolic and physiologic stressors, and psychosocial stressors. Each can vary in terms of magnitude and duration and is colored by an individual’s intrinsic reactivity to and past experience with that class of stress, and the environmental context in which it occurs. Yet, remarkably, a final common path is to converge on the HPA axis and trigger a shared physiological response.
“Good Stress” and “Bad Stress”—Relationship to Neuroplasticity, Vulnerability, and Resilience.
While it is common to think of stress in negative terms, stress biologists underscore the importance of the acute stress response in preparing the organism to cope with environmental demands, harnessing sources of energy, shaping and fine-tuning strategies for active or passive coping and enhancing cognitive functions to facilitate learning from experience. Thus, a healthy stress response is considered “good stress” and has a well-defined set of physiological characteristics. It entails a rapid rise in circulating ACTH which triggers a subsequent rapid rise in glucocorticoids in response to the stressor. However, it also involves a swift termination of the endocrine stress response that is mediated via well-established negative feedback mechanisms (19, 20). An adaptive stress response can be seen as the first step in building neurobiological preparedness for future stressors of the same general class—i.e., inducing resilience or an enhanced ability to cope. Indeed, we have previously proposed that initial activation of glucocorticoids and their receptors is a key early step in inducing resilience (22).
Key to learning from experience and building resilience are mechanisms of adaptive neuroplasticity, the ability of the brain to physically reshape itself in response to demand. One important example of neuroplasticity is hippocampal neurogenesis, whereby a specific region of the hippocampus, the dentate gyrus, maintains stem cell activity within the adult brain and regulates the rate of cell birth and death and the integration of newly born neurons in existing neural circuits (23, 24).
By contrast, sustained, chronic, and traumatic stress, which is consistent with the most extreme negative connotations associated with the term, has severe negative consequences at the biological level, both in terms of brain and peripheral systems (17). Chronic, uncontrollable stress prevents a full return to homeostasis (i.e., interferes with the termination of the healthy stress response) and results in ongoing biological expenditures that lead to “a new normal”–termed allostasis. It comes at a significant biological cost, termed “allostatic load,” which has long-term consequences on both neural and peripheral functions (25). Thus, chronic stress is a primary trigger for mood and anxiety disorders and enhances vulnerability to a range of other disorders including diabetes, cardiovascular disease, cancer, and immune disorders. In parallel, allostatic load triggers mechanisms of maladaptive neuroplasticity, such as the inhibition of neurogenesis, coupled with a decrease in certain growth factors (26) such as brain-derived growth factor (BDNF) or fibroblast growth factor 2 (FGF2), that are essential for neural remodeling (27–28).
In sum, the impact of stress on the brain is determined by its type, timing, and duration and the ability of the individual to cope with it, with the potential to alter the very structure as well as the function of key brain circuits to either induce resilience or vulnerability to subsequent stressors.
Stress Responsiveness: Genetics, Temperament, Experience, and Stress Disorders.
A great deal of evidence shows that psychosocial stress is an initial trigger of clinical depression as well as a trigger of relapse in many individuals who are in remission from these illnesses (29). This is also the case for other mood and anxiety disorders, e.g., PTSD. However, the relationship of stress to these disorders is more profound than simply being an environmental precipitating factor. Indeed, these illnesses can be construed as disorders of stress reactivity, the way autoimmune disorders are diseases of immune responsiveness. Both the stress and the immune systems have evolved as critical defense mechanisms against a potentially threatening world. However, these mechanisms can become overactive or dysregulated and cause damage in their own right. Indeed, a large GWAs study on depression highlighted the HPA axis as one of the top gene pathways associated with risk for depression (30).
Thus, the biology of susceptibility or resilience to depression is closely linked to the biology of stress reactivity—i.e., the process of perceiving and evaluating different types of stressors, coping with them at both physiological and behavioral levels, and being shaped by experience in anticipation of subsequent exposure. This conceptualization leads directly to the idea of individual differences in reactivity to stress. Indeed, the same event, for example, skydiving, can be perceived as the ultimate fun by one individual and highly anxiety provoking by another. Lifelong patterns of stress reactivity are called temperaments and predispose the individual to different types of psychiatric disorders. Temperamental traits are normally distributed, with one extreme representing those who are highly risk-averse and prone to anxiety and the other extreme representing those who seek risk and find it exciting and rewarding. The anxious phenotype is prone to so-called “internalizing disorders”, such as clinical depression, anxiety, and PTSD, while the risk-taking phenotype is prone to so-called “externalizing disorders”, such as conduct disorders, antisocial personality, and substance use disorders. One of the papers in this issue from the Kalin laboratory (31) focuses directly on the brain circuitry associated with anxious temperament in nonhuman primates.
