Abstract
Purpose:
The purpose of this study was to investigate the extent to which a naturalistic communication intervention, Enhanced Milieu Teaching with Phonological Emphasis (EMT + PE) improved the speech outcomes of toddlers with cleft palate with or without cleft lip (CP ± L)
Method:
This study was a stratified randomised controlled trial.
Setting:
Treatment was delivered in a university clinic by a trained speech-language pathologist.
Thirty children aged between 15 and 36 months (M = 25) with nonsyndromic CP ± CL and typical cognitive development were randomly assigned to a treatment (EMT + PE) or business as usual comparison condition.
Participants in the EMT+PE treatment group received 48, 30-min sessions, over a 6-month period. Fidelity of treatment was high across participants.
The primary outcome measures were percent consonants correct (PCC), consonant inventory, compensatory articulation errors, and nasal emission.
Result:
Regression analyses controlling for pre-intervention child characteristics were conducted for PCC and consonant inventory. Intervention was not a significant predictor of post-intervention outcome. Words per minute differentiated the children who benefitted from the intervention from those who did not. Reduction in compensatory errors and nasal emission occurred in both groups but to a greater degree in the EMT+PE group.
Conclusion:
EMT + PE is a promising early speech intervention for young children with CP ± L, especially for children with higher rates of word use.
Keywords: nonsyndromic cleft palate, speech development, speech disorders
Introduction
Early speech and language development in children with cleft palate with or without cleft lip (CP ± L) is characterised by delays in the onset and complexity of canonical babbling and slow early development of vocabulary and speech sound development (Chapman, Hardin-Jones, & Halter, 2003; Chapman, Hardin-Jones, Schulte, & Halter, 2001). Some children appear to make progress on their speech and language milestones following palate repair without intervention, while others continue to show delays or differences in their speech and/or language performance. Research to date has provided possible factors that affect early speech and language development for children with CP ± L (Chapman et al., 2001; Scherer, 1999) and identified skills predictive of communication outcomes.
Limitations in consonant inventory that are characteristic of children with CP ± L may limit the differentiation of vocabulary acquisition due to the restrictions in the sounds available for early words (Scherer, Williams, Stoel-Gammon, & Kaiser, 2012). Studies suggest that young children with CP ± L show slower early vocabulary development and increased lexical selectivity; they produce more words beginning with nasals, glides, and vowels than words with high-pressure consonants (Chapman et al., 2003; Scherer, 1999; Scherer, Williams, & Proctor-Williams, 2008). These speech sound limitations reduce intelligibility, which, in turn, may reduce children’s communicative attempts using words (Scherer, Boyce, & Martin, 2013). When children make fewer communicative attempts using words, they have fewer opportunities to practice sound production and to receive feedback from their communicative partners (Frey, Kaiser, & Scherer, 2018).
In previous research, when language intervention was used to bootstrap speech sound production, young children with CP ± L made gains in both vocabulary and phonologic acquisition; however, these few studies have limitations in the description of the intervention, fidelity measurement, and/or absence of a comparison group (Ha, 2015; Pamplona, Ysunza, & Ramirez, 2004; Scherer, 1999; Scherer, D’Antonio, & McGahey, 2008). The limitations of these published studies restrict the interpretation of early intervention effects and decision-making regarding recommendations for intervention timing, dosage, and approach.
The effects of Enhanced Milieu Teaching (EMT) have been documented over a wide range of language targets, including vocabulary and word combinations, across populations of children with language, behaviour, or cognitive challenges (Kaiser, Scherer, Frey, & Roberts, 2017; Kaiser & Roberts, 2013; Peredo, Zeyala, & Kaiser 2017). The impact of EMT on speech development, however, has been less studied but is of interest for a number of clinical populations receiving early intervention. Camarata (2010) used naturalistic early intervention augmented with speech recasting to improve both language and speech in children with speech sound disorders, Down syndrome, and autism. The proximity of the adult model to the child production within a functional context provides an opportunity for the child to compare the model to his/her production. Scherer (1999) assessed the effects of EMT on a set of broad speech recasts for three children with cleft palate. No specific sounds were targeted within the target vocabulary. This study shows the impact of vocabulary expansion on speech production even without targeting specific sounds.
