Abstract
This case report describes a laparoscopic approach using fluorescence imaging guidance to treat gangrenous cholecystitis with perforation (GCP). A male patient in his early 60s presented with 3 days of right upper abdominal pain. Computed tomography and ultrasonography findings were consistent with a stone incarcerated in the gallbladder neck, GCP, and localized peritonitis. Percutaneous gallbladder drainage was initially performed, followed by laparoscopic cholecystectomy 7 days later, using combined intravenous and intracholecystic fluorescent cholangiography. This technique allowed visualization of the cystic and common bile ducts during surgery and enabled safe removal of the diseased gallbladder. The patient recovered well without complications, and reported no pain or discomfort at a 2-month follow-up.
Keywords: Laparoscopic cholecystectomy, gangrenous cholecystitis, fluorescent cholangiography, incarcerated gallstone, gallbladder perforation, abdominal pain
Introduction
Laparoscopic cholecystectomy is the standard treatment for benign gallbladder disease. 1 Percutaneous transhepatic gallbladder drainage is a safe technique for treatment of gangrenous cholecystitis, gallbladder perforation, pericholecystic abscess, and localized or diffuse peritonitis. 2 Early biliary drainage is generally recommended in patients with these diseases and cholecystectomy is performed 1–2 months later. 3 The goal of this approach is prevention of iatrogenic bile duct injury during laparoscopic cholecystectomy; however, having a drain in place for such a long period of time is associated with physical pain and psychological distress.
Intraoperative intravenous fluorescence cholangiography, performed by injection of indocyanine green (ICG) dye through a peripheral vein, can provide real-time images of extrahepatic bile duct structure. Multiple studies have shown that intravenous fluorescence cholangiography may reduce the incidence of bile duct injury.4–6 However, in the present authors’ experience, this technique is often insufficient for displaying the confluence of the cystic duct and common hepatic duct in cases where a stone is incarcerated in the gallbladder neck. Here, the case of a patient with gangrenous cholecystitis and a perforated gallbladder, in whom combined intravenous and intracholecystic fluorescent cholangiography during laparoscopic cholecystectomy was performed after 7 days of percutaneous transhepatic gallbladder drainage, is reported. This approach enabled accurate intraoperative imaging of the cystic and common bile ducts to guide the operation. The patient provided written informed consent for publication of this case report and any accompanying images, and the reporting of this case is in accordance with CARE guidelines. 7
Case report
A man in his early 60s with a history of diabetes presented at hospital in March 2023 with 3 days of right upper abdominal pain. Abdominal computed tomography showed gallbladder swelling and a small amount of fluid between the bottom of the gallbladder and the right lower liver space, suggesting gallbladder perforation (Figure 1). Ultrasonography indicated a small stone incarcerated in the gallbladder neck and approximately 5-mm thickening of the gallbladder wall. Laboratory test results were as follows: procalcitonin, 1.170 ng/ml; leukocyte count, 21.7 × 109 cells/L; and random blood glucose, 19.6 µmol/L. On examination, the patient exhibited tenderness, muscle tension, and rebound pain in the right upper abdomen; Murphy's sign was positive, indicating localized peritonitis. He was diagnosed with gangrenous cholecystitis with perforated gallbladder according to the American Association for the Surgery of Trauma (AAST) grading system, 8 and was admitted to the hospital. Percutaneous transhepatic gallbladder drainage was performed at the bedside (Figure 2a). Enhanced abdominal computed tomography, performed 4 days later, revealed that the percutaneous transhepatic gallbladder drainage tube was in place and fluid collection around the gallbladder had decreased in size (Figure 2b). The patient's condition improved after 7 days of antibiotic treatment and blood glucose regulation, comprising 2 g cefoperazone sodium via intravenous infusion in 100 ml normal saline, every 8 h, 3 times a day, and 20 U insulin before bedtime, 10 U before breakfast, 12 U before lunch, and 12 U before dinner, all by subcutaneous injection. Laparoscopic cholecystectomy was then performed using a laparoscopic fluorescence imaging system (Beijing Digital Precision Medical Technology Co., Ltd, Beijing, China) (Figure 3).