Both human and animal studies have demonstrated the genetic basis for these temperamental tendencies (32–33). Indeed, uncovering genetic variations associated with temperament may prove more fruitful than searching more specifically for the genetic basis of major depression which, as noted above, has proven to be challenging given the many hundreds of loci that likely contribute to risk, with each contributing a minuscule effect.
Beyond genetic and temperamental variables, there are several other key factors that shape susceptibility to mood and anxiety disorders. A major variable is sex. It is well established that women and girls have approximately twice the risk for depression and anxiety disorders than men and boys, and this trend continued during recent years, with the Covid-19 pandemic having a dramatic impact on females, as exemplified in the work from the Akil group in humans (14). There is also increasing evidence that the molecular pathology associated with depression in males overlaps by only ~10% with that in females as assessed with genome-wide transcriptomic measures (34), highlighting the fact that stress-related disorders may be biologically distinct between the two sexes.
Equally important in modifying susceptibility and resilience to depression is experience, which triggers both epigenetic changes and neural remodeling that modify the stress circuitry. This is especially true during early childhood and adolescence, which are considered “critical periods” for shaping the neural circuitry of emotionality and its molecular underpinnings (35). Adversity during development is a major risk factor for depression, not only increasing the odds but also accelerating the initial incidence of the illness (36).
Multiple Levels of Analysis and the Role of Animal Models.
The brain is a biological computational machine, and as such it relies on all the classic elements of biological systems, at the genetic, molecular, and cellular levels, but also adds a layer of integration via the use of neural circuitry. Thus, networks of neurons and associated glial cells work in a coordinated manner, often across multiple brain regions, to control neural functions, including responsiveness to multiple types of stressors (37). As importantly, the functions of the brain include encoding environmental context, adapting its responses to that context in shaping behavior, and using experience to learn and reprogram itself to finetune future responses. Environmental context ranges from the individual’s immediate physical setting in a given moment to the psychological, social, and cultural context over the lifespan.
Understanding stress biology and its relationship to mood and anxiety disorders requires analysis at all these levels of brain function—at the genetic and epigenetic, molecular, cellular, and circuit levels. It requires consideration of differential responsiveness to the environment based on both the characteristics of the individual, including age, sex, and other biological factors, as well as characteristics of their environment. As such, this field of research relies on all the tools of modern biology and computational sciences, as is exemplified in this issue.
Animal models have been invaluable in understanding the fundamental mechanisms of stress biology and their relationship to mood and anxiety disorders (1, 17). They are especially critical in dissecting the role of genetics, experience, and other variables that shape susceptibility or resilience to stress. As noted above, there are genetic rodent models that capture traits of relevance to internalizing vs. externalizing disorders (33). In addition, there are models that demonstrate the differential impact of experience even in inbred mice which share the same genetic background. One of the leading rodent models of depression and other human stress disorders, chronic social defeat stress, illustrates how social stress in a specific inbred strain of mice results in a range of behavioral phenotypes, with animals at one end of the spectrum termed resilient (i.e., they maintain mostly normal behavioral function despite the social stress), while animals at the other end of the spectrum termed susceptible exhibit numerous behavioral abnormalities (38), as well as alterations in gene expression patterns (39) that mimic human depression or related disorders. The consideration of stress resilience in animal models marks an important milestone in stress research because it provides a path toward discerning whether stress-related changes observed in humans mediate adaptive, coping mechanisms or instead mediate stress-induced abnormalities. The paper from the Peña group (40) in this issue relies on the chronic social defeat animal model and highlights the impact of early-life stress and its interaction with sex in shaping neural expression profiles with and without treatment with antidepressants.
Treating Depression.
