Abstract
Preserving questionable maxillary teeth for aesthetics is challenging for many practitioners. This report presents the clinical and radiographic results of an orthodontic extrusion technique for clinical crown lengthening of female patients’ maxillary teeth to increase the restorability of teeth. Splinting was carried out by using specially designed hucks cast with custom-made post joined with orthodontic brackets with adjusting teeth. Teeth were carefully extruded to the desired level without harming the marginal bone areas or root apices. Clinical follow-up evaluations were performed for 3 months before construction of the final prosthesis. Intra-oral radiographs showed normal periodontal contour consistent with new bone formation in the periapical area of all cases, with no evidence of root or crestal bone resorption or endodontic problems. This technique is highly recommended in the aesthetic area of the maxillary arch.
Keywords: aesthetic, biologic width, crown lengthening, orthodontic extrusion, tooth restorability
Introduction
Tooth extrusion refers to the movement of teeth beyond the natural occlusal plane that occurs without accompanied movement of their supporting tissues.1 Surgical extrusion or intra-alveolar transplantation is necessary to restore unrestorable teeth through intentional coronal displacement of the remaining root within the socket.2 In situations where insufficient clinical crown and adequate crown ferrule are not achievable, root extrusion can be carried out orthodontically.3
Three options can be considered: crown lengthening, orthodontic extrusion, and surgical extrusion.4 Although, different techniques have been suggested for clinical crown lengthening in the maxillary area, some of them have limitations in terms of aesthetics and procedural requirements.5 Clinical crown lengthening is an effective method for overcoming adverse clinical conditions such as teeth with short or destructive clinical crown length. Three kinds of methods can be used in clinical crown lengthening, namely, surgical crown lengthening, orthodontic extrusion, and surgical extrusion.6 In general, clinicians should select the most appropriate technique for promising results.
A multidisciplinary approach involving endodontics, orthodontics, periodontics, and prosthodontics is necessary for cases with complex clinical conditions. Orthodontic extrusion followed by surgical crown lengthening of maxillary canine is considered the safest technique in the field to develop and maintain a sufficient crown–root ratio and achieve an excellent functionally aesthetic and clinical condition.7 Crown lengthening is an invasive technique that causes the removal of part of the bony support, although both orthodontic and surgical extrusion can avoid this inconvenience and can be used successfully in the treatment of severely damaged teeth.4
A group of studies were conducted and documented the success of orthodontic extrusion at long-period follow-up. Farmakis and Giuseppe et al concluded that at the 7–10-year follow-up, no signs of clinical or radiographic inflammation were recorded.8,9 Others said that this type of treatment is a conservative modality to restore fractured or extensively damaged teeth at a subgingival level, and it can preserve the natural tooth and maintain periodontal architecture.10 Also, orthodontic extrusion may represent a valid option for clinicians in different clinical situations as it results in improvement in the vertical amount of both hard and soft tissues.11
Recently, Graf et al investigated surgical crown lengthening through clinical observations. They noted low biological complication rates in the surrounding periodontal tissues and periapical regions over the follow-up period, and during provisional treatment and after the delivery of the final crown.12 In a narrative review by Cordaro et al, they concluded that both orthodontic and surgical extrusion can be used successfully in the treatment of severely compromised teeth, because they do not cause removal of a part of the bony support.4
This case series aimed to demonstrate how a simplified orthodontic extrusion technique was successfully performed for saving severely damaged maxillary teeth in the aesthetic zone for female patients. This work provides clinicians with guidelines about its application. Moreover, we evaluated patient satisfaction of the cemented prostheses by using a visual analogue scale at different follow-up intervals.
