Abstract
Millions of people’s health is at risk because of several factors and multiple overlapping crises, all of which hit the vulnerable the most. These challenges are dynamic and evolve in response to emerging health challenges and concerns, which need effective collaboration among countries working toward achieving Sustainable Development Goals (SDGs) and securing global health. Mental Health, the Impact of climate change, cardiovascular diseases (CVDs), diabetes, Infectious diseases, health system, and population aging are examples of challenges known to pose a vast burden worldwide. We are at a point known as the “digital revolution,” characterized by the expansion of artificial intelligence (AI) and a fusion of technology types. AI has emerged as a powerful tool for addressing various health challenges, and the last ten years have been influential due to the rapid expansion in the production and accessibility of health-related data. The computational models and algorithms can understand complicated health and medical data to perform various functions and deep-learning strategies. This narrative mini-review summarizes the most current AI applications to address the leading global health challenges. Harnessing its capabilities can ultimately mitigate the Impact of these challenges and revolutionize the field. It has the ability to strengthen global health through personalized health care and improved preparedness and response to future challenges. However, ethical and legal concerns about individual or community privacy and autonomy must be addressed for effective implementation.
Keywords: global health, artificial intelligence, public health, global health challenges, machine learning, health care, mortality
Introduction
Millions of people’s health and well-being are at risk of several factors and multiple overlapping crises, including but not limited to infectious disease outbreaks, rising malnutrition rates, and lack of sufficient medical access; all hit the vulnerable the most (1). As we are heading toward the end of 2023, a record 339 million people globally need urgent aid. Several critical issues need to be addressed urgently to improve health globally and build resilience against future threats (1); the recent COVID-19 has shown that each country’s security and prosperity depend on creating a healthier, safer, more resilient world.
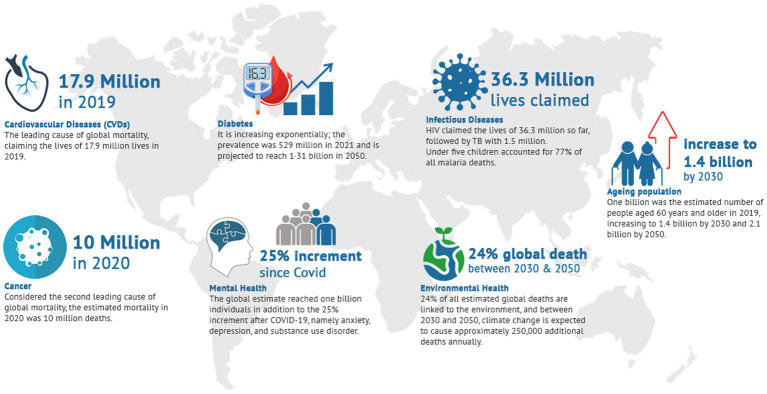
Global public health priorities play a crucial role in addressing the most pressing health challenges faced by populations worldwide. They are dynamic and evolve in response to emerging health challenges and crises, which need effective collaboration among countries to secure global health. Mental Health, the Impact of climate change, cardiovascular diseases (CVDs), diabetes, Infectious diseases, health system, and population aging are examples of challenges that are examples of these challenges that are known to pose a vast burden worldwide (Figure 1) (2, 3).
Figure 1.
Examples of global health challenges.
We are at a point known as the “digital revolution,” characterized by the expansion of artificial intelligence (AI) and a fusion of technology types; the rapid and transformative changes brought about by these advances in digital technology led to increased connectivity and accessibility of vast amounts of information (4). AI has emerged as a powerful tool for addressing various challenges, and the last ten years have been influential in the digital health (5, 6). AI and its subfields or techniques, such as deep learning (DL), natural language processing (NLP), and machine learning (ML), have prospects to benefit healthcare, including public health, because of the rapid expansion in the production and accessibility of health-related data (7–9). The computational models and algorithms can understand complicated health and medical care data to perform various functions and deep-learning strategies. AI in health care improves disease surveillance, diagnosis, treatment selection, and clinical laboratory testing (10, 11). Harnessing its capabilities can ultimately mitigate the impact of global public health issues and revolutionize the field.
However, the burgeoning interest was accompanied by caution over using it, especially in health-related fields. Crucial ethics, privacy, and bias issues were raised to ensure AI’s responsible and equitable integration in the global public health landscape. Additionally, the human inability to see how ML systems make their decisions “black box,” brought uncertainty and threatened trust among the users regarding its application (12). This review aims to explore the current state of AI in those mentioned global public health challenges and provide insights about its current application in disease diagnosis, medicinal product development, and medical intervention. This step will provide more comprehension, and interpretability for most of AI’s leading evidence-based applications and contribute to a better understanding of AI in dealing with the increasing scale and complexity of challenges to global health.
AI in non-communicable diseases
The global development over the last years was also associated with the change in disease burden, and NCDs have almost become the leading cause of mortality, resulting in 200 million premature deaths and expectation of another 150 million people deaths during the next ten years; most of them in low and middle-income countries (13).
NCDs are usually multifactorial diseases, and several factors are associated with their development, including genetic and environmental factors, which make them challenging to prevent and treat effectively. They are exacerbated by four key modifiable risk factors, namely tobacco use, harmful use of alcohol, physical inactivity, and unhealthy diets (14). It was estimated that behavioral factors and genetic factors are the main contributors to preterm death in the USA with (40%), and (30%) respectively (15), and the role of public health awareness and intervention have a vast impact (16). AI can offer the potential to analyze large and complex datasets obtained from lifestyle, clinical, and biological data in a way that exceeds the human ability to make sense of it. ML, NLP, Robotic, virtual agents (chatbots), and speech analysis are just a few examples of the available AI applications that are used to improve public health (17). For example, Florence, which is the WHO’s first virtual health worker, is designed to help the world’s 1.3 billion tobacco users quit smoking (18); STop obesity Platform that can offer personalized support to people with obesity (19), and chatbots to personalized fitness strategies.
If we discuss kidney disease progression as a case illustration, AI has its application in pre/post-diagnosis, which can ultimately lead to improved outcomes in a timely and accurate manner (20). During the analysis phase of patient data, AI can identify the early signs of the diseases from the lab results, medical history, and images (21, 22), it can also help in the diagnosis of kidney disease from a kidney biopsy through deep learning-based approaches (23), and to improve outcome and early detection of other comorbidity in renal patients (24). The flowing part discusses AI’s applications in the major of NCDs.
AI in cardiovascular diseases
Cardiovascular diseases (CVDs) are the leading cause of global mortality, taking an estimated 17.9 million lives in 2019. Strategies to tackle this considerable burden are directed toward reducing risk factors, enhancing the health system, and monitoring disease patterns and trends to inform national and global actions. The application of AI can identify, process, integrate, and analyze massive amounts of data, including but not limited to medical records, ultrasounds, medications, and experimental results. The gold standard in diagnosing most CVDs is an echocardiogram (ECG) and cardiac magnetic resonance (CMR). However, the clinician’s interpretation of ECG depends on their experience. Hence, ECG information might be missed due to clinicians’ difficulty analyzing them (25, 26).
Additionally, most ECGs are done on symptomatic patients, even though many CVDs, such as valvular heart diseases, involve long asymptomatic periods (27). However, the AI algorithm interpretation of ECG can diagnose heart failure, atrial fibrillation, hypertrophic cardiomyopathy, pulmonary hypertension, aortic valve stenosis, and anemia (28–36). An approach that reduced time and the physician’s cognitive burden by offering pre-diagnosis, correcting clinician errors and preventing the occurrence of misdiagnosis. Moreover, AI enhances the prompt efficiency of medical tools such as computed tomography (CT), echocardiography, magnetic resonance imaging (MRI), and Coronary computed tomography angiography (CCTA) (37–39). In addition to its application in CVD prediction and predictive modeling, such as mortality prediction, vascular aging, and predicting major adverse cardiovascular events in asymptomatic subjects (40–43).
