Abstract
Background
EBV pneumonia with multiple cavitary pulmonary lesions is clinically rare. We analyzed the clinical characteristics, diagnosis and treatment, with an aim to enhance clinicians’ awareness of this disease and reduce misdiagnosis and missed diagnoses.
Case Presentation
This paper presents A 59-year-old male patient’s initial symptoms included fever, cough, sputum, and asthma. The pulmonary CT imaging demonstrated multiple patchy and ground glass consolidation in both lungs, partial cavitary formation, and subpleural mesh lattice changes in the lower lobe of both lungs. Further analysis, including bronchoalveolar lavage fluid (BALF) metagenomic next-generation sequencing (mNGS) and CT-guided percutaneous lung biopsy mNGS, supported the diagnosis of EBV pneumonia. The patient was treated with acyclovir antiviral therapy for a week, resulting in symptom relief. Follow-up lung CT scans indicated interval reduction of inflammatory lesions, cavities, and interstitial changes. As the patient’s condition improved significantly and he was discharged from hospital. The treatment was continued with oral acyclovir for 12 days. Subsequent outpatient follow-up CT performed 12 days after discharge revealed further improvement of the inflammatory lesions, as well as a reduction in cavitary and interstitial changes.
Conclusion
The clinical imaging findings in the presented case were highly distinctive and have not been documented in either domestic or international literature. This uniqueness could have potentially contributed to misdiagnosis or overlooked diagnosis. mNGS of percutaneous lung puncture tissue is valuable for the diagnosis of infection with rare lung pathogens.
Keywords: adult EBV pneumonia, metagenomic next-generation sequencing, imaging characteristics, diagnosis, treatment
Background
Epstein-Barr virus (EBV) is a human herpesvirus that primarily infects B lymphocytes. It is classified as human herpesvirus type 4 and is globally prevalent. EBV infection can lead to a range of diseases, including both neoplastic (cancerous) and non-neoplastic (non-cancerous) conditions. Neoplastic diseases associated with EBV infection include nasopharyngeal cancer, lymphoma, and EBV-related gastric cancer.1,2 Non-neoplastic conditions include infectious mononucleosis, hemophagocytic syndrome, and chronic EBV infection.3 EBV pneumonia is rare.4 Mild, asymptomatic pneumonia has been reported to be found in about 5% to 10% of cases of EBV infection,5 with clinical symptoms including fever, cough, expectoration, and dyspnea.6 The imaging findings show pulmonary interstitial changes in general. The presented case involves an EBV pneumonia patient who exhibited exceptional lung imaging characteristics. By considering relevant literature from domestic and international sources, this paper summarizes the recent advancements in understanding the clinical manifestations and diagnosis of patients with EBV infection. The aim is to provide valuable insights for clinical diagnosis and treatment, thereby reducing the risk of misdiagnosis and missed diagnoses.
Case Presentation
A 59-year-old male was admitted to hospital in April with persistent productive cough and wheeze for 17 days. The symptoms began spontaneously, evolving from a non-productive cough to a small volume white mucus cough, which was difficult to expectorate. The patient also had a fever for 2 days, with temperature peaking at 39.1 degrees. Wheezing was noted with minimal physical activity. There was no accompanying chest tightness, palpitations, chest pain, hemoptysis, sore throat, nasal congestion, or rhinorrhea. Night sweats, weight loss, urinary changes and edema were also absent. The patient did not report skin rash, joint swelling, or canker sores. After taking p-acetamidophenol, there was a reduction in fever but no resolution of any other symptomology. The patient’s previous medical history was significant for type II diabetes, managed with oral antihyperglycemic agents (acarbose, glimepiride, dapagliflozin and metformin), and hypertension, managed with three agents (perindopril, amlodipine and metoprolol). There was a history of occasional alcohol consumption and long-term smoking habit of over 30 pack-years.
