Abstract
Background
Pediatric hematology and oncology disease is a physically and emotionally demanding health condition for families. High self-esteem and ego-resilience among caregivers, which have recently gained increased recognition, might help ease caregiver burdens. Few studies, however, have simultaneously investigated the relationships between self-esteem, ego-resilience, and caregiver burden among caregivers of children with hematologic and oncologic disease.
Objective
The purpose of this study is to investigate the relationships between caregiver burden, self-esteem, and ego-resilience and examine whether ego-resilience plays a role in mediating the relationship between self-esteem and caregiver burden among family caregivers of children with hematologic and oncologic disease.
Design
Descriptive correlational study.
Setting
The outpatient clinic of the department of pediatric hematology and oncology at a flagship university hospital in a metropolitan city in South Korea.
Participants
The sample comprised 109 primary family caregivers of children with hematologic and oncologic disease. Convenience sampling method was used.
Methods
The participants completed the Ego-Resiliency Scale, Rosenberg Self-Esteem Scale, and Family Burden Questionnaire. One-way analysis of variance, independent t-tests, and correlation analyses were conducted using IBM SPSS 25.0. The mediating effect of ego-resilience was estimated using the PROCESS macro and bootstrap method in SPSS.
Results
Caregiver burden showed significant negative associations with self-esteem and ego-resilience, with moderate effect sizes (r = −.391 and −0.361, respectively, p = .001). Ego-resilience mediated the relationship between self-esteem and caregiver burden (b = −0.019; 95 % bias-corrected bootstrap confidence interval −0.035 and −0.001).
Conclusions
Self-esteem and ego-resilience may lessen caregiver burden among families of children with hematologic and oncologic disease, and self-esteem of caregivers tends to promote their ego-resilience. Therefore, self-esteem and ego-resilience should be improved among family caregivers to reduce their caregiver burden.
Keywords: Caregiver burden, Ego-resilience, Self-esteem, Childhood cancer
1. Introduction
Caregiver burden is defined as “the extent to which caregivers perceive their emotional health, physical health, social life, and financial status as having been negatively impacted as a result of caring for their relative” (p. 261) [1]. Previous studies on caregiver burden have mostly focused on the relationship between spouses [2] and adult children of adult patients, such as patents with dementia [3] and older adults with advanced cancer [4]. However, depending on the type of caregiving dyad, the dynamics and functions of caregiving will vary [2]. Thus, the experiences of families caring for children with hematologic and oncologic disease may also vary. These families may be diverse and may experience various financial, social, physical, dependency, and emotional burdens. Families may suffer from high medical expenses due to the continuous treatment of a child with hematologic and oncologic disease [5] and/or experience social and emotional challenges and/or relationship issues due to anxiety at the thought of losing their child [6]. These detrimental effects could decrease the quality of life of caregivers and increase their chance of developing physical and mental health issues. Eventually, these effects could decrease the ability of caregivers to care for their sick children and result in family instability.
1.1. Traditional concept: self-esteem
Self-esteem is defined as subjective evaluation of oneself, and a person with high self-esteem considers himself or herself as a valued human being [7]. Self-esteem is the idea that one is valuable, important, and capable; as such, it is an aspect of self-concept that can be expressed either positively or negatively [8]. Self-esteem may have a significant role in caregivers' ability to overcome burdens [9]. The traditional concept is that caregivers can create a positive attitude and deal with challenging situations by having high self-esteem. Self-esteem has been negatively correlated with caregiver burden [10]. In other words, caregivers with strong positivity and self-esteem experience lower levels of caregiver burden [9]. This is because caregivers with strong self-esteem can deal with various burdens with a psychologically positive mindset [8]. Thus, having high self-esteem may help relieve caregivers of their burden, improving their overall health [9]. Among the caregivers of children with hematologic and oncologic disease, those who have strong self-esteem will feel more confident and appreciated as valued caregivers, and they will have a positive outlook on their child's treatment.
1.2. New rising concept: ego-resilience
Ego-resilience is a relatively new concept; thus, research on ego-resilience in the context of caregiver burden is limited. Studies in children have defined resilience as the capacity to recover and subsequently maintain adaptive behaviors after a stressful event that may trigger initial retreat or incapacity [11]. Strong ego-resilience allows a person to continue functioning normally despite emotional turmoil. A cross-sectional survey conducted at the Mayo Clinic revealed that resilience exhibited large inverse relationships with anxiety and depression [12]. The anxiety level was fourfold higher and the depression level was threefold higher among participants with low resilience than those with high resilience [12]. Therefore, it is expected that ego-resilience among caregivers will influence how effectively they cope with difficult situations and make them feel less stressed and burdened. A study among caregivers of patients with Alzheimer's disease showed that resilience allowed caregivers to manage and respond positively to stressful demands of care [13]. In a different study on patients with head and neck cancer, resilient patients reported experiencing positive changes during their cancer experience [14]. These positive changes included increased appreciation of life, changes in health-related behaviors, hope for new possibilities, feelings of control, personal strength, interpersonal effectiveness, and spiritual well-being [14]. Ultimately, increasing resilience of caregivers improves the well-being and overall quality of life for both caregivers and patients [15].