It is notable that classical antidepressant treatments were not originally conceptualized in relation to stress biology, susceptibility-resilience, or neuroplasticity. Rather, the original tricyclic antidepressants emerged through serendipity and were only later found to act primarily by inhibiting monoamine reuptake (41) Through reverse translation, this led to the “monoamine hypothesis” of depression, namely, that monoaminergic systems in the brain, especially noradrenergic and serotonergic pathways, were dysregulated and causal in the emergence of clinical depression. This led to the next generation of more selective antidepressants, the specific serotonin-reuptake inhibitors (SSRIs), the selective noradrenaline reuptake inhibitors (SNRIs), and drugs with both targets. While effective in a significant proportion of patients suffering from depression, these drugs require several weeks before exerting their full antidepressant effects, in spite of the fact that their impact on brain levels of serotonin or noradrenaline becomes maximal within a few days. This raised questions about the validity of the concept that depression consisted of a simple “serotonin imbalance”. Rather, the delay in their effectiveness led to the hypothesis that neural remodeling is essential for their action and that growth factors are mediators of this neural remodeling (42). This represented the start of a convergence with the conceptualization presented above that “bad stress” and the resulting allostatic load can modify the brain in harmful ways, disrupt normal neuroplasticity, and play a causative role in depression. In turn, treating depression, likely through a combination of pharmacological and behavioral approaches, requires either reversing the deleterious effects of stress or, rather, inducing mechanisms of resilience. As will be described in the review by Krystal (43), there are more recent treatments for depression, such as ketamine, that are rapidly acting, are thought to target the NMDA glutamate receptor, and induce resilience-associated neuroplasticity more swiftly than classical antidepressants. Additionally, nonpharmacological treatment modalities, such as deep brain stimulation and transcranial magnetic stimulation, have emerged that target the neural circuitry implicated in affect regulation and depression.
Together, these new treatments promise to help a significant proportion of patients who suffer from so-called treatment-resistant depression, i.e., individuals who do not respond to classical antidepressants. Nevertheless, much remains to be done in harnessing the molecular discoveries that are emerging from animal models and postmortem human studies and are implicating a large number of novel molecular and cellular mechanisms in the regulation of affect and as possible causal factors in mood disorders, including the role of other cell types in the brain such as astrocytes and microglia. Given the complexity of the causes and manifestations of these illnesses, it is essential to develop biomarkers to identify the multiple paths to depression and related affective disorders and the unique biological signature in distinct groups of patients as a key step to achieving a true precision approach to the treatment of these illnesses.
In This Issue
This special issue offers examples of the scientific advances being made, spanning animal models to human translation. The proposed contributors illustrate new tools and techniques being deployed in understanding the biology of stress, highlight developmental and sex differences as key factors, describe the complex interplay between genetic and environmental variables, discuss biomarkers of vulnerability or resilience in humans, and frame a new understanding and recent directions in the treatment of human depression and related stress disorders that do not fully respond to currently available therapies.
Transcriptional Signatures of Early-Life Stress and Antidepressant Treatment Efficacy, by Toriano Parel et al. (Peña Laboratory) (40).
As noted above, early-life stress significantly increases the risk for depression. It also appears to reduce responsiveness to antidepressants and increase the odds of treatment-resistant depression. This study integrates bioinformatic analyses in humans and in mice undergoing the chronic social defeat stress to better understand why early-life stress is associated with poorer antidepressant treatment outcomes, especially in females. The study focuses on the overlap between genome-wide data from humans and mice treated with different antidepressants to arrive at predictors of treatment responsiveness or treatment resistance. This is followed up by in vivo pharmacological studies to investigate how early-life stress induces molecular changes that may mediate altered antidepressant responses. Notably, early-life stress in mice induces a gene expression profile in the nucleus accumbens which resembles the expression profile associated with antidepressant treatment failure in humans. Transcriptional patterns predicting treatment failure were strongest among female subjects (mice and humans), consistent with a greater risk for depression among women. Together, this research provides important neurobiological support for the clinical notion that depressed individuals—and particularly women—with a history of early-life stress constitute a unique subpopulation of patients, have unique and long-lasting transcriptional signatures in the brain, and may need unique treatment strategies.
Gene Expression in the Primate Orbitofrontal Cortex Related to Anxious Temperament. By Kenwood et al. (Kalin Laboratory) (31).