The patient initially presented to Jinjiang Dongshi Health center, where a CT-chest revealed bilateral pulmonary consolidation. Treatment at the time involved a course of antibiotics, including ceftriaxone, levofloxacin, and an extended course of moxifloxacin. In addition, the patient was prescribed a short course of dexamethasone, with some clinical improvement in respiratory symptoms, but poor appetite and fatigue persisted. The patient was subsequently hospitalized. On admission, the patient’s physical examination revealed the following: temperature: 36.2°C, pulse: 111 beats/min, respiratory rate: 20 breaths/min, and blood pressure: 109/75 mmHg. The patient was conscious, and there was no visible jaundice in the skin or mucous membranes. Superficial lymph nodes were not palpably enlarged. Auscultation of the lungs revealed coarse breath sounds and both dry and wet crackles. The heart examination did not indicate cardiac enlargement, and the heart rate was 111 beats/min. The abdomen was flat and soft. There was no palpable enlargement of the liver or spleen. The neurological examination did not reveal any abnormalities.
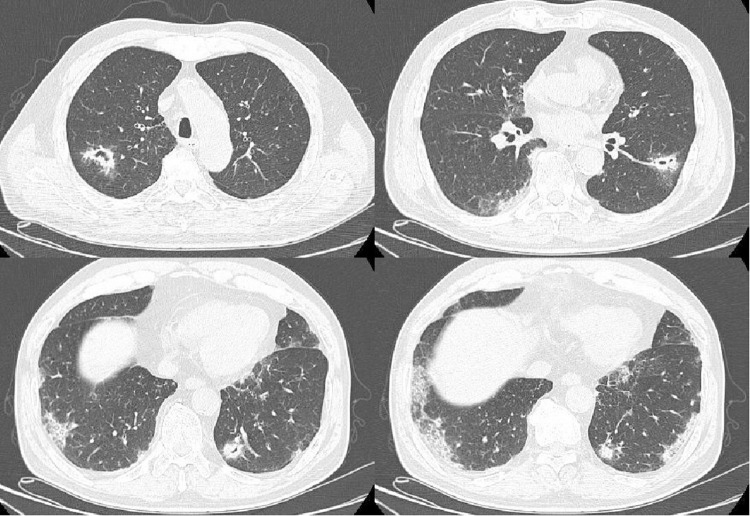
Upon admission to our hospital, a chest CT scan revealed the following findings: multiple patchy solid and ground glass opacifications in both lungs, partial cavitary formation, and subpleural mesh lattice changes in the lower lobe of both lungs (Figure 1). The blood gas analysis revealed a pH value of 7.450, PCO2 of 37.00 mmHg, and PO2 of 82.00 mmHg, indicating normal gas exchange in the lungs. The D-dimer level was measured at 1.092 mg/L. Liver function tests revealed an albumin level of 33.5 g/L, alanine aminotransferase level of 282 u/L, aspartate amino transferase level of 68 u/L, γ-glutamyl transpeptidase level of 570 u/L, and alkaline phosphatase level of 312 u/L, suggesting abnormalities in liver function. The complete blood count showed a white blood cell count of 5.16 × 10^9/L, with monocytes accounting for 0.54 × 10^9/L, representing 10.4% of the total white blood cell count, and neutrophils accounting for 3.8410×10^9/L, lymphocytes accounting for 1.3410 × 10^9/L. Interleukin level was measured at 6.57 pg/mL. C-reactive protein was elevated at 40.80 mg/L, indicating ongoing inflammation. Sputum tuberculosis smear results were negative. Though the patient tested positive for M. pneumonia IgG antibodies, IgM antibodies were negative, suggesting previous infection. Nasopharyngeal swabs for influenza A virus antigen and novel coronavirus nucleic acid were negative, ruling out influenza A and novel coronavirus infection as the cause of the patient’s symptoms. ENA testing showed antinuclear antibody karyotype cytoplasmic type at a titer of 1:100 and positive ribosomal P protein. Antinuclear antibodies were negative for puncta, nucleolar, homogeneous, peripheral type, and kinetochores, while kinetomeric protein B, SS-B, histone, JO-1, nucleosome, RNP, Scl-70, Sm, double-stranded DNA, native SS-A, and recombinant Ro-52 were negative. ANCA testing showed serine protease 3 was positive, Anti-glomerular basement membrane antibody and myeloblast peroxidase were negative. Renal function, coagulation function, myocardial zymography, procalcitonin, (1,3)-β-D-dextran test, and Galactomannan beta-glucose test were all normal, indicating no major abnormalities in these aspects.
