Abstract
Objective
This study aimed to investigate the association between heart failure (HF) severity measured based on brain natriuretic peptide (BNP) levels and future bleeding events after percutaneous coronary intervention (PCI).
Background
The Academic Research Consortium for High Bleeding Risk presents a bleeding risk assessment for antithrombotic therapy in patients after PCI. HF is a risk factor for bleeding in Japanese patients.
Methods
Using an electronic medical record-based database with seven tertiary hospitals in Japan, this retrospective study included 7160 patients who underwent PCI between April 2014 and March 2020 and who completed a 3-year follow-up and were divided into three groups: no HF, HF with high BNP level and HF with low BNP level. The primary outcome was bleeding events according to the Global Use of Streptokinase and t-PA for Occluded Coronary Arteries classification of moderate and severe bleeding. The secondary outcome was major adverse cardiovascular events (MACE). Furthermore, thrombogenicity was measured using the Total Thrombus-Formation Analysis System (T-TAS) in 536 consecutive patients undergoing PCI between August 2013 and March 2017 at Kumamoto University Hospital.
Results
Multivariate Cox regression showed that HF with high BNP level was significantly associated with bleeding events, MACE and all-cause death. In the T-TAS measurement, the thrombogenicity was lower in patients with HF with high BNP levels than in those without HF and with HF with low BNP levels.
Conclusions
HF with high BNP level is associated with future bleeding events, suggesting that bleeding risk might differ depending on HF severity.
Keywords: heart failure, percutaneous coronary intervention, biomarkers
WHAT IS ALREADY KNOWN ON THIS TOPIC
Heart failure (HF) is a risk factor for high bleeding (HBR) after percutaneous coronary intervention (PCI).
So far, little is known if the severity of HF and future bleeding events after PCI are associated.
WHAT THIS STUDY ADDS
HF with high brain natriuretic peptide (BNP) levels (≥100 pg/mL) is independent of HBR, and its thrombogenicity also supports this association.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
In patients with severe HF under PCI, it is necessary to consider HBR and choose appropriate antithrombotic therapy.
Introduction
Dual antiplatelet therapy (DAPT) is the standard of care for ischaemic heart disease (IHD) following percutaneous coronary intervention (PCI). Long-term DAPT causes significant haemorrhagic complications.1 2 Therefore, selection of appropriate antithrombotic therapy, including DAPT duration, by stratification of bleeding risk is required. The Academic Research Consortium (ARC) has developed a consensus document, the ARC-high bleeding risk (HBR) evaluation criteria, as a common definition of HBR in patients undergoing PCI.3 4 Furthermore, low body weight; frailty; chronic kidney disease (CKD), including dialysis; heart failure (HF) and peripheral vascular disease, which are not included in the ARC-HBR, were identified as important patient characteristics for HBR in a Japanese cohort study.5–8 Therefore, Japan-HBR, which adds these four factors to the ARC-HBR, has been proposed in Japan.9 However, whether the phenotype (left ventricular function or severity) of HF is associated with HBR remains unknown.
Total Thrombus-Formation Analysis System (T-TAS (Fujimori Kogyo, Tokyo, Japan)), a microchip-based flow chamber system used to evaluate whole-blood thrombogenicity, was developed as an easy-to-use system to quantitatively analyse thrombus formation.10 11 Previous studies have demonstrated the usefulness of the T-TAS parameter in predicting 1-year bleeding events in patients undergoing PCI and a significant predictor of procedural bleeding events in patients undergoing catheter ablation for atrial fibrillation (AF).12 13 However, whether the phenotype of HF is associated with thrombogenicity remains unknown.
This study aimed to investigate the association between HF severity measured based on BNP levels and future bleeding events after PCI using a large-scale, multicentre cohort database, the Clinical Deep Data Accumulation System (CLIDAS) database in Japan and then investigate the association between the whole-blood thrombogenicity measured by the T-TAS and phenotype of HF in patients undergoing PCI at Kumamoto University Hospital.
Methods
Database
The CLIDAS, a multicentre database with seven tertiary medical hospitals in Japan, was developed to collect data directly for oral medicine, injection drugs, laboratory tests, physiological tests, echocardiographic parameters, ECGs, cardiac catheterisations and PCI treatments in electronic medical records using Standardised Structured Medical Information eXchange Extended Storage and patient characteristics and long-term prognosis by each hospital data manager.14 15 The CLIDAS was developed from the Japan Ischaemic Heart Disease Multimodal Prospective Data Acquisition for preCision Treatment project and aimed to build a clinical data registry system that electronically collects medical records and multimodal data, including coronary angiography and PCI report.15 16
Study population
In total, 9690 consecutive patients who were admitted for diagnosis or treatment of IHD at a CLIDAS-accredited facility and underwent PCI between April 2013 and March 2019 were screened in this study. After excluding 2530 patients with missing data for prior HF and BNP levels within 30 days of index PCI or who were lost to follow-up, the remaining 7160 patients were enrolled in this study. The patients were divided into two groups: non-HF (n=6645) and HF (n=515). We defined a history of HF as a prior hospitalisation for HF.
Furthermore, patients with HF were reclassified based on (1) BNP level, (2) left ventricular ejection fraction (LVEF) and (3) aetiology: (1) HF with low BNP level (<100 pg/mL) (n=131) and HF with high BNP level (≥100 pg/mL) (n=384) and (2) HF with reduced EF (<40%) (n=177), with HF with mild reduced EF (40%–49%) (n=109), with preserved EF (≥50%) (n=186) and with unknown EF (n=43). Regarding aetiology, CLIDAS allows us to assess the medical history of old myocardial infarction (OMI), previous PCI and previous CABG. We defined patients with HF with a history of OMI, PCI or CABG as ischaemic HF (n=239), and we defined patients with HF without these histories as non-ischaemic HF (n=276) (online supplemental figure 1).
openhrt-2023-002489supp001.pdf (175.5KB, pdf)
Patient involvement
Patients were not involved in setting the research question, the outcome measures and intimately involved in design and analysis.
