INTRODUCTION
Many interactions occur between the immune, neural, and psychological systems. These interactions include communication pathways from the brain to the immune system, particularly the hypothalamic-pituitary-adrenal (HPA) axis and the autonomic nervous system, that mediate the influence of psychological variables, such as stress and emotions, on immunity and resistance to disease.1
In addition, when the body is confronted by pathogens, the immune system serves as a sensory organ, alerting the brain to the presence of infection-induced immune activation.2 The communication from the immune system to the brain is mediated by cytokines, which are peptides that orchestrate the immune response with a wide range of other biologic activities. During immune stimulation, cytokines such as interleukins and interferons are produced both in the periphery and in the brain, where they can affect neural, neuroendocrine, and behavioral functions through specific receptors.2,3
In addition to physiologic responses, such as fever, and hormonal responses, such as activation of the HPA axis, brain cytokines also produce behavioral changes. A person with a physical illness may show depressed mood, anorexia, weight loss, sleepiness and altered sleep patterns, fatigue and retardation of motor activity, reduced interest in the physical and social environment, and impaired cognitive abilities.3,4 During an acute infection, these behavioral symptoms, collectively termed “sickness behavior,” are considered to be an adaptive response, rather than due to the disease process itself and the fever that accompanies it. However, during chronic infections and other chronic medical conditions associated with intense immune activation, the sickness behavior syndrome can develop into a depressive episode. Illness-associated depression can cause high levels of distress in a sick person and may further complicate the existing physical symptoms and compliance with therapy.
In this review, I present the current knowledge on the role of cytokines in mediating the depressive symptoms that accompany various medical conditions. I also consider the possible use of antidepressant drugs—and their mechanism of action—in the treatment of illness-associated depression.
METHODS
This review is based on a MEDLINE search from 1966 to the present, using the search terms “physical disease,” “depression,” “cytokines,” and “antidepressants,” together with my own research and publications in the field.
Summary points
Cytokines are nonantibody proteins release by cells on contact with antigens and that act as intercellular mediators
During physical illness, the immune system serves as a sensory organ, communicating with the brain through the secretion of cytokines
An association exists between high cytokine levels and psychological disturbances, particularly depression
Experimental immune activation can lead to depressed mood and other psychological disturbances
Antidepressants can be used to prevent or treat illness-associated depression, possibly through their immunomodulatory effects
Depressive symptoms in physically ill patients may be a result of immune activation and cytokine secretion, rather than a psychological reaction to the distress and incapacitation induced by the illness
PHYSICAL DISEASE AND DEPRESSED MOOD
Depression is a common, disturbing concomitant of medical conditions. The reported prevalence of major depressive episodes in physically ill patients varies from 5% to more than 40%. However, because depression is often unrecognized and undertreated in sick patients, the prevalence reported in most studies is probably an underestimate.5
The high prevalence of depression in various medical conditions is reflected by the special psychiatric diagnosis of “depression due to a general medical condition.”6 To be diagnosed with this condition, “the clinician should establish the presence of a general medical condition and determine that the depression is etiologically related to the general medical condition through a physiological mechanism.”6(p367) Several lines of evidence suggest that this mechanism involves the immune system. In other words, the depression associated with various medical conditions is not merely a reaction to the incapacitation, pain, and losses that accompany the physical disease process, but may be directly caused by activation of the immune system.4,7
The evidence for illness-associated mood changes and a depressive symptom complex is mainly anecdotal, and few studies have examined these symptoms systematically. Experimentally induced viral infections (such as common cold and influenza) and the natural occurrence of upper respiratory tract illness or influenza8,9,10 produce depressed mood and other depressive symptoms, as well as various neuropsychological impairments. Similar disturbances have also been reported following chronic infections with herpesvirus, cytomegalovirus, Epstein-Barr virus, gastroenteritis, Borna disease virus, and human immunodeficiency virus.3,,
Table 1.
| Noninfectious conditions associated with chronic activation of the immune system and secretion of cytokines |
|---|
|
Table 2.
| Depressive symptoms caused by administration of cytokines to patients with cancer or hepatitis C |
|---|
|
Many noninfectious conditions are also associated with chronic activation of the immune system and secretion of cytokines (first box). Patients with these diseases have a high incidence of depression.4,11 Studies have shown that immune dysregulation precedes the development of depression. This suggests that illness-associated depression may be causally related to immune activation, rather than being a psychological reaction to the medical condition per se.