Case Series Reports
Three female patients with age between 38 and 56 years visited the Specialized Dental Center, Ministry of Health, Jazan, Saudi Arabia, between January and October 2022. Their chief complaint was the unsatisfactory color of crowned teeth in the maxillary arch, resulting in a short tooth due to previous root canal treatment RCT and caries. The protocol used in the treatment of these cases was adopted from Troiano et al and Qali et al, with some modifications.9,13
Case 1
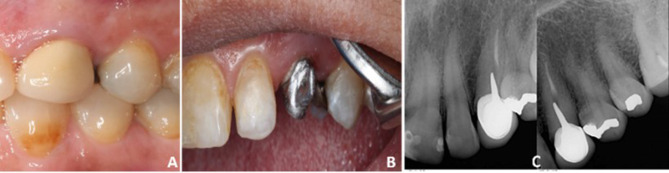
A 38-year-old female patient was referred to the abovementioned clinic. She complained about the color of the upper left canine. She underwent RCT and porcelain fused to metal (PFM) crown 8 years ago. Intraoral examination showed a discolored, loosened PFM crown of tooth # 23; after removal of the crown, a short and non-restorable tooth was observed (Figure 1A). After the PFM removal, a small amount of healthy hard tissues remained at the level of the gingiva, with absence of ferrule (Figure 1B). Radiographic evaluation revealed incomplete RCT with short post core for the same tooth (Figure 1C).
Figure 1.
Preoperative intraoral view (A), after removal of crown (B), and periapical X-rays (C) of tooth # 23.
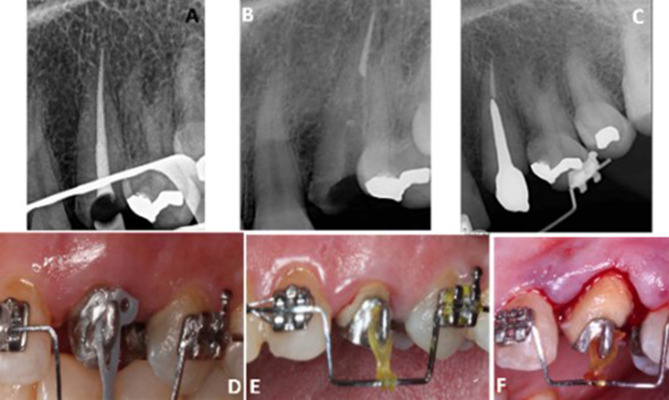
After data interpretation, the tooth was diagnosed for RCT retreatment with a new custom-made post, followed by orthodontic extrusion. The selected treatment plan began with nonsurgical RCT retreatment for tooth # 23, orthodontic extrusion, surgical crown lengthening, and provisional crown for 3 months. The patient agreed to this treatment. RCT was carried out (Figure 2A and B), followed by post and core fabrication and cementation with special design as hook on the buccal wall/side of the post for attachment and anchorage of the elastic for the extrusion of the remaining tooth structure and root (Figure 2C). The adjusting teeth were involved in the bonding of the orthodontic braces for use as anchorage for the extrusion. The extrusion period lasted for 8 weeks with weekly changing of the elastic band, and occlusal reduction was performed weekly. Three months of stabilization for the healing processes were completed (Figure 2D and E).
Figure 2.
Tooth # 23 during RCT and custom-made post constriction (A–C), orthodontic extrusion (D), and surgical crown lengthening (E and F).
A surgical crown lengthening procedure was performed to restore biologic width and restorability of the tooth (Figure 2F). Three months of stabilization were needed for the healing processes and to prevent the relapse after orthodontic extrusion. The prosthetic part was prepared by using a PFM crown after a provisional crown for 3 months, as seen clinically and radiographically in Figure 3A–D.
Figure 3.
During prosthetic treatment, retraction cord application (A), final impression (B), post-operative cemented crown (C), and periapical X-ray (D).