Variables
BNP values were obtained from the lowest value 30 days before and after the index PCI. Other baseline laboratory data were calculated as average values from 60 days before the index PCI to 30 days after the procedure. Hypertension was defined as systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg or medical treatment for hypertension at index PCI.17 Diabetes mellitus (DM) was defined as a haemoglobin A1C level ≥6.5%, casual blood glucose level ≥200 mg/dL, fasting blood glucose level ≥126 mg/dL or medical treatment for DM at index PCI.18 Dyslipidaemia was defined as medical treatment for dyslipidaemia at the index PCI. We calculated the estimated glomerular filtration rate (eGFR) based on the serum creatinine level, age, weight and sex using the following formula: eGFR=194×Cr−1.094×age−0.287 (men) and eGFR=194×Cr−1.094×age−0.287×0.739 (women).19 We defined CKD as eGFR <60 mL/min/1.73 m2.19 Hyperuricaemia was defined as serum uric acid levels ≥7.0 and ≥6.0 mg/dL for men and women, respectively, and/or taking urate-lowering drugs according to previous studies.20 We used echocardiographic findings closest to the index PCI, performed between –100 and 0 days before index PCI. LVEF was calculated using modified Simpson’s rule.21 However, the Teichholz method was used for LVEF measurement if the data of the modified Simpson’s rule were missing.21 The number of diseased vessels was defined as the number of coronary arteries with severe stenosis (≥75%) in the major epicardial coronary segments of the right coronary, left anterior descending and left circumflex arteries and their branch lesions that underwent PCI. The diseased left main trunk (LMT), defined as ≥75% stenosis, was counted separately. The patients were categorised according to the combination of the number of diseased vessels and LMT disease.
Clinical outcomes
We defined primary outcome as a major bleeding event in moderate or severe bleeding according to the Global Use of Streptokinase and t-PA for Occluded Coronary Arteries (GSUTO) bleeding criteria.22 Moderate bleeding requires blood transfusion but does not result in haemodynamic compromise, and severe bleeding indicates intracerebral haemorrhage or results in substantial haemodynamic compromise requiring treatment. Secondary outcomes were defined as all-cause death and major adverse cardiac events (MACE), including cardiac death, myocardial infarction (MI) and stroke.
Thrombogenicity in patients with heart failure
T-TAS is an automated microchip-based flow chamber system developed for easy and rapid assessment of platelet thrombus formation under certain flow conditions, as previously described.23 Briefly, this system analyses different thrombus formation processes using a simple procedure with microchips coated with thrombogenic surfaces. One chip, the platelet chip (PL), is coated with type I collagen. Inside the microchip, platelets adhere and aggregate on the surface of the collagen, and microchip capillaries are occluded.23 The other chip, the atheroma chip (AR), is covered with type I collagen and tissue thromboplastin. Inside the microchips, the platelets are simultaneously activated with the triggering of the coagulation system by collagen and tissue thromboplastin.23 The process of thrombus formation inside the two chips was analysed by monitoring the flow pressure change. The area under the curve (AUC) for the flow pressure was computed to assess platelet thrombogenicity inside the microchips. The PL18-AUC10 parameter represented the AUC for the first 10 min of the PL test at a flow rate of 18 μL/min, and AR10-AUC30 is the parameter representing the AUC for the first 30 min for the AR tested at a flow rate of 10 µL/min.23
We measured the T-TAS of 690 consecutive patients who underwent PCI between August 2013 and March 2017 at Kumamoto University Hospital. We excluded 154 patients who were using anticoagulants, such as warfarin and direct oral anticoagulants (DOACs), or were undergoing dialysis. Blood samples were obtained using a 6 Fr sheath inserted into the femoral vein before treatment with unfractionated heparin immediately before the first CAG or at the time of PCI. We categorised the 536 patients into two groups according to their history of HF: non-HF (n=422) and HF (n=114) groups. HF was defined according to the diagnostic algorithm of the European Society of Cardiology guidelines.24 Furthermore, the HF group was reclassified based on the BNP level: HF with low BNP level (<100 pg/mL) (n=47) and HF with high BNP level (≥100 pg/mL) (n=67) groups (online supplemental figure 2).
Statistical analyses
Continuous variable data are presented as median values (IQR) and categorical variables as frequencies and percentages. Group comparisons were analysed using the Mann-Whitney U test for continuous variables between the two groups, the Kruskal-Wallis test for continuous variables followed by multiple comparisons with the Bonferroni method among the three groups, the χ2 or Fisher’s exact test for categorical variables and the log-rank test for bleeding events, MACE and all-cause-free survival curves, as appropriate. Cox proportional hazards regression analysis was performed to compute HRs and 95% CIs as estimates of the clinical outcomes. The multivariate Cox proportional hazards model adjusted for age, sex, body mass index (BMI), systolic blood pressure at admission, acute or chronic coronary syndrome, hypertension, diabetes, dyslipidaemia, CKD, haemodialysis, previous PCI, previous coronary artery bypass grafting (CABG), prior MI, prior stroke, prior AF, prior peripheral arterial disease (PAD), LMT disease, multivessel disease (MVD) and anticoagulant, DAPT and proton pump inhibitor use was used in complete case analysis. For sensitivity analysis, a multiple imputation analysis was performed with 20 imputed datasets generated by the fully conditional specification method. The results across the 20 imputed datasets were combined using Rubin’s rules.25 A two-tailed p value <0.05 denoted a statistically significant difference. All statistical analyses were performed using the SPSS software V.23 (IBM, Armonk, New York, USA).
Regarding a cut-off value of 100 pg/mL for the BNP level, BNP is a promising biomarker that represents the severity of HF. In Japanese guideline, it is recommended that if the BNP level is 100 pg/mL or above, there is a possibility of HF warranting treatment, and thus a further examination or referral to a specialist is advised.26 Furthermore, in the European Society of Cardiology guidelines, a cut-off value of 100 pg/mL for BNP is specified as indicative of acute heart failure.27 Based on these considerations, we established a cut-off value of 100 pg/mL for the BNP level.