AI in cancer
Cancer is a large group of diseases and is considered the second leading cause of global mortality; the estimated mortality in 2020 was 10 million deaths. Despite the several accomplishments that have been made in the field of cancer diagnosis, prognosis, and treatment, individualized and data-driven care remains challenging. The challenge lies in the specific characteristics of distinct molecular, genetic, and tumor-based features (44). However, using machine learning and AI positively supports cancer prevention and management, as it is reshaping the existing picture, and is developing rapidly (45–47). AI has become pivotal as it can provide patients with forecasting and prediction and improved risk stratification according to specific criteria, such as in the cases of some breast, colon, ovarian, lung, and skin cancers (48–54). Further, it can detect hidden patterns from several sources such as molecular profiling, pathology, and medical imaging, and integration of-omics data to provide a more comprehensive understanding of cancer and improve the precision oncology (55). During a surgical procedure, AI can provide real-time detection and diagnosis of some cancers; through its ability to differentiate between cancerous and normal tissues (56, 57). Recently, mounting evidence indicated the potential role of microRNAs (miRNA) in cancer diagnosis and prognosis. MiRNAs, a small, single-stranded, non-coding ribonucleic acids (RNAs), are essential for all biological functions including cancer development. ML provides an opportunity to explore miRNA’s ability to serve as a reliable biomarker targeting drugs and improve cancer clinical classification (58, 59).
A recent achievement is the genetics-based classification and treatment response of Cancer of unknown primary (CUP); this type of cancer usually leads to poor outcomes because primary cancer is unknown (60). The study used ML to classify the cancer based on its genetic profile. This model identifies the likely prior site and predicts the best treatment option (60). Another example is pancreatic cancer, one of the most challenging cancers to diagnose as it is often asymptomatic until it metastasises, causing poor and ineffective treatment. AI modeling enables the detection of individuals at high risk of developing pancreatic cancer; the detection was up to 3 years earlier than currently by using medical records (61).
AI in diabetes
A global crisis that is increasing exponentially and is considered a significant cause of blindness, kidney failure, heart attacks, stroke, and lower limb amputation. It was estimated that the prevalence was 529 million in 2021 and is projected to reach 1·31 billion in 2050 (62), a burden that has a global agreement to halt before. According to several recommendations, the starting point is prevention by screening, especially for obese or overweight adults (63, 64). However, a significant number of cases were missed with these approaches. The current clinical application of AI in diabetes diagnosis and management is categorized into four domains: (1) automatic retinal screening, (2) clinical diagnosis support, (3) patient self-management tools, and (4) risk stratification (65). AI for automatic retinal screening enables early diagnosis with high specificity and sensitivity (66). Several studies have evaluated the prediction of new-onset diabetes mellitus by AI and ML models, and it was recommended to include data as an omics database (e.g., genomics) (67). Recently, a new model based on AI was developed to detect diabetes warning signs, even in patients who did not meet the guidelines for diabetes elevated risk. This model can enhance type 2 diabetes (T2D) detection; it uses the patient’s X-ray image collected during routine medical care and their medical records to detect T2D (68).
In diabetes management, AI devices can help patients monitor their glucose levels in real-time and predict spikes or drops in healthcare. AI-based medical devices, such as the Guardian Connect System by Medtronic and the DreaMed Diabetes system (DreaMed Diabetes Ltd), have been approved to help control diabetes (69, 70). Another mobile application (GoCARB) is used to estimate the carbohydrate content in meals, which can help enhance the patients’ skills in managing diabetic disease through diet management (71, 72). The future application of AI will introduce a paradigm shift in Diabetes care from conventional management to more personalized and data-driven precision care.
AI in population aging
As a result of significant increases in life expectancy, the global population of people aged 60 years and older is increasing (73). One billion was the estimated number in 2019, rising to 1.4 billion by 2030, accounting for 16.7% of the global population, and projected to reach 2.1 billion by 2050; around 80% will live in low and middle-income countries (74, 75). The increase in age is associated with common health conditions, leading to several complex health states due to multiple underlying factors, such as disability. However, there is no linearity or consistency in developing these changes, and individual characteristics have a vast impact. They will continuously demand primary and long-term care, a more trained workforce, and physical and social environments for social support. Around 92% of global older adults have at least one chronic disease, and more than 81% of those aged ≥85 years suffer from two chronic diseases or more (76–78). Additionally, disability and its consequences also have a huge burden on the aging population. Globally, 1.3 billion people (16% of the world’s population) suffer from a physical or cognitive disability; although these estimates cover all age groups, starting from 18 years old (79). However, AI can provide intelligent solutions for longer lives, satisfy the growing unmet healthcare needs, and overcome the limited number of insufficient healthcare resources. Currently, AI technologies for aging population are used in the robotic intervention (80, 81), applications on smartphones or computers (82, 83), social interaction and support, such as improved mental well-being and quality of life (84–86); rehabilitation therapy, such as its application in the recovery of upper and lower extremity functions, gait robotic rehabilitation, or improve sleep quality and daily living activities (87–90), and wearables, voice-activated (91–94). It can create more advanced algorithms to provide more precise holistic interventions tailored to address the elders’ multiple needs in a safer and more friendly manner (78, 95, 96). Ambient-assisted working and ambient-assisted living are examples of smart systems that can adapt themselves to older adult needs by exploiting ambient intelligence solutions. These systems focus on using technology to support and enhance the quality of life of the older adult population, either in work, or indoor and outdoor environments (97, 98). Recently, a group of researchers have helped develop drugs that might potentially delay the effects of aging by eliminating senescent cells (96, 99).
AI in mental health
The global estimate of mental health disorders is one billion individuals (100). Since the beginning of the COVID-19 pandemic, the rates of anxiety, depression, and substance use disorder have increased (101, 102). This situation is worse in low-and middle-income countries, where the estimated number of people with limited access and no treatment is around 75% of people with mental, neurological and substance use disorders (100, 102).
Despite the significant advantages of using AI in healthcare, mental health has been slower to adopt AI since the primary factor contributing to successful psychiatric diagnosis and treatment is the interaction with the patients’ (103–105). However, AI applications have great potential in diagnosing different kinds of mental illness. This is a great advantage given the available heterogeneity in the pathophysiology of mental illness. AI can access and analyze relevant information about a patient’s unique bio-psycho-social characteristics and identify pertinent data patterns that might help provide more objective, improved definitions of these illnesses (106). Further, AI can be used in biomarkers identification, develop better diagnoses and formulate risk models to predict individual risk (105, 107). Moreover, it can be used for some cases, such as depression or autism, where face-to-face interaction might be challenging. In autism, for example, AI could be a more useful tool than a psychotherapy session with a human doctor; it can provide tailored, personalized interventions or bridge the communication gap they may experience (105). Nevertheless, the variation of AI applications is persistent in dealing with sensitive issues like mental health.
AI in infectious diseases
As the world becomes increasingly globalized, health and illnesses have no borders. Concerns about One Health have gained prominence recently, which is justified as the world emerges from the most significant global emergency and the increasing number of infectious pathogens that spread from humans, animals, or the environment. COVID-19 has highlighted the high spreading rate with which infections can devastate the world’s health and economy. Results in more investment and investigation into the occurrence, prevalence, prevention, control, and treatment of infectious diseases to strengthen the epidemic response and mobilize quickly for public health priority.
Globally, the leading communicable diseases associated with high mortalities are HIV/AIDS, tuberculosis (TB), malaria, viral hepatitis, sexually transmitted infections, and neglected tropical diseases (NTDs). HIV continues to be a major global issue, claiming the lives of 36.3 million so far, and TB-associated mortalities reached 1.5 million annually, making it the world’s second top infectious killer after COVID-19 (108). Tackling AI applications in HIV will yield several examples in HIV prevention, testing, and treatment to achieve sustained viral suppression (109–111). It was used also for rapid detection and response through monitoring clusters of vulnerable groups to reduce HIV transmission (111). Another example is Syphilis, which is a sexually transmitted disease (STD). To eliminate congenital syphilis (CS), the WHO launched an initiative in Latin America and the Caribbean (112). However, as the syphilis epidemic increased in Brazil, the government of Brazil developed a national project, the “Syphilis No!” Project (SNP), for implementing and integrating a syphilis response into healthcare networks, (113, 114). This project encompasses four dimensions: (a) management and governance, (b) surveillance, (c) comprehensive care, and (d) strengthening of the educommunication (113, 115). The application of AI such as data mining and NLP in these strategies augments the country’s capabilities in combating syphilis (113).
It is essential to analyze global infectious disease cases regularly. However, some countries’ investment in contagious disease identification was typically based on the identification of presenting symptoms and the likelihood of exposure due to the high cost and feasibility of the primary approach of detection (116, 117). However, using big data, AI and ML algorithms can contribute to global infection control and help with the spatial and temporal prediction of the evolution and spread of infectious diseases (118). Their advanced capabilities can analyze several factors: population demographics, environmental conditions, and individual behaviors, all of which can be used simultaneously (119). Such as case prediction according to historical data (120), predicting the likelihood of an individual contracting an infectious disease according to personal and behavioral characteristics, using pathogen genetic makeup to identify the most likely sources of an outbreak, identifying or anticipating an epidemic by analyzing massive data; it can be used for early warning systems, hot spot detection, forecasting, and improving the recourses allocation at a country and a global level (68–72). After the exposure or presence of a potential outbreak, AI can advance in diagnostic approaches and differentiate various pathogens by using the pathogen genetic makeup, such as its ability to distinguish between COVID-19 and other circulating respiratory viruses with COVID-like symptoms (121, 122).