This research article provides a brief review of the work from this group on the relationship between temperamental tendencies, stress reactivity, and susceptibility to the development of affective disorders in a nonhuman primate model of behavioral inhibition. Anxious temperament, the lifetime tendency to experience high levels of anxiety and enhanced responses to potentially threatening situations, can be identified early in life and is a well-established risk factor for the later development of pathological anxiety, depression, comorbid substance abuse, and other stress-related disorders. By working with a large cohort of preadolescent rhesus monkeys and preadolescent children, Kalin’s group has developed and validated a highly reliable nonhuman primate model of anxious temperament that is directly translatable to humans. Using similar neuroimaging methods across young monkeys and children, they have established the neural circuity that underlies individual differences in this at-risk temperament, which includes the orbitofrontal cortex, a frontal region which interacts with subcortical regions to modulate responses to potential threats. In the current study, they use laser capture microdissection and RNA sequencing to characterize the transcriptional properties of neurons in the deep and superficial layers of the orbitofrontal cortex as they relate to individual differences in anxious temperament. Several previously implicated molecular systems, including the GR and neurotrophic signaling, are highlighted as potential mechanisms underlying temperamental variability. Transcriptional heterogeneity between neurons in deep and superficial layers is explored, as well as cellular heterogeneity within the region using single-cell sequencing. Finally, as the cohort included in this study comprises both males and females, transcriptional differences related to the interaction of sex and anxious temperament are explored. Together, this work provides a thorough characterization of the transcriptional landscape of the primate orbitofrontal cortex with respect to anxious temperament, laminar and cellular organization, and sex, highlighting several potential molecular pathways that influence individual differences in this highly translational primate model for stress-related psychopathology. These novel findings in nonhuman primates can guide the development of new, neurobiologically informed treatments for enhancing resilience and decreasing the burden associated with stress-related disorders.
Social Stress Induces Autoimmune Responses against the Brain, by Shimo et al. (Russo Laboratory) (12).
This original research paper focuses on the observation of high comorbidity between autoimmune disorders and psychiatric disorders, including MDD. This series of studies seeks to identify the processes by which stress impacts the adaptive immune system and the implications of such responses in depression. This involves studies of antibody responses and autoimmunity in the chronic social defeat stress model in mice and parallel studies in clinical samples from patients with major depression. In the animal model, multiple measures show increased immune responses following stress especially in susceptible individuals and increased levels of reactivity of these antisera against brain tissue correlating with social avoidance behavior in mice. Similarly, in humans, increased peripheral levels of brain-reactive IgG antibodies are associated with increased anhedonia. These and other findings provide novel mechanistic insights connecting stress-induced autoimmune reactions against the brain and stress susceptibility. Depletion of antibody-producing cells from mice results in increased stress resilience, suggesting a possible causal link between antibody responses and stress susceptibility. The authors suggest that therapeutic approaches targeting autoimmune responses may offer a useful strategy in treating the specific subset of patients with major depression who feature immune abnormalities.
High Throughput Screening of Glucocorticoid-Induced Enhancer Activity Reveals Mechanisms of Stress-Related Psychiatric Disorders, by Penner-Goeke et al. (Binder Laboratory) (21).
This original research article seeks to identify molecular mechanisms whereby genetic factors moderate the impact of stress and other adverse life events on risk for psychiatric disorders, including major depression. The authors present data from massively parallel reporter assays for over 3,500 SNPs (Single Nucleotide Polymorphisms) that identify several hundred genetic variants that moderate enhancer responses to GR activation. The paper provides functional annotation of both inductive and repressive enhancers, coupled with CRISPR-Cas9 validation of selected targets. The work demonstrates that these SNP variants regulate transcripts enriched for genes differentially expressed in postmortem brain of subjects with psychiatric disorders. Furthermore, phenome-wide Mendelian randomization analysis of over 4,000 phenotypes reveals potentially causal associations of these functional variants in specific neurobehavioral traits. Finally, the study reports that functional gene scores derived from these variants are significantly associated with differences in physiological stress measures, suggesting that these may alter disease risk by moderating the individual set point of the stress response. Thus, this study provides strong evidence that genetic variants modulating the transcriptomic response to glucocorticoids may be causally involved in major depression, possibly by influencing the physiological stress response and stress-responsive brain transcription.