Results
Baseline characteristics
We categorised the 7160 patients into the non-HF and HF groups. The baseline patient characteristics are summarised in online supplemental table 1. Compared with the non-HF group, the HF group had higher rates of female sex; hypertension; diabetes; CKD; haemodialysis; malignancy; previous MI, PCI, CABG and stroke; AF; PAD; PCI to the left circumflex artery; PCI to the right coronary artery; PCI to the LMT; MVD; BNP level and anticoagulant, DOAC and warfarin use. In addition, patients with HF had lower BMI, eGFR and rate of acute coronary syndrome, dyslipidaemia and family history of IHD and EF than those without HF.
Primary outcome
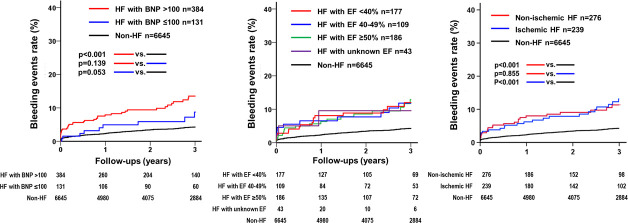
After PCI, 276 (3.9%) patients experienced major bleeding events during the 3-year follow-up period. Among these patients, 227 had no HF, 40 had HF with high BNP levels and 9 had HF with low BNP levels (online supplemental tables 2 and 3). Kaplan-Meier survival curves showed a higher rate of bleeding events in the HF group than in the non-HF group (p<0.001, online supplemental figure 3). Kaplan-Meier survival curves showed a higher rate of bleeding events in the HF with high BNP level group than in the non-HF group (p<0.001); however, no significant difference was observed between the other groups (figure 1). Multivariate Cox regression analysis showed a significantly higher rate of major bleeding events in the HF (HR 1.63; 95% CI 1.11 to 2.39; p=0.012) and HF with high BNP level (HR 1.68; 95% CI 1.11 to 2.54; p=0.014) groups, whereas the rate was almost identical in the HF with low BNP level group (HR 1.43; 95% CI 0.63 to 3.26; p=0.390) compared with that in the non-HF group (table 1). Additionally, in multivariate Cox regression analysis including LVEF value as adjusted factor, the HF and HF with high BNP level group had higher bleeding events compared with non-HF group (HR 1.53; 95% CI 1.01 to 2.30; p=0.042, HR 1.59; 95% CI 1.02 to 2.49; p=0.035), whereas there were no significant event rate between the HF with low BNP level group and the non-HF group (HR 1.22; 95% CI 0.49 to 3.01; p=0.659) (table 1).
Figure 1.
Kaplan-Meier estimates of bleeding events (GUSTO severe/moderate) between non-HF groups and the HF groups classified according to BNP, EF level, ischaemic aetiology. Kaplan-Meier curves show the rate of major bleeding events after PCI according to HF and severity (BNP and EF level). The bleeding event rate was significantly higher in the HF with high BNP level group than in the non-HF group. There was no difference in the rate of major bleeding events among patients with HF, regardless of the EF. BNP, brain natriuretic peptide; EF, ejection fraction; GUSTO, Global Use of Streptokinase and t-PA for Occluded Coronary Arteries; HF, heart failure; PCI, percutaneous coronary intervention.
Table 1.
Cox proportional hazard regression for clinical outcomes
| Univariate | Multivariable model 1* † | Multivariable model 2‡ † | Multiple imputation* § | |
| HR (95% CI), p value | HR (95% CI), p value | HR (95% CI), p value | HR (95% CI), p value | |
| Bleeding events | ||||
| (GUSTO severe/moderate) | ||||
| Non-HF | Ref | Ref | Ref | Ref |
| HF | 2.90 (2.13 to 3.94), <0.001 | 1.63 (1.11 to 2.39), 0.012 | 1.53 (1.01 to 2.30), 0.042 | 1.70 (1.23 to 2.37), 0.002 |
| HF with BNP ≤100 | 1.91 (0.98 to 3.72), 0.057 | 1.43 (0.63 to 3.26), 0.390 | 1.22 (0.49 to 3.01), 0.659 | 1.53 (0.78 to 3.00), 0.216 |
| HF with BNP >100 | 3.28 (2.34 to 4.59), <0.001 | 1.68 (1.11 to 2.54), 0.014 | 1.59 (1.02 to 2.49), 0.035 | 1.75 (1.22 to 2.51), 0.002 |
| Intracranial bleeding | ||||
| Non-HF | Ref | Ref | Ref | Ref |
| HF | 3.06 (1.64 to 5.73), <0.001 | 2.59 (1.21 to 5.54), 0.014 | 2.70 (1.17 to 6.24), 0.19 | 2.03 (1.04 to 3.95) 0.039 |
| HF with BNP ≤100 | 1.79 (0.44 to 7.35), 0.419 | 2.63 (0.62 to 11.14), 0.189 | 2.89 (0.67 to 12.53), 0.154 | 1.51 (0.36 to 6.30), 0.570 |
| HF with BNP >100 | 3.57 (1.82 to 7.02), <0.001 | 2.57 (1.11 to 5.97), 0.028 | 2.65 (1.05 to 6.64), 0.037 | 2.20 (1.06 to 4.54), 0.034 |
| Gastrointestinal bleeding | ||||
| Non-HF | Ref | Ref | Ref | Ref |
| HF | 3.33 (2.11 to 5.26), <0.001 | 1.68 (0.93 to 3.02), 0.083 | 1.79 (0.95 to 3.35), 0.069 | 2.07 (1.27 to 3.40), 0.004 |
| HF with BNP ≤100 | 2.06 (0.76 to 5.60), 0.157 | 1.00 (0.24 to 4.12), 0.996 | 1.08 (0.25 to 4.49), 0.916 | 1.63 (0.59 to 4.51), 0.343 |
| HF with BNP >100 | 3.83 (2.34 to 6.27), <0.001 | 1.88 (1.01 to 3.52), 0.047 | 2.02 (1.03 to 3.97), 0.040 | 2.21 (1.29 to 3.77), 0.004 |
| MACE | ||||
| Non-HF | Ref | Ref | Ref | |
| HF | 2.25 (1.76 to 2.88), <0.001 | 1.89 (1.41 to 2.51), <0.001 | 1.34 (0.97 to1.85), 0.071 | 1.69 (1.30 to 2.19), <0.001 |