High ego-resilience might be a key factor in bringing about positive changes in the life quality, treatment efficacy, and general health of children with hematologic and oncologic disease and their caregivers. To our knowledge, no study has simultaneously investigated the relationship between caregiver burden, self-esteem, and ego-resilience in caregivers of children with hematologic and oncologic disease. Therefore, the purpose of this study is to investigate the association of self-esteem and ego-resilience on caregiver burden among caregivers of children with hematologic and oncologic disease. First, we hypothesized that family caregivers of children with cancer would experience different levels of caregiver burden, which is associated with either the characteristics of children or family caregivers (e.g., age, sex, diagnosis, health insurance, and pain or uncomfortable symptoms). Second, we hypothesized that family caregivers with higher self-esteem have lower level of caregiver burden. Finally, we hypothesized that this relationship is mediated by the ego-resilience of family caregivers.
2. Methods
2.1. Study design and participants
A cross-sectional anonymous survey targeted at primary family caregivers of children with hematologic and oncologic disease was employed as part of the study's descriptive correlational design. It was part of a research project examining the quality of life and death among families of children with cancer (A & B) [16]. Participants were recruited by using convenience sampling methods from the outpatient clinic of the department of pediatric hematology and oncology at a flagship university hospital in a metropolitan city in South Korea from March to May 2018.
The inclusion criteria were as follows: family caregivers of children (1) between 7 and 18 years of age who were (2) diagnosed with pediatric hematologic and oncologic disease and (3) currently receiving any treatment for their hematologic and oncologic disease, including chemotherapy, irradiation, transfusion, or neutropenic fever treatment. The exclusion criteria included (1) age under 7 years old because they may have some difficulties in expressing their thoughts and feelings to their parents, for example, age between 2 and 7 is “preoperational stage” and age between 7 and 12 is “concrete operation stage” [17], and (2) after treatment for childhood cancer (e.g., children with cancer doing only follow-up visits and checking their labs only).
2.2. Procedures
This study was approved by the institutional review boards of Kyungpook National University and Kyungpook National University Hospital before research initiation (KNU 2018-0041 and KNUH 2018-03-003). A trained research assistant (RA) was stationed in outpatient department and flyers were posted there to recruit participants. Interested family caregivers contacted the RA for further information; the RA provided information regarding the study's purpose, confidentiality, consent, and questionnaire items. They were provided written study information and an informed consent form to sign once they agreed to participate. The participants were assisted by the RA in completing the written information, the informed consent form, and the questionnaire. The entire process took approximately 20–30 min to complete. To reduce risks of validity, RAs were tasked with contacting potential participants instead of direct contact with researchers [18]. There was no direct contact with researchers in the recruitment and survey procedure to avoid any potential biases. Each participant was given a $10 gift card as compensation.
2.3. Measures
Mediator: ego-resilience. Each participant's ego-resilience was measured by using the Korean version of the Ego-Resiliency Scale (ER89) [19], which was translated into Korean [20]. This scale is a 14-item self-report instrument, and each item is assessed on a four-point scale. Higher scores indicate more resilience. The Cronbach's alpha coefficient of the original scale was 0.76 [19], and that of the Korean version was 0.67 [20]. The Cronbach's alpha of the overall 14 items in this study was 0.82.
Independent variable: self-esteem. Each participant's self-esteem was measured by using the Korean version of the Rosenberg Self-Esteem Scale [21], which was translated into Korean and evaluated for reliability and validity [22]. This scale is a 10-item self-report instrument, and each item is scored on a four-point scale. Higher scores indicate a higher self-esteem level. The Cronbach's alpha coefficient of the original scale was 0.88 [], and that of the Korean version was 0.90 [22]. The Cronbach's alpha of the overall 10 items in this study was 0.72.
Dependent variable: caregiver burden. Each family caregiver's burden was measured by using the Family Burden Questionnaire [23], which was developed for Korean chronically ill family members based on Zarit Burden Interview [1] and Novak and Guest's Caregiver Burden Inventory [24]. Its reliability and validity among parents of pediatric patients were previously established [25]. This questionnaire is a 25-item self-report instrument, and each item is scored on a five-point scale. Higher scores indicate a greater burden of caring for a child with cancer. The Cronbach's alpha coefficient of the original scale was 0.89 [23]. The Cronbach's alpha of the 25 overall items in this study was 0.91, and the alphas of each subscale were 0.74 for financial burden, 0.85 for social burden, 0.73 for physical burden, 0.72 for dependence burden, and 0.76 for emotional burden.