Case 2
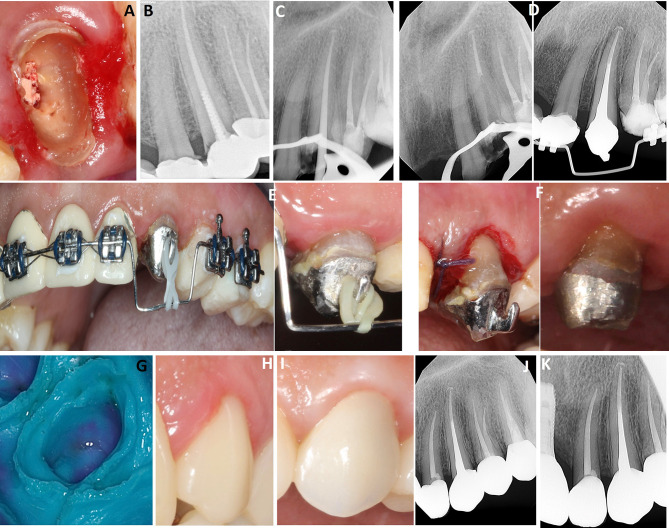
A 43-year-old female patient was referred to the abovementioned dental center. She complained of porcelain fracture and discoloration of the maxillary bridge. During clinical examination, the tooth was badly decayed with a fracture of the clinical crown up to the cervical line (Figure 4A). Radiographic examination revealed the presence of RCT failure for the same tooth (Figure 4B). After data interpretation, the tooth was diagnosed for RC retreatment and custom-made post with orthodontic extrusion to improve the restorability of the tooth. The selected treatment plan was nonsurgical retreatment for tooth #23, orthodontic extrusion, surgical crown lengthening, and provisional crown for 3 months. The patient agreed to this treatment. RC retreatment was performed (Figure 4C), followed by post and core fabrication and cementation with special design as hook on the buccal wall of the post for attachment and anchorage of the elastic for the extrusion of the remaining tooth structure and root (Figure 4D). The extrusion period lasted for 8 weeks, and the elastic was changed once a week. Three months of stabilization were needed for the healing processes (Figures 4E). A surgical crown lengthening procedure was performed to improve the level of tissues exposed and restore the biologic width (Figure 4F). The prosthetic phase was carried out using a zirconia core with facial cutback by e.max after 3 months of provisional crown cementation in the patient (Figure 4G–K).
Figure 4.
Preoperative intraoral view (A) and periapical view (B). During RCT, post space cementation (C and D), orthodontic extrusions (E), crown lengthening (F), prosthetic phase; final impression (G), provisional restoration (H), postoperative final prostheses (I), periapical X-ray (J), 6 months follow-up (K).
Case 3
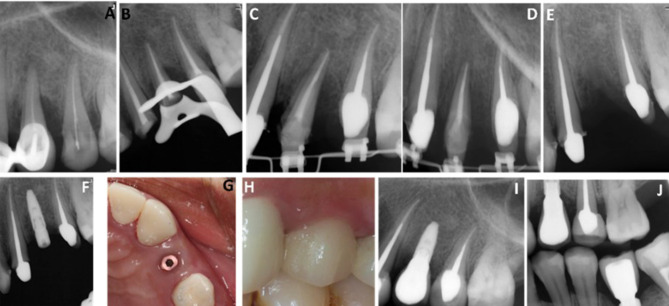
A 56-year-old female patient was referred to the previously mentioned dental center. She complained of discoloration of the PFM maxillary bridge. Clinical examination showed a bridge extending from tooth # 11 to tooth # 14 with mobility. Radiographic examination revealed severe vertical bone resorption, RCT failure, and poor crown–root ratio for tooth #24 (Figure 5A). After data interpretation, the tooth was diagnosed for extraction and restoration with a dental implant because of severe vertical bone resorption (7 mm at the distal side). Moreover, the dental implant could maintain the level of bone in relation to the adjacent tooth. Thus, the treatment option discussed with the patient was RCT retreatment and custom-made post with orthodontic extrusion to maintain the bone level before the implant. RC retreatment of tooth # 24 was followed by post and core fabrication and cementation with a special design as hook on the buccal wall of the post for attachment and anchorage of the elastic to facilitate the extrusion of the remaining bone and root (Figure 5B). The orthodontic extrusion period lasted for 5 months, and the elastic was changed once a week. Subsequently, 3 months of stabilization were needed for the healing processes (Figure 5C and D). Tooth #24 was replaced by a dental implant with a length of 10 mm and width of 5 mm via a conventional protocol (Figure 5E–G). The prosthetic part was made by using a PFM crown (Figure 5H), periapical X-ray (Figure 5I), and 6-months follow-up (Figure 5J).
Figure 5.