My colleagues and I have recently used a double-blind prospective design to investigate the immediate and prolonged psychological and physiologic effects of a specific viral infection in humans.12 The subjects were 240 teenaged girls who were vaccinated with live attenuated rubella virus. Based on an analysis of the levels of antibodies to rubella, subjects were divided into 2 groups: an experimental group comprising those who were initially seronegative and were infected following vaccination and a control group comprising those who were already immune to rubella before vaccination. Compared with control subjects, and their own baseline, subjects in the experimental group showed a significant rise in several standard measures of depressed mood, as well as an increased incidence of social and attention problems and delinquent behavior.12 These effects were particularly evident in girls from low, but not middle or high, socioeconomic status and could be predicted by personality traits measured at baseline.13 Thus, even a mild viral infection can produce a prolonged increase in depressive symptoms in vulnerable persons.
ROLE OF CYTOKINES IN ILLNESS-ASSOCIATED DEPRESSION
The best evidence for the involvement of cytokines in mediating the psychological effects of physical disease is that the exogenous administration of cytokines in patients with cancer or with hepatitis C produces marked psychological and neuroendocrine symptoms that are similar to those induced by viral infection.
The administration of cytokines (interferon alfa, interleukin [IL] 2, or tumor necrosis factor [TNF]α) causes flulike and depressive symptoms (second box).14 The fact that these symptoms appear almost immediately after cytokine administration and usually disappear shortly after termination of the cytokine treatment strongly suggests a causal role for cytokines in producing the depressive symptoms.
Table 3.
| Conditions associated with depression in which depressive symptoms respond to antidepressants |
|---|
|
To further examine the role of cytokines in the psychological alterations that accompany infection and inflammation, my colleagues and I recently studied the effects of lipopolysaccharide (LPS) on affective and cognitive variables in healthy volunteers.15 The administration of a low dose of purified LPS (the major cell wall component of gram-negative bacteria) is the most established and frequently used experimental model for safely and accurately assessing the initial host response to infection in humans. We used a crossover design, in which each subject completed a battery of psychological and neuropsychological tests at various times following LPS injection on 1 day and following the administration of saline solution on another day. We used a double-blind design, in which neither the experimenter nor the subject knew the group assignment. LPS had no effect on physical sickness symptoms, blood pressure, or heart rate, but it caused a mild increase in temperature and markedly elevated the circulating levels of many cytokines and cortisol. Following LPS administration, the subjects showed a transient substantial increase in levels of anxiety and depressed mood. In addition, verbal and nonverbal memory functions were substantially impaired.
Significant positive correlations were found between the secretion of specific cytokines (such as IL-6 and TNFα) and LPS-induced depressed mood and anxiety and the severity of memory impairments.15 The findings suggest that in humans, a mild stimulation of the primary host defense—that does not induce subjective symptoms of physical sickness—is associated with emotional and cognitive disturbances, which may be caused by cytokine release.
Studies in animals provide more direct evidence for the role of cytokines in mediating the behavioral effects of various pathogens. As found in humans, both infectious and noninfectious diseases in animals are associated with anorexia and weight loss; hypersomnia; psychomotor retardation; fatigue; anhedonia; and impaired cognitive abilities, exploration, and social behavior.2,3,11 Similar sickness behavior symptoms can be observed following the exogenous administration of cytokines (particularly IL-1β and TNFα), either in the periphery or directly into the brain.4,11,16 Moreover, the behavioral effects of immune challenges can be attenuated by pretreatment with cytokine synthesis blockers and cytokine antagonists, as well as by the manipulation of cytokine genes.4,11,16
ANTIDEPRESSANTS REDUCE ILLNESS-ASSOCIATED DEPRESSION
Antidepressant medication has been used successfully in treating depressive symptoms associated with medical illness.5 Both tricyclic antidepressant medications and selective serotonin-reuptake inhibitors are of proven value in treating depression associated with a wide range of conditions (third box).17,18,19,20,21
Antidepressants have been shown to have many immunomodulatory effects. In vitro, exposure to antidepressants is mainly immunosuppressive, particularly with respect to cytokine secretion from human immune cells.22,23,24,25 In depressed patients, antidepressants may also have immunomodulatory effects. Studies have shown conflicting results—long-term treatment with antidepressant medication has been associated with the suppression of immune function and cytokine secretion, an increase in cytokine production, or no effect on cytokine levels.26
To further elucidate the relationship between immune activation and depression and to explore the mechanisms underlying the therapeutic action of antidepressants, we used an experimental animal model. Specifically, we examined the effects of antidepressants on LPS-induced behavioral and neuroendocrine alterations in rats.27 We showed that long-term but not initial administration of imipramine or fluoxetine attenuated or completely abolished LPS-induced sickness behavior as well as some of the physiologic and neuroendocrine effects of LPS.11,27
In a recent study, this procedure has been adopted for the treatment of cytokine-induced depression in humans. In a double-blind, placebo-controlled design, patients were pretreated with the antidepressant, paroxetine, or placebo for 2 weeks before the initiation of long-term highdose interferon therapy for malignant melanoma.28 Most patients receiving placebo met the criteria for major depression or had to discontinue interferon because of toxic reactions before 3 months. In contrast, less than a third of the patients receiving paroxetine developed depression, and no patients taking paroxetine had dropped out of treatment, representing a statistically significant improvement in morbidity and compliance. Together, these data indicate that antidepressants provide useful treatment and prophylaxis against the development of illness-associated mood disorders.