Characteristics of family caregiver and children with cancer. Included in this study were the demographics of children with cancer and family caregivers were included in the survey. For example, both the sex and age of children with cancer and family caregivers were considered. We considered financial issue would have an impact, so a “number of private health insurances in addition to National Health Insurance” were asked. In addition, children's severity of symptom may be a contributing factor to caregiver burden, as indicated by the 4-point Likert scale “frequency of pain or uncomfortable symptoms” (always, often, sometimes/rarely, never).
2.4. Statistical analyses
IBM SPSS version 25 (IBM Corp., Armonk, NY, USA) was used to conduct statistical analyses. Descriptive statistics were used to investigate the demographic characteristics of participants and their children with cancer and the main study variables (ego-resilience, self-esteem, and caregiver burden). Additionally, one-way analysis of variance (ANOVA) with Bonferroni post hoc test, independent t-tests, and Pearson correlations was used to evaluate associations between variables. If there was any difference between a demographic characteristic and the dependent variable, the characteristic was used as a covariate in the analysis.
The PROCESS macro and bootstrap method in SPSS were used to perform mediation tests [26]. To analyze the mediating role of ego-resilience in the relationship between self-esteem and caregiver burden in children with cancer, model 4 of the PROCESS macro was used. The PROCESS macro and bootstrap method were used instead of Baron and Kenny's three regression models [27] or the Sobel test [28] to evaluate the significance of the indirect effect. This is because they do not require an assumption of normal distribution. The PROCESS macro implements bias-corrected bootstrap confidence intervals (CIs) for the indirect effect. If bias-corrected bootstrap CIs for the indirect effect do not contain 0, an indirect effect is supported.
3. Results
3.1. Characteristics of study participants
The descriptive statistics for the 109 participants and main variables are shown in Table 1. Most family caregivers were female (85.3 %), and the mean age was 35.88 years (standard deviation [SD] = 4.42). More than half of the children with hematologic and oncologic disease were male (55.0 %), and the mean age was 9.65 years (SD = 5.88). Leukemia and lymphoma were the common diagnoses (31.3 %), followed by other hematologic diagnoses, such as hemophilia or von Willebrand disease (47.7 %) and solid tumors (21.1 %). In addition to the National Health Insurance, almost 92.6 % of children in South Korea had at least one private health insurance. Considering the general health of children, 32.4 % self-reported having pain and/or uncomfortable symptoms (e.g., nausea, anorexia, fatigue) occasionally, while 29.6 % self-reported having these symptoms often. The total mean score of caregiver burden was 2.33 (SD = 0.66). Among the five subcategories of caregiver burden, financial burden received the highest score (mean = 2.81; SD = 1.02), whereas emotional burden received the lowest score (mean = 2.15; SD = 0.64). The participants’ score for self-esteem was 30.57 (SD = 3.83), and that for ego-resilience was 38.28 (SD = 5.04).
Table 1.
Characteristics of study participants and main variables (N = 109).
| N | % | M | SD | Range | |
|---|---|---|---|---|---|
| Family caregivers of children with cancer | |||||
| Age | 35.88 | 4.42 | |||
| Sex | |||||
| Female | 93 | 85.3 | |||
| Male | 16 | 14.7 | |||
| Children with cancer | |||||
| Age | 9.65 | 5.88 | |||
| Sex | |||||
| Female | 49 | 45.0 | |||
| Male | 60 | 55.0 | |||
| Diagnosis of child | |||||
| Leukemia and lymphoma | 34 | 31.3 | |||
| Hematology, others | 52 | 47.7 | |||
| Solid oncology | 23 | 21.1 | |||
| Number of private health insurances (in addition to national health insurance) | |||||
| 0 | 8 | 7.4 | |||
| 1 | 61 | 56.5 | |||
| ≥2 | 39 | 36.1 | |||
| Frequency of pain or uncomfortable symptoms | |||||
| Never | 41 | 38.0 | |||
| Sometimes | 35 | 32.4 | |||
| Often | 32 | 29.6 | |||
| Always | 0 | 0 | |||
| Main variables | |||||
| Self-esteem | 30.57 | 3.83 | 20–38 | ||
| Ego-resilience | 38.28 | 5.04 | 26–54 | ||
| Caregiver burden, total (Mean score) | 2.33 | 0.66 | 1.24–4.32 | ||
| Financial burden | 2.81 | 1.02 | 1.00–5.00 | ||
| Social burden | 2.23 | 1.11 | 1.00–5.00 | ||
| Physical burden | 2.39 | 0.97 | 1.00–5.00 | ||
| Dependence burden | 2.39 | 0.56 | 1.17–3.83 | ||
| Emotional burden | 2.15 | 0.64 | 1.00–4.11 |
M: mean; SD: standard deviation.