Another example is the possible application to the rising incidence of antimicrobial resistance (AMR), which has become a significant challenge. For this purpose, a group of researchers were able to develop a mobile application to classify bacterial susceptibility to various antibiotics, especially in resource-limited settings (123). Further, reducing transmission is essential to control global widespread infections such as those that occur in pandemics. The application of AI for screening technologies targeting infections and integrating them into data visualization has been introduced broadly, especially during the COVID-19 pandemic (117). This improved the surveillance and generated meaningful insights from multidimensional data, which can be widely used for public health practice.
In addition to surveillance, early detection, and diagnosis, AI is used to develop anti-infective therapies, although it became challenging with the spread of drug resistance (124). ML models can help explore the pathway of pathogen’s interaction with host cells and immune responses, facilitating antigen determination, vaccine design, and treatment strategies (124–127). Finally, the WHO global report on infection prevention and control estimated that implementing infection prevention and control (IPC) can reduce healthcare-associated infections (HAIs) by 70% (128). Using AI can improve current and past processes to speed infection prevention and control response, such as identifying the correlations associated with medically relevant conditions, identifying potential risk factors, and surveillance of emerging infectious diseases (129–131), improving hand hygiene compliance (132), and in-hospital analysis of transmission, and outbreak events identification and investigation (133).
AI in environmental health
The impact of environmental health on human lives and health are interconnected in various ways. The Global Health Observatory estimated that 24% of all estimated global deaths are linked to the environment. Between 2030 and 2050, climate change is expected to cause approximately 250,000 additional deaths per year, mainly from undernutrition, malaria, diarrhea and heat stress (134). Because of the adynamic of the environment, AI applications in this field are immense; its deployment will provide a better capacity to deal with the growing climate exigency and related challenges. In exposure assessment, AI can use satellite observations, meteorological variables, land use, and traffic data to predict the spatiotemporal patterns and concentrations of pollutants (135–138). AI were used in monitoring, such as its application during COVID-19, for airport security checks and patient tracking (139), or to improve the prediction of harmful algal blooms (140).
Additionally, it can predict diseases based on environmental factors, such as its application to predict the spread of Zika virus and Dengue fever (141, 142). In waste management, AI reduces fuel consumption and emissions, increases recycling rates, and reduces landfill waste (143). GeoAI is one of the emerging AI tools that can handle complex spatial and temporal data to adjust algorithms and workflows according to the specific characteristics of spatial processes (136, 144). It can develop various environmental exposure models across different geographical regions in prospective and retrospective approaches (136). In 2022, the United Nations launched The World Environment Situation Room, a new digital platform that can provide real-time analysis, track air quality, measure environmental footprint, and monitor (145).
AI in health systems
Through good stewardship, resource development, funding and services, health systems support initiatives to prevent, promote, and provide for more health and well-being (146). They are complex and are in a constant state of flux; according to the World Health Organization (WHO), “A well-functioning health system working in harmony is built on having trained and motivated health workers, a well-maintained infrastructure, and a reliable supply of medicines and technologies backed by adequate funding, strong health plans and evidence-based policies” (147). At the global level, it should be able to control and address global health challenges and severe events (147). However, several myriads of difficulties impede their ability to provide these services. This includes but is not limited to the sudden onset or the slowly growing crises, such as the COVID-19 pandemic, the natural disasters the world is encountering, or the slow time impact of climate change (148–150), the rising number of older people, and the associated complex chronic medical illness. To overcome these difficulties and achieve effective and lasting change, four factors were proposed: (a) the acorn-to-oak tree principle (small initiative), (b) the data-to-information-to-intelligence principle (information technology (IT) and data), (c) the many-hands principle (stakeholders); and (d) the patients-the-preeminent-player principle (individuals) (151). These factors were established across 60 health systems; the role of data and technology cannot be missed (5, 151). AI applications are steadily entering novel domains previously governed solely by human experts. They can improve health financing, make public health more effective, and reach underserved populations by making health care more efficient and effective through more personal health services (152).
Further, the Primary health care system (PHC) is vital to addressing health issues effectively; they are considered the front door of the health care system. Using AI will enhance the holistic approach of PHC in outcome prediction, data mining, and personalized treatment (153–155). The current tools in PHC have several applications, including the risk prediction (156–158), workforce assessment (159), record data extraction (160, 161), control of healthcare-associated infections (162), and performing medical tasks remotely that contribute to public health domain (154, 163, 164).
Conclusion
AI integration and application to global health challenges have immense potential to overcome them efficiently and effectively. Disease prevention, detection, and response can quickly mobilize and yield medicinal products. As mentioned earlier, around 40% of preterm death was associated with behavioral factors. With AI advancement, data analysis and segmentation can be done for several characteristics such as behavior, opinion, and attitude. Using these data, the ML can analyze the online health information and provide personalized massaging to influence individuals’ health behaviors with high quality and clarity, amplifying their influence and effectiveness (165–167). This health communication can also inform AI technology in developing effective communication systems with patients and their healthcare providers. The health communication theories and models can highlight the available barriers to behavioral change and the available limitations of technology-driven health interventions. Which can help improve the efficacy of AI-supported systems or intervention designs (167–169).
AI in health care is expected to grow from nearly US $15 billion to $103 billion between 2023 and 2028 (170). However, incongruent with AI’s benefits, exacerbation of inequities was accompanied, and ethical and legal concerns about individual or community privacy and autonomy were raised (118, 171). The EU AI Act is nearing implementation, and it will be the first comprehensive regulation that addresses the risks of artificial intelligence; European Parliament proposed it to ensure better conditions for developing and using this innovative technology (172). Further, to avoid the risk of hindering AI applications in healthcare due to lack of sufficient transparency “black box,” researchers were urged to provide more research and explanation for AI; explainable AI (xAI), as an approach to more understandable and human-interpretable AI-based applications (173, 174).
However, AI stands as a cornerstone of the upcoming digital revolution. Despite the moral dilemmas in AI application in health care, it is likely to meager, co-exist or replace current systems and assets as a potent amplifier of human potential. It has the ability to strengthen global health through personalized health care and improved preparedness and response to future challenges.
Author contributions
AZ: Conceptualization, Writing – original draft.
Funding Statement
The author declares that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.World Health Organization . WHO's health emergency appeal 2023. Geneva: World Health Organization; (2023a). [Google Scholar]
- 2.Chan A. Eleven global health issues to watch in 2023, according to IHME experts: the Institute for Health Metrics and Evaluation. (2022). Available at: https://www.healthdata.org/news-events/insights-blog/acting-data/11-global-health-issues-watch-2023-according-ihme-experts.
- 3.Lucero-Prisno DE, Shomuyiwa DO, Kouwenhoven MBN, Dorji T, Odey GO, Miranda AV, et al. Top 10 public health challenges to track in 2023: shifting focus beyond a global pandemic. Public Health Challenges. (2023) 2:e86. doi: 10.1002/puh2.86 [DOI] [Google Scholar]
- 4.Schwab K. The fourth industrial revolution: what it means, how to respond New York. (2016). Available at: https://www.weforum.org/agenda/2016/01/the-fourth-industrial-revolution-what-it-means-and-how-to-respond/.