Preoperative view with vertical bone defect around tooth #24 (A), during RCT (B), orthodontic extrusion (C and D), extraction and implant of tooth #24 (E and F), postoperative view of dental implant (G), cemented crown (H), periapical X-ray (I), and 6 months postoperative (J).
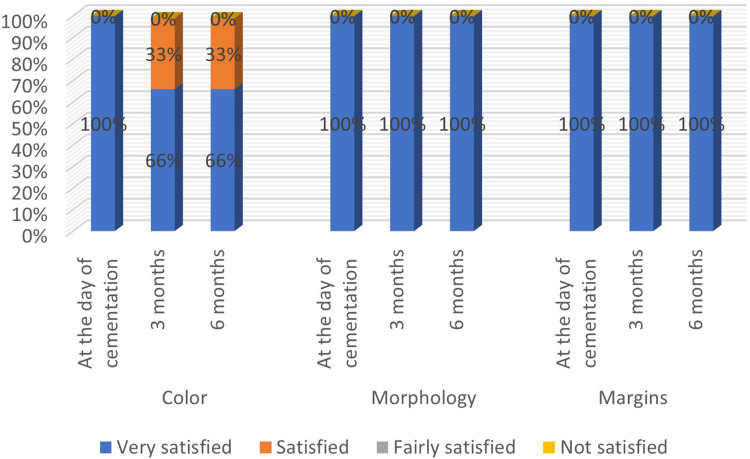
All cases were followed up after 1 week, 3 months, and 6 months (Figures 3D, 4K, and 5J). After the day of cementation of the final crowns and after 3 and 6 months, patient satisfaction for the color of the new crowns was assessed by using a visual analog scale. This scale can measure the color, morphology, and margins of restoration or cemented prosthesis.14 Almost all patients were satisfied with their color, morphology, and margins of cemented restorations, as shown in Figure 6.
Figure 6.
Percentage of patient satisfaction during follow-up intervals.
Discussion
The treatment of complicated crowns of maxillary canines and premolars is a clinical challenge. With the recent shift toward implants, conservative approaches to preserve the natural tooth are being overlooked. In clinical situations where the biological width is not compromised, surgical crown lengthening alone is sufficient to expose the subgingival margins. In cases where the fracture line extends subgingivally, and an adequate crown ferrule is not possible, orthodontic root extrusion can be carried out.3 This case series aimed to provide a concise demonstration of how a simplified orthodontic extrusion can be successfully performed to save severely damaged maxillary teeth in the aesthetic zone for female patients, as well as guidelines for its application. This work also evaluated patient satisfaction of the cemented prostheses via a visual analogue scale at different follow-up intervals.
The posts and core with hooks were designed during the casting of the post and core (at the wax-up stage). This simple design allowed the periodic changes of an elastic band that allowed to extrude the remaining roots. Also, it is a straightforward, non-costly design, does not interfere with mastication or aesthetic, and can be removed easily by smoothing the core at the end of the treatment. Throughout the appointments of the activation of root extrusion and elastic changes, the multidisciplinary team evaluated the presence of biological width and sufficient height of natural remaining roots to the site and location of the finish line.
After orthodontic extrusion, a stabilization period of 3–6 weeks is recommended to allow reorganization of the periodontal ligament.15 Long stabilization periods can help in reducing relapse tendencies. Thus, a long period of 2 months or more before fabrication of the permanent crown may be advised to ensure stability. In the present cases, the extruded teeth were stable and showed no bone relapse despite providing a stabilization period of 8–12 weeks. This result was in agreement with the findings of Parthiban et al, who reported the use of a bonded retainer to prevent further relapse, accompanied with monitoring at 1-year follow-up intervals.3 As recommended by Montevecchi et al in their clinical pilot study, 2 months is necessary to wait during provisional restoration for adequate woven bone form and histomorphometric bone analysis before construction of the final prostheses.16
In relation to case three (Figure 5J), orthodontic extrusion was carried out to maintain the crestal bone of this tooth and adjacent tooth. Orthodontic extrusion is being implemented as a treatment alternative to enhance hard and soft tissue prior to implant placement. Although the current literature does not provide clear guidelines, the decision-making process for a specific approach is based on the clinician’s preferences. Clinical studies are needed to verify the validity of this treatment option.17,18 Thus, orthodontic extrusion or forced eruption for prosthetic treatment and implant site development is a viable treatment option with successful long-term effects.