Stress, Genetics and Mood: Impact of COVID-19 on a College Freshman Sample by Turner, Khalil et al. (Akil Laboratory) (14).
This original research paper describes the Michigan Freshman Study, a multiyear longitudinal effort that characterizes the vulnerability or resilience to life stress and defines the genetic and environmental factors that trigger significant symptoms of clinical depression or anxiety in young healthy human subjects. The study follows college freshmen from the start of the academic year through the following summer and into the fall of their sophomore year, gathering genetic data, behavioral and sleep data, stress and neuroendocrine data, and tracking affective states with measures of clinical symptoms of depression and anxiety. The report spans a prepandemic cohort as well as two consecutive cohorts of freshmen following the start of the Covid-19 pandemic. The study captures the significant impact of the pandemic on mental health in college students, especially in females. It characterizes the interplay of genetics and environment (including the magnitude of stress conditions) in shaping stress vulnerability vs. resilience. It describes the predictive power of the polygenic risk score for depression (MDD-PRS) prior to the pandemic and how the pandemic eradicated the relationship between this genetic index and susceptibility to depression and anxiety, especially in young women. By contrast, a baseline Affect Score derived through machine learning proved to be highly predictive of susceptibility or resilience to subsequent stress, both prior and throughout the pandemic, regardless of gender. Implications are discussed including the concept of genetic and nongenetic resilience to stress and depression.
New Concepts and Approaches to Treatment Resistant Depression by Krystal et al. (Krystal Laboratory) (43).
In this review paper, Krystal and colleagues first discuss the classical approaches to the treatment of depression and the associated monoamine hypothesis. They then summarize progress with novel treatments now available for depression and their implications for future research strategies. Ketamine and its S-enantiomer, termed esketamine, were the first rapid-acting antidepressants to be identified. Their discovery was associated with the emergence of new perspectives of antidepressant-related neuroplasticity that could support these strikingly fast and robust effects. This review updates our understanding of the mechanisms through which ketamine produces its antidepressant effects. It outlines strategies to extend these effects and discusses potential alternatives to ketamine. At the mechanistic level, it highlights two complementary forms of neuroplasticity (nonhomeostatic and homeostatic) that might contribute to ketamine efficacy. The paper also reviews strategies for extending the efficacy of ketamine, including behavioral interventions during and 24 hours after infusions, as well as cotreatment with an mTORC1 inhibitor. New treatment strategies are highlighted which involve targeting downstream signaling mechanisms (e.g., GABAA a5-containing receptors, mGluR2, AMPA glutamate receptors, BDNF, TrkB, and mTOR). Lastly, the review discusses convergence and divergence between ketamine and psychedelic drugs and points to future directions for continuing to enhance the armamentarium for treating severe depression.
Together, these contributions capture some of the rich, multifaceted scientific strategies being used to uncover the biological and psychosocial mechanisms that are contributing to the current mental health crisis. The combination of shorter-term interventions which could be initiated immediately with the highly promising scientific insights that will lead to precision treatments for human stress disorders provides the hope but also the expectation for using scientific knowledge to confront the second pandemic.
Acknowledgments
H.A. is supported by the Office of Naval Research Grants N00014-09-1-0598, N00014-12-1-0366 and N00014-19-1-2149, National Institute on Drug Abuse (NIDA) U01DA043098, the Hope for Depression Research Foundation, and the Pritzker Neuropsychiatric Disorders Research Consortium Fund (http://www.pritzkerneuropsych.org). E.J.N. is supported by NIMH R01MH129306 and R01MH051399 and the Hope for Depression Research Foundation.
Author contributions
H.A. and E.J.N. wrote the paper.
Competing interests
The authors declare no competing interest.