Enhanced Milieu Teaching with Phonological Emphasis (EMT+PE) is a specific modification of traditional EMT that was adapted to address the specific needs of young children with both speech and language delays (Scherer & Kaiser, 2010). The phonological emphasis (PE) integrates speech recasting strategies within the EMT language modelling and prompting strategies. Speech production criteria are included in the procedures for selecting speech and language intervention targets. Speech recasting has been an effective naturalistic strategy for improving young children’s speech accuracy and intelligibility and may address the particular speech production deficits common in children with clefts (Camarata, 2010).
EMT + PE includes four components: (a) Environmental Arrangement which involves arranging the physical and social context to maintain child interest and engagement and optimise opportunities to prompt language; (b) Responsive Interaction strategies that balance turns, mirror child nonverbal play and communicative behaviours as an opportunity for modelling, respond to child communicative initiations with models, and expand children’s utterances; (c) Milieu Teaching episodes that prompt children to use target vocabulary and increase intelligibility with elicited modelling, time delay, and incidental teaching; and (d) Speech Recasting to provide feedback and models for correct production of children’s target sounds. EMT+PE attempts to increase consonant inventory and vocabulary development concurrently by selecting words that incorporate target speech sounds, increasing child rate of talking, modelling correct phonological and semantic forms, and providing contingent semantic and phonological feedback from an adult.
Kaiser et al. (2017) reported the language and broad speech outcomes of a pilot study comparing EMT + PE intervention to a “business-as-usual” (BAU) comparison for children under three years of age with nonsyndromic CP ± L. The children receiving the EMT+PE intervention showed significant pre- to post- intervention gains in receptive language, expressive vocabulary skills, and percent consonants correct (PCC) in comparison to the gains by the comparison group. Significant differences between groups were not found for number of different words (NDWs) used per minute, complexity of language use as measured by mean length of utterance in morphemes (MLUm), rate of communication, as measured by the number of vocalisations per minute, or expressive language scores on the Pre-school Language Scales – Fourth Edition (PLS-4). Effect sizes, however, for all language and speech measures were positive and ranged from 0.04 to 0.65, indicating that children in the EMT+PE group performed better at the end of the study than children in the BAU group on vocabulary and speech accuracy measures. This study extended the findings from Kaiser et al. (2017) through conducting a more in-depth analysis of the treatment effects on speech skills.
The purpose of this study was to examine the specific speech outcomes for toddlers with CP ± L who received the EMT + PE early intervention compared to a group of children assigned to the comparison group. The following research questions were addressed:
Does intervention condition predict post intervention PCC and consonant inventories after controlling for pre-intervention child characteristics?
Are pre-intervention child characteristics (i.e. speech, word rate, and/or vocabulary) correlated with post-intervention speech outcomes (i.e. PCC and consonant inventory)?
What are the observed changes in place, manner of articulation features, audible nasal emission (ANE) and compensatory articulation for children in the EMT+PE and BAU groups following intervention?
Method
A small, stratified, randomised group design study was conducted to evaluate the effects of EMT + PE on the speech of young children with nonsyndromic, repaired CP ± L.
Participants
Thirty children with CP ± L were enrolled in this study; 15 were randomly assigned to the EMT + PE intervention (Age M = 23.13 months) and 15 to the “business as usual” (BAU) comparison group (Age M = 24.07 months). BAU comparison groups are those in which children may attend the same or similar interventions available in the community.
Children were recruited for participation in the study at two sites in the southeastern United States continuously between December 2009 and June 2012. Children were included in this study if they (a) were between 15 and 36 months old; (b) had a cognitive scale composite score of 80 or above on the Bayley Scales of Infant and Toddler Development-III (Bayley-III; Bayley, 2006); (c) could produce at least five different words per parent report on the MacArthur-Bates Communicative Development Inventory (MCDI; Fenson et al., 2007); and (d) were considered at-risk for speech and language delay based on their errors on the Profiles of Early Expressive Phonology (PEEPS; Stoel-Gammon & Williams, 2013). Children were excluded from the sample if they (a) had a sensorineural hearing loss or sound field hearing threshold over 30dB HL, as measured by an audiologist or confirmed by the medical record; (b) were multilingual or non-English speaking based on parent report; (c) had a syndrome diagnosis from a geneticist; and/or (d) had more than three additional dysmorphic features in addition to the cleft palate (Jones, 1988). Table I shows participant characteristics for the EMT + PE intervention and BAU comparison group. After the initial screening, children who met the inclusion criteria were assigned to the EMT + PE or BAU comparison group using a random number generator for assignment.
Table I.