Orthodontic treatment via forced eruption for restorative purposes and crown lengthening surgery is a viable option for increasing the restorative restorability or improving aesthetic appearance. However, when planning a crown lengthening procedure, the whole periodontal condition of the patient and their hygiene habits should be evaluated. Moreover, an accurate diagnostic and interdisciplinary approach is mandatory for improved, conservative, and predictable results in aesthetic areas.13,19 This type of protocol is followed at the time or during surgery and follow-up periods of all cases presented in this article, and it includes strong emphasis on the use of proper oral hygiene aids and techniques.
Compared with other surgical procedures, slow or rapid orthodontic extrusion is a conservative approach that minimizes the need for reduction of adjacent teeth for conventional fixed bridge and prevents the bone needed for periodontal support.7,20 Surgical crown lengthening loosens the crestal bone of the adjacent tooth as well.20,21 Thus, in the third case, we started treatment by orthodontic extrusion and then extraction of the extruded teeth in which we maintained the level of the bone of the adjacent tooth. One of the indications of orthodontic extrusion is when surgical extractions are contraindicated to preserve the crestal bone level of the extraction site and adjacent tooth.7,20
The high percentages recorded from the survey about patient satisfaction with aesthetic treatment were consistent with the results by Mosallam et al, Bekhiet et al, and Abou-Steit et al; they documented excellent patient satisfaction in natural optical appearance for prostheses made by lithium disilicate glass ceramics (e.max CAD).22–24 However, PFM prostheses are preferred in most cases.
In the two cases presented in this paper, we used PFM crowns for the extruded teeth because of the presence of the custom-made post and core. PFM restorations represent the most widely used restorative technique in fixed prosthodontics, and their popularity may be due to their clinical longevity, accepted aesthetics, familiarity among most dental technicians, and cost.25,26 In the third case, a zirconia core with facial cut by lithium disilicate glass ceramic (e.Max) was considered because the patient is a consumer of different beverages. This CAD/CAM material shows color stability for such patients,27,28 and it is the most preferred material used by general practitioners in SA.29
The potential complications and drawbacks in such cases were minimized as no potential problems during treatment and follow-up arose, noticed, or recorded as a negative outcome. While the clinical significance in this case series is that orthodontic tooth eruption is a time-consuming treatment modality. However, its ease of application and cost–benefit effects make it acceptable to general practitioners and patients.
Conclusions
Although a number of techniques have been proposed for clinical crown lengthening procedures, all have some limitations in terms of function and aesthetics. This report presents the clinical and radiographic results of orthodontic extrusion for clinical crown lengthening to increase tooth restorability. A rigid splint was applied for 3 months before final prosthesis construction. Follow-up examinations performed at 3 and 6 months after surgery, teeth revealed normal functioned, probing depths around all teeth at all sites without bleeding, and no mobility. Radiographs showed normal bone contour with new bone formation in the periapical area, without any evidence of root or crestal bone resorption or endodontic problems. The presented technique proved to be an effective alternative surgical approach to crown lengthening because of its good functional and aesthetic outcome in the maxillary anterior region.
Acknowledgments
The authors would like to thank the patients who have agreed to take part in this report.