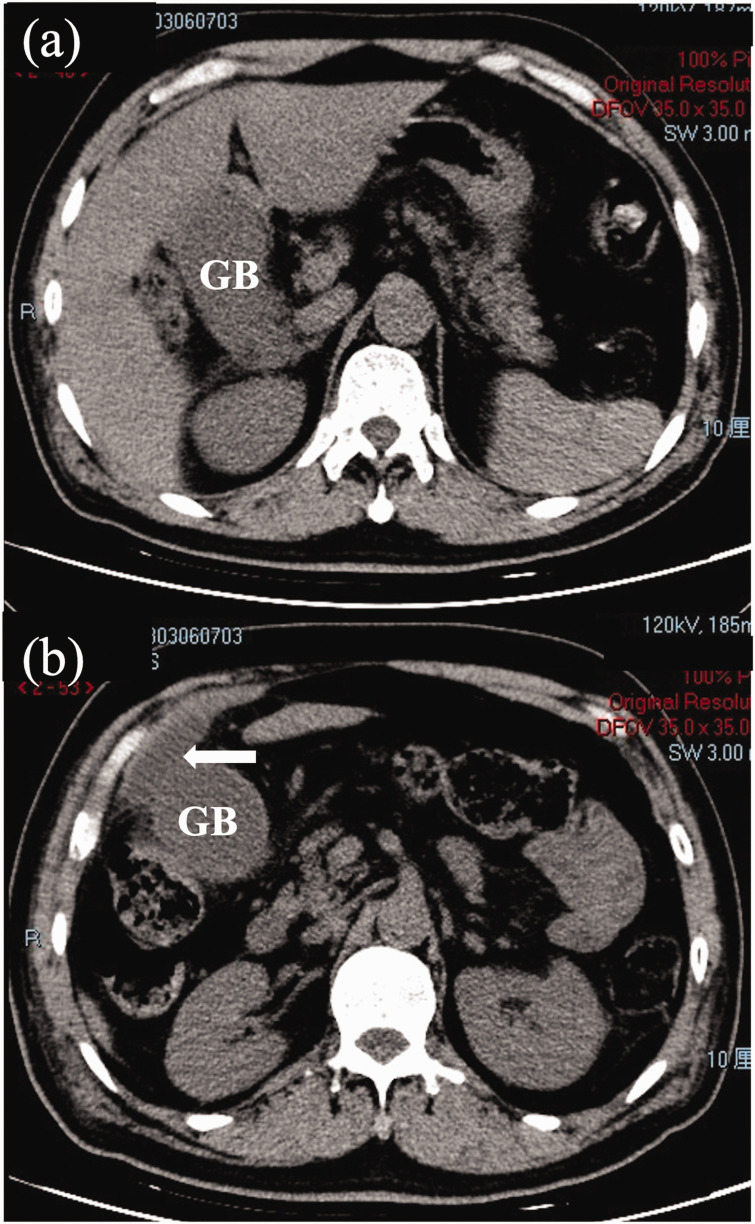
Figure 1.
Abdominal computed tomography axial plane images from a male patient in his early 60s who presented with 3 days of right upper abdominal pain, showing: (a and b) distension of the gallbladder (GB); and (b) a small volume of fluid collection between the GB fundus and right hepatic recess (arrow).
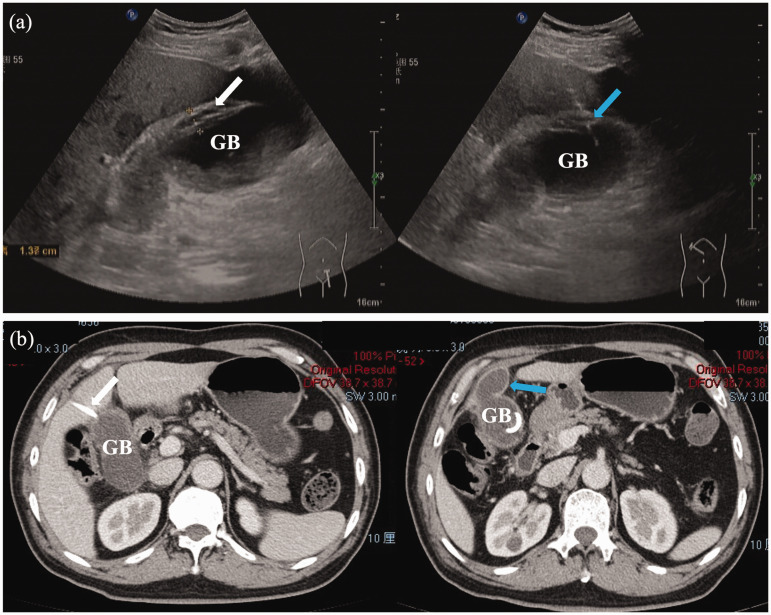
Figure 2.