CONCLUSION
Accumulating evidence indicates that immune activation during various medical conditions is associated with a depressive syndrome. Taken together with the reports that brain cytokines influence the neurochemical systems involved in depression,11 these findings support the hypothesis that immune activation, through the release of cytokines, is involved in the cause and symptoms of illness-associated depression. Antidepressants have effective protective and therapeutic effects on illness- and cytokine-mediated depressive episodes. Future research should examine the effects of cytokine-synthesis blockers and antagonists on mood disorders associated with medical conditions.
Figure 1.
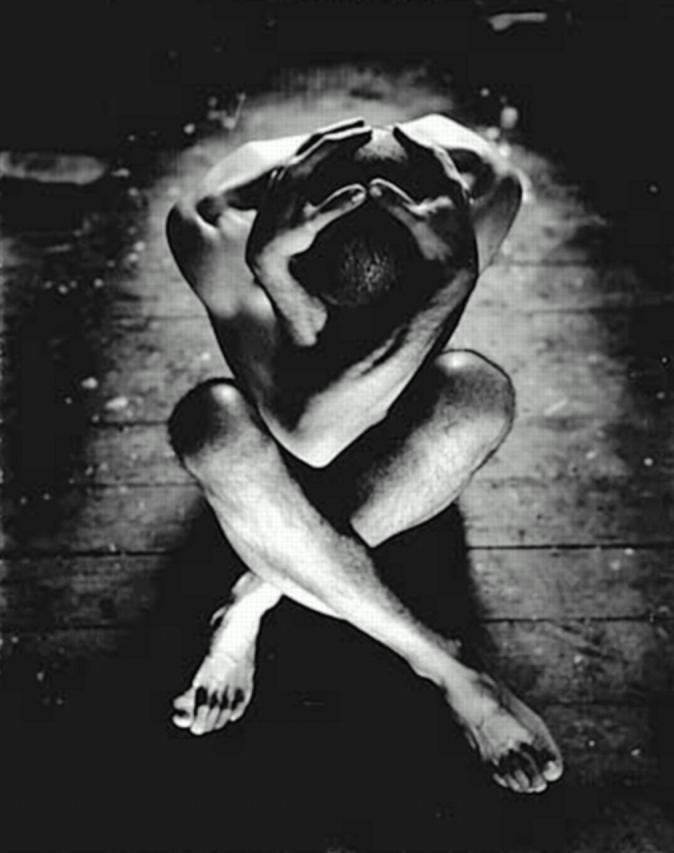
Depression may be due to immune activation
© Trevillion Picture Library, London
Competing interests: None declared
Funding: Supported by grant 94-204 from the United-States-Israel Binational Science Foundation, the German-Israeli Foundation for Research and Development, and the Eric Roland Center for Neurodegenerative Diseases.
References
- 1.Ader R, Cohen N, Felten D. Psychoneuroimmunology: interactions between the nervous system and the immune system. Lancet 1995;345: 99-103. [DOI] [PubMed] [Google Scholar]
- 2.Maier SF, Watkins LW. Implications of immune-to-brain communication for sickness and pain. Proc Natl Acad Sci U S A 1999;96: 7710-7713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dantzer R, Aubert A, Bluthe RM, et al. Mechanisms of the effects of cytokines. In: Dantzer R, Wollman EE, Yirmiya R, eds. Cytokines, Stress and Depression. New York: Kluwer Academic/Plenum Publishers; 1999: 83-106.
- 4.Yirmiya R. Behavioral and psychological effects of immune activation: implications for “depression due to a general medical condition.” Curr Opin Psychiatry 1997;10: 470-476. [Google Scholar]
- 5.Katon W, Sullivan MD. Depression and chronic medical illness. J Clin Psychiatry 1990;51(suppl): 3-11. [PubMed] [Google Scholar]
- 6.Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994.