| HF with BNP ≤100 | 0.55 (0.23 to 1.32), 0.180 | 0.73 (0.30 to 1.78), 0.489 | 0.55 (0.20 to 1.49), 0.244 | 0.55 (0.23 to 1.32), 0.180 |
| HF with BNP >100 | 2.91 (2.25 to 3.75), <0.001 | 2.21 (1.64 to 2.98), <0.001 | 1.54 (1.10 to 2.17), 0.011 | 2.02 (1.54 to 2.65), <0.001 |
| All-cause death | ||||
| Non-HF | Ref | Ref | Ref | |
| HF | 2.46 (1.93 to 3.12), <0.001 | 1.49 (1.12 to 1.99), 0.007 | 1.07 (0.77 to 1.47), 0.685 | 1.61 (1.25 to,2.08), <0.001 |
| HF with BNP ≤100 | 0.79 (0.37 to 1.67), 0.535 | 0.44 (0.14 to 1.36), 0.153 | 0.27 (0.68 to 1.10), 0.069 | 0.82 (0.38 to 1.73), 0.593 |
| HF with BNP >100 | 3.09 (2.41 to 3.97), <0.001 | 1.72 (1.28 to 2.32), <0.001 | 1.22 (0.88 to 1.71), 0.225 | 1.79 (1.37 to 2.33), <0.001 |
*Adjusted for age, sex, body mass index, systolic blood pressure at admission, acute coronary syndrome or chronic coronary syndrome, hypertension, diabetes, dyslipidaemia, chronic kidney disease, haemodialysis, previous PCI, previous coronary artery bypass grafting, prior myocardial infarction, prior stroke, prior atrial fibrillation, prior peripheral artery disease, left main trunk, multivessel disease, anticoagulants, dual-antiplatelet therapy, proton pump inhibitor.
†Complete case analysis.
‡Adjusted for age, sex, body mass index, systolic blood pressure at admission, acute coronary syndrome or chronic coronary syndrome, hypertension, diabetes, dyslipidaemia, chronic kidney disease, haemodialysis, previous PCI, previous coronary artery bypass grafting, prior myocardial infarction, prior stroke, prior atrial fibrillation, prior peripheral artery disease, left main trunk, multivessel disease, left ventricular ejection fraction, anticoagulants, dual-antiplatelet therapy, proton pump inhibitor.
§A multiple imputation analysis was performed with 20 imputed datasets generated by the fully conditional specification method. The results across 20 imputed datasets were combined using Rubin’s rules.
BNP, B-type natriuretic peptide; GUSTO, Global Use of Streptokinase and t-PA for Occluded Coronary Arteries; HF, heart failure; MACE, major adverse cardiovascular event; PCI, percutaneous coronary intervention; Ref, reference.
In the classification according to EF (HF with reduced EF (<40%), with HF with mild reduced EF (40%–49%), with preserved EF (≥50%) and with unknown EF), there was no significant difference in major bleeding events among the four groups (figure 1).
Among the 276 patients who underwent PCI and experienced major bleeding events during the 3-year follow-up period, 227 had no HF, 25 had non-ischaemic HF and 24 had ischaemic HF. Kaplan-Meier survival curves showed a higher rate of bleeding events in the ischaemic and non-ischaemic HF group than non-HF group (p<0.001); however, no significant difference was observed between ischaemic and non-ischaemic HF groups (p=0.855) (figure 1). Multivariate Cox regression analysis showed a significantly higher rate of major bleeding events in the non-ischaemic HF group compared with non-HF group (HR 1.74; 95% CI 1.07 to 2.83; p=0.024), whereas no significant difference between ischaemic HF and non-HF groups (HR 1.36; 95% CI 0.82 to 2.27; p=0.225).
Secondary outcomes: major adverse cardiovascular events and all-cause death
After PCI, 508 (7.09%) and 502 (7.01%) patients experienced MACE and all-cause death within the 3-year follow-up period, respectively. Kaplan-Meier survival curves showed a higher rate of MACE and all-cause death in the HF with high BNP level group than in the other two groups (p<0.001); however, no significant difference was observed between the HF with low BNP level and non-HF groups (figure 2). Multivariate Cox regression analysis without LVEF level also showed a significantly higher rate of MACE in the HF (HR 1.89; 95% CI 1.41 to 2.51; p<0.001) and HF with high BNP level (HR 2.21; 95% CI 1.64 to 2.98; p<0.001) groups, whereas the rate was almost identical in the HF with low BNP level group (HR 0.73; 95% CI 0.30 to 1.78; p=0.489) compared with the non-HF group. Regarding all-cause death, multivariate Cox regression analysis also showed a significantly higher rate of all-cause death in the HF (HR 1.49; 95% CI 1.12 to 1.99; p=0.007) and HF with high BNP level (HR 1.72; 95% CI 1.28 to 2.32; p<0.001) groups, whereas the rate was almost identical in the HF with low BNP level group (HR 0.44; 95% CI 0.14 to 1.36; p=0.153) compared with the non-HF group (table 1). However, in the multivariate Cox regression analysis including LVEF as adjusted factor, there were no significant difference between HF group and non-HF group regarding MACE (HR 1.34; 95% CI 0.97 to 1.85; p=0.071) and all-cause death (HR 1.07; 95% CI 0.77 to 1.47; p=0.685) (table 1).
Figure 2.