Significant differences were observed in caregiver burden based on the child's diagnosis and frequency of pain or uncomfortable symptoms (Table 2). One-way ANOVA with post hoc test showed that family caregivers of children with leukemia and lymphoma experienced higher burdens than those of children with other hematologic cancer (F = 4.302; p = .016). The family caregivers also experienced higher burdens when their children with hematologic and oncologic disease often complained about pain or other uncomfortable symptoms as opposed to those who never or sometimes complained (F = 6.689; p = .002). Other demographic characteristics were not associated with any significant difference in caregiver burden. Therefore, the diagnosis and frequency of pain or uncomfortable symptoms of the child were taken as covariates in the mediation analysis.
Table 2.
Differences in caregiver burden based on participant characteristics (only significant or marginally significant results are listed).
| Caregiver Burden | |||
|---|---|---|---|
| M | SD | F (p) | |
| Diagnosis of child | 4.302 (.016) | ||
| Leukemia and lymphomaa | 2.60 | 0.60 | a> b |
| Hematology, othersb | 2.22 | 0.68 | |
| Solid oncologyc | 2.18 | 0.62 | |
| Frequency of pain or uncomfortable symptoms | |||
| Nevera | 2.21 | 0.65 | 6.689 (.002) |
| Sometimesb | 2.16 | 0.62 | c > b, a |
| Oftenc | 2.67 | 0.62 | |
M: mean; SD: standard deviation.
3.2. Correlation among ego-resilience, self-esteem, and caregiver burden
Based on Pearson bivariate correlations shown in Table 3, self-esteem and ego-resilience were negatively correlated with caregiver burden (r = −0.391 and −0.361, respectively, p = .001) with a moderate effect size [29]. The normality of the distribution of the main variables was determined by using skewness and kurtosis statistics. According to Curran et al. [30], skewness within the range of ±2.0 and kurtosis of ±7.0 are considered normal distribution. Thus, it was determined that the main variables in this study were considered to be normally distributed.
Table 3.
Correlations among self-esteem, ego resilience, and caregiver burden (N = 109).
| Variable | Skewness | Kurtosis | 1 | 2 | 3 |
|---|---|---|---|---|---|
| r (p) | r (p) | r (p) | |||
| 1. Self-esteem | −0.29 | −0.10 | – | ||
| 2. Ego-resilience | 0.62 | 1.05 | .518 (.001) | – | |
| 3. Caregiver burden | 0.29 | −0.60 | −.391 (.001) | −.361 (.001) | – |
3.3. Mediation effect of ego-resilience on self-esteem and caregiver burden
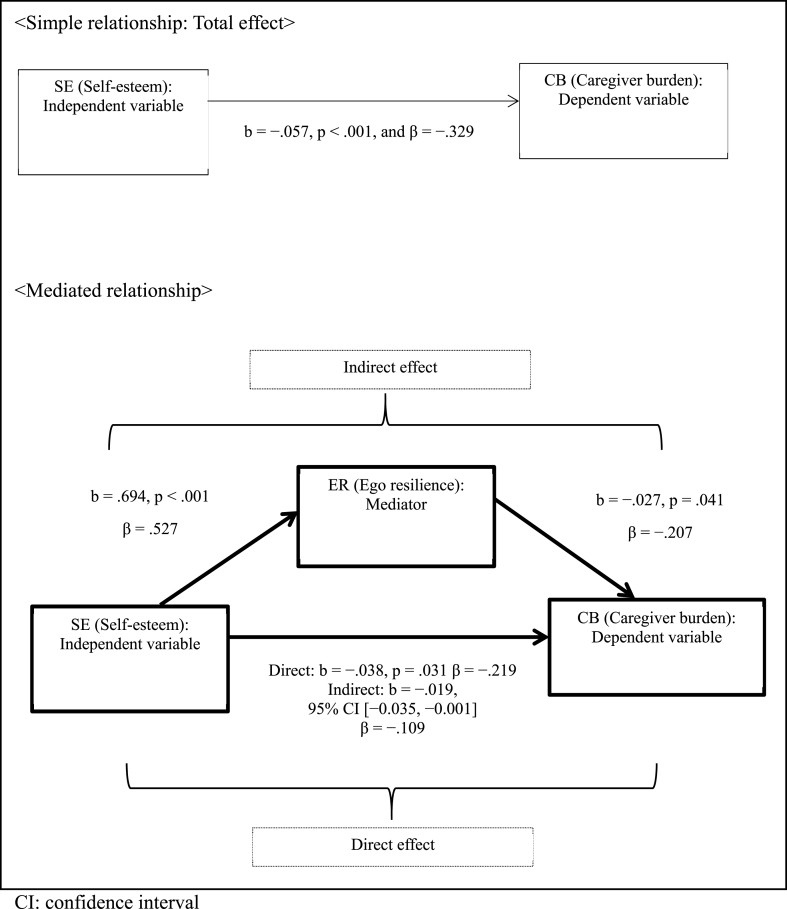
The results of our mediation analysis shown in Fig. 1 indicated that self-esteem had a significant indirect effect on caregiver burden through ego-resilience (b = −0.019, bias-corrected and accelerated bootstrapped CI [−0.035 and −0.001] based on 5000 samples) when we controlled for demographic characteristics and the diagnosis and frequency of pain or uncomfortable symptoms of the child. Self-esteem negatively predicted caregiver burden (β = −0.219 for direct effect and −0.329 for total effect, p < .05) and 26.4 % of the variance in caregiver burden. Moreover, self-esteem positively predicted ego-resilience (β = 0.527; p < .001) and explained 39.9 % of the variance in ego-resilience. The relationship between self-esteem and caregiver burden was partially mediated by ego-resilience, as shown by the statistical significance of both indirect and direct effects.