(a) Images obtained during ultrasound-guided percutaneous gallbladder (GB) drainage performed at the bedside to treat a male patient in his early 60s who presented with 3 days of right upper abdominal pain, showing GB wall oedema (white arrow) and the needle puncturing the GB through the liver parenchyma (blue arrow); and (b) abdominal contrast-enhanced computed tomography axial plane images obtained 4 days later showing proper positioning of the drainage tube (white arrow) and a decreased amount of fluid around the GB (blue arrow).
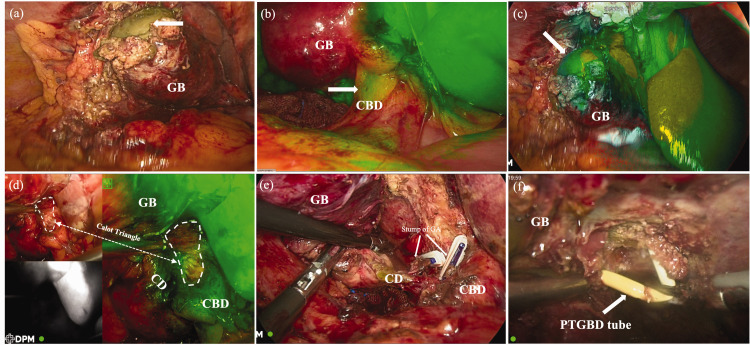
Figure 3.
Images from laparoscopic cholecystectomy performed using comprehensive fluorescence imaging to visualize the gallbladder (GB), cystic duct (CD), and common bile duct (CBD) at 7 days after percutaneous drainage in a male patient in his early 60s who presented with 3 days of right upper abdominal pain, showing: (a) the gangrenous perforation at the base of the gallbladder (white arrow); (b) fluorescence of the common bile duct (white arrow); (c) fluorescence of the gallbladder (white arrow); (d) anatomical localization of the Calot triangle (dashed line) and complete visualization of the critical view of safety enabled by image guidance; (e) successful surgical dissection and ligation of both cystic arteries (GA); and (f) the percutaneous transhepatic gallbladder drainage (PTGBD) tube, which was subsequently removed.
During the operation, gangrenous tissue and perforation were discovered at the bottom of the gallbladder, with an encapsulated adhesion formed between the bottom of the gallbladder and the abdominal wall of the omentum (Figure 3a). At 30 min before pneumoperitoneum was established, 1 ml of ICG dye (2.5 mg/ml) had been injected through a peripheral vein. Fluorescence imaging enabled visualization of the liver and common bile duct during the operation, but not the gallbladder (Figure 3b). Consequently, 4 ml of ICG dye (0.25 mg/ml) was then injected into the percutaneous transhepatic gallbladder drainage tube, resulting in visualization of the gallbladder and cystic duct (Figure 3c) and enabling safe surgical dissection of the Calot’s triangle (Figure 3d). The cystic artery and bile duct were completely exposed, clipped, and severed (Figure 3e). During the process of severing the gallbladder bed, the percutaneous transhepatic gallbladder drainage tube was removed (Figure 3f) followed by removal of the gallbladder. The patient recovered well without complications and was discharged the second day after surgery. He reported no pain or discomfort at a 2-month follow-up assessment.
Discussion
Misidentification of extrahepatic bile duct anatomy is the main cause of iatrogenic bile duct injury during laparoscopic cholecystectomy. 9 To reduce the risk, the critical view of safety (CVS) technique was introduced by Strasberg et al. in 1995. 10 To achieve the CVS, three criteria must be met: 11 (1) clearance of adipose and fibrotic tissues from the hepatocystic triangle without exposing the common bile duct and common hepatic duct, (2) separation of the lower third of the gallbladder from the liver bed to expose the cystic plate, and (3) visualization of only two structures entering the gallbladder. Within this technical framework, surgeons are able to identify crucial anatomical structures, thereby minimizing the risk of accidental injury during surgery. Additionally, this technique aids surgeons in detecting and removing any remaining gallstones, thus preventing postoperative recurrence.12–14 The CVS has been widely acknowledged as the gold standard for cholecystectomy, 11 and the three criteria of the CVS were demonstrated during treatment of the present case (shown in Figure 3e).