- 5.World Bank . Digital-in-health: Unlocking the value for everyone. Washington DC: World Bank; (2023). [Google Scholar]
- 6.U.S. Agency for International Development . Artificial intelligence in Global Health: Defining a collective path forward. Washington: U.S. Agency for International Development; (2019). [Google Scholar]
- 7.Suleimenov IE, Vitulyova YS, Bakirov AS, Gabrielyan OA. Artificial intelligence: What is it? Proceedings of the 2020 6th International Conference on Computer and Technology Applications Antalya, Turkey: Association for Computing Machinery (2020). [Google Scholar]
- 8.Davenport T, Kalakota R. The potential for artificial intelligence in healthcare. Future Healthcare J. (2019) 6:94–8. doi: 10.7861/futurehosp.6-2-94, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kubat M. A simple machine-learning task. An introduction to machine learning. Cham: Springer International Publishing; (2017). [Google Scholar]
- 10.Alowais SA, Alghamdi SS, Alsuhebany N, Alqahtani T, Alshaya AI, Almohareb SN, et al. Revolutionizing healthcare: the role of artificial intelligence in clinical practice. BMC Med Educ. (2023) 23:689. doi: 10.1186/s12909-023-04698-z, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rubens M, Ramamoorthy V, Saxena A, Shehadeh N. Public health in the twenty-first century: the role of advanced technologies. Front Media. (2014) 2:224. doi: 10.3389/fpubh.2014.00224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Steerling E, Siira E, Nilsen P, Svedberg P, Nygren J. Implementing AI in healthcare—the relevance of trust: a scoping review. Front Health Serv. (2023) 3:150. doi: 10.3389/frhs.2023.1211150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization . Noncommunicable diseases. Geneva: World Health Organization; (2014). [Google Scholar]
- 14.World Health Organization . Noncommunicable diseases: Key facts. Geneva: World Health Organization; (2023b). [Google Scholar]
- 15.Schroeder SA. We can do better — improving the health of the American people. N Engl J Med. (2007) 357:1221–8. doi: 10.1056/NEJMsa073350, PMID: [DOI] [PubMed] [Google Scholar]
- 16.Frieden TR. The future of public health. N Engl J Med. (2015) 373:1748–54. doi: 10.1056/NEJMsa1511248 [DOI] [PubMed] [Google Scholar]
- 17.Pan American Health Organization . Artificial intelligence in public health. Washington: Pan American Health Organization; (2021). [Google Scholar]
- 18.World Health Organization . Using AI to lead a healthier lifestyle: How Florence can help you. Geneva: World Health Organization; (2022a). [Google Scholar]
- 19.European Commission . STop obesity platform. (2019). Available at: https://cordis.europa.eu/project/id/823978.
- 20.Bellocchio F, Zhang H. Editorial: artificial intelligence in nephrology. Front. Nephrol. (2023) 3:769. doi: 10.3389/fneph.2023.1270769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fayos De Arizón L, Viera ER, Pilco M, Perera A, De Maeztu G, Nicolau A, et al. Artificial intelligence: a new field of knowledge for nephrologists? Clin Kidney J. (2023). doi: 10.1093/ckj/sfad182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nong Y, Wei X, Qiu H, Yang H, Yang J, Lu J, et al. Analysis of risk factors for severe acute kidney injury in patients with acute myocardial infarction: a retrospective study. Front Nephrology. (2023) 3:249. doi: 10.3389/fneph.2023.1047249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Basso MN, Barua M, Meyer J, John R, Khademi A. Machine learning in renal pathology. Front Nephrology. (2022) 2:7002. doi: 10.3389/fneph.2022.1007002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Canaud B, Kooman J, Davenport A, Campo D, Carreel E, Morena-Carrere M, et al. Digital health technology to support care and improve outcomes of chronic kidney disease patients: as a case illustration, the Withings toolkit health sensing tools. Front Nephrol. (2023) 3:565. doi: 10.3389/fneph.2023.1148565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Elias P, Poterucha TJ, Rajaram V, Moller LM, Rodriguez V, Bhave S, et al. Deep learning electrocardiographic analysis for detection of left-sided Valvular heart disease. J Am Coll Cardiol. (2022) 80:613–26. doi: 10.1016/j.jacc.2022.05.029, PMID: [DOI] [PubMed] [Google Scholar]
- 26.Siontis KC, Noseworthy PA, Attia ZI, Friedman PA. Artificial intelligence-enhanced electrocardiography in cardiovascular disease management. Nat Rev Cardiol. (2021) 18:465–78. doi: 10.1038/s41569-020-00503-2, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lancellotti P, Magne J, Dulgheru R, Clavel MA, Donal E, Vannan MA, et al. Outcomes of patients with asymptomatic aortic stenosis followed up in heart valve clinics. JAMA Cardiol. (2018) 3:1060–8. doi: 10.1001/jamacardio.2018.3152, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Attia ZI, Kapa S, Lopez-Jimenez F, McKie PM, Ladewig DJ, Satam G, et al. Screening for cardiac contractile dysfunction using an artificial intelligence-enabled electrocardiogram. Nat Med. (2019) 25:70–4. doi: 10.1038/s41591-018-0240-2, PMID: [DOI] [PubMed] [Google Scholar]
- 29.Attia ZI, Kapa S, Noseworthy PA, Lopez-Jimenez F, Friedman PA. Artificial intelligence ECG to detect left ventricular dysfunction in COVID-19: a case series. Mayo Clin Proc. (2020) 95:2464–6. doi: 10.1016/j.mayocp.2020.09.020, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Attia ZI, Noseworthy PA, Lopez-Jimenez F, Asirvatham SJ, Deshmukh AJ, Gersh BJ, et al. An artificial intelligence-enabled ECG algorithm for the identification of patients with atrial fibrillation during sinus rhythm: a retrospective analysis of outcome prediction. Lancet. (2019) 394:861–7. doi: 10.1016/S0140-6736(19)31721-0, PMID: [DOI] [PubMed] [Google Scholar]
- 31.Yao X, Rushlow DR, Inselman JW, McCoy RG, Thacher TD, Behnken EM, et al. Artificial intelligence-enabled electrocardiograms for identification of patients with low ejection fraction: a pragmatic, randomized clinical trial. Nat Med. (2021) 27:815–9. doi: 10.1038/s41591-021-01335-4, PMID: [DOI] [PubMed] [Google Scholar]
- 32.Kwon JM, Cho Y, Jeon KH, Cho S, Kim KH, Baek SD, et al. A deep learning algorithm to detect anaemia with ECGs: a retrospective, multicentre study. Lancet Digit Health. (2020) 2:e358–67. doi: 10.1016/S2589-7500(20)30108-4, PMID: [DOI] [PubMed] [Google Scholar]
- 33.Kwon JM, Kim KH, Medina-Inojosa J, Jeon KH, Park J, Oh BH. Artificial intelligence for early prediction of pulmonary hypertension using electrocardiography. J Heart Lung Transplant. (2020) 39:805–14. doi: 10.1016/j.healun.2020.04.009, PMID: [DOI] [PubMed] [Google Scholar]
- 34.Ko WY, Siontis KC, Attia ZI, Carter RE, Kapa S, Ommen SR, et al. Detection of hypertrophic cardiomyopathy using a convolutional neural network-enabled electrocardiogram. J Am Coll Cardiol. (2020) 75:722–33. doi: 10.1016/j.jacc.2019.12.030 [DOI] [PubMed] [Google Scholar]
- 35.Kwon JM, Lee SY, Jeon KH, Lee Y, Kim KH, Park J, et al. Deep learning-based algorithm for detecting aortic stenosis using electrocardiography. J Am Heart Assoc. (2020) 9:e014717. doi: 10.1161/JAHA.119.014717, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cohen-Shelly M, Attia ZI, Friedman PA, Ito S, Essayagh BA, Ko WY, et al. Electrocardiogram screening for aortic valve stenosis using artificial intelligence. Eur Heart J. (2021) 42:2885–96. doi: 10.1093/eurheartj/ehab153 [DOI] [PubMed] [Google Scholar]
- 37.Choi AD, Marques H, Kumar V, Griffin WF, Rahban H, Karlsberg RP, et al. CT evaluation by artificial intelligence for atherosclerosis, stenosis and vascular morphology (CLARIFY): a multi-center, international study. J Cardiovasc Comput Tomogr. (2021) 15:470–6. doi: 10.1016/j.jcct.2021.05.004, PMID: [DOI] [PubMed] [Google Scholar]
- 38.Lin A, Manral N, McElhinney P, Killekar A, Matsumoto H, Kwiecinski J, et al. Deep learning-enabled coronary CT angiography for plaque and stenosis quantification and cardiac risk prediction: an international multicentre study. Lancet Digit Health. (2022) 4:e256–65. doi: 10.1016/S2589-7500(22)00022-X, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Knott KD, Seraphim A, Augusto JB, Xue H, Chacko L, Aung N, et al. The prognostic significance of quantitative myocardial perfusion: an artificial intelligence-based approach using perfusion mapping. Circulation. (2020) 141:1282–91. doi: 10.1161/CIRCULATIONAHA.119.044666, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.CGdS E Silva, Buginga GC, Eads E Silva, Arena R, Rouleau CR, Aggarwal S, et al., Prediction of mortality in coronary artery disease: role of machine learning and maximal exercise capacity. Mayo Clinic proceedings; (2022). Elsevier. [DOI] [PubMed] [Google Scholar]