Fig. 1.
Model of self-esteem as a predictor of caregiver burden mediated by ego resilience. The confidence for the indirect effect represents a bias-corrected and accelerated bootstrapped CI based on 5000 samples.. (The covariates included were diagnosis of child and frequency of pain or uncomfortable symptoms, which were used as dummy variables.)
4. Discussion
The purpose of this study was to investigate the protective role of self-esteem and ego-resilience of family caregivers against burden on the family caregivers of children with hematologic and oncologic disease. According to our research, higher self-esteem among family caregivers is associated with less caregiver burden, and ego-resilience acts as a mediating factor between self-esteem and caregiver burden. The level of overall caregiver burden in the present study (M = 2.33) was higher than that in a previous study that used the same scale to assess individuals caring for chronically ill adult patients (M = 2.16) [23]. We hypothesize that parents have a stronger feeling of responsibility toward their children compared with caring a spouse or aging parents.
4.1. The role of ego-resilience for family caregivers
Our present findings show that ego-resilience mediates the relationship between self-esteem and caregiver burden, with higher self-esteem being related to lower level of caregiver burden. Ego-resilience has a role in helping caregivers in adjusting to and managing illness-related changes [15]. It has been demonstrated that caregivers with higher level of self-esteem had lower caregiver burden, improving their caregiver overall health [9]; in addition, self-esteem tends to promote the ego-resilience of family caregiver. Therefore, a family caregiver of children with hematologic and oncologic disease may experience less caregiver burden if they have both self-esteem and ego-resilience. Self-esteem and ego-resilience are positive, modifiable, and improvable aspects of an individual [14]. This may suggest that family caregivers of children with hematologic and oncologic disease have an advantage in their ability to recover from traumatic experiences, supporting their confidence that they can overcome their child's challenging situation.
Various interventions aimed at improving self-esteem and ego-resilience of family caregivers could be useful to further enhance these effects. One of the few interventions that promote and foster resilience within clinical settings for women who have breast cancer stress management and resilience training [31], which is a 12-week group-based cognitive behavioral therapy (CBT) program. This program reduces distress and anxiety symptoms and promotes resilience and well-being of patients and family caregivers. According to a study at Seattle Children's Hospital, one-on-one application of the Promoting Resilience in Stress Management for Parents (PRISM-P) [32], which is specifically targeted toward family caregivers of children with cancer, was significantly associated with improvements in resilience compared with the usual parent support care [32]. PRISM-P aims to enhance resilience among caregivers; in addition to reducing depression, anxiety, and stress, it also helps family caregivers to cope and find meaning in their child's care and increases emotional well-being of the family caregiver(s) and the child [32]. The various interventions that can be utilized to train patients and caregivers about resilience may promote self-esteem, hope, and optimism and allow such individuals to manage their burdens more efficiently. Therefore, healthcare professionals caring for children with hematologic and oncologic disease may be able to enhance the ego-resilience of family caregivers by conducting interventions that promote resilience, thereby improving the well-being of the families of children with hematologic and oncologic disease. In addition, family caregivers may be reluctant to participate in these interventions for themselves rather than focusing on their child care. Thus, in order to reduce attrition rate, researchers may need to make extra efforts, such as being deliberately flexible to encourage participation, scheduling intervention sessions in conjunction with planned hospital visits, making a phone call a week before intervention session for confirmation, and so on.