Figure 1.
CT Chest on April 11th, 2023 (multiple patchy solid and ground glass opacifications in both lungs, partial cavitary formation, and subpleural mesh lattice changes in the lower lobe of both lungs).
Given the patient’s chest CT was not a typical presentation of viral infection, the patient started infusion on moxifloxacin 0.4g daily. According to the imaging findings, and in the context of the patient’s preexisting diabetes, further investigation for tuberculosis was warranted. As the patient’s sputum production was low, and given the low sensitivity of sputum samples, bronchoscopy was performed, revealing a patent bilateral bronchial lumen without any obvious abnormalities. Bronchoalveolar lavage was performed in specific lung segments, including the right upper lung apex segment, left upper tip, and left outer basal segment. The bronchoalveolar lavage fluid (BALF) analysis showed negative results for tubercule bacillus, bacteria, fungi cultures and tubercule bacillus DNA. The BALF mNGS detected the presence of the EB virus (sequence 16, relative abundance of 100%), and bacteria, fungi, and parasites were not detected in the BALF sample. However, the likelihood of EBV pulmonary infection was deemed low, and the images of the paitient were not typical of viral pneumonia. Furthermore the BALF may have been contaminated during the collection. So antiviral treatment was not administered. After admission, the antibody karyotype cytoplasmic type, ribosomal P protein and serine protease 3 were weakly positive. But the antibody titer was not high, and the patient had no clinical symptoms, such as rash, joint swelling, or oral ulcers, so connective tissue disease was deemed unlikely. After one week of anti-infection treatment, the clinical symptoms did not improve, and there was no significant change in pulmonary CT which was performed on April 18, 2023. A CT-guided percutaneous lung biopsy was performed to further investigate the right upper lung lesion. mNGS of the biopsy sample suggested the presence of herpesvirus type 4, also known as Epstein-Barr virus, specifically sequence 25, with a relative abundance of 100%, and bacteria, fungi, and parasites were not detected in the sample. The pathological examination of the lung biopsy indicated a small amount of free alveolar epithelial and inflammatory exudation (Figure 2), and the EBV encoded RNAs (EBER) in situ hybridization of this lung biopsy was positive (Figure 3). Studies demonstrated that EBERs are secreted via exosomes by EBV-infected cells.7 At the same time, Blood tests revealed elevated levels of anti-EBV capsid antigen IgG antibody (VCA‐IgG)>750 U/mL (n<20U/mL) and