- 7.Dantzer R, Wollman E, Vitkovic L, Yirmiya R. Cytokines and depression: fortuitous or causative association? Mol Psychiatry 1999;4: 328-332. [DOI] [PubMed] [Google Scholar]
- 8.Hall S, Smith AP. Investigation of the effects and aftereffects of naturally occurring upper respiratory tract illnesses on mood and performance. Physiol Behav 1996;59: 569-577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith A, Thomas M, Kent J, Nicholson K. Effects of the common cold on mood and performance. Psychoneuroendocrinology 1998;23: 733-739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Capuron L, Lamarque D, Dantzer R, Goodall G. Attentional and mnemonic deficit associated with infectious disease in humans. Psychol Med 1999;29: 291-297. [DOI] [PubMed] [Google Scholar]
- 11.Yirmiya R, Weidenfeld J, Pollak Y, et al. Cytokines, “depression due to a general medical condition,” and antidepressant drugs. In: Dantzer R, Wollman EE, Yirmiya R, eds. Cytokines, Stress and Depression. New York: Kluwer Academic/Plenum Publishers; 1999: 283-316. [DOI] [PubMed]
- 12.Morag M, Yirmiya R, Lerer B, Morag A. Influence of socioeconomic status on behavioral, emotional and cognitive effects of rubella vaccination: a prospective, double blind study. Psychoneuroendocrinology 1998;23: 337-351. [DOI] [PubMed] [Google Scholar]
- 13.Morag M, Morag A, Reichenberg A, Lerer B, Yirmiya R. Psychological variables as predictors of rubella antibody titers and fatigue: a prospective, double blind study. J Psychiatr Res 1999;33: 389-395. [DOI] [PubMed] [Google Scholar]
- 14.Meyers CA. Mood and cognitive disorders in cancer patients receiving cytokine therapy. In: Dantzer R, Wollman EE, Yirmiya R, eds. Cytokines, Stress and Depression. New York: Kluwer Academic/Plenum Publishers; 1999: 75-81. [DOI] [PubMed]
- 15.Reichenberg A, Yirmiya R, Schuld A, et al. Cytokine-associated emotional and cognitive disturbances in humans. Arch Gen Psychiatry, in press. [DOI] [PubMed]
- 16.Anisman H, Merali Z. Anhedonic and anxiogenic effects of cytokine exposure. In: Dantzer R, Wollman EE, Yirmiya R, eds. Cytokines, Stress and Depression. New York: Kluwer Academic/Plenum Publishers; 1999: 199-233 [DOI] [PubMed]
- 17.Schiffer RB, Wineman NM. Antidepressant pharmacotherapy of depression associated with multiple sclerosis. Am J Psychiatry 1990;147: 1493-1497. [DOI] [PubMed] [Google Scholar]
- 18.Lauritzen L, Bendsen BB, Vilmar T, Bendsen EB, Lunde M, Bech P. Post-stroke depression: combined treatment with imipramine or desipramine and mianserin: a controlled clinical study. Psychopharmacology (Berl) 1994;114: 119-122. [DOI] [PubMed] [Google Scholar]
- 19.Gottfries CG. Recognition and management of depression in the elderly. Int Clin Psychopharmacol 1997;12(suppl): S31-S36. [DOI] [PubMed] [Google Scholar]
- 20.van Heeringen K, Zivkov M. Pharmacological treatment of depression in cancer patients: a placebo-controlled study of mianserin. Br J Psychiatry 1996;169: 440-443. [DOI] [PubMed] [Google Scholar]
- 21.Rabkin JG, Wagner G, Rabkin R. Effects of sertraline on mood and immune status in patients with major depression and HIV illness: an open trial. J Clin Psychiatry 1994;55: 433-439. [PubMed] [Google Scholar]
- 22.Levenson JL, Fallon HJ. Fluoxetine treatment of depression caused by interferon-alpha. Am J Gastroenterol 1993;88: 760-761. [PubMed] [Google Scholar]
- 23.Xia Z, DePierre JW, Nassberger L. Tricyclic antidepressants inhibit IL-6, IL-1β and TNF-α release in human blood monocytes and IL-2 and interferon-γ in T cells. Immunopharmacology 1996;34: 27-37. [DOI] [PubMed] [Google Scholar]
- 24.Sommer N, Loschmann PA, Northoff GH, et al. The antidepressant rolipram suppresses cytokine production and prevents autoimmune encephalomyelitis. Nat Med 1995;1: 244-248. [DOI] [PubMed] [Google Scholar]
- 25.Maes M, Song C, Lin AH, et al. Negative immunoregulatory effects of antidepressants: inhibition of interferon-gamma and stimulation of interleukin-10 secretion. Neuropsychopharmacology 1999;20: 370-379. [DOI] [PubMed] [Google Scholar]
- 26.Neveu P, Castanon N. Is there evidence for an effect of antidepressant drugs on immune function? In: Dantzer R, Wollman EE, Yirmiya R, eds. Cytokines, Stress and Depression. New York: Kluwer Academic/Plenum Publishers; 1999: 267-281.
- 27.Yirmiya R. Endotoxin produces a depressive-like syndrome in rats. Brain Res 1996;711: 163-174. [DOI] [PubMed] [Google Scholar]
- 28.Miller A, Musselman D, Penna S, et al. Pretreatment with the antidepressant paroxetine prevents cytokine-induced depression during IFN-alpha therapy for malignant melanoma. Neuroimmunomodulation 1999;6: 237. [Google Scholar]