Emotional burden among caregivers of children with hematologic and oncologic disease. Out of the five subcategories of caregiver burden, in this study, financial burden received the highest score among family caregivers of adult patients [33] and children. Social burden was the lowest-scoring subcategory for caregivers of adult patients [33], whereas emotional burden was the lowest-scoring subcategory for family caregivers of children with cancer. In contrast to this study's findings, a previous study on emotional burden found that family caregivers of children with hematologic and oncologic disease experienced higher levels of emotional distress, including feelings of worry, guilt, and depression [34]. Family caregivers of pediatric patients, who are often their parents or mothers, experience severe emotional challenges from the moment of diagnosis due to fear of losing their child. Mothers, in particular, may experience social isolation because they think that interacting with others can worsen their child's illness [6]. In this study, we recruited the family caregivers from the outpatient department, which may indicate that their children's general condition is good enough to stay at home for the time being, compared with newly diagnosed children or admitted in the ICU or unit. This fact could explain why emotional burden received a lower overall score in this study than other types of burden.
Healthcare professionals can apply psychological interventions to potentially strengthen the affective bonds and levels of support and security between family caregivers and children with hematologic and oncologic disease [6]. For example, the implementation of interventions such as CBT, problem-solving skills training, and discussion therapy has demonstrated to lower distress, reduce anxiety, strengthen the sense of control, and improve the overall quality of life among family caregivers of children with leukemia [35,36].
Financial burden among family caregivers of children with hematologic and oncologic disease. Out of the five subcategories of caregiver burden, financial burden had the highest score among family caregivers of children with hematologic and oncologic disease, which suggests that these caregivers are highly concerned with medical costs. South Korea has the National Health Insurance, a universal healthcare system that provides every resident of South Korea with access to medical care [37]. Children with hematologic and oncologic disease, however, often have to receive medical services that are not covered by the National Health Insurance, such as chemotherapy, radiotherapy, chimeric antigen receptor T-cell (CAR T-cell) therapy, the usage of clofarabine and nelarabine, and other uninsured medical services [38,39]. In the CAR T-cell therapy, which was first approved by the US Food and Drug Administration in 2017 [[38], [39], [40]], the patient's T cells are genetically engineered so that they can directly kill cancer cells. This type of treatment has a high success rate and is now widely available in the USA and many other countries, but the median total cost of the treatment can exceed $300,000 (in the USA), which can put financial burden to family caregivers [40]. We also asked participants, in the current study, how many private health insurances they currently have, in addition to the National Health Insurance. Interestingly, almost all of them (92.6 %) responded that they had one or more private insurances. Some of the factors that draw family caregivers into private health insurances in South Korea More include a variety of plan options, relatively low premiums, and access to a wider range of advanced medical treatments [41]. Thus, family caregivers must be concerned about both private health insurances and out-of-pocket (OOP) expenses for medical services that are not covered by the National Health Insurance. OOP expenditure is the underlying source of private expenditure on health (PVEH), and PVEH is further amplified by subscribing to multiple private health insurances; this places more financial burden on family caregivers in South Korea [41].
According to previous research on healthcare expenditure for children with cancer, treatment for pediatric cancer requires higher medical expenses than that for adult cancer [42]. For instance, in Canada, which has a universal healthcare, the average OOP cost is $200 per adult patient per month and $800 per pediatric patient per month [43]. Medical service costs can also vary depending on the type of cancer; leukemia, which can affect children, has the highest medical service costs, followed by cancers of the bone and articular cartilage [5]. This is consistent with our results (Table 2), as the burden of family caregivers of children with leukemia had the highest median score than those with hematologic cancer and solid tumors.
5. Limitations
First, given the cross-sectional design and use of a self-report survey, it is not possible to assume causal relationships among family caregivers' self-esteem, ego-resilience, and caregiver burden. Additionally, the study did not examine whether the current negative situation and caregiver burden may have reduced the self-esteem of family caregivers. Thus, future research should examine caregiver burden using a longitudinal study design. Second, given that the participants were recruited from the outpatient setting, the family caregivers’ children with hematologic and oncologic disease may have had a relatively better health status than those undergoing active treatment. The results indicated this as low frequency of pain or uncomfortable symptoms. However, these subjective data were assessed by family caregivers and may not be the exact objective data indicating the severity of symptoms of children. Lastly, the data on time since treatment or intensity of treatment were not collected in this study, however, this might influence perceived caregiver burden. Thus, the overall level of caregiver burden may not be fully reflected in this study. Future studies should focus on ego-resilience and caregiver burden at different stages of cancer treatment, including late-stage cancer, with objective data on the severity of symptoms.
6. Conclusions
Family caregivers of children with hematologic and oncologic disease experience financial, physical, and emotional burdens. However, caregivers' self-esteem and ego-resilience may help to lessen these burdens. Family caregivers who have high self-esteem are expected to do better in overcoming the challenges they encounter when caring for their child with hematologic and oncologic disease. This effect is mediated by ego-resilience, with strong ego-resilience helping family caregivers maintain their well-being during difficult times. Therefore, healthcare professionals should consider each family caregiver's level of self-esteem and ego-resilience and help them maximize their inner resources by providing programs focused at fostering resilience among family caregivers.
