PROVIDER SHORTAGES IN RURAL AMERICA
Many rural Americans have limited access to health care. This problem stems from 2 characteristics of the health care system: the many Americans without health care insurance and the tendency of health care professionals to locate and practice in relatively affluent urban and suburban areas.
The relative shortage of physicians in rural areas of the United States is 1 of the few constants in any description of the US medical care system. About 20% of the US population—more than 50 million people—live in rural areas, but only 9% of the nation's physicians practice in rural communities.1
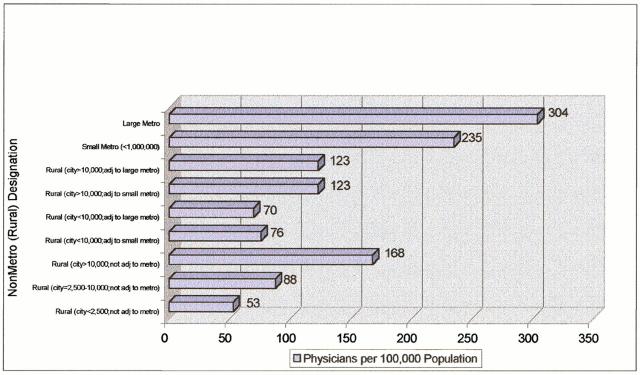
Crude comparisons of the physician-to-population ratio in rural versus urban areas can be extremely misleading and provide almost no information about whether shortages or surpluses exist in either location.2 In 1995—the latest year for which data are available—gaps existed between the supply of active physicians in counties of different size (figure 1). As can be seen in this figure, major differences persist between the aggregate supply in urban and rural areas, with the larger counties having many more physicians per 100,000 population.
Figure 1.
Active physicians per 100,000 population by location, 1995. From AMA from BHPr ARF data, 1997.
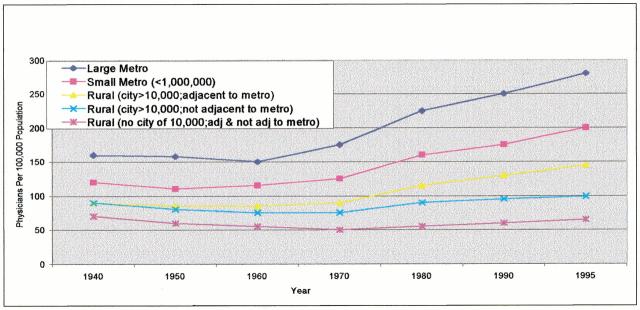
But this information obscures the fact that the physician supply has grown in rural areas in the past 20 years, although the growth has not been uniform. The supply of rural physicians has increased modestly in the past few decades, with most of the increase in the larger rural communities adjacent to metropolitan areas (figure 2). Rural supply lags far behind the current urban supply of physicians, but the urban supply of physicians is, in the opinion of many, excessive.
Figure 2.
Active physicians per 100,000 population by year and location, 1940 through 1995. From AMA from BHPr ARF data, 1997.
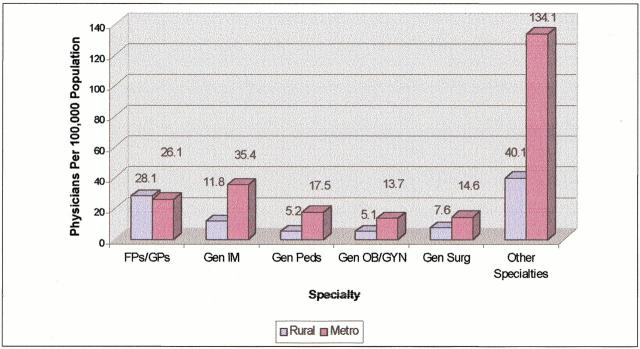
Physician supply in rural areas is closely tied to the specialty mix of American physicians. Specialty has a powerful effect on physician location choice for each of the major specialty groups (figure 3). Family physicians distribute themselves in proportion to the population in both rural and urban locations and are the largest single source of physicians in rural areas. All other specialties are much more likely to settle in urban areas.
Figure 3.
Patient care physicians per 100,000 population by location and specialty, 1995. From AMA from BHPr ARF data, 1997.
Given the expansion of the rural physician supply, it is important to distinguish between rural areas that have definite shortages of critical health professionals and those that have fewer health professionals relative to oversupplied urban areas. Historically, the government has designated areas as seriously underserved based on the physician-to-population ratio within a specific health service area. Populations with too few physicians have been categorized as health professional shortage areas, thus becoming eligible for a broad array of governmental assistance.