Demographic characteristics of the groups at preintervention.
| EMT + PE | BAU | |
|---|---|---|
| Sample size | 15 | 15 |
| Gender | ||
| Male | 8 (53.33%) | 10 (66.67%) |
| Female | 7 (46.67%) | 5 (33.33%) |
| Race/ethnicitya | ||
| Caucasian | 12 (80%) | 11 (73.33%) |
| African-American | 0 | 1 (6.67%) |
| Hispanic | 0 | 1 (6.67%) |
| Asian | 3 (20%) | 1 (6.675) |
| Cleft palate type | ||
| Cleft palate only | 4 (26.67%) | 4 (26.67%) |
| Unilateral CL/P | 8 (53.33%) | 8 (53.33%) |
| Bilateral CL/P | 3 (20%) | 3 (20%) |
| Age of palate repaira,b | 12.47 (4.10) | 10.54 (1.73) |
| Range | [9, 25] | [7, 14] |
| Mother’s education levela | ||
| GED | 1 (6.67%) | 0 |
| High school | 3 (20%) | 0 |
| Some college or 2-year degree | 4 (26.67%) | 4 (26.67%) |
| 4-year degree or more | 7 (46.67%) | 10 (66.67%) |
| Annual gross incomea | ||
| <$25,000 | 0 | 2 (13.33%) |
| $30,000–$74,999 | 7 (46.67%) | 6 (40%) |
| ≥$75,000 | 8 (53.33%) | 6 (40%) |
Notes. EMT+PE: Enhanced Milieu Teaching with Phonological Emphasis; BAU: business as usual; CL/P: cleft lip/palate; GED: General Educational Development.
One record was not completed for participant in BAU group.
Mean (standard deviation) [minimum, maximum]. Count (percentage).
Procedures
Pre-post assessment
All children received a comprehensive assessment of speech and language skills prior to and following intervention. The Bayley Scales of Infant Development III- Cognitive subtest (Bayley, 2006) was administered to all participants during the pre-intervention assessment only. The PLS-4 (Zimmerman, Steiner, & Pond, 2002), a standardised, norm-referenced assessment, was individually administered to assess children’s receptive and expressive language skills before and after intervention. Children’s language skills were also assessed through 30-min, naturalistic, play-based language samples (LS) with a trained clinician and parent–child interaction (PCX) sessions in the clinic (Miller & Chapman, 2009). In addition to the standardised, norm-referenced and observational measures, parents completed the MCDI (Fenson et al., 2007) as a measure of expressive vocabulary before and after intervention. The PEEPS (Stoel-Gammon & Williams, 2013) was the primary speech measure used throughout the study. The phonetic transcriptions of the PEEPS were used to calculate PCC, consonant inventory, and ANE (Scherer et al., 2012). Toys representing each word are available in Supplementary Table 1.
During the assessment, children wore a digital recorder inserted in a vest to ensure high-quality recordings of their speech. The session also was video and audio recorded. After the session, each child response on the PEEPS was phonetically transcribed using the international phonetic alphabet while listening to the digital recording and viewing the video recording.
BAU comparison group
The children in the comparison group did not participate in any of the experimental intervention (EMT + PE) sessions but did participate in routine follow-up through their local cleft palate team. Participants’ cleft palate teams and community intervention providers received copies of the assessments performed in this study. Six children in the comparison group received community-based early intervention services, per parent report, during the study period. Six of the 15 children received communitybased services in their homes once monthly for 4–6 months during the study.
EMT + PE group
Children in the EMT + PE treatment group received intervention during individual, 30-min play sessions, twice weekly, in a clinic room. Children participated in a total of 48 intervention sessions over the course of about 6 months. The intervention was provided with two licenced speech-language pathologists (SLPs), one at each of the collaborating sites. Parents were permitted to be in the room during the assessments and intervention or in an observation room during the session; however, the parents were not specifically trained to administer the intervention. The children received routine follow-up by their craniofacial teams but no other speech-language or early intervention during the EMT + PE intervention. Procedures for implementing EMT + PE included are described in detail in Kaiser et al. (2017). A description of the strategies and fidelity criterion is included in Supplementary Table 2.