Consent Statements
Written informed consent was provided by the patients to have the case details and any accompanying images published. Also, an institutional approval was obtained from Jazan Health Ethics Committee, Ministry of Health, Jazan, Saudi Arabia under # 23118.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.GPT-9. The glossary of prosthodontic terms: the academy of prosthodontics foundation editorial staff glossary of prosthodontic terms committee of the academy of prosthodontics. J Prosthet Dent. 2017;117(5S):e1–e105. doi: 10.1016/j.prosdent.2016.12.001. [DOI] [PubMed] [Google Scholar]
- 2.Tegsjo U, Valerius-Olsson H, Frykholm A, Olgart K. Clinical evaluation of intra-alveolar transplantation of teeth with cervical root fractures. Swedish Dent J. 1987;11:235–250. [PubMed] [Google Scholar]
- 3.Parthiban G, Nagesh S, Karale R, Reddy S. Multidisciplinary approach to the management of a subgingivally fractured anterior tooth using an aligner based esthetic orthodontic extrusion appliance – a case report. Saudi Endod J. 2020;10(2):157–159. doi: 10.4103/sej.sej_3_19 [DOI] [Google Scholar]
- 4.Cordaro M, Staderini E, Torsello F, Grande NM, Turchi M, Cordaro M. Orthodontic extrusion vs. Surgical extrusion to rehabilitate severely damaged teeth: a literature review. Int J Environ Res Public Health. 2021;18:9530. doi: 10.3390/ijerph18189530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Argueta J, Orellana A, Plotino G. Surgical extrusion: a reliable technique for saving compromised teeth. A 5-years follow-up case report. Giornale Italiano di Endodonzia. 2018;32:25–30. doi: 10.1016/j.gien.2018.03.005 [DOI] [Google Scholar]
- 6.E-H J, K-H K, Huh Y-H, Cho L-R, Park C-H. Considerations in the selection of method for clinical crown lengthening. J Korean Acad Prosthodont. 2018;56:134–140. doi: 10.4047/jkap.2018.56.2.134 [DOI] [Google Scholar]
- 7.Jatol-Tekade S, Tekade SA, Pathak K, Patni V. Forceful orthodontic extrusion of maxillary canine in an adult patient: a case report. Dent J Adv Stud. 2018;6:37–39. doi: 10.1055/s-0038-1670730 [DOI] [Google Scholar]
- 8.Farmakis ETR. Orthodontic extrusion of an incisor with a complicated crown root fracture, utilising a custom-made intra-canal wire loop and endodontic treatment: a case report with 7-years follow-up. Eur Arch Paediatr Dent. 2018;19(5):379–385. doi: 10.1007/s40368-018-0373-5 [DOI] [PubMed] [Google Scholar]
- 9.Troiano G, Parente B, Laino L, et al. Use of orthodontic extrusion as aid for restoring extensively destroyed teeth: a case series. J Transl Sci. 2016;2(5):252–255. doi: 10.15761/JTS.1000148 [DOI] [Google Scholar]
- 10.Kermanshah H, Najafrad E, Valizadeh S. Forced eruption: alternative treatment approach to restore teeth with subgingival structure. Case Rep Dent. 2022;2022:9521915. doi: 10.1155/2022/9521915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kondapuram Seshu MR, Gash CL. Multidisciplinary management of a fractured premolar: a case report with followup. Case Rep Dent. 2012;2012:192912. doi: 10.1155/2012/192912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Graf T, Stimmelmayr M, Gutmann P, et al. Forced surgical extrusion using an axial tooth extraction system as a practicable technique for preserving severely destroyed teeth? - Clinical outcomes up to 4.8 years. J Esthet Restor Dent. 2023;1–10. doi: 10.1111/jerd.13059. [DOI] [PubMed] [Google Scholar]
- 13.Qali M, Chang YC, Teixeira H, Sabir M, Fiorellini J. Evaluation of long-term efficacy of forced erupted teeth for restorative purposes: a clinical retrospective study. Int J Periodontics Restorative Dent. 2022;42(6):809–815. doi: 10.11607/prd.5928. [DOI] [PubMed] [Google Scholar]
- 14.Chander NG. Visual analog scale in prosthodontics. J Indian Prosthodont Soc. 2019;19:99–100. doi: 10.4103/jips.jips_94_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Proffit WR, Fields HW, Sarver DM. Contemporary Orthodontics. 6th ed. Missouri: St Louis: Mosby; 2018. [Google Scholar]