Summary points
There is a relative shortage of physicians in rural areas of America
The more highly specialized the physician, the less likely he or she will settle in a rural area
The preference of women for urban practice may pose a problem for the future recruitment of rural physicians
Although managed care systems can recruit physicians to rural areas, systems are growing slowly in rural areas and their doctors may be of little use to the working poor who have neither Medicaid nor conventional health insurance
Possible solutions to the problem of physician shortages in rural areas include changing the medical education system so that it trains more physicians who choose rural practice, changing the reimbursement strategies of Medicare and Medicaid, and changing the existing federal and state programs
EFFECT OF SPECIALTY CHOICE AND DISTRIBUTION
Nothing affects the location decision of physicians more than specialty. The more highly specialized the physician, the less likely he or she will settle in a rural area. As a consequence, the growth of specialization is a major contributor to the geographic maldistribution of physicians. Many of the shortages in communities with fewer than 10,000 residents could have been reduced or eliminated if even a small fraction of subspecialists produced over the past 15 years had chosen to become primary care physicians in rural or underserved areas (T R Konrad: “Shortages of Physicians and Other Health Professionals in Rural Areas: Background Paper Produced for COGME”; Cecil G Sheps Center for Health Services Research, University of North Carolina at Chapel Hill, unpublished, 1997).
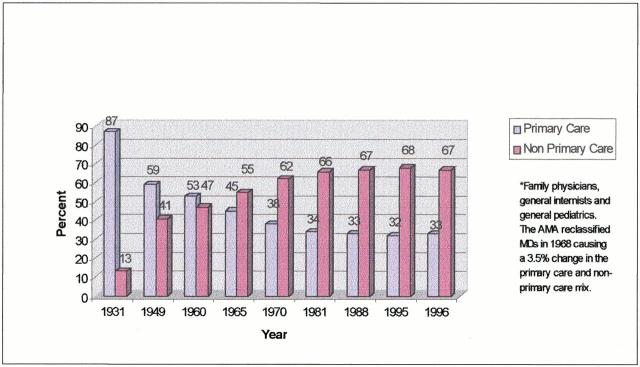
The recently revived interest in family medicine and the other generalist disciplines is a major factor in addressing rural geographic maldistribution. The decreasing proportion of generalist physicians leveled off in the 1980s (figure 4).3 Despite recently increased interest in primary care, the percentage in generalist disciplines has not yet shown a substantial increase. An improvement in the balance of generalists and specialists is a necessary precondition for eliminating rural physician shortages.
Figure 4.
Percentage of primary care and non-primary care physicians for selected years, 1931 through 1996. From AMA from BHPr ARF data, 1997.
EFFECT OF GENDER ON CHOICE OF PRACTICE LOCATION
Starting a decade ago, the proportion of women attending medical school increased rapidly. The number of female physicians in the United States more than quadrupled between 1970 and 1991 and has continued to rise.4
Historically, rural medical care was almost exclusively provided by male physicians. This was a product of the paucity of women in medicine and the tendency of the few female graduates to locate in urban areas. Male generalist physicians far outnumber their female counterparts in rural areas across the United States. As the proportion of women in medical schools has increased, there have been concerns that the supply of rural physicians might dwindle if women continue to settle almost exclusively in urban areas and the largest rural cities.
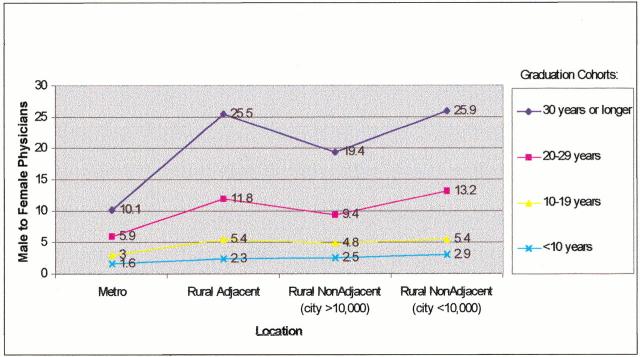
Recent work suggests that the disparity between male and female physicians may be growing less acute with time.5 The gap between male and female family physicians has narrowed dramatically for more recent graduates (figure 5). Still, even women in the most recent graduate cohort are much less likely than their male counterparts to locate in rural areas, and the disparity is greatest for the smaller and more remote communities. The continuing preference of women for urban practice—even though less pronounced than in earlier years—may still pose a problem for the future recruitment of rural physicians.