Despite reducing risk, the CVS is implemented in approximately only 10% of laparoscopic cholecystectomy procedures, 15 suggesting that its application is more difficult than anticipated. Another option for accurate ductal identification during laparoscopic cholecystectomy is fluorescent biliary imaging guidance, as described by Ishizawa et al. 5 in 2008. In 2015, a systematic review of 16 studies on the use of fluorescent cholangiography in laparoscopic cholecystectomy showed that this technique was highly sensitive in displaying and detecting bile duct anatomy, potentially helping to prevent bile duct injuries, based on a pooled group of 590 patients. 16 However, a study of data from the European Fluorescence Image-Guided Surgery (FIGS) registry revealed a wide disparity in ICG dose and timing in fluorescence cholangiography. 17 During fluorescence cholangiography, where ICG dye is injected through a peripheral vein, an elevated background liver signal is commonly observed, which may hinder the correct visualization of biliary anatomy. To address this interference caused by the background signal, Liu et al. 18 and Gené Škrabec et al. 19 have described two methods for achieving fluorescence cholangiography by injecting ICG directly into the gallbladder, comprising percutaneous transhepatic gallbladder drainage and intra-operative direct gallbladder puncture. The studies identified a limitation of the technique of injecting ICG into the gallbladder, which is that stone obstruction may prevent ICG from entering the common bile duct, thus hindering complete visualization of the extrahepatic biliary system. To overcome this limitation, a novel approach was attempted in the present case by combining the percutaneous transhepatic gallbladder technique with classical fluorescence cholangiography. The percutaneous transhepatic gallbladder technique was utilized to visualize the gallbladder duct on the side of the stone obstruction, while employing classical fluorescence cholangiography to visualize the hepatic and bile ducts on the other side of the obstruction. By merging the fluorescence images from both sides, a rough guidance for anatomical visualization of the hepatocystic triangle was provided. Fortunately, the gallbladder neck and common bile duct was successfully visualized in the present case of stone obstruction (as shown in Figure 3d) and the CVS technique was confidently performed in the non-fluorescent imaging area. In future studies, the present authors plan to expand the study sample to validate the feasibility, safety, and effectiveness of this combined technique.
According to the 2018 Tokyo Guidelines, 2 percutaneous transhepatic gallbladder drainage should be considered as the first alternative to surgical intervention in surgically high-risk patients with acute cholecystitis. This is because several studies have shown that percutaneous transhepatic gallbladder drainage is less invasive and has a lower risk of adverse events compared with cholecystectomy. A meta-analysis conducted by Han et al. 20 found that performing percutaneous transhepatic gallbladder drainage before early laparoscopic cholecystectomy may effectively reduce surgical complexity, postoperative complication rate, and length of hospital stay in patients with moderate acute cholecystitis. The patient in the present case had gangrenous cholecystitis with a perforated gallbladder and a stone incarcerated in the gallbladder duct. Stone incarceration in the gallbladder neck and bacterial invasion may result in insufficient blood supply to the gallbladder and increased tension of the gallbladder wall. This might ultimately lead to a complex type of acute cholecystitis comprising progressive ischemia, necrosis and perforation of the gallbladder wall, and even Mirizzi syndrome caused by compression of the common bile duct.21–23 This type of gangrenous cholecystitis is often accompanied by significant thickening of the tissues in the Calot's triangle region. ICG is known to penetrate only up to approximately 1.0 cm, which may not be sufficient to visualize the bile ducts when they are covered by thickened tissue. Therefore, the method of using intravenous injection of ICG for fluorescence imaging of the extrahepatic bile ducts cannot fully elucidate Calot's triangle. 24 However, these two fluorescence cholangiography CF techniques (intravenous ICG injection and percutaneous transhepatic gallbladder ICG administration) were successfully combined in the present case of gallbladder neck obstruction. This approach reduces the difficulty of subsequent surgeries and allows for more effective implementation of CVS techniques.