anti-EBV early antigen IgG antibody (EA‐IgG)>10.01 U/mL (n<10.00U/mL), while anti-EBV capsid antigen IgM antibody (VCA‐IgM) and nuclear antigen IgG antibody (EBNA‐IgG) were negative. According to the time of producing corresponding antibodies against different antigens after EBV infection, clinically, serological detections of EBV-specific antibodies are frequently used to identify EBV infection and distinguish infection status. VCA-IgM appeared after the first infection, while EBNA-IgG appeared late, generally at least one month after the primary infection, and along with the appearance of VCA-IgG. VCA-IgG can also be elevated in the reactivated state. Generally, VCA-IgG can serve as an indicator of acute infection or reactivation. EA-IgG can be detected in the first infection and in the state of EBV reactivation. Thus, elevated EA-IgG and VCA-IgG are considered to accurately confirm evidence of acute or convalescent EBV infection generally,8 consistent with this patient’s presentation. The plasma EBV DNA level was measured at 501 gene copies/mL, slightly above the reference value of 500. Positive EBV-DNA in plasma indicates that active EBV infection or diseases closely associated with EBV (eg, early stage of primary EBV infection, EBV associated hemophagocytic lymphohistiocytosis (EBV-HLH), most chronic active EBV (CAEBV), EBV-related tumors, etc). As both BALF and lung biopsy specimen mNGS indicated only EBV, no other pathogens were detected infection, and with the dearth of other positive findings. At last a diagnosis of EBV pneumonia was made. Subsequently the patient was started infusion on acyclovir once every eight hours for one week, with rapid resolution of symptoms. Follow-up lung CT after the antiviral treatment showed a decrease in bilateral lung consolidation, with some reduction in cavitary and interstitial changes (Figure 4). The patient was soon discharged from hospital, and treatment continued with acyclovir orally at a dose of 0.4g every eight hours. Subsequent outpatient follow-up CT performed 12 days after discharge revealed further improvement of the inflammatory lesions, as well as a reduction in cavitary and interstitial changes (Figure 5). Overall, the treatment approach targeting EBV pneumonia with acyclovir led to favorable outcomes in this patient.
Figure 2.
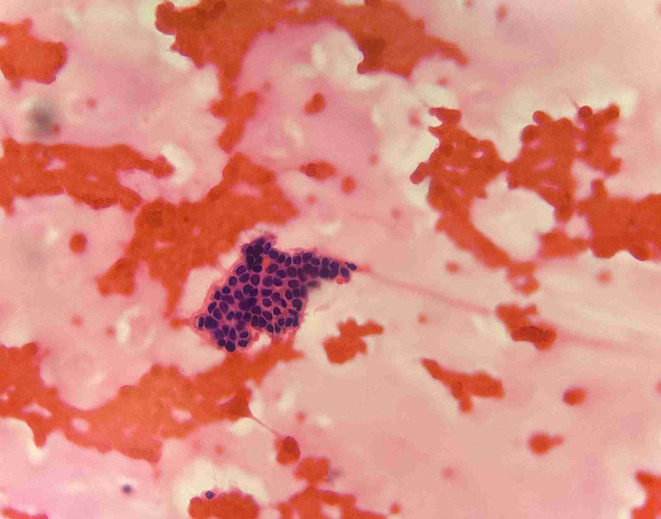
Pathology of the right upper lung biopsy (small amount of free alveolar epithelial and inflammatory exudation).
Figure 3.
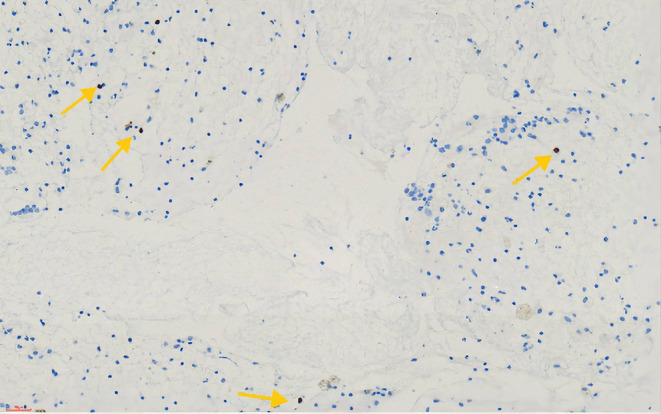
Detection of EBER in lung biopsy tissue, ISH (original magnification ×400, yellow arrow (brown puncta) indicates EBER signal located in the nucleus).