Figure 5.
Male to female family or general physicians by graduation cohort, 1997. From Ellsbury KE, Doescher MP, Hart LG. US medical schools and the rural family physician gender gap. Fam Med 2000;32:331-337.
INFLUENCE OF MANAGED CARE
Managed care is a major emerging influence on the delivery of rural health care. Although it has become dominant in many urban areas, its effect in rural areas is just beginning to be felt. More than 80% of all rural counties were in the service area of at least 1 health maintenance organization (HMO) by the end of 1995, although the percentage of the rural population enrolled in HMOs is estimated to be less than 8%.6 Managed care is not only a creature of the private sector; nationally, about a tenth of rural Medicaid recipients are enrolled in Medicaid HMOs and prepaid plans, and the number is increasing rapidly.
Managed care is a 2-edged sword, both with regard to geographic maldistribution and rural medical underservice. Managed care networks have the potential to provide organizational vehicles for hiring and deploying physicians in areas that could not support independent physicians on their own.
But there are 2 potentially adverse effects of managed care systems on rural health: the loss of local control of health care systems and the reluctance of private managed care systems to provide care to the uninsured. Most managed care systems are sponsored by large metropolitan organizations, and these entities may have little understanding of or empathy for isolated rural areas. The presence of physicians hired through vertically integrated systems may mean that the community has health professionals, but they may be of little use to the working poor who have neither Medicaid nor conventional health insurance. The managed care industry is in rapid flux, and the extent to which managed care will ultimately dominate rural areas as it has dominated some urban ones is difficult to predict.
POSSIBLE SOLUTIONS TO THE PROBLEM OF INEQUITIES IN RURAL HEALTH
Educational initiatives
One of the most powerful ways to remedy problems of rural geographic maldistribution is to change the medical education system so that it selects, trains, and deploys more health care workers who choose to practice in rural areas. Much of the federal support incorporated within the Title VII programs—the major federal vehicle for generalist training—is based on the premise that this is an achievable goal. Talley has discussed the 4 basic “truths” about rural health3:
Students with rural origins are more likely to train in primary care and return to rural areas,
Residents trained in rural areas are more likely to choose to practice in rural areas,
Family medicine is the key discipline of rural health care, and
Residents practice close to where they train.
To the extent that these relationships are accurate—and evidence supports associations between these characteristics and the decision to practice in rural areas—modifications of the training milieu to incorporate these factors make sense.
The advantage of this approach is that it takes optimum advantage of free-market solutions to the problem of geographic physician maldistribution. Rather than requiring the establishment of federal or state delivery systems that may be controversial, complex, and expensive, graduating residents gravitate to underserved areas to fill their personal desires.
Although this type of intervention does not lend itself to controlled experiments, ample evidence exists that such an approach works. Publicly owned medical schools in rural states, particularly those that see their mission as training future family physicians, have high proportions of their graduating classes ultimately practicing in rural areas. By contrast, research-intensive private schools in metropolitan areas with no commitment to family medicine have virtually no rural graduates.4
Changes in reimbursement strategies of Medicare and Medicaid
A powerful mechanism to improve the flow of health professionals to rural areas is the use of targeted incentives. Central to this approach is the belief that physicians and others act as rational economic beings. If some form of economic inducement enhances the reimbursement for rural services, then physicians are more likely to locate in these areas. This approach has been used with some success in Britain, Canada, and Australia, where a variety of bonuses increase reimbursement for selected rural practitioners.
Changes in existing direct federal and state programs
When educational interventions and economic incentives fail to remedy geographic maldistribution, the major recourse is the creation of programs that provide direct services to underserved areas. There are numerous examples of such programs, the largest of which are the community health centers and the National Health Service Corps (NHSC). There is no question that these 2 federal programs remain the preeminent safety net programs for rural America. Studies by the Rural Health Research Centers in Chapel Hill, NC, and Seattle demonstrate that about 1 in 4 of every new primary care physician entering a health professional shortage area in the late 1980s was placed there under NHSC auspices7 and that 1 in 5 physicians practicing independently in many of the smallest rural communities was initially brought to those areas through their service in the NHSC.8,
Table 1.