Fluorescence cholangiography is an innovative method used as a teaching tool for young surgeons during difficult cholecystectomies that helps surgical residents in better learning and understanding of the biliary anatomy. 25 In a survey of trained surgeons using the Likert scale to evaluate the perceived benefits of fluorescent cholangiography, 26 all residents were shown to strongly agree with the device's usefulness in surgical training and to believe that it facilitated Calot's dissection. Similarly, in an investigation of the benefits of fluorescence cholangiography for enhancing surgical residents’ identification skills, fluorescence cholangiography was indicated to improve the identification skills of inexperienced surgeons during laparoscopic cholecystectomy compared with conventional training. 27 When combined with simulation-based video training, fluorescence cholangiography becomes a promising tool for enhancing the technical and decision-making skills of trainees and inexperienced surgeons.
The patient in the present case recovered rapidly without any perioperative complications. For patients with a stone incarcerated in the gallbladder neck, the combined technique provides better surgical guidance compared with intravenous fluorescence imaging alone, as it allows visualization of the cystic duct and common bile duct. Additionally, for patients with gangrenous cholecystitis and perforated gallbladder, this technique may offer a simple and safe solution, promoting rapid patient recovery.
Acknowledgements
The authors would like to thank the patient and his family for providing consent to use his data in this case report. We thank Liwen Bianji (Edanz; https://www.liwenbianji.cn) for editing the language of a draft of this manuscript.
Footnotes
Author contributions: Qingyun Xie, Manyu Yang, Kangyi Jiang, Ling Zhang, and Tianyang Mao were the patient’s attending physicians. Kangyi Jiang and Ling Zhang performed the percutaneous gallbladder drainage procedure. Qingyun Xie, Manyu Yang, and Fengwei Gao performed the laparoscopic cholecystectomy. Qingyun Xie, Manyu Yang, and Xin Zhao reviewed the literature and contributed to manuscript drafting. Fengwei Gao was responsible for manuscript revision. All authors provided final approval for the submitted version.
The authors declare that there is no conflict of interest.
Funding: This work was supported by grants from the Science and Technology Program of Sichuan Province (2023JDR0077).
ORCID iD: Fengwei Gao https://orcid.org/0009-0004-4963-5979
References
- 1.Yokoe M, Takada T, Hwang TL, et al. Descriptive review of acute cholecystitis: Japan-Taiwan collaborative epidemiological study. J Hepatobiliary Pancreat Sci 2017; 24: 319–328. [DOI] [PubMed] [Google Scholar]
- 2.Mori Y, Itoi T, Baron TH, et al. Tokyo Guidelines 2018: management strategies for gallbladder drainage in patients with acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci 2018; 25: 87–95. [DOI] [PubMed] [Google Scholar]
- 3.Baron TH, Grimm IS, Swanstrom LL. Interventional approaches to gallbladder disease. N Engl J Med 2015; 373: 357–365. [DOI] [PubMed] [Google Scholar]
- 4.Fletcher DR, Hobbs MS, Tan P, et al. Complications of cholecystectomy: risks of the laparoscopic approach and protective effects of operative cholangiography: a population-based study. Ann Surg 1999; 229: 449–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ishizawa T, Bandai Y, Kokudo N. Fluorescent cholangiography using indocyanine green for laparoscopic cholecystectomy: an initial experience. Arch Surg 2009; 144: 381–382. [DOI] [PubMed] [Google Scholar]
- 6.Dip F, LoMenzo E, Sarotto L, et al. Randomized trial of near-infrared incisionless fluorescent cholangiography. Ann Surg 2019; 270: 992–999. [DOI] [PubMed] [Google Scholar]
- 7.Gagnier JJ, Kienle G, Altman DG, et al. The CARE guidelines: consensus-based clinical case reporting guideline development. Glob Adv Health Med 2013; 2: 38–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schuster KM, O'Connor R, Cripps M, et al. Revision of the AAST grading scale for acute cholecystitis with comparison to physiologic measures of severity. J Trauma Acute Care Surg 2022; 92: 664–674. [DOI] [PubMed] [Google Scholar]