- 41.Raghunath S, Ulloa Cerna AE, Jing L, vanMaanen DP, Stough J, Hartzel DN, et al. Prediction of mortality from 12-lead electrocardiogram voltage data using a deep neural network. Nat Med. (2020) 26:886–91. doi: 10.1038/s41591-020-0870-z, PMID: [DOI] [PubMed] [Google Scholar]
- 42.Toya T, Ahmad A, Attia Z, Cohen-Shelly M, Ozcan I, Noseworthy PA, et al. Vascular aging detected by peripheral endothelial dysfunction is associated with ECG-derived physiological aging. J Am Heart Assoc. (2021) 10:e018656. doi: 10.1161/JAHA.120.018656, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Eisenberg E, McElhinney PA, Commandeur F, Chen X, Cadet S, Goeller M, et al. Deep learning-based quantification of Epicardial adipose tissue volume and attenuation predicts major adverse cardiovascular events in asymptomatic subjects. Circ Cardiovasc Imaging. (2020) 13:e009829. doi: 10.1161/CIRCIMAGING.119.009829, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bhinder B, Gilvary C, Madhukar NS, Elemento O. Artificial intelligence in Cancer research and precision medicine. Cancer Discov. (2021) 11:900–15. doi: 10.1158/2159-8290.CD-21-0090, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gaur K, Jagtap MM. Role of artificial intelligence and machine learning in prediction, diagnosis, and prognosis of Cancer. Cureus. (2022) 14:e31008. doi: 10.7759/cureus.31008, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Huang S, Yang J, Fong S, Zhao Q. Artificial intelligence in cancer diagnosis and prognosis: opportunities and challenges. Cancer Lett. (2020) 471:61–71. doi: 10.1016/j.canlet.2019.12.007, PMID: [DOI] [PubMed] [Google Scholar]
- 47.Wang S-H, Chen G, Zhong X, Lin T, Shen Y, Fan X, et al. Global development of artificial intelligence in cancer field: a bibliometric analysis range from 1983 to 2022. Front Oncol. (2023) 13:1215729. doi: 10.3389/fonc.2023.1215729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Enshaei A, Robson CN, Edmondson RJ. Artificial intelligence systems as prognostic and predictive tools in ovarian Cancer. Ann Surg Oncol. (2015) 22:3970–5. doi: 10.1245/s10434-015-4475-6, PMID: [DOI] [PubMed] [Google Scholar]
- 49.Nartowt BJ, Hart GR, Muhammad W, Liang Y, Stark GF, Deng J. Robust machine learning for colorectal Cancer risk prediction and stratification. Front Big Data. (2020) 3:6. doi: 10.3389/fdata.2020.00006, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nartowt BJ, Hart GR, Roffman DA, Llor X, Ali I, Muhammad W, et al. Scoring colorectal cancer risk with an artificial neural network based on self-reportable personal health data. PLoS One. (2019) 14:e0221421. doi: 10.1371/journal.pone.0221421, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hart GR, Roffman DA, Decker R, Deng J. A multi-parameterized artificial neural network for lung cancer risk prediction. PLoS One. (2018) 13:e0205264. doi: 10.1371/journal.pone.0205264, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Stark GF, Hart GR, Nartowt BJ, Deng J. Predicting breast cancer risk using personal health data and machine learning models. PLoS One. (2019) 14:e0226765. doi: 10.1371/journal.pone.0226765, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Roffman D, Hart G, Girardi M, Ko CJ, Deng J. Predicting non-melanoma skin cancer via a multi-parameterized artificial neural network. Sci Rep. (2018) 8:1701. doi: 10.1038/s41598-018-19907-9, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hunter B, Chen M, Ratnakumar P, Alemu E, Logan A, Linton-Reid K, et al. A radiomics-based decision support tool improves lung cancer diagnosis in combination with the herder score in large lung nodules. EBioMedicine. (2022) 86:104344. doi: 10.1016/j.ebiom.2022.104344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Perez-Lopez R, Reis-Filho JS, Kather JN. A framework for artificial intelligence in cancer research and precision oncology. NPJ Prec Oncology. (2023) 7:43. doi: 10.1038/s41698-023-00383-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hollon TC, Pandian B, Adapa AR, Urias E, Save AV, Khalsa SSS, et al. Near real-time intraoperative brain tumor diagnosis using stimulated Raman histology and deep neural networks. Nat Med. (2020) 26:52–8. doi: 10.1038/s41591-019-0715-9, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhang B, Shi H, Wang H. Machine learning and AI in Cancer prognosis, prediction, and treatment selection: a critical approach. J Multidiscip Healthc. (2023) 16:1779–91. doi: 10.2147/JMDH.S410301, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Luo Y, Peng L, Shan W, Sun M, Luo L, Liang W. Machine learning in the development of targeting microRNAs in human disease. Front Genet. (2023) 13:189. doi: 10.3389/fgene.2022.1088189, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Azari H, Nazari E, Mohit R, Asadnia A, Maftooh M, Nassiri M, et al. Machine learning algorithms reveal potential miRNAs biomarkers in gastric cancer. Sci Rep. (2023) 13:6147. doi: 10.1038/s41598-023-32332-x, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Moon I, LoPiccolo J, Baca SC, Sholl LM, Kehl KL, Hassett MJ, et al. Machine learning for genetics-based classification and treatment response prediction in cancer of unknown primary. Nat Med. (2023) 29:2057–67. doi: 10.1038/s41591-023-02482-6, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Placido D, Yuan B, Hjaltelin JX, Zheng C, Haue AD, Chmura PJ, et al. A deep learning algorithm to predict risk of pancreatic cancer from disease trajectories. Nat Med. (2023) 29:1113–22. doi: 10.1038/s41591-023-02332-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.The Lancet . Diabetes: a defining disease of the 21st century. Lancet. (2023) 401:2087. doi: 10.1016/S0140-6736(23)01296-5, PMID: [DOI] [PubMed] [Google Scholar]
- 63.Duan D, Kengne AP, Echouffo-Tcheugui JB. Screening for diabetes and prediabetes. Endocrinol Metab Clin. (2021) 50:369–85. doi: 10.1016/j.ecl.2021.05.002, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Davidson KW, Barry MJ, Mangione CM, Cabana M, Caughey AB, Davis EM, et al. Screening for prediabetes and type 2 diabetes: US preventive services task force recommendation statement. JAMA. (2021) 326:736–43. doi: 10.1001/jama.2021.12531, PMID: [DOI] [PubMed] [Google Scholar]
- 65.Ellahham S. Artificial intelligence: The future for diabetes care. Am J Med. (2020) 133:895–00. doi: 10.1016/j.amjmed.2020.03.033 [DOI] [PubMed] [Google Scholar]
- 66.Huang X, Wang H, She C, Feng J, Liu X, Hu X, et al. Artificial intelligence promotes the diagnosis and screening of diabetic retinopathy. Front Endocrinol. (2022) 13:946915. doi: 10.3389/fendo.2022.946915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nomura A, Noguchi M, Kometani M, Furukawa K, Yoneda T. Artificial intelligence in current diabetes management and prediction. Curr Diab Rep. (2021) 21:61. doi: 10.1007/s11892-021-01423-2, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pyrros A, Borstelmann SM, Mantravadi R, Zaiman Z, Thomas K, Price B, et al. Opportunistic detection of type 2 diabetes using deep learning from frontal chest radiographs. Nat Commun. (2023) 14:4039. doi: 10.1038/s41467-023-39631-x, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Abraham SB, Arunachalam S, Zhong A, Agrawal P, Cohen O, McMahon CM. Improved real-world glycemic control with continuous glucose monitoring system predictive alerts. (2021) 1932–2968 Contract No: 1 [DOI] [PMC free article] [PubMed]
- 70.Benjamens S, Dhunnoo P, Meskó B. The state of artificial intelligence-based FDA-approved medical devices and algorithms: an online database. NPJ Digit Med. (2020) 3:118. doi: 10.1038/s41746-020-00324-0, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Guan Z, Li H, Liu R, Cai C, Liu Y, Li J, et al. Artificial intelligence in diabetes management: advancements, opportunities, and challenges. Cell Rep Med. (2023) 4:101213. doi: 10.1016/j.xcrm.2023.101213, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Vasiloglou MF, Mougiakakou S, Aubry E, Bokelmann A, Fricker R, Gomes F, et al. A comparative study on carbohydrate estimation: GoCARB vs. Diet Nutr. (2018) 10:741. doi: 10.3390/nu10060741, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Beard JR, Officer A, De Carvalho IA, Sadana R, Pot AM, Michel J-P, et al. The world report on ageing and health: a policy framework for healthy ageing. Lancet. (2016) 387:2145–54. doi: 10.1016/S0140-6736(15)00516-4, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.World Health Organization . Ageing and health. (2022b). Available at: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health.