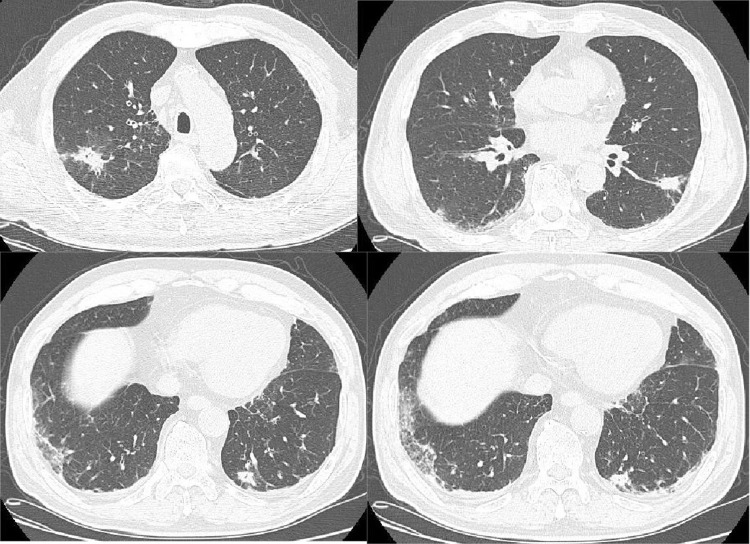
Figure 4.
CT Chest on April 27th, 2023 (a decrease in bilateral lung consolidation, with some reduction in cavitary and interstitial changes compared with CT Chest on April 11th, 2023).
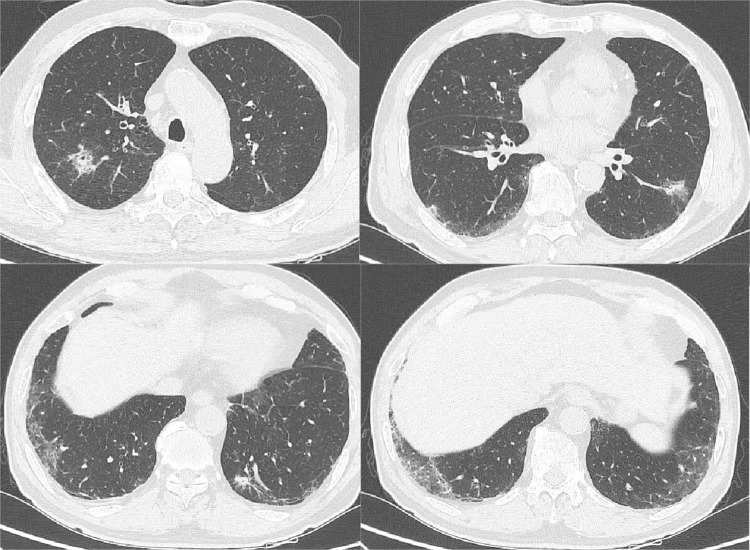
Figure 5.
CT Chest on May 9th, 2023 (further improvement of the inflammatory lesions, more reduction in cavitary and interstitial changes compared with CT Chest on April 27th, 2023).
Discussion and Conclusions
EBV infection primarily affects children between the ages of 3 and 5, and it can affect various systems of the body, leading to heterogeneous clinical manifestations.1 Current evidence suggests that approximately 50% of adolescents infected with EBV can develop infectious mononucleosis. Serological studies have also identified associations between EBV infection and conditions such as Burkitt lymphoma, nasopharyngeal carcinoma (NPC), and gastric cancer. EBV infection is ubiquitous, and about 95% of older adults worldwide have been infected.9 In only rare cases, individuals fail to resolve and control EBV infection, resulting in the development of chronic active EBV (CAEBV)disease.10 During CAEBV infection, EBV-positive lymphocytes infiltrate different organs, increase the viral load in the blood and leading to fever and splenomegaly. While EBV can cause viral pneumonia and invade the lungs, the incidence of pneumonia resulting from EBV infection is generally lower compared to other respiratory viruses like influenza, parainfluenza, and respiratory syncytial viruses. Adult cases of EBV-related pneumonia have been reported infrequently both domestically and internationally.