- 9.Way LW, Stewart L, Gantert W, et al. Causes and prevention of laparoscopic bile duct injuries: analysis of 252 cases from a human factors and cognitive psychology perspective. Ann Surg 2003; 237: 460–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg 1995; 180: 101–125. [PubMed] [Google Scholar]
- 11.Pesce A, Diana M. Critical view of safety during laparoscopic cholecystectomy: from the surgeon's eye to fluorescent vision. Surg Innov 2018; 25: 197–198. [DOI] [PubMed] [Google Scholar]
- 12.Strasberg SM, Brunt LM. Rationale and use of the critical view of safety in laparoscopic cholecystectomy. J Am Coll Surg 2010; 211: 132–138. [DOI] [PubMed] [Google Scholar]
- 13.Buddingh KT, Nieuwenhuijs VB, Van Buuren L, et al. Intraoperative assessment of biliary anatomy for prevention of bile duct injury: a review of current and future patient safety interventions. Surg Endosc 2011; 25: 2449–2461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dziodzio T, Weiss S, Sucher R, et al. A 'critical view' on a classical pitfall in laparoscopic cholecystectomy! Int J Surg Case Rep 2014; 5: 1218–1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nijssen MA, Schreinemakers JM, Meyer Z, et al. Complications after laparoscopic cholecystectomy: a video evaluation study of whether the critical view of safety was reached. World J Surg 2015; 39: 1798–1803. [DOI] [PubMed] [Google Scholar]
- 16.Pesce A, Piccolo G, La Greca G, et al. Utility of fluorescent cholangiography during laparoscopic cholecystectomy: a systematic review. World J Gastroenterol 2015; 21: 7877–7883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Agnus V, Pesce A, Boni L, et al. Fluorescence-based cholangiography: preliminary results from the IHU-IRCAD-EAES EURO-FIGS registry. Surg Endosc 2020; 34: 3888–3896. [DOI] [PubMed] [Google Scholar]
- 18.Liu YY, Liao CH, Diana M, et al. Near-infrared cholecystocholangiography with direct intragallbladder indocyanine green injection: preliminary clinical results. Surg Endosc 2018; 32: 1506–1514. [DOI] [PubMed] [Google Scholar]
- 19.Gené Škrabec C, Pardo Aranda F, Espin F, et al. Fluorescent cholangiography with direct injection of indocyanine green (ICG) into the gallbladder: a safety method to outline biliary anatomy. Langenbecks Arch Surg 2020; 405: 827–832. [DOI] [PubMed] [Google Scholar]
- 20.Han J, Xue D, Tuo H, et al. Percutaneous transhepatic gallbladder drainage combined with laparoscopic cholecystectomy versus emergency laparoscopic cholecystectomy for the treatment of moderate acute cholecystitis: a meta-analysis. J Laparoendosc Adv Surg Tech A 2022; 32: 733–739. [DOI] [PubMed] [Google Scholar]
- 21.Morfin E, Ponka JL, Brush BE. Gangrenous cholecystitis. Arch Surg 1968; 96: 567–573. [DOI] [PubMed] [Google Scholar]
- 22.Witte CL. Choledochal obstruction by cystic duct stone. Mirizzi's syndrome. Am Surg 1984; 50: 241–243. [PubMed] [Google Scholar]
- 23.Safa R, Berbari I, Hage S, et al. Atypical presentation of gangrenous cholecystitis: a case series. Am J Emerg Med 2018; 36: 2135.e1–2135.e5. [DOI] [PubMed] [Google Scholar]
- 24.Ankersmit M, Van Dam DA, Van Rijswijk AS, et al. Fluorescent imaging with indocyanine green during laparoscopic cholecystectomy in patients at increased risk of bile duct injury. Surg Innov 2017; 24: 245–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roy M, Dip F, Nguyen D, et al. Fluorescent incisionless cholangiography as a teaching tool for identification of Calot's triangle. Surg Endosc 2017; 31: 2483–2490. [DOI] [PubMed] [Google Scholar]
- 26.Pesce A, Latteri S, Barchitta M, et al. Near-infrared fluorescent cholangiography – real-time visualization of the biliary tree during elective laparoscopic cholecystectomy. HPB (Oxford) 2018; 20: 538–545. [DOI] [PubMed] [Google Scholar]
- 27.Rungsakulkij N, Thewmorakot S, Suragul W, et al. Fluorescence cholangiography enhances surgical residents' biliary delineation skill for laparoscopic cholecystectomies. World J Gastrointest Surg 2020; 12: 93–103. [DOI] [PMC free article] [PubMed] [Google Scholar]