- 75.World health Organization . (2023c). Ageing Geneva Available at: https://www.who.int/health-topics/ageing#tab=tab_1.
- 76.Tkatch R, Musich S, MacLeod S, Alsgaard K, Hawkins K, Yeh CS. Population health management for older adults: review of interventions for promoting successful aging across the health continuum. Gerontol Geriatr Med. (2016) 2:787. doi: 10.1177/2333721416667877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Salive ME. Multimorbidity in older adults. Epidemiol Rev. (2013) 35:75–83. doi: 10.1093/epirev/mxs009 [DOI] [PubMed] [Google Scholar]
- 78.Ma B, Yang J, Wong FKY, Wong AKC, Ma T, Meng J, et al. Artificial intelligence in elderly healthcare: a scoping review. Ageing Res Rev. (2023) 83:101808. doi: 10.1016/j.arr.2022.101808, PMID: [DOI] [PubMed] [Google Scholar]
- 79.World Health Organization . Disability. Geneva: WHO; (2023d). [Google Scholar]
- 80.Hu X, Zeng X, Xu Y, Luo C, Jia L, Zhao Z, et al. A soft robotic intervention for gait enhancement in older adults. IEEE Trans Neural Syst Rehabil Eng. (2021) 29:1838–47. doi: 10.1109/TNSRE.2021.3109729, PMID: [DOI] [PubMed] [Google Scholar]
- 81.Pu L, Moyle W, Jones C, Todorovic M. The effect of a social robot intervention on sleep and motor activity of people living with dementia and chronic pain: a pilot randomized controlled trial. Maturitas. (2021) 144:16–22. doi: 10.1016/j.maturitas.2020.09.003, PMID: [DOI] [PubMed] [Google Scholar]
- 82.Valero MÁ, Bravo J, Chamizo JMG, López-de-Ipiña D. Integration of multisensor hybrid reasoners to support personal autonomy in the smart home. Sensors. (2014) 14:17313–30. doi: 10.3390/s140917313, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.VandeWeerd C, Yalcin A, Aden-Buie G, Wang Y, Roberts M, Mahser N, et al. HomeSense: design of an ambient home health and wellness monitoring platform for older adults. Heal Technol. (2020) 10:1291–09. doi: 10.1007/s12553-019-00404-6 [DOI] [Google Scholar]
- 84.Follmann A, Schollemann F, Arnolds A, Weismann P, Laurentius T, Rossaint R, et al. Reducing loneliness in stationary geriatric care with robots and virtual encounters—a contribution to the COVID-19 pandemic. Int J Environ Res Public Health. (2021) 18:4846. doi: 10.3390/ijerph18094846, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pei-Ti H, Chen-Shie H, Ya-Fang H, Jeu-Jung C. The effects of a social participation app on seniors. J Nurs Res. (2021) 29:e168. doi: 10.1097/JNR.0000000000000451 [DOI] [PubMed] [Google Scholar]
- 86.Aggar C, Sorwar G, Seton C, Penman O, Ward A. Smart home technology to support older people's quality of life: a longitudinal pilot study. Int J Older People Nursing. (2023) 18:e12489. doi: 10.1111/opn.12489, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Park J-H. The effects of robot-assisted left-hand training on hemispatial neglect in older patients with chronic stroke: a pilot and randomized controlled trial. Medicine. (2021) 100:e24781. doi: 10.1097/MD.0000000000024781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Calabrò RS, De Luca R, Leo A, Balletta T, Marra A, Bramanti P. Lokomat training in vascular dementia: motor improvement and beyond! Aging Clin Exp Res. (2015) 27:935–7. doi: 10.1007/s40520-015-0343-2, PMID: [DOI] [PubMed] [Google Scholar]
- 89.Koumpouros Y, Toulias TL, Tzafestas CS, Moustris G. Assessment of an intelligent robotic rollator implementing navigation assistance in frail seniors. Technol Disabil. (2020) 32:159–77. doi: 10.3233/TAD-200271 [DOI] [Google Scholar]
- 90.Mizuno J, Saito D, Sadohara K, Nihei M, Ohnaka S, Suzurikawa J, et al. Effect of the information support robot on the daily activity of older people living alone in actual living environment. Int J Environ Res Public Health. (2021) 18:2498. doi: 10.3390/ijerph18052498, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ahmed MU. A personalized health-monitoring system for elderly by combining rules and case-based reasoning. pHealth. (2015) 1:249–54. [PubMed] [Google Scholar]
- 92.Tsamis KI, Rigas G, Nikolaos K, Fotiadis DI, Konitsiotis S. Accurate monitoring of Parkinson’s disease symptoms with a wearable device during COVID-19 pandemic. In Vivo. (2021) 35:2327–30. doi: 10.21873/invivo.12507, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wang L-H, Hsiao Y-M, Xie X-Q, Lee S-Y. An outdoor intelligent healthcare monitoring device for the elderly. IEEE Trans Consum Electron. (2016) 62:128–35. doi: 10.1109/TCE.2016.7514671 [DOI] [Google Scholar]
- 94.Lazarou I, Stavropoulos TG, Meditskos G, Andreadis S, Kompatsiaris IY, Tsolaki M. Long-term impact of intelligent monitoring technology on people with cognitive impairment: an observational study. J Alzheimers Dis. (2019) 70:757–92. doi: 10.3233/JAD-190423, PMID: [DOI] [PubMed] [Google Scholar]
- 95.Pu L, Moyle W, Jones C, Todorovic M. The effectiveness of social robots for older adults: a systematic review and meta-analysis of randomized controlled studies. The Gerontologist. (2019) 59:e37–51. doi: 10.1093/geront/gny046 [DOI] [PubMed] [Google Scholar]
- 96.Marino N, Putignano G, Cappilli S, Chersoni E, Santuccione A, Calabrese G, et al. Towards AI-driven longevity research: an overview. Front Aging. (2023) 4:1057204. doi: 10.3389/fragi.2023.1057204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Guerra BMV, Torti E, Marenzi E, Schmid M, Ramat S, Leporati F, et al. Ambient assisted living for frail people through human activity recognition: state-of-the-art, challenges and future directions. Front Neurosci. (2023) 17:1256682. doi: 10.3389/fnins.2023.1256682, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Spoladore D, Trombetta A. Ambient assisted working solutions for the ageing workforce: a literature review. Electronics. (2023) 12:101. doi: 10.3390/electronics12010101 [DOI] [Google Scholar]
- 99.Smer-Barreto V, Quintanilla A, Elliott RJR, Dawson JC, Sun J, Campa VM, et al. Discovery of senolytics using machine learning. Nat Commun. (2023) 14:3445. doi: 10.1038/s41467-023-39120-1, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.World Health Organization (2020). World mental health day: an opportunity to kick-start a massive scale-up in investment in mental health. Geneva: World Health Organization. [Google Scholar]
- 101.National Institutes of Health (2023). Mental Health During the COVID-19 Pandemic: an urgent issue. Available at: https://covid19.nih.gov/covid-19-topics/mental-health#:~:text=Rates%20of%20anxiety%2C%20depression%2C%20and,have%20mental%20illnesses%20or%20disorders.
- 102.Gao Y, Bagheri N, Furuya-Kanamori L. Has the COVID-19 pandemic lockdown worsened eating disorders symptoms among patients with eating disorders? systematic review. A Z Gesundh Wiss. (2022) 30:2743–52. doi: 10.1007/s10389-022-01704-4, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Fei J, Yong J, Hui Z, Yi D, Hao L, Sufeng M, et al. Artificial intelligence in healthcare: past, present and future. Stroke Vasc Neurol. (2017) 2:230–43. doi: 10.1136/svn-2017-000101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Miller DD, Brown EW. Artificial intelligence in medical practice: the question to the answer? Am J Med. (2018) 131:129–033. doi: 10.1016/j.amjmed.2017.10.035 [DOI] [PubMed] [Google Scholar]
- 105.Minerva F, Giubilini A. Is AI the future of mental healthcare? Topoi (Dordr). (2023) 42:1–9. doi: 10.1007/s11245-023-09932-3, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Graham S, Depp C, Lee EE, Nebeker C, Tu X, Kim HC, et al. Artificial intelligence for mental health and mental illnesses: an overview. Curr Psychiatry Rep. (2019) 21:116. doi: 10.1007/s11920-019-1094-0, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.D’Alfonso S. AI in mental health. Curr Opin Psychol. (2020) 36:112–7. doi: 10.1016/j.copsyc.2020.04.005 [DOI] [PubMed] [Google Scholar]
- 108.World Health Organization (n.d.). Communicable and noncommunicable diseases, and mental health. Available at: https://www.who.int/our-work/communicable-and-noncommunicable-diseases-and-mental-health
- 109.Feller DJ, Zucker J, Yin MT, Gordon P, Elhadad N. Using clinical notes and natural language processing for automated HIV risk assessment. J Acquir Immune Defic Syndr. (2018) 77:160–6. doi: 10.1097/QAI.0000000000001580, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Kakalou C, Lazarus JV, Koutkias V. Mining social Media for Perceptions and Trends on HIV pre-exposure prophylaxis. Stud Health Technol Inform. (2019) 264:959–63. doi: 10.3233/SHTI190366, PMID: [DOI] [PubMed] [Google Scholar]
- 111.Xiang Y, Du J, Fujimoto K, Li F, Schneider J, Tao C. Application of artificial intelligence and machine learning for HIV prevention interventions. Lancet HIV. (2022) 9:e54–62. doi: 10.1016/S2352-3018(21)00247-2, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Pan American Health Organization . PAHO launches new initiative to eliminate mother-to-child transmission of four diseases. (2017) Available at: https://www3.paho.org/hq/index.php?option=com_content&view=article&id=13567:paho-launches-new-initiative-to-eliminate-mother-to-child-transmission-of-four-diseases&Itemid=0&lang=en#gsc.tab=0.