| Key factors in improving the delivery of telemedicine to rural areas |
|---|
|
Given the realities of the current system, future efforts should concentrate on improving the fit between need and services, enhanced coordination—and reduced duplication—of services provided, better identification of students to ultimately serve in the NHSC and state programs, and improved effectiveness and efficiency of governmentally sponsored health care services, including those of rural health clinics.9 The wide variety of programs available—and the natural variability in the way they are organized and administered—leads to enormous complexity in the provision of services. It is certainly worth the effort to simplify programs and their administration and to ensure that governmental resources follow human need, not the administrative prowess of officials who excel at the bureaucratic skills that can obtain these services for their communities.
New technologies: possible effect of telemedicine
Telemedicine is an emerging technology with enormous potential for mitigating the effects of the geographic maldistribution of health professionals. Although telemedicine has a legitimate, important, and growing role in rural medicine,10 the path to the future is uncertain. As pointed out in the 2nd Invitational Consensus Conference on Telemedicine and the National Information Infrastructure, multiple and significant obstacles exist that make the current efforts uncoordinated, expensive, inaccessible, and at times even illegal.11
The current state of telemedicine could be characterized as creative but relatively unstructured, with a wide variety of public and private sector experiments proceeding simultaneously. Some applications, such as reading electrocardiograms at a distance, have become common-place. Others, such as dermatology consultations, are being performed in many different places but without standard protocols for transmission, interaction, evaluation, or charging. And others, such as doing an appendectomy at a distance, remain in the realm of science fiction, if just barely. From the standpoint of geographic maldistribution, there are 3 key issues (see box).
CONCLUSIONS
Geographic maldistribution of health providers is 1 of the most deep-seated characteristics of the American health care system. Even though the 1990s have been marked by rapid expansion in the absolute and relative number of practicing physicians, substantial rural shortages have persisted. Rural areas will continue to have structural barriers that will require special programs to assist in the training, deployment, and support of health professionals.
Figure a.

© Douglas Diekema
Figure b.

© Douglas Diekema
Competing interests: None declared
This article is adapted, with permission, from Ricketts III TC: Rural Health in the United States. New York: Oxford University Press; 1999.
References
- 1.Bureau of Health Professions. Rural Health Professions Facts: Supply and Distribution of Health Professions in Rural America. Rockville, MD: Health Resources and Services Administration; 1992.
- 2.Center for the Evaluative Clinical Sciences, Dartmouth Medical School. The Dartmouth Atlas of Health Care. Chicago: American Hospital Publishing; 1996. [PubMed]
- 3.Talley RC. Graduate medical education and rural health care. Acad Med 1990;65: 522-525. [DOI] [PubMed] [Google Scholar]
- 4.Rosenblatt RA, Whitcomb ME, Cullen TJ, Lishner DM, Hart LG. Which medical schools produce rural physicians? JAMA 1992;268: 1559-1565. [PubMed] [Google Scholar]
- 5.Doescher MP, Ellsbury KE, Hart LG. The distribution of rural female generalist physicians in the United States. J Rural Health 2000;16: 111-118. [DOI] [PubMed] [Google Scholar]
- 6.Casey MM. Rural managed care. In: Ricketts TC III, ed. Rural Health in the United States. New York: Oxford University Press; 1999: 113-118.
- 7.Konrad TR. The Rural HPSA Physician Retention Study: Final Report for Grant No. RO HS 06544-0 from Agency for Health Care Policy and Research. Chapel Hill, NC: Cecil G Sheps Center for Health Services Research, University of North Carolina; 1994.
- 8.Cullen TJ, Hart LG, Whitcomb ME, Lishner DM, Rosenblatt RA. The National Health Service Corps: rural physician service and retention. J Am Board Fam Pract 1997;10: 272-279. [PubMed] [Google Scholar]
- 9.Rural Health Clinics: Rising Program Expenditures Not Focused on Improving Care in Isolated Areas. Washington, DC: General Accounting Office; 1996. GAO/HEHS-97-24.
- 10.Balas EA, Jaffrey F, Kuperman GJ, et al. Electronic communication with patients: evaluation of distance medicine technology. JAMA 1997;278: 152-158. [PubMed] [Google Scholar]
- 11.Bashshur RL, Puskin D, Silva J. Telemedicine and the national information infrastructure. Telemed J 1995;1: 321-375. [PubMed] [Google Scholar]