Intervention target selection
Five speech targets were identified from the PEEPS pre- test results for each participant. These were embedded in single and multiple word target language levels. Speech targets were identified after reviewing the PEEPS analyses and were selected based on the guidelines included in PetersonFalzone, Hardin-Jones, and Karnell (2001). Nasals, stops, and fricatives were given priority as target sounds, anterior place of articulation was targeted before posterior place of articulation, and pre-vocalic positions were addressed before post-vocalic position. The target words were chosen based on their syllable structure in the PEEPS assessment (i.e. CV, VC, CVC, CVCV, CVCVC), recommendations from the parent regarding use in the home environment and ease with which they could be incorporated into age appropriate play. Typical word targets included names for objects, actions, or locations that began with stop and fricative consonants.
Treatment fidelity
Before beginning the study, clinicians received extensive training on EMT + PE intervention through practice in the clinic with children with CP+/−L and/or other language impairments not enrolled in the study, review of written materials (research articles, chapters describing the intervention, handouts summarising intervention strategies), review of video examples of the intervention implemented by other therapists, and practice with coaching and feedback from senior therapists experienced in the components of the intervention. Data were summarised for each component category and reviewed in relation to established fidelity criterion in EMT research literature (see Kaiser & Hampton, 2017).
Reliability
The SLP was knowledgeable of group assignment. To control for potential bias, child responses on the PEEPS were scored independently a second time by the first author, who was blind to group assignment. Point-to-point agreement was calculated for all of the items on each PEEPS assessment for each child. Disagreements in consonant transcription were resolved by consensus. The first coder also re-transcribed 50% of each sample to assess intraobserver agreement. Intra- and inter-judge reliability was assessed for 50% of the total PEEPS transcriptions; reliability for coding place and manner agreements, compensatory articulation, and nasal emission was calculated separately. Intra-judge PEEPS transcription reliability was 92–95% agreement, and interjudge rating was 87–90% across the two time points for total transcriptions. Both place and manner features showed intra-judge reliability of 97–98% agreement and inter-judge reliability of 95–98% across the two time points. Reliability of compensatory errors and ANE are reported separately since they are often problematic. Intra- and inter-judge reliability for compensatory articulation agreement was 90–92% and 85–89%, respectively. Intra- and inter-judge reliability for ratings of nasal emission were 86–88% and 78–85%.
All intervention and interaction assessment sessions were video recorded, transcribed, and then coded. Average percentage of agreement for each coding category was as follows: 80% (SD = 9.3) for child language targets, 97% (SD = 3.98) for matched/unmatched turns, 86% (SD = 5.41) for recasts/expansions, and 88% (SD = 6.60) for therapist language level. If agreement was below 85% on any coding category within any session, the two coders met to review and discuss each coding discrepancy before coding any additional intervention sessions.
Data analysis
Assessment data were double entered independently by two research assistants into a database, and any disagreements in data entry were resolved by consensus. Demographic information and assessment data were summarised using appropriate descriptive statistics, and group differences at pre-intervention were examined. Data analyses were conducted in R (R Core Team, 2018) using ggplot2 (3.1.0; Wickham, 2016) and ez (4.4–0; Lawrence, 2016).
For Research Question 1, we conducted a general linear model (GLM) regression analysis, which is a statistical procedure to examine the predictive relationship between one or more independent variables and a dependent variable (e.g. post-intervention PCC). We examined the predictive power of experimental condition, NDWs, and words per minute (WPM), controlling for number of words produced on pre-test and age, for post-intervention PCC and consonant inventory. All predictors were entered into the model simultaneously, as there were no predictions about the unique or increasing contribution of a single predictor. NDW and WPM were based on transcripts of the 20-min PCX observation at pretest. These predictors were selected a priori based on previous studies using a portion of the data presented here (Frey et al., 2018; Kaiser et al., 2017). NDW, WPM, and pre-intervention consonant inventory were all highly correlated with one another suggesting the presence of multicollinearity; however, all predictors were included in the model as they represented unique theoretical constructs.
To address Research Question 2, we examined the correlations among pre-intervention characteristics and post-intervention PCC and consonant inventories. For Research Questions 3 and 4, we completed a descriptive analysis of change from pre to post intervention for ANE (Research Question 3) and for changes in place and manner of articulation features and percentage of compensatory articulation (Research Question 4) for children in the EMT + PE and comparison groups.
Result
Descriptive statistics of pre-intervention characteristics for Enhanced Milieu Teaching with Phonological Emphasis group (EMT + PE) and Business as Usual group (BAU) are presented in Supplementary Table 3. Linear regression statistics, examining predictors of treatment response, are presented in Table II. Results of the correlation analyses, examining the relationship between child characteristics and post-intervention speech outcomes, are provided in Supplementary Table 4. Table III and Supplementary Table 5 present data associated with our post hoc descriptive analyses.