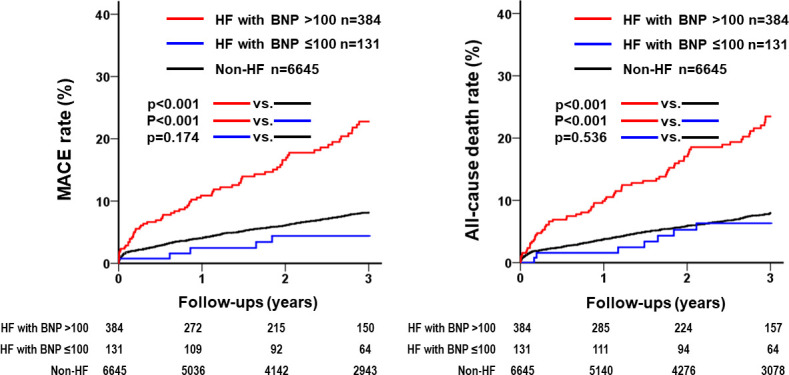
Kaplan-Meier estimates of MACE and all-cause death. Kaplan-Meier curves show the rates of MACE and all-cause death after PCI according to HF and severity (BNP level). The MACE and all-cause rates were significantly higher in the HF with high BNP level group than in the other groups. BNP, brain natriuretic peptide; HF, heart failure; MACE, major adverse cardiac events; PCI, percutaneous coronary intervention.
Sensitivity analysis
We performed a sensitivity analysis to assess the validity of the study results by imputing missing values. This analysis revealed that the HF with high BNP level group had a higher rate of bleeding, MACE and all-cause death than the non-HF group; otherwise, no significant difference was observed among other groups (table 1).
Total Thrombus-Formation Analysis System parameter
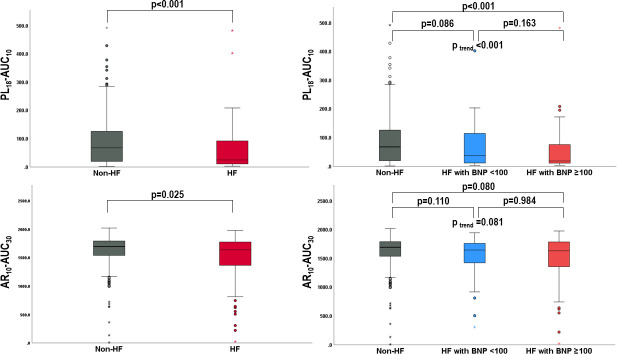
We measured the PL18-AUC10 and AR10-AUC30 of 536 patients. The PL18-AUC10 levels ranged from 1.5 to 492.4, with a median value of 60.7, and the 25th–75th percentiles were 16.1–120.2. PL18-AUC10 levels were significantly lower in the HF group than in the non-HF group (25.0 (95% CI 11.0 to 93.7) vs 68.0 (95% CI 19.8 to 127.3), p<0.001) (figure 3). There were significant differences in the PL18-AUC10 levels among the non-HF, HF with low BNP level and HF with high BNP level groups (68.0 (95% CI 19.8 to 127.3) vs 37.5 (95% CI 11.1 to 116.1) vs 18.8 (95% CI 10.7 to 77.1), p<0.001) (figure 3). PL18-AUC10 levels were significantly lower in the HF with high BNP level group than in the non-HF group (p<0.001), whereas there were no significant differences among the other groups. The AR10-AUC30 levels ranged from 8.3 to 2020.8, with a median value of 1685.8, and the 25th–75th percentiles were 1527.8–1787.5. AR10-AUC30 levels were significantly lower in the HF group than in the non-HF group (1696.0 (95% CI 1538.4 to 1793.1) vs 1637.4 (95% CI 1365.3 to 1776.7), p=0.025) (figure 3). However, among the three groups, there were no significant differences in the AR10-AUC30 levels (1696.0 (95% CI 1538.4 to 1793.1) vs 1647.9 (95% CI 1393.9 to 1765.1) vs 1634.5 (95% CI 1354.6 to 1789.6), p=0.081) (figure 3).
Figure 3.
Total Thrombus-Formation Analysis System level in patients with and without HF and patients with HF with high BNP levels, HF with low BNP levels and without HF. Upper box plot shows the level of PL-AUC in patients with and without HF and patients according to HF and severity (BNP level). Lower box plot shows the level of AR-AUC in patients with and without HF and patients according to HF and severity (BNP level). AR, atheroma chip; AUC, area under the curve; BNP, B-type natriuretic peptide; HF, heart failure; PL, platelet chip.
Discussion
This large-scale, multicentre, observational cohort study of 7160 patients after PCI during a 3-year follow-up period investigated the association between HF severity and bleeding events. Regarding the primary outcome, the present study showed that the HF group had more bleeding events than the non-HF group, which supports the inclusion of HF in addition to the ARC-HBR in Japan. This study also revealed that the high BNP level group had a higher rate of bleeding events than the non-HF group, whereas there was no significant difference between the non-HF and HF with low BNP level groups. This finding suggests that HF with high BNP level is a more appropriate HBR factor than HF.
The incidence rate of bleeding events ranges from 1.6% to 7.3%.8 28 29 The incidence rate of bleeding events was 3.8% in our database, which was consistent with the results of these studies. Other previous studies reported bleeding events in patients undergoing PCI, with the incidence rate of HF ranging from 8.0% to 12.9%, and the incidence rate of these bleeding events was significantly higher in patients with HF than in those without HF.30 31 The incidence rate of bleeding events in patients with HF was 9.5% in our database, which was also consistent with the results of these studies.
The reasons why bleeding events increase in patients with HF after PCI, especially in the high BNP level group, should be further discussed. In general, patients undergoing PCI are treated with antiplatelet therapy to reduce atherothrombotic risk and prevent coronary thrombotic events. Antiplatelet agents are metabolised by hepatocytes. HF leads to multiple organ failure owing to congestion and malperfusion. In particular, with regard to drug metabolism, a reduction in liver metabolic activity can also be observed in patients with congestive HF.32 That may occur to increase the plasma levels of antiplatelet agents, resulting in a high risk of bleeding complications. In this study, the T-TAS analysis showed that the PL18-AUC10 values were significantly lower in patients with HF with high BNP levels than in patients without HF, whereas the PL18-AUC10 values in patients with HF with low BNP levels did not decrease. This result ex vivo can support the association between HF severity and bleeding events observed in the analysis of the CLIDAS database.