Ethics statement
Written informed consent was obtained from all participants.
Funding
This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Government of Korea (MISP No. 2016R1C1B2013649) for study design and data collection, as well as a National Research Foundation of Korea (NRF) grant funded by the Government of Korea (MSIT No. 2020R1C1C1010602) for data analysis, manuscript development, and publication.
Data availability statement
The authors do not have permission to share data.
CRediT authorship contribution statement
Ji Yoon Kim: Writing – review & editing, Writing – original draft, Methodology, Data curation, Conceptualization. Bu Kyung Park: Writing – review & editing, Writing – original draft, Methodology, Investigation, Funding acquisition, Formal analysis, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Bu kyung park reports financial support was provided by National Research Foundation of Korea.
References
- 1.Zarit S.H., Reever K.E., Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. Gerontol. 1980;20(6):649–655. doi: 10.1093/geront/20.6.649. [DOI] [PubMed] [Google Scholar]
- 2.Utz R.L., Warner E.L. Caregiver burden among diverse caregivers. Cancer. 2022;128(10):1904–1906. doi: 10.1002/cncr.34171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roberto K.A., Savla J. Extended family caregivers for persons living with dementia. J. Fam. Nurs. 2022;28(4):396–407. doi: 10.1177/10748407221115455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Semere W., et al. Poor patient health is associated with higher caregiver burden for older adults with advanced cancer. Journal of Geriatric Oncology. 2021;12(5):771–778. doi: 10.1016/j.jgo.2021.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chae W., et al. The financial burden associated with medical costs among childhood cancer patients and their families related to their socioeconomic status: the perspective of national health insurance service. Int. J. Environ. Res. Publ. Health. 2020;17(17) doi: 10.3390/ijerph17176020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shattnawi K.K., et al. Caring for a child with cancer: experiences of Jordanian mothers. Clin. Nurs. Res. 2021;30(8):1144–1152. doi: 10.1177/10547738211002021. [DOI] [PubMed] [Google Scholar]
- 7.Rosenberg M. Academic Press; Orlando, FL: 1985. Self-concept and Psychological Well-Being in Adolescence. [Google Scholar]
- 8.Kim D. Relationships between caregiving stress, depression, and self-esteem in family caregivers of adults with a disability. Occup. Ther. Int. 2017;2017 doi: 10.1155/2017/1686143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang Y., et al. The association of self-esteem with caregiving demands, coping, burden, and health among caregivers of breast cancer patients: a structural equation modeling approach. Cancer Nurs. 2022;45(5):E820–E827. doi: 10.1097/NCC.0000000000001011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pudelewicz A., Talarska D., Bączyk G. Burden of caregivers of patients with Alzheimer's disease. Scand. J. Caring Sci. 2019;33(2):336–341. doi: 10.1111/scs.12626. [DOI] [PubMed] [Google Scholar]
- 11.Garmezy N. Resilience in children's adaptation to negative life events and stressed environments. Pediatr. Ann. 1991;20(9):459–460. doi: 10.3928/0090-4481-19910901-05. 463-460. [DOI] [PubMed] [Google Scholar]
- 12.Kermott C.A., et al. Is higher resilience predictive of lower stress and better mental health among corporate executives? PLoS One. 2019;14(6) doi: 10.1371/journal.pone.0218092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosa R., et al. Caregivers' resilience in mild and moderate Alzheimer's disease. Aging Ment. Health. 2020;24(2):250–258. doi: 10.1080/13607863.2018.1533520. [DOI] [PubMed] [Google Scholar]
- 14.Seiler A., Jenewein J. Resilience in cancer patients. Front. Psychiatr. 2019;10:208. doi: 10.3389/fpsyt.2019.00208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Palacio G.C., et al. Resilience in caregivers: a systematic review. Am J Hosp Palliat Care. 2020;37(8):648–658. doi: 10.1177/1049909119893977. [DOI] [PubMed] [Google Scholar]
- 16.Kim J.Y., Park B.K. The most important aspects for a good death: perspectives from parents of children with cancer. Inquiry. 2021;58 doi: 10.1177/00469580211028580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Piaget J. Routledge; London, UK: 1950. The Psychology of Intelligence. [Google Scholar]
- 18.Cook T.D., Campbell D.T., Shadish W. Houghton Mifflin; Boston: 2002. Experimental and Quasi-Experimental Designs for Generalized Causal Inference. [Google Scholar]