Table II.
General linear regression model statistics for post-intervention speech outcomes.
| Variable | B | SEB | β | t | p |
|---|---|---|---|---|---|
| Percent consonant correct | |||||
| Constant | 17.76 | 13.72 | - | 1.29 | 0.21 |
| Pre-test score | 0.93 | 0.26 | 0.71 | 3.58 | 0.001 |
| Age | −0.19 | 0.63 | −0.05 | −0.29 | 0.77 |
| Treatment condition (EMT + PE) | 7.85 | 6.94 | 0.16 | 1.13 | 0.26 |
| Number of different words | −0.46 | 0.50 | −0.29 | −0.92 | 0.37 |
| Rate of speaking | 2.42 | 1.37 | 0.52 | 1.76 | 0.37 |
| Adj. R2 | 0.59 | ||||
| F (5, 24) | 9.31 (p = 0.0000) | ||||
| Consonant inventory | |||||
| Constant | 10.68 | 4.47 | - | 2.39 | 0.03 |
| Pre-test score | 1.02 | 0.36 | 0.90 | 2.80 | 0.009 |
| Age | −0.09 | 0.23 | −0.08 | −0.42 | 0.68 |
| Treatment condition (EMT + PE) | 1.71 | 2.29 | 0.10 | 0.74 | 0.46 |
| Number of different words | −0.18 | 0.19 | −0.34 | −0.88 | 0.38 |
| Rate of speaking | 0.46 | 0.47 | 0.30 | 0.98 | 0.33 |
| Adj. R2 | 0.56 | ||||
| F (5, 24) | 7.95 (p = 0.0001) |
Note. EMT+PE: Enhanced Milieu Teaching with Phonological Emphasis; B: unstandardised β estimate; SE B: standard error of unstandardised β; β: standardised β estimate; t: t-statistic estimate; p:p-value estimate.
Table III.
Pre-intervention characteristics by treatment condition and rate of speaking grouping.
| Treatment condition | ||||
|---|---|---|---|---|
|
|
||||
| EMT + PE | BAU | |||
|
|
|
|||
| Variable | Low-rate (<10 words per min) | High-rate (>10 words per min) | Low-rate (<10 words per min) | High-rate (>10 words per min) |
| Age (months) | 20.50 (4.93) [13, 30] | 28.40 (3.85) [25, 33] | 21.80 (7.84) [15, 35] | 28.60 (3.85) [24, 34] |
| Parent report vocabulary (CDI raw) | 54.60 (62.72) | 314.80 (179.26) | 163.40 (251.34) | 405.25 (260.27) |
| Number different words (PCX) | 5.80 (4.12) | 28.60 (16.10) | 8.20 (8.93) | 38.80 (10.40) |
| Words per minute (PCX) | 3.54 (3.06) | 13.30 (1.45) | 3.36 (2.94) | 13.77 (2.56) |
| Pre-intervention total PCC (PEEPS) | 18.70 (12.92) | 41.60 (19.11) | 33.8 (16.69) | 55.2 (13.33) |
| Pre-intervention consonant inventory (PEEPS) | 4.40 (4.27) | 12.60 (5.31) | 6.40 (6.22) | 19.60 (4.16) |
Note. Mean (standard deviation). [minimum, maximum]. EMT + PE: Enhanced Milieu Teaching with Phonological Emphasis; BAU: business as usual; CDI: MacArthur-Bates Communicative Development Inventory (Fenson et al., 2007); PCX: parent–child interaction; PCC: total percent consonants correct; PEEPS: profiles of early expressive phonology (Stoel-Gammon & Williams, 2013).
Pre-intervention comparison
No significant differences between groups were observed for age (t(26.66) = −0.38, p = 0.7054, d = −0.14), NDW (t(26.89) = −0.85, p = 0.4051, d = −0.31), WPM (t(27.89) = −0.02, p = 0.9857, d = −0.01), CDI (t(21.46) = −1.08, p = 0.2884, d = 0), or consonant inventory (t(25.23) = 1.37, p = 0.1822, d = −0.50); however, there was a difference for pre-intervention PCC (t(27.99) = −2.17, p = 0.0382, d = −0.79) which indicated that children in the EMT + PE group had lower speech accuracy as measured by PCC at pre-intervention. Supplementary Table 3 presents pre-intervention characteristics by treatment group.