- 113.da Rocha MA, dos Santos MM, Fontes RS, de Melo ASP, Cunha-Oliveira A, Miranda AE, et al. The text mining technique applied to the analysis of health interventions to combat congenital syphilis in Brazil: The case of the “syphilis no!” Project. Front Public Health. (2022) 10:680. doi: 10.3389/fpubh.2022.855680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Pinto R, Valentim R, Fernandes da Silva L, Fontoura de Souza G, Farias G, De Moura Santos Lima T, et al. Use of interrupted time series analysis in understanding the course of the congenital syphilis epidemic in Brazil. The Lancet regional health. Americas. (2022) 7:100163. doi: 10.1016/j.lana.2021.100163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Caitano AR, Gusmão CMG, Dias-Trindade S, Barbalho IMP, Morais PSG, Caldeira-Silva GJP, et al. Massive health education through technological mediation: analyses and impacts on the syphilis epidemic in Brazil. Front Public Health. (2022) 10:944213. doi: 10.3389/fpubh.2022.944213, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Sisimayi C, Harley C, Nyabadza F, Visaya MV. AI-enabled case detection model for infectious disease outbreaks in resource-limited settings. Front Appl Math Statis. (2023) 9:9. doi: 10.3389/fams.2023.1133349 [DOI] [Google Scholar]
- 117.Brownstein JS, Rader B, Astley CM, Tian H. Advances in artificial intelligence for infectious-disease surveillance. N Engl J Med. (2023) 388:1597–607. doi: 10.1056/NEJMra2119215, PMID: [DOI] [PubMed] [Google Scholar]
- 118.World Health Organization . Ethics and governance of artificial intelligence for health: WHO guidance. Geneva: World Health Organization; (2021). [Google Scholar]
- 119.Santangelo OE, Gentile V, Pizzo S, Giordano D, Cedrone F. Machine learning and prediction of infectious diseases: a systematic review. Mach Learn Knowl Extract. (2023) 5:175–98. doi: 10.3390/make5010013 [DOI] [Google Scholar]
- 120.Palaniappan S, David B. Prediction of epidemic disease dynamics on the infection risk using machine learning algorithms. SN Comp Sci. (2021) 3:97. doi: 10.1007/s42979-021-00902-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Maharaj AS, Parker J, Hopkins JP, Gournis E, Bogoch II, Rader B, et al. The effect of seasonal respiratory virus transmission on syndromic surveillance for COVID-19 in Ontario Canada. Lancet Infect Dis. (2021) 21:593–4. doi: 10.1016/S1473-3099(21)00151-1, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Roy S, Biswas P, Ghosh P. Spatiotemporal tracing of pandemic spread from infection data. Sci Rep. (2021) 11:17689. doi: 10.1038/s41598-021-97207-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Pascucci M, Royer G, Adamek J, Asmar MA, Aristizabal D, Blanche L, et al. AI-based mobile application to fight antibiotic resistance. Nat Commun. (2021) 12:1173. doi: 10.1038/s41467-021-21187-3, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Wong F, de la Fuente-Nunez C, Collins JJ. Leveraging artificial intelligence in the fight against infectious diseases. Science. (2023) 381:164–70. doi: 10.1126/science.adh1114, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Bojar D, Powers RK, Camacho DM, Collins JJ. Deep-learning resources for studying glycan-mediated host-microbe interactions. Cell Host Microbe. (2021) 29:132–44.e3. doi: 10.1016/j.chom.2020.10.004, PMID: [DOI] [PubMed] [Google Scholar]
- 126.Hie B, Zhong ED, Berger B, Bryson B. Learning the language of viral evolution and escape. Science. (2021) 371:284–8. doi: 10.1126/science.abd7331, PMID: [DOI] [PubMed] [Google Scholar]
- 127.Wheeler NE, Gardner PP, Barquist L. Machine learning identifies signatures of host adaptation in the bacterial pathogen Salmonella enterica. PLoS Genet. (2018) 14:e1007333. doi: 10.1371/journal.pgen.1007333, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.World Health Organization . Global report on infection prevention and control. Geneva, World Health Organization: (2022c). [Google Scholar]
- 129.Fitzpatrick F, Doherty A, Lacey G. Using artificial intelligence in infection prevention. Curr Treat Options Infect Dis. (2020) 12:135–44. doi: 10.1007/s40506-020-00216-7, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Bechmann L, Geginat G. Semi-automated contact tracing and management of contact precautions during the COVID-19 pandemic within a tertiary hospital. Infect Prev Pract. (2023) 5:100266. doi: 10.1016/j.infpip.2022.100266, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Milinovich GJ, Williams GM, Clements AC, Hu W. Internet-based surveillance systems for monitoring emerging infectious diseases. Lancet Infect Dis. (2014) 14:160–8. doi: 10.1016/S1473-3099(13)70244-5, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Worlikar H, Vadhiraj VV, Murray A, O'Connell J, Connolly C, Walsh JC, et al. Is it feasible to use a humanoid robot to promote hand hygiene adherence in a hospital setting? Infect Prev Pract. (2022) 4:100188. doi: 10.1016/j.infpip.2021.100188, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Branch-Elliman W, Sundermann AJ, Wiens J, Shenoy ES. The future of automated infection detection: innovation to transform practice (part III/III). Antimicrob Steward Healthc Epidemiol. (2023) 3:e26. doi: 10.1017/ash.2022.333, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.World Health Organization . Public health and environment. Geneva: World Health Organization; (2023e). [Google Scholar]
- 135.Nti EK, Cobbina SJ, Attafuah EA, Senanu LD, Amenyeku G, Gyan MA, et al. Water pollution control and revitalization using advanced technologies: uncovering artificial intelligence options towards environmental health protection, sustainability and water security. Heliyon. (2023) 9:e18170. doi: 10.1016/j.heliyon.2023.e18170, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.VoPham T, Hart JE, Laden F, Chiang Y-Y. Emerging trends in geospatial artificial intelligence (geoAI): potential applications for environmental epidemiology. Environ Health. (2018) 17:40. doi: 10.1186/s12940-018-0386-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Chinnaswamy A, Walton N. AI and environmental health: a platform ecosystem perspective In: Ong HL, Doong R-a, Naguib R, Lim CP, Nagar AK, editors. Artificial intelligence and environmental sustainability: Challenges and solutions in the era of industry 40. Singapore: Springer Nature Singapore; (2022) [Google Scholar]
- 138.Weichenthal S, Hatzopoulou M, Brauer M. A picture tells a thousand… exposures: opportunities and challenges of deep learning image analyses in exposure science and environmental epidemiology. Environ Int. (2019) 122:3–10. doi: 10.1016/j.envint.2018.11.042, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Alafif T, Tehame AM, Bajaba S, Barnawi A, Zia S. Machine and deep learning towards COVID-19 diagnosis and treatment: survey, challenges, and future directions. Int J Environ Res Public Health. (2021) 18:1117. doi: 10.3390/ijerph18031117, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Lee S, Lee D. Improved prediction of harmful algal blooms in four Major South Korea’s Rivers using deep learning models. Int J Environ Res Public Health. (2018) 15:1322. doi: 10.3390/ijerph15071322, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Gangula R, Thirupathi L, Parupati R, Sreeveda K, Gattoju S. Ensemble machine learning based prediction of dengue disease with performance and accuracy elevation patterns. Mater Today Proceed. (2023) 80:3458–63. [Google Scholar]
- 142.Dadheech P, Mehbodniya A, Tiwari S, Kumar S, Singh P, Gupta S, et al. Zika virus prediction using AI-driven technology and hybrid optimization algorithm in healthcare. J Healthcare Eng. (2022) 2022:1–13. doi: 10.1155/2022/2793850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Fayyazi M, Sardar P, Thomas SI, Daghigh R, Jamali A, Esch T, et al. Artificial intelligence/machine learning in energy management systems, control, and optimization of hydrogen fuel cell vehicles. Sustainability. (2023) 15:5249. doi: 10.3390/su15065249 [DOI] [Google Scholar]