Regarding secondary outcomes, the HF with high BNP level group had higher rates of MACE and all-cause death than the non-HF and HF with low BNP level groups, as shown in the Kaplan-Meier survival curves. Furthermore, multivariate Cox regression analysis without LVEF level showed a significant difference between the HF with high BNP level and non-HF groups. An elevated BNP level is an independent predictor of new-onset MACE and all-cause death in patients with IHD, which is consistent with the results of this study.33 34 Moreover, a previous study revealed that patients with bleeding events after PCI had significantly higher rates of MACE and all-cause mortality.35 The plausible mechanisms of bleeding events with subsequent mortality include activation of the coagulation cascade, increased prothrombotic cytokine levels, hypovolemia, anaemia (compromised oxygen delivery), reflex tachycardia (increased myocardial oxygen demand), transfusion of blood products and cessation of antiplatelet and anticoagulant therapies.36 Thus, patients with HF with higher BNP levels might have a higher risk of bleeding events and subsequent MACE and all-cause death. When conducting multivariate Cox regression analysis using LVEF level as adjusted factor, significant difference between HF with high BNP group and non-HF group was not observed, indicating that the reduced LVEF was significantly associated with these events. Previous studies revealed that patients with ischaemia and low EF had higher rates of mortality and MACE.37 38 Based on these findings, lower LVEF might be more strongly associated with MACE and all-cause death. Conversely, elevated levels of BNP might be more strongly associated with bleeding events.
Regarding antithrombotic therapy including anticoagulants, according to the AFIRE (Atrial Fibrillation and Ischemic Events With Rivaroxaban in Patients With Stable Coronary Artery Disease) study, patients underwent PCI complicated with AF had lower bleeding events in rivaroxaban monotherapy compared with combination therapy including antiplatelet agent.39 Furthermore, in this subanalysis, investigating based on the presence of HF, rivaroxaban monotherapy was effective in suppressing bleeding events regardless of the presence of HF.40 However, with respect to MACE, rivaroxaban monotherapy might be suitable for patients with HF, although the p value for interaction was not statistically significant at 0.063.40 In patients with HF with BNP ≥100 pg/mL complicated by AF, it may be worth considering an early switch to DOAC monotherapy. However, as the AFIRE trial targeted patients >1 year after undergoing PCI, it is necessary to evaluate the efficacy and safety of DOAC monotherapy in clinical trials focusing on patients in the earlier phase after PCI.
This study had some limitations. First, because this was a retrospective study, there was a possibility of selection bias and unmeasured confounding factors, such as dosage of diuretics, duration of antiplatelet agents and history of blood transfusion. To reduce selection bias, this study included all patients from the seven hospitals during the study period. Second, owing to the nature of the database, the definition of HF as a prior hospitalisation for HF was used, resulting in an underestimation of the number of HF cases. However, as this differential misclassification would almost bias towards the null hypothesis, the results of this study might be unlikely to be overestimated. Third, the CLIDAS database includes data from the Japanese Diagnosis Procedure Combination system that lacks traceability after changing hospitals. If a patient was hospitalised in another hospital after PCI, we could not follow the events, resulting in an underestimation of the number of events.
Conclusion
The CLIDAS real-world database reveals that HF with high BNP levels (≥100 pg/mL) is independent of HBR, and PL10-AUC18 levels measured using the T-TAS also support this association, suggesting that the bleeding risk might be altered depending on HF severity.
Acknowledgments
The authors thank the Kowa Company for funding the development of CLIDAS. The authors appreciate the contributions of all CLIDAS research group members. The authors thank Yuri Matoba (Precision, Tokyo, Japan) for helping them integrate the data.
Footnotes
Twitter: @MasanobuIshii
Contributors: All authors have contributed to this manuscript. YOt, MI, SI, TN and KT performed the statistical analysis. MI, TN, KT, TM, TKo, YOb, TKa, KKar, YI, AK, YMiz, KN, MN, TI, YMiy, HS, NA, HF and RN acquired the data of CLIDAS. YOt, MI, SI, TN, KT and KKai acquired the data of T-TAS. YOt, MI, SI, TN and KT conceived and designed the study. YOt drafted the manuscript. MI, TN and KT made critical revisions of the manuscript for key intellectual content. NA provided overall supervision for this study and manuscript. MI is the gurantor of this study.
Funding: This work was supported by Kowa Company and Health Labour Sciences Research Grant (22FA1016).
Competing interests: TM received research grants from Amgen and honoraria from Abbott Medical and Bayer. TK received scholarship funds from Abbott Medical. YI received honoraria from Daiichi Sankyo and Toa Eiyo. KKario received research grants and honoraria from Sanwa Kagaku Kenkyusho. AK received honoraria from AstraZeneca, Eli Lilly and Sumitomo Pharma. YMizuno received research grants and consulting fees from Bayer. KT received research grants from PPD-Shin Nippon Biomedical Laboratories and Alexion Pharmaceuticals; and scholarship funds from Abbott Medical, Bayer, Boehringer Ingelheim, Daiichi Sankyo, ITI, Ono Pharmaceutical, Otsuka Pharmaceutical and Takeda Pharmaceutical; affiliation with the endowed department from Abbott Medical, Boston Scientific, Cardinal Health, Fides-ONE, Fukuda Denshi, GM Medical, ITI, Japan Lifeline, Kaneka Medix, Medical Appliance, Medtronic, Nipro and Terumo and honoraria from Abbott Medical, Amgen, AstraZeneca, Bayer, Daiichi Sankyo, Medtronic, Kowa, Novartis Pharma, Otsuka Pharmaceutical, Pfizer and Janssen Pharmaceutical. HS reports stock or stock options in Precision. HF received consulting fees from Mehergen Group Holdings; and honoraria from Novartis Pharma and Otsuka Pharmaceutical. RN received honoraria from Kowa, Takeda Pharmaceutical, Tanabe-Mitsubishi Pharmaceutical and Boehringer-Ingelheim. All other authors have no conflicts of interest to declare.