Factors predicting Post-Intervention outcomes
EMT + PE and the BAU groups were compared on post-intervention performance on speech measures using age and pre-intervention performance as control variables.
Pre-intervention NDW and WPM were examined as predictors for the PCC and consonant inventory (Table II). Both regressions were significant (PCC: F (5, 24) = 9.31, p<0.001; consonant inventory: F (5, 24) = 7.95, p <0.001). Treatment condition was not a significant predictor for PCC (t = 1.13, p = 0.2696) or consonant inventory (t = 0.74, p = 0.4643). Models could be simplified by removing pre-intervention NDW and WPM as neither of these predicted post-intervention PCC or consonant inventory and for consonant inventory were highly correlated with pre-intervention scores (r = 0.90 and 0.82, respectively). Although for post-intervention consonant inventory, the assumption of independent predictors was violated, the model does provide us with initial information about which pre-intervention characteristics might predict post-intervention performance.
Relationships between child characteristics and speech outcomes
All pre-intervention variables were significantly correlated with post-intervention PCC and consonant inventories. Pre-intervention PLS scores, PCC, and WPM showed large effect sizes (i.e. r2 > 0.68; Supplementary Table 4). The pre-intervention MCDI raw score and NDW had moderate effect sizes (r2 between 0.60 and 0.65). Small effect sizes differences between groups in age were observed, indicating that age was a relatively poor predictor of later speech outcomes.
Examination of audible nasal emissions
ANE was observed in the speech of three children in the EMT + PE group and two children in the comparison group prior to intervention affecting between 7 and 15% of responses per child. Percent ANE decreased for three children (two in EMT/PE and one in comparison group) to 5–10% at post-intervention; two children (one in EMT/PE and one in comparison group) showed no change in ANE from preto post-intervention, with 7% and 11%, respectively. We do not have definitive information on velopharyngeal function for these children. To date, two of the five children with ANE have had secondary palatal management. One of the children was in the comparison group (11% ANE post-intervention), and one was in the EMT/PE group (5% ANE post-intervention).
Changes in articulation
Treatment group findings
The mean and standard deviation of the change scores for place and manner of articulation was compared for EMT + PE and BAU comparison groups, and no differences were observed between the groups. (The complete data set for the change scores is in Supplementary Table 5). Given the importance of rate of word use as demonstrated by WPM’s high correlation with intervention outcome, we examined the descriptive statistics for WPM in the whole sample (M = 6.81, SD = 5.94, range = [0, 17.10], median = 6.10). Inspection of the data showed that there was a bi-modal distribution, with no scores between 8.20 and 11.20 WPM at pre-intervention. Therefore, we split the treatment and controls samples at 10 WPM and completed a series of post hoc analyses comparing the changes from pre to post intervention for place, manner, and compensatory articulation using the resulting four groups. Means and standard deviations for age, NDW, vocabulary size (as reported by parents on the MCDI), WPM, and pre-intervention speech scores for participants divided into four groups based on number of words at pre-test (EMT + PE: High-rate and Low- rate; BAU: High-rate and Low-rate) are provided in Table III.