- 19.Block J., Kremen A.M. IQ and ego-resiliency: conceptual and empirical connections and separateness. J. Pers. Soc. Psychol. 1996;70(2):349. doi: 10.1037//0022-3514.70.2.349. [DOI] [PubMed] [Google Scholar]
- 20.Yoo S.K., Shim H.W. Psychological protective factors in resilient adolescents in Korea. The Korean Journal of Educational Psychology. 2002;16(4):189–206. [Google Scholar]
- 21.Rosenberg M. Princeton University Press; Princeton, NJ: 1965. Society and the Adolescent Self-Image. [Google Scholar]
- 22.Bae H.-N., et al. Reliability and validity of the Korean version of the Rosenberg self-esteem scale (K-rses) in adult. Mood Emot. 2014;12(1):43–49. [Google Scholar]
- 23.Suh M.H., Oh K.S. A study of well-being in caregivers caring for chronically ill family members. Journal of Korean Academy of Nursing. 1993;23(3):467–486. [Google Scholar]
- 24.Novak M., Guest C. Application of a multidimensional caregiver burden inventory. Gerontol. 1989;29(6):798–803. doi: 10.1093/geront/29.6.798. [DOI] [PubMed] [Google Scholar]
- 25.Oh K.-S., Chae S.-M., Cheon N.-Y. The reliability and validity of family burden questionnaire. Child Health Nursing Research. 2002;8(3):272–280. [Google Scholar]
- 26.Hayes A.F. vols. 507-xvii. Guilford Press. xvii; New York, NY, US: 2013. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; p. 507. [Google Scholar]
- 27.Baron R.M., Kenny D.A. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 28.Sobel M.E. Asymptotic confidence intervals for indirect effects in structural equation models. Socio. Methodol. 1982;13:290–312. [Google Scholar]
- 29.Cohen J. second ed. Erlbaum; Hillsdale: 1988. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- 30.Curran P.J., West S.G., Finch J.F. The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychol. Methods. 1996;1(1):16–29. [Google Scholar]
- 31.Loprinzi C.E., et al. Stress Management and Resilience Training (SMART) program to decrease stress and enhance resilience among breast cancer survivors: a pilot randomized clinical trial. Clin. Breast Cancer. 2011;11(6):364–368. doi: 10.1016/j.clbc.2011.06.008. [DOI] [PubMed] [Google Scholar]
- 32.Rosenberg A.R., et al. Effect of the promoting resilience in stress management intervention for parents of children with cancer (prism-P): a randomized clinical trial. JAMA Netw. Open. 2019;2(9) doi: 10.1001/jamanetworkopen.2019.11578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kang S.J., Lee H.J., Smi C.-K. Caregivers' Burden in patients with acute stroke. The Korean Journal of Rehabilitation Nursing. 2002;5(1):27–37. [Google Scholar]
- 34.Chodidjah S., Kongvattananon P., Liaw J.J. Changed our lives: psychosocial issues experienced by families of early adolescents with leukemia. Eur. J. Oncol. Nurs. 2022;56 doi: 10.1016/j.ejon.2021.102077. [DOI] [PubMed] [Google Scholar]
- 35.Koumarianou A., et al. A review of psychosocial interventions targeting families of children with cancer. Palliat. Support Care. 2021;19(1):103–118. doi: 10.1017/S1478951520000449. [DOI] [PubMed] [Google Scholar]
- 36.Asadi Noughabi F., et al. Effect of instructing care program through group discussion on the quality of life of the parents of the children afflicted with leukemia. Glob J Health Sci. 2015;8(5):197–204. doi: 10.5539/gjhs.v8n5p197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lee J.C. Health care reform in South Korea: success or failure? Am J Public Health. 2003;93(1):48–51. doi: 10.2105/ajph.93.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Neelapu S.S., et al. Axicabtagene ciloleucel CAR T-cell therapy in refractory large B-cell lymphoma. N. Engl. J. Med. 2017;377(26):2531–2544. doi: 10.1056/NEJMoa1707447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Maude S.L., et al. Tisagenlecleucel in children and young adults with B-cell lymphoblastic leukemia. N. Engl. J. Med. 2018;378(5):439–448. doi: 10.1056/NEJMoa1709866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Borgert R. Improving outcomes and mitigating costs associated with CAR T-cell therapy. Am. J. Manag. Care. 2021;27(13 Suppl):S253–S261. doi: 10.37765/ajmc.2021.88737. [DOI] [PubMed] [Google Scholar]
- 41.Shin J. Private health insurance in South Korea: an international comparison. Health Pol. 2012;108(1):76–85. doi: 10.1016/j.healthpol.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 42.Merrill C.T., Nagamine M., Hambrick M.M. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. 2006. Rockville (MD); 2005. Pediatric hospital stays for cancer. [Google Scholar]
- 43.Iragorri N., et al. The out-of-pocket cost burden of cancer care-A systematic literature review. Curr. Oncol. 2021;28(2):1216–1248. doi: 10.3390/curroncol28020117. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors do not have permission to share data.