Patient and public involvement statement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study was approved by the Institutional Review Board of Kumamoto University Hospital (Senshin-No. 1655 and 2406) and each institutional ethics committee, and was in accordance with the Declaration of Helsinki. This study was waived from the requirement for individual informed consent because all data were anonymised by the participating institutions and were then collected in the CLIDAS database.
References
- 1.Mauri L, Kereiakes DJ, Yeh RW, et al. Twelve or 30 months of dual antiplatelet therapy after drug-eluting stents. N Engl J Med 2014;371:2155–66. 10.1056/NEJMoa1409312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Watanabe H, Domei T, Morimoto T, et al. Effect of 1-month dual antiplatelet therapy followed by clopidogrel vs 12-month dual antiplatelet therapy on cardiovascular and bleeding events in patients receiving PCI: the STOPDAPT-2 randomized clinical trial. JAMA 2019;321:2414–27. 10.1001/jama.2019.8145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Urban P, Mehran R, Colleran R, et al. Defining high bleeding risk in patients undergoing percutaneous coronary intervention. Circulation 2019;140:240–61. 10.1161/CIRCULATIONAHA.119.040167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Urban P, Mehran R, Colleran R, et al. Defining high bleeding risk in patients undergoing percutaneous coronary intervention: a consensus document from the academic research consortium for high bleeding risk. Eur Heart J 2019;40:2632–53. 10.1093/eurheartj/ehz372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yamamoto K, Natsuaki M, Yoshikawa Y, et al. Effects of body weight on bleeding and ischemic events in patients undergoing percutaneous coronary intervention - from the CREDO-Kyoto registry Cohort-2. Circ J 2020;84:1734–45. 10.1253/circj.CJ-20-0343 [DOI] [PubMed] [Google Scholar]
- 6.Numasawa Y, Inohara T, Ishii H, et al. An overview of percutaneous coronary intervention in dialysis patients: insights from a Japanese nationwide registry. Catheter Cardiovasc Interv 2019;94:E1–8. 10.1002/ccd.27986 [DOI] [PubMed] [Google Scholar]
- 7.Natsuaki M, Morimoto T, Yamaji K, et al. Prediction of thrombotic and bleeding events after percutaneous coronary intervention: CREDO-Kyoto thrombotic and bleeding risk scores. J Am Heart Assoc 2018;7:e008708. 10.1161/JAHA.118.008708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Numasawa Y, Kohsaka S, Ueda I, et al. Incidence and predictors of bleeding complications after percutaneous coronary intervention. J Cardiol 2017;69:272–9. 10.1016/j.jjcc.2016.05.003 [DOI] [PubMed] [Google Scholar]
- 9.Nakamura M, Kimura K, Kimura T, et al. JCS 2020 guideline focused update on antithrombotic therapy in patients with coronary artery disease. Circ J 2020;84:831–65. 10.1253/circj.CJ-19-1109 [DOI] [PubMed] [Google Scholar]
- 10.Hosokawa K, Ohnishi T, Sameshima H, et al. Analysing responses to aspirin and clopidogrel by measuring platelet thrombus formation under arterial flow conditions. Thromb Haemost 2013;109:102–11. 10.1160/TH12-06-0441 [DOI] [PubMed] [Google Scholar]
- 11.Hosokawa K, Ohnishi T, Kondo T, et al. A novel automated microchip flow-chamber system to quantitatively evaluate thrombus formation and antithrombotic agents under blood flow conditions. J Thromb Haemost 2011;9:2029–37. 10.1111/j.1538-7836.2011.04464.x [DOI] [PubMed] [Google Scholar]
- 12.Nakanishi N, Kaikita K, Ishii M, et al. Development and assessment of total thrombus-formation analysis system-based bleeding risk model in patients undergoing percutaneous coronary intervention. Int J Cardiol 2021;325:121–6. 10.1016/j.ijcard.2020.10.015 [DOI] [PubMed] [Google Scholar]
- 13.Ito M, Kaikita K, Sueta D, et al. Total thrombus-formation analysis system (T-TAS) can predict periprocedural bleeding events in patients undergoing catheter ablation for atrial fibrillation. J Am Heart Assoc 2016;5:e002744. 10.1161/JAHA.115.002744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Akashi N, Matoba T, Kohro T, et al. Sex differences in long-term outcomes in patients with chronic coronary syndrome after percutaneous coronary intervention: insights from a Japanese real-world database using a storage system. Circ J 2023;87:775–82. 10.1253/circj.CJ-22-0653 [DOI] [PubMed] [Google Scholar]
- 15.Akashi N, Kuwabara M, Matoba T, et al. Hyperuricemia predicts increased cardiovascular events in patients with chronic coronary syndrome after percutaneous coronary intervention: a nationwide cohort study from Japan. Front Cardiovasc Med 2022;9:1062894. 10.3389/fcvm.2022.1062894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matoba T, Kohro T, Fujita H, et al. Architecture of the Japan ischemic heart disease multimodal prospective data acquisition for precision treatment (J-IMPACT) system. Int Heart J 2019;60:264–70. 10.1536/ihj.18-113 [DOI] [PubMed] [Google Scholar]
- 17.Umemura S, Arima H, Arima S, et al. The Japanese society of hypertension guidelines for the management of hypertension (JSH 2019). Hypertens Res 2019;42:1235–481. 10.1038/s41440-019-0284-9 [DOI] [PubMed] [Google Scholar]
- 18.Araki E, Goto A, Kondo T, et al. Japanese clinical practice guideline for diabetes 2019. J Diabetes Investig 2020;11:1020–76. 10.1111/jdi.13306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Japan Nephrology S. [Special issue: clinical practice guidebook for diagnosis and treatment of chronic kidney disease 2012]. Nihon Jinzo Gakkai Shi 2012;54:1034–191. [PubMed] [Google Scholar]