References
- 1.Akil H., et al. , Treatment resistant depression: A multi-scale, systems biology approach. Neurosci. Biobehav. Rev. 84, 272–288 (2018), 10.1016/j.neubiorev.2017.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, ed. 5, 2013), 10.1176/appi.books.9780890425596. [DOI] [Google Scholar]
- 3.GBD 2019 Disease and Injuries Collaborators, Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 396, 1204–1222 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.COVID-19 Mental Disorders Collaborators, Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 398, 1700–1712 (2021), 10.1016/S0140-6736(21)02143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhu H., Yang X., Xie S., Zhou J., Prevalence of burnout and mental health problems among medical staff during the COVID-19 pandemic: A systematic review and meta-analysis. BMJ Open 13, e061945 (2023), 10.1136/bmjopen-2022-061945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eboigbe L. I., Simon C. B., Wang Y. S., Tyrell F. A., The compounded effect of the dual pandemic on ethnic-racial minority adolescents’ mental health and psychosocial well-being. Curr. Opin. Psychol. 52, 101626 (2023), 10.1016/j.copsyc.2023.101626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kwapong Y. A., et al. , Association of depression and poor mental health with cardiovascular disease and suboptimal cardiovascular health among young adults in the United States. J. Am. Heart Assoc. 12, e028332 (2023), 10.1161/JAHA.122.028332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beurel E., Toups M., Nemeroff C. B., The bidirectional relationship of depression and inflammation: Double trouble. Neuron 107, 234–256 (2020), 10.1016/j.neuron.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization, World Mental Health Report: Transforming Mental Health for All (World Health Organization, Geneva, Switzerland, 2022), Licence: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- 10.Pan A., et al. , Bidirectional association between depression and metabolic syndrome: A systematic review and meta-analysis of epidemiological studies. Diabetes Care 35, 1171–1180 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Watson K. T., et al. , Incident major depressive disorder predicted by three measures of insulin resistance: A dutch cohort study. Am. J. Psychiatry 178, 914–920 (2021), 10.1176/appi.ajp.2021.20101479. [DOI] [PubMed] [Google Scholar]
- 12.Shimo Y., et al. , Social stress induces autoimmune responses against the brain. Proc. Natl. Acad. Sci. U.S.A. (2023), this issue, 2023-05778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Southwick S. M., Charney D. S., DePierro J. M., Resilience (Cambridge University Press, ed. 3, 2023). [Google Scholar]
- 14.Turner C. A., et al. , Stress, genetics and mood: Impact of COVID-19 on a college freshman sample. Proc. Natl. Acad. Sci. U.S.A. (2023), this issue, 2023–05779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cannon W. B., Bodily Changes in Pain, Hunger, Fear and Rage: An Account of Recent Researches into the Function of Emotional Excitement (D Appleton & Company, 1915). [Google Scholar]
- 16.Selye H., A syndrome produced by diverse nocuous agents. 1936. J. Neuropsychiatry Clin. Neurosci. 10, 230–231 (1998), 10.1176/jnp.10.2.230a. [DOI] [PubMed] [Google Scholar]
- 17.McEwen B. S., Akil H., Revisiting the stress concept: Implications for affective disorders. J. Neurosci. 40, 12–21 (2020), 10.1523/JNEUROSCI.0733-19.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Kloet E. R., Meijer O. C., de Nicola A. F., de Rijk R. H., Joëls M., Importance of the brain corticosteroid receptor balance in metaplasticity, cognitive performance and neuro-inflammation. Front. Neuroendocrinol. 49, 124–145 (2018), 10.1016/j.yfrne.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 19.Keller-Wood M., Hypothalamic-pituitary–adrenal axis-feedback control. Compr. Physiol. 5, 1161–1182 (2015). [DOI] [PubMed] [Google Scholar]