Previous literature has described manifestations of EBV-related lung diseases, including; ①mediastinal/hilar lymph node enlargement: the EBV infection mainly involves the lymphatic system, and often presents as mediastinal/hilar lymphadenopathy, leading to associated lymphadenitis;6,11 ②interstitial pneumonia: On CT-chest, most manifestations include ground glass density opacification, perilymphatic nodules, irregular thickening of lobular septa, nodules along the the bronchovascular bundle and subpleural nodules, which can be combined with bronchial vascular bundle thickening and intralobular septal thickening;6,12 ③pleural effusion. Among these manifestations, mediastinal lymph node enlargement is the most observed imaging abnormality, while interstitial lung infiltration and extensive ground glass density patches are relatively rare.13 In this case, the chest CT showed multiple patchy solid and ground glass opacification in both lungs, partial cavitary formation, and subpleural mesh lattice changes in the lower lobe of both lungs. The images were not typical of viral pneumonia, but the blood tests revealed elevated levels of anti-EBV capsid antigen IgG, anti-EBV early antigen IgG antibody and EBV DNA, which were considered as the evidence of EBV acute infection or reactivation state. EBER in situ hybridization in lung biopsy tissue showed positive results, which could be considered the gold standard for the detection of EBV in tissue samples. Currently, the main diagnosis of EBV infection mainly relies on EBV-specific antibody detection, heterophile antibody tests, quantitative EBV DNA measurement, and EBER in situ hybridization.14 Furthermore the BALF mNGS and lung biopsy mNGS both detected unique EBV. All these investigations supported EBV pneumonia, and the lung lesions resolution after antiviral treatment further confirmed the diagnosis.
The role of EBV as an infectious pathogen in the development of lung disease is controversial,15 and few reports have documented EBV-induced lung infections. The clinical imaging findings in the presented case were highly distinctive and have not been documented in either domestic or international literature. This uniqueness could have potentially contributed to misdiagnosis or overlooked diagnosis. Ultimately, the diagnosis was confirmed with mNGS. Compared to traditional detection techniques, mNGS offers distinct advantages in diagnosing difficult and critical cases involving pathogenic pathogens. In clinical practice, mNGS is more commonly employed for the diagnosis of challenging and critical patients, particularly those with immune deficiencies or infections involving various pathogens, including rare or novel pathogens. mNGS enables accurate identification of mixed infections, rare pathogens, and unique pathogens in a timely manner.16–18
In this case, BALF may have been contaminated during the collections, but the sterility of percutaneous aspiration lung biopsy is well maintained, which improves the accuracy of pathogen detection. Compared with BALF, percutaneous puncture lung biopsy has higher accuracy and greater clinical reference value but is significantly more invasive.
Some questions remain in this case, including the lack of significant intranuclear or intracytoplasmic viral inclusions on histological examination.
Acknowledgments
We would like to acknowledge the patient and his family, who provided their informed consent for this publication.
Funding Statement
No funding was received from any public, commercial, or non-profit organization for this research.
Abbreviations
EBV, Epstein-Barr Virus; BALF, bronchoalveolar lavage fluid; mNGS, metagenomic next-generation sequencing; CT, Computed tomography.
Data Sharing Statement
All relevant data has been presented in the manuscript and further inquiry can be directed to the corresponding author.