- 16.Montevecchi M, Marucci G, Pignataro B, Piana G, Alessandri-Bonetti G, Checchi V. Bone modeling after orthodontic extrusion: a histomorphometric pilot study. J Clin Med. 2022;11:7329. doi: 10.3390/jcm11247329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alsahhaf A, Att W. Orthodontic extrusion for pre-implant site enhancement: principles and clinical guidelines. J Prosth Res. 2016;60:145–155. doi: 10.1016/j.jpor.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 18.Plotino G, Abella Sans F, Duggal MS, et al. Present status and future directions: surgical extrusion, intentional replantation and tooth autotransplantation. Inte Endo J. 2022;55(Suppl):827–842. doi: 10.1111/iej.13723 [DOI] [PubMed] [Google Scholar]
- 19.de Oliveira PS, Chiarelli F, Rodrigues JA, et al. Aesthetic Surgical Crown Lengthening Procedure. Case Rep Dentis. 2015:4. doi: 10.1155/2015/437412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bach N, Baylard JF, Voyer R. Orthodontic extrusion: periodontal considerations and applications. J Can Dent Assoc. 2004;70(11):775–780. [PubMed] [Google Scholar]
- 21.Belevcikli M, Altan H, Altan A. Surgical extrusion of anterior teeth with intrusion traumatic injury: a report of two cases. Eur Endod J. 2020;5(3):295–299. doi: 10.14744/eej.2020.07379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mosallam R, Taymour M, Katamish H, Kheirallah L. Clinical assessment of color stability and patient satisfaction for polished versus glazed lithium disilicate glass ceramic restorations: randomized controlled clinical trial. Inter J Health Sciences. 2022;6(S4):2819–2830. doi: 10.53730/ijhs.v6nS4.7842 [DOI] [Google Scholar]
- 23.Bekhiet M, Taymour M, Zamzam ML. CLINICAL EVALUATION AND PATIENT SATISFACTION OF SHADE MATCHING BETWEEN NATURAL TEETH AND MONOLITHIC ALL-CERAMIC CROWNS FABRICATED FROM TWO MATERIALS (RANDOMIZED CONTROLLED CLINICAL TRIAL). Egyp Dent J. 2021;67:2231–2240. doi: 10.21608/edj.2021.62512.1495 [DOI] [Google Scholar]
- 24.Abou-Steit S, Al-Guindy J, Zaki A. Evaluation of patient satisfaction and shade matching of vita suprinity versus lithium disilicate (E-max) ceramic crowns in esthetic zone (randomized controlled clinical trial). F1000Research. 2019;8:371. doi: 10.17605/OSF.IO/ZH6SC [DOI] [Google Scholar]
- 25.Al Moaleem MM, Shah FK, Khan NS, Porwal A. Porwal A. The effect of thermocycling on the bonding of different restorative materials to access opening through porcelain fused to metal restorations. J Adv Prosthodont. 2011;3(4):186–189. doi: 10.4047/jap.2011.3.4.186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Al Moaleem MM, Alkhayrat FM, Madkhali HA, et al. Subjective differences between dentists and patients about relative quality of metal ceramic restorations placed in the esthetic zone. J Contemp Dent Pract. 2017;18(2):112–116. doi: 10.5005/jp-journals-10024-2000 [DOI] [PubMed] [Google Scholar]
- 27.Abdalkadeer HK, Almarshedy SM, Al Ahmari NM, et al. Influence of the coca-cola drinks on the overall color of glazed or polished porcelain veneers fabricated from different materials and thicknesses: an in vitro study. J Contemp Dent Pract. 2020;21(1):56–61. doi: 10.5005/jp-journals-10024-2705 [DOI] [PubMed] [Google Scholar]
- 28.Alghazali N, Hakami AA, AlAjlan GA, et al. Influence of the Arabic-coffee on the overall color of glazed or polished porcelain veneers – in vitro study. Open Dent J. 2019;13:365. doi: 10.2174/1874210601913010364 [DOI] [Google Scholar]
- 29.Al Moaleem MM, Al Ahmari NM, Alqahtani SM, et al. Unlocking endocrown restoration expertise among dentists: insights from a multi-center cross-sectional study. Med Sci Monit. 2023;29:e940573. doi: 10.12659/MSM.940573. [DOI] [PMC free article] [PubMed] [Google Scholar]