- 20.Herman J. P., et al. , Regulation of the hypothalamic-pituitary-adrenocortical stress response. Compr. Physiol. 6, 603–621 (2016), 10.1002/cphy.c150015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Penner-Goeke S., et al. , High throughput screening of glucocorticoid-induced enhancer activity reveals mechanisms of stress-related psychiatric disorders. Proc. Natl. Acad. Sci. U.S.A. (2023), this issue, 2023-05773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spencer-Segal J. L., Akil H., Glucocorticoids and resilience. Horm. Behav. 111, 131–134 (2019), 10.1016/j.yhbeh.2018.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kuhn H. G., Toda T., Gage F. H., Adult hippocampal neurogenesis: A coming-of-age story. J. Neurosci. 38, 10401–10410 (2018), 10.1523/JNEUROSCI.2144-18.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Anacker C., Hen R., Adult hippocampal neurogenesis and cognitive flexibility–Linking memory and mood. Nat. Rev. Neurosci. 18, 335–346 (2017), 10.1038/nrn.2017.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McEwen B. S., Stress, adaptation, and disease. Allostasis and allostatic load. Ann. N. Y. Acad. Sci. 840, 33–44 (1998), 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- 26.Tartt A. N., Mariani M. B., Hen R., Mann J. J., Boldrini M., Dysregulation of adult hippocampal neuroplasticity in major depression: Pathogenesis and therapeutic implications. Mol. Psychiatry 27, 2689–2699 (2022), 10.1038/s41380-022-01520-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Duman R. S., Deyama S., Fogaça M. V., Role of BDNF in the pathophysiology and treatment of depression: Activity-dependent effects distinguish rapid-acting antidepressants. Eur. J. Neurosci. 53, 126–139 (2021), 10.1111/ejn.14630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Turner C. A., Watson S. J., Akil H., The fibroblast growth factor family: Neuromodulation of affective behavior. Neuron 76, 160–174 (2012), 10.1016/j.neuron.2012.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Monroe S. M., Harkness K. L., Major depression and its recurrences: Life course matters. Annu. Rev. Clin. Psychol. 18, 329–357 (2022), 10.1146/annurev-clinpsy-072220-021440. [DOI] [PubMed] [Google Scholar]
- 30.Wray N. R., et al. , Genome-wide association analyses identify 44 risk variants and refine the genetic architecture of major depression. Nat. Genet. 50, 668–681 (2018), 10.1038/s41588-018-0090-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kenwood M. M., et al. , Gene expression in the primate orbitofrontal cortex related to anxious temperament. Proc. Natl. Acad. Sci. U.S.A. (2023), this issue, 2023-05775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Poore H. E., et al. , A multivariate approach to understanding the genetic overlap between externalizing phenotypes and substance use disorders. Addict. Biol. 28, e13319 (2023), 10.1111/adb.13319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chitre A. S., et al. , Genome-wide association study in a rat model of temperament identifies multiple loci for exploratory locomotion and anxiety-like traits. Front. Genet. 13, 1003074 (2023), 10.3389/fgene.2022.1003074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Labonté B., et al. , Sex-specific transcriptional signatures in human depression. Nat. Med. 23, 1102–1111 (2017), 10.1038/nm.4386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Peña C. J., et al. , Early life stress confers lifelong stress susceptibility in mice via ventral tegmental area OTX2. Science 356, 1185–1188 (2017), 10.1126/science.aan4491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.LeMoult J., et al. , Meta-analysis: Exposure to early life stress and risk for depression in childhood and adolescence. J. Am. Acad. Child. Adolesc. Psychiatry 59, 842–855 (2020), 10.1016/j.jaac.2019.10.011. [DOI] [PubMed] [Google Scholar]
- 37.Ulrich-Lai Y. M., Herman J. P., Neural regulation of endocrine and autonomic stress responses. Nat. Rev. Neurosci. 10, 397–409 (2009), 10.1038/nrn2647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Krishnan V., et al. , Molecular adaptations underlying susceptibility and resistance to social defeat in brain reward regions. Cell 131, 391–404 (2007), 10.1016/j.cell.2007.09.018. [DOI] [PubMed] [Google Scholar]
- 39.Scarpa J. R., et al. , Shared transcriptional signatures in major depressive disorder and mouse chronic stress models. Biol. Psychiatry 88, 159–168 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Toriano Parel S., et al. , Transcriptional signatures of early-life stress and antidepressant treatment efficacy. Proc. Natl. Acad. Sci. U.S.A. (2023), this issue, 2023-05776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lopez-Munoz F., Alamo C., Monoaminergic neurotransmission: The history of the discovery of antidepressants from 1950s until today. Curr. Pharm. Des. 15, 1563–1586 (2009). [DOI] [PubMed] [Google Scholar]
- 42.Krishnan V., Nestler E. J., The molecular neurobiology of depression. Nature 455, 894–902 (2008), 10.1038/nature07455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Krystal J. H., et al. , Ketamine and the neurobiology of depression: toward next-generation rapid-acting antidepressant treatments. Proc. Natl. Acad. Sci. U.S.A. (2023), this issue, 2023-05772. [DOI] [PMC free article] [PubMed] [Google Scholar]