- 20.Suwazono Y, Kobayashi E, Uetani M, et al. G-protein Beta3 subunit gene variant is unlikely to have a significant influence on serum uric acid level in Japanese workers. Tohoku J Exp Med 2006;209:149–57. 10.1620/tjem.209.149 [DOI] [PubMed] [Google Scholar]
- 21.Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American society of echocardiography and the European association of cardiovascular imaging. J Am Soc Echocardiogr 2015;28:1–39. 10.1016/j.echo.2014.10.003 [DOI] [PubMed] [Google Scholar]
- 22.Mehran R, Rao SV, Bhatt DL, et al. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the bleeding academic research consortium. Circulation 2011;123:2736–47. 10.1161/CIRCULATIONAHA.110.009449 [DOI] [PubMed] [Google Scholar]
- 23.Mitsuse T, Kaikita K, Ishii M, et al. Total thrombus-formation analysis system can predict 1-year bleeding events in patients with coronary artery disease. J Atheroscler Thromb 2020;27:215–25. 10.5551/jat.49700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ponikowski P, Voors AA, Anker SD, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European society of cardiology (ESC)Developed with the special contribution of the heart failure association (HFA) of the ESC. Eur Heart J 2016;37:2129–200. 10.1093/eurheartj/ehw128 [DOI] [PubMed] [Google Scholar]
- 25.Marshall A, Altman DG, Holder RL, et al. Combining estimates of interest in prognostic modelling studies after multiple imputation: current practice and guidelines. BMC Med Res Methodol 2009;9:57. 10.1186/1471-2288-9-57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tsutsui H, Isobe M, Ito H, et al. Guideline on diagnosis and treatment of acute and chronic heart failure - digest version. Circ J 2019;83:2084–184. 10.1253/circj.CJ-19-0342 [DOI] [PubMed] [Google Scholar]
- 27.McDonagh TA, Metra M, Adamo M, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 2021;42:3599–726. 10.1093/eurheartj/ehab368 [DOI] [PubMed] [Google Scholar]
- 28.Mehran R, Pocock S, Nikolsky E, et al. Impact of bleeding on mortality after percutaneous coronary intervention results from a patient-level pooled analysis of the REPLACE-2 (randomized evaluation of PCI linking angiomax to reduced clinical events), ACUITY (acute Catheterization and urgent intervention triage strategy), and HORIZONS-AMI (harmonizing outcomes with revascularization and stents in acute myocardial infarction) trials. JACC Cardiovasc Interv 2011;4:654–64. 10.1016/j.jcin.2011.02.011 [DOI] [PubMed] [Google Scholar]
- 29.Mehran R, Pocock SJ, Nikolsky E, et al. A risk score to predict bleeding in patients with acute coronary syndromes. J Am Coll Cardiol 2010;55:2556–66. 10.1016/j.jacc.2009.09.076 [DOI] [PubMed] [Google Scholar]
- 30.Généreux P, Giustino G, Witzenbichler B, et al. Incidence, predictors, and impact of post-discharge bleeding after percutaneous coronary intervention. J Am Coll Cardiol 2015;66:1036–45. 10.1016/j.jacc.2015.06.1323 [DOI] [PubMed] [Google Scholar]
- 31.Yeh RW, Secemsky EA, Kereiakes DJ, et al. Development and validation of a prediction rule for benefit and harm of dual antiplatelet therapy beyond 1 year after percutaneous coronary intervention. JAMA 2016;315:1735–49. 10.1001/jama.2016.3775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maleki M, Vakilian F, Amin A. Liver diseases in heart failure. Heart Asia 2011;3:143–9. 10.1136/heartasia-2011-010023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang LJ, Li N, Li Y, et al. Cardiac biomarkers predicting MACE in patients undergoing noncardiac surgery: a meta-analysis. Front Physiol 2018;9:1923. 10.3389/fphys.2018.01923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mueller C, McDonald K, de Boer RA, et al. Heart failure association of the European society of cardiology practical guidance on the use of natriuretic peptide concentrations. Eur J Heart Fail 2019;21:715–31. 10.1002/ejhf.1494 [DOI] [PubMed] [Google Scholar]
- 35.Kaikita K, Yasuda S, Akao M, et al. Bleeding and subsequent cardiovascular events and death in atrial fibrillation with stable coronary artery disease: insights from the AFIRE trial. Circ Cardiovasc Interv 2021;14:e010476. 10.1161/CIRCINTERVENTIONS.120.010476 [DOI] [PubMed] [Google Scholar]
- 36.Kazi DS, Leong TK, Chang TI, et al. Association of spontaneous bleeding and myocardial infarction with long-term mortality after percutaneous coronary intervention. J Am Coll Cardiol 2015;65:1411–20. 10.1016/j.jacc.2015.01.047 [DOI] [PubMed] [Google Scholar]
- 37.Wu S, Wei J, Lauzon M, et al. Left ventricular ejection fraction and long-term outcomes in women presenting with signs and symptoms of ischaemia. Heart 2023;109:1624–30. 10.1136/heartjnl-2023-322494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Karedath J, Nazly S, Murtaza SF, et al. Comparison of early and long-term mortality in patients with reduced and preserved ejection fraction undergoing coronary artery bypass graft: a systematic review and meta-analysis. Cureus 2023;15:e43245. 10.7759/cureus.43245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yasuda S, Kaikita K, Akao M, et al. Antithrombotic therapy for atrial fibrillation with stable coronary disease. N Engl J Med 2019;381:1103–13. 10.1056/NEJMoa1904143 [DOI] [PubMed] [Google Scholar]
- 40.Yazaki Y, Nakamura M, Iijima R, et al. Clinical outcomes of rivaroxaban monotherapy in heart failure patients with atrial fibrillation and stable coronary disease: insights from the AFIRE trial. Circulation 2021;144:1449–51. 10.1161/CIRCULATIONAHA.121.055374 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
openhrt-2023-002489supp001.pdf (175.5KB, pdf)
Data Availability Statement
Data are available on reasonable request.