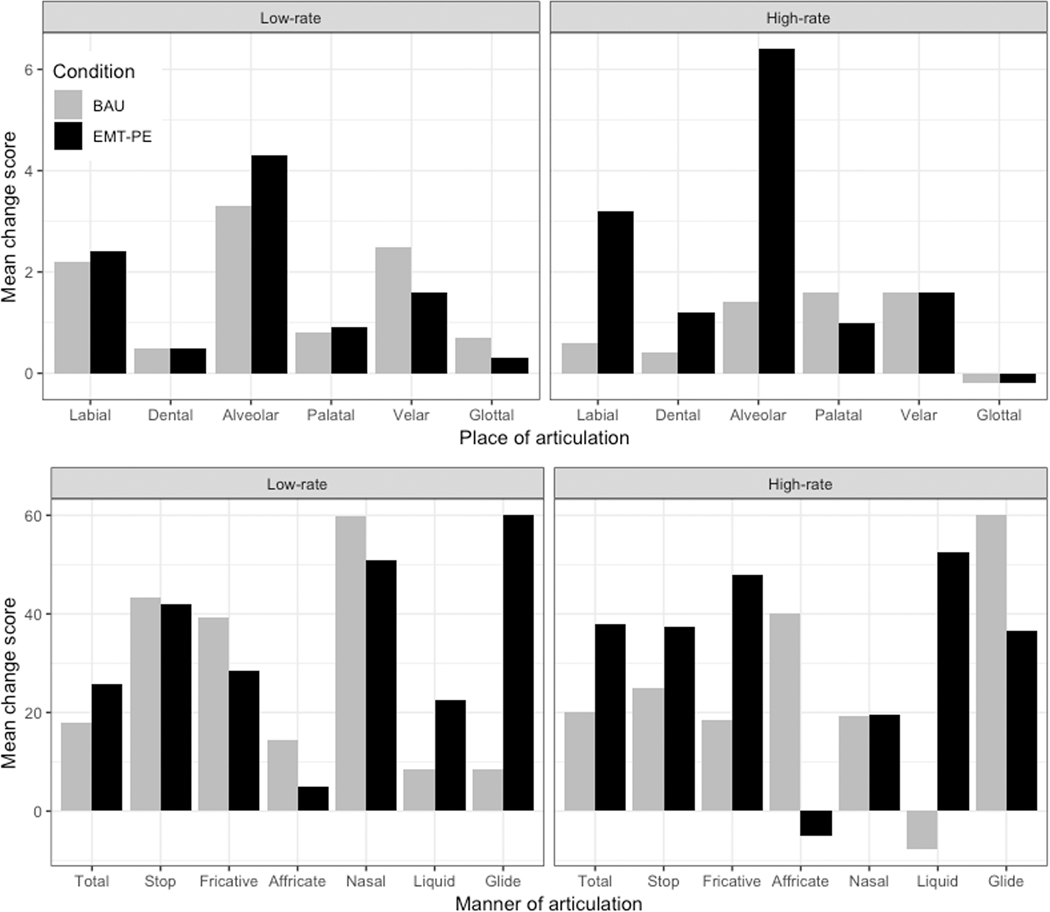
Place and manner
Place and manner of articulation performance for children in the four groups, based on performance on the PEEPS, are presented in Figure 1 and Supplementary Table 5. The complete data set for the change scores is in Supplementary Material. Effect sizes were calculated for the low-rate and high-rate EMT+PE and comparison groups. There were clinically meaningful benefits (i.e. d>0.5) for the low-rate EMT+PE group for changes for liquids (d = 0.58) and glides (d = 0.94) only; all other effect sizes for the low-rate groups were not clinically meaningful and ranged from 0 (dentals) to −0.47 (affricates). Effects sizes indicated that children with a speaking rate of less than 10 WPM had limited benefits of EMT + PE. However, for the high-rate children, EMT + PE resulted in greater change, which was also clinically meaningful. The high-rate intervention group exceeded the comparison group in overall consonants (d = 1.91), and stop (d = 0.79), fricative (d = 1.43), and liquid (d = 2.88) consonants. The greatest gains were observed in the high-pressure consonant categories of stop and fricatives, which were speech targets in this study. In addition, there was an advantage for high-rate children in the EMT+PE intervention for alveolar consonants (d = 2.48) with the EMT + PE group gaining approximately six alveolar consonants while the comparison group gained one from pre- to post-intervention. Effect sizes also revealed clinically meaningful differences in favour of the high-rate EMT + PE group for dental (d = 0.72) and labial (d = 1.73) consonants; other effect sizes ranged from −1.04 (affricates) to zero (velars, glottals, and nasals). The effect sizes for the high-rate group indicate that participation in EMT + PE results in clinically meaningful changes in both manner and place of articulation.
Figure 1.
The gain in number of consonants by place of articulation (top panels) and percent consonants correct (PCC) for manner of production (bottom panels) between pre- and post-intervention on the PEEPS is presented for the Enhanced Milieu Teaching with Phonological Emphasis (EMT + PE) groups (black bars) and the business-as-usual (BAU) groups (grey bars). A positive gain score indicates that children had a higher score at post-test than pre-test on the PEEPS measure. For example, on average the high-rate children in the EMT+PE group produced six more alveolar consonants at post-test than pre-test, while the BAU group produced one more alveolar consonant. Another example is that on average high-rate children in the EMT + PE group gained approximately 40% stop PCC from preto post-test, while the BAU group gained 20% on stop production, a 20% advantage for the EMT + PE group. The data for the low-rate children in each group are presented in the left panels and the high-rate children in the right panels.