- 144.Fan Z, Yan Z, Wen S. Deep learning and artificial intelligence in sustainability: a review of SDGs, renewable energy, and environmental health. Sustainability. (2023) 15:13493. doi: 10.3390/su151813493 [DOI] [Google Scholar]
- 145.United Nations . World environment situation room: data, information and knowledge on the environment. (n.d.). United Nation Environment Programme Available at: https://wesr.unep.org
- 146.Darrudi A, Ketabchi Khoonsari MH, Tajvar M. Challenges to achieving universal health coverage throughout the world: a systematic review. J Prev Med Public Health. (2022) 55:125–33. doi: 10.3961/jpmph.21.542, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.World Health Organization . Health systems strengthening. Geneva: World Health Organization; (2023f). [Google Scholar]
- 148.Mora C, McKenzie T, Gaw IM, Dean JM, von Hammerstein H, Knudson TA, et al. Over half of known human pathogenic diseases can be aggravated by climate change. Nat Clim Chang. (2022) 12:869–75. doi: 10.1038/s41558-022-01426-1, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.World Health Organization . Climate action: fast facts [press release]. Geneva: World Health Organization; (2022d). [Google Scholar]
- 150.Wilson D, Sheikh A, Görgens M, Ward K. Technology and universal health coverage: examining the role of digital health. J Glob Health. (2021) 11:16006. doi: 10.7189/jogh.11.16006, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Braithwaite J, Mannion R, Matsuyama Y, Shekelle P, Whittaker S, Al-Adawi S, et al. Accomplishing reform: successful case studies drawn from the health systems of 60 countries. Int J Qual Health Care. (2017) 29:880–6. doi: 10.1093/intqhc/mzx122, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.McKinsey & Company . How digital tools could boost efficiency in African health systems. Chicago: McKinsey & Company; (2023). [Google Scholar]
- 153.Kueper JK. Primer for artificial intelligence in primary care. Can Fam Physician. (2021) 67:889–93. doi: 10.46747/cfp.6712889, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Lin SY, Mahoney MR, Sinsky CA. Ten ways artificial intelligence will transform primary care. J Gen Intern Med. (2019) 34:1626–30. doi: 10.1007/s11606-019-05035-1, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Terry AL, Kueper JK, Beleno R, Brown JB, Cejic S, Dang J, et al. Is primary health care ready for artificial intelligence? What do primary health care stakeholders say? BMC Med Inform Decis Mak. (2022) 22:237. doi: 10.1186/s12911-022-01984-6, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Amit G, Girshovitz I, Marcus K, Zhang Y, Pathak J, Bar V, et al. Estimation of postpartum depression risk from electronic health records using machine learning. BMC Pregnancy Childbirth. (2021) 21:630. doi: 10.1186/s12884-021-04087-8, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Black JE, Kueper JK, Terry AL, Lizotte DJ. Development of a prognostic prediction model to estimate the risk of multiple chronic diseases: constructing a copula-based model using Canadian primary care electronic medical record data. Int J Popul Data Sci. (2021) 6:1395. doi: 10.23889/ijpds.v5i1.1395, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Pearce C, McLeod A, Rinehart N, Whyte R, Deveny E, Shearer M. Artificial intelligence and the clinical world: a view from the front line. Med J Aust. (2019) 210:S38–s40. doi: 10.5694/mja2.50025 [DOI] [PubMed] [Google Scholar]
- 159.Wingrove P, Liaw W, Weiss J, Petterson S, Maier J, Bazemore A. Using machine learning to predict primary care and advance workforce research. Ann Fam Med. (2020) 18:334–40. doi: 10.1370/afm.2550, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.MacRae J, Darlow B, McBain L, Jones O, Stubbe M, Turner N, et al. Accessing primary care big data: the development of a software algorithm to explore the rich content of consultation records. BMJ Open. (2015) 5:e008160. doi: 10.1136/bmjopen-2015-008160, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Turner NM, MacRae J, Nowlan ML, McBain L, Stubbe MH, Dowell A. Quantifying the incidence and burden of herpes zoster in New Zealand general practice: a retrospective cohort study using a natural language processing software inference algorithm. BMJ Open. (2018) 8:e021241. doi: 10.1136/bmjopen-2017-021241, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Scardoni A, Balzarini F, Signorelli C, Cabitza F, Odone A. Artificial intelligence-based tools to control healthcare associated infections: a systematic review of the literature. J Infect Public Health. (2020) 13:1061–77. doi: 10.1016/j.jiph.2020.06.006, PMID: [DOI] [PubMed] [Google Scholar]
- 163.Patel VL, Shortliffe EH, Stefanelli M, Szolovits P, Berthold MR, Bellazzi R, et al. The coming of age of artificial intelligence in medicine. Artif Intell Med. (2009) 46:5–17. doi: 10.1016/j.artmed.2008.07.017, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Morgenstern JD, Rosella LC, Daley MJ, Goel V, Schünemann HJ, Piggott T. AI's gonna have an impact on everything in society, so it has to have an impact on public health: a fundamental qualitative descriptive study of the implications of artificial intelligence for public health. BMC Public Health. (2021) 21:40. doi: 10.1186/s12889-020-10030-x, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Stalgaitis CA, Jordan JW, Djakaria M, Saggese DJ, Bruce HR. Psychographic segmentation to identify higher-risk teen peer crowds for health communications: validation of Virginia's Mindset Lens Survey. Front Public Health. (2022) 10:864. doi: 10.3389/fpubh.2022.871864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Hasikin K, Lai KW, Satapathy SC, Sabanci K, Aslan MF. Editorial: emerging applications of text analytics and natural language processing in healthcare. Front Digital Health. (2023) 5:948. doi: 10.3389/fdgth.2023.1227948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Lim S, Schmälzle R. Artificial intelligence for health message generation: an empirical study using a large language model (LLM) and prompt engineering. Front Commun. (2023) 8:82. doi: 10.3389/fcomm.2023.1129082 [DOI] [Google Scholar]
- 168.Hudlicka E. Virtual training and coaching of health behavior: example from mindfulness meditation training. Patient Educ Couns. (2013) 92:160–6. doi: 10.1016/j.pec.2013.05.007, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Green N, Rubinelli S, Scott D, Visser A. Health communication meets artificial intelligence. Patient Educ Couns. (2013) 92:139–41. doi: 10.1016/j.pec.2013.06.013 [DOI] [PubMed] [Google Scholar]
- 170.The Lancet . Can artificial intelligence improve cancer care? Lancet Oncol. (2023) 24:577. doi: 10.1016/S1470-2045(23)00240-1 [DOI] [PubMed] [Google Scholar]
- 171.Naik N, Hameed BMZ, Shetty DK, Swain D, Shah M, Paul R, et al. Legal and ethical consideration in artificial intelligence in healthcare: who takes responsibility? Front Surgery. (2022) 9:322. doi: 10.3389/fsurg.2022.862322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Europarleuropaeu . Report on the proposal for a regulation of the European Parliament and of the council on the protection of individuals with regard to the processing of personal data and on the free movement of such data (general data protection regulation). (2023) Available at: https://www.europarl.europa.eu/doceo/document/A-7-2013-0402_EN.html.
- 173.Spoladore D, Sacco M, Trombetta A. A review of domain ontologies for disability representation. Expert Syst Appl. (2023) 228:120467. doi: 10.1016/j.eswa.2023.120467 [DOI] [Google Scholar]
- 174.Barredo Arrieta A, Díaz-Rodríguez N, Del Ser J, Bennetot A, Tabik S, Barbado A, et al. Explainable artificial intelligence (XAI): concepts, taxonomies, opportunities and challenges toward responsible AI. Inform Fusion. (2020) 58:82–15. doi: 10.1016/j.inffus.2019.12.012 [DOI] [Google Scholar]