Ethics Approval and Consent to Participate
Written informed consent for the publication of the publication of case details and accompanying images was obtained from the patient. And the consent form is available for reviewing by the editor when needed. Details of the case and any accompanying images can be published without institutional approval.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Damania B, Kenney SC, Raab-Traub N. Epstein-Barr virus: biology and clinical disease. Cell. 2022;185(20):3652–3670. doi: 10.1016/j.cell.2022.08.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sarwari NM, Khoury JD, Hernandez CM. Chronic Epstein Barr virus infection leading to classical Hodgkin lymphoma. BMC Hematol. 2016;16:19. doi: 10.1186/s12878-016-0059-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ok CY, Li L, Young KH. EBV-driven B-cell lymphoproliferative disorders: from biology, classification and differential diagnosis to clinical management. Exp Mol Med. 2015;47(1):e132. doi: 10.1038/emm.2014.82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Joo EJ, Ha YE, Jung DS, et al. An adult case of chronic active Epstein-Barr virus infection with interstitial pneumonitis. Korean J Intern Med. 2011;26(4):466–469. doi: 10.3904/kjim.2011.26.4.466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gautschi O, Berger C, Gubler J, Laube I. Acute respiratory failure and cerebral hemorrhage due to primary Epstein-Barr virus infection. Respiration. 2003;70(4):419–422. doi: 10.1159/000072908 [DOI] [PubMed] [Google Scholar]
- 6.Xin H, Zhigang Y, Yuhuan F, et al. Analysis of chest high-resolution CT characteristics in patients with pulmonary infection caused by EB virus infection. Beijing Med. 2022;44(3):236–240. [Google Scholar]
- 7.Nanbo A, Kawanishi E, Yoshida R, Yoshiyama H. Exosomes derived from Epstein-Barr virus-infected cells are internalized via caveola-dependent endocytosis and promote phenotypic modulation in target cells. J Virol. 2013;87(18):10334–10347. doi: 10.1128/JVI.01310-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gulley ML. Molecular diagnosis of Epstein-Barr virus-related diseases. J Mol Diagn. 2001;3(1):1–10. doi: 10.1016/S1525-1578(10)60642-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chan KA, Woo JK, King A, et al. Analysis of plasma Epstein-Barr virus DNA to screen for nasopharyngeal cancer. N Engl J Med. 2018;378(10):973. doi: 10.1056/NEJMx180004 [DOI] [PubMed] [Google Scholar]
- 10.Kimura H, Fujiwara S. Overview of EBV-associated T/NK-cell lymphoproliferative diseases. Front Pediatr. 2019;6:417. doi: 10.3389/fped.2018.00417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang WJ, Tang XX. Virus infection induced pulmonary fibrosis. J Transl Med. 2021;19(1):496. doi: 10.1186/s12967-021-03159-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McManus TE, Coyle PV, Lawson J, Elborn JS, Kidney JC. Epstein - Barr virus Pneumonitis. Ulster Med J. 2009;78(2):137–138. [PMC free article] [PubMed] [Google Scholar]
- 13.Koo HJ, Lim S, Choe J, Choi SH, Sung H, Do KH. Radiographic and CT features of viral Pneumonia. Radiographics. 2018;38(3):719–739. doi: 10.1148/rg.2018170048 [DOI] [PubMed] [Google Scholar]
- 14.Gulley ML, Tang W. Laboratory assays for Epstein-Barr virus-related disease. J Mol Diagn. 2008;10(4):279–292. doi: 10.2353/jmoldx.2008.080023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kerr JR. Epstein-Barr virus (EBV) reactivation and therapeutic inhibitors. J Clin Pathol. 2019;72(10):651–658. doi: 10.1136/jclinpath-2019-205822 [DOI] [PubMed] [Google Scholar]
- 16.Miao Q, Ma Y, Wang Q, et al. Microbiological diagnostic performance of metagenomic next-generation sequencing when applied to clinical practice. Clin Infect Dis. 2018;67(suppl_2):S231–S240. doi: 10.1093/cid/ciy693 [DOI] [PubMed] [Google Scholar]
- 17.van Rijn AL, van Boheemen S, Sidorov I, et al. The respiratory virome and exacerbations in patients with chronic obstructive pulmonary disease. PLoS One. 2019;14(10):e0223952. doi: 10.1371/journal.pone.0223952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zou X, Tang G, Zhao X, et al. Simultaneous virus identification and characterization of severe unexplained pneumonia cases using a metagenomics sequencing technique. Sci China Life Sci. 2017;60(3):279–286. doi: 10.1007/s11427-016-0244-8 [DOI] [PMC free article] [PubMed] [Google Scholar]