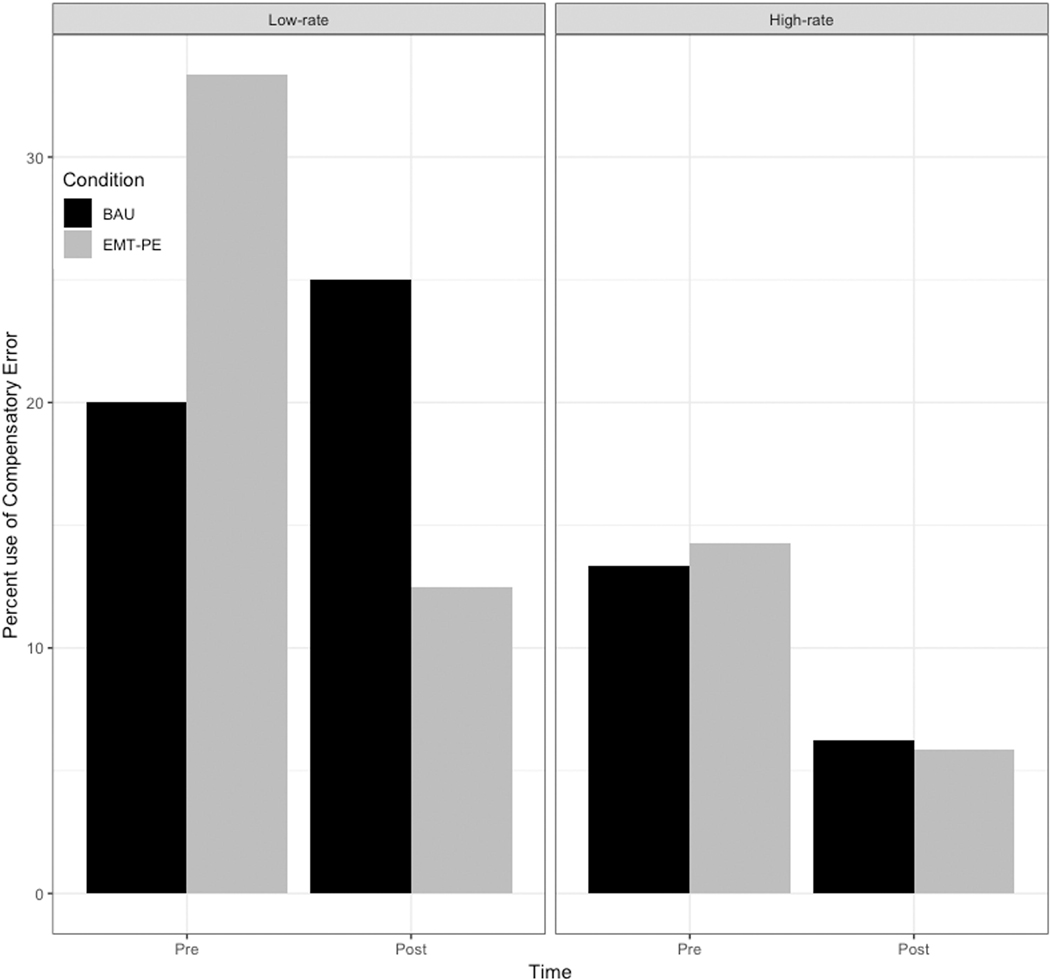
Compensatory articulation
The percent of compensatory substitutions produced pre- and post-intervention by children in each group is presented in Figure 2. The data suggest that children in the EMT + PE group who were low-rate talkers had a greater decrease in the use of compensatory errors from pre-intervention to post-intervention. Children who were high-rate talkers in both EMT + PE and comparison groups showed a reduction in compensatory errors from pre- to post- intervention. For all participants, compensatory errors occurred more often in word final position (86.67% in final position collapsed across time). Examination of the change in use of compensatory errors (glottal stops) was examined in two ways: first, we looked at children who had glottal stops at T0 and what changes occurred at T1. Of the 15 children in the intervention group, 8 of them had some glottal stops at T0 and, although they still were using glottals at T1, they decreased their use of glottals particularly in word final position at T1 by replacing glottals with oral consonants. In addition, three children used some glottals at T1 when they had not used them in T0. These children were those that used very few consonants at T0. We also examined the six children in the BAU group who used glottal stops at T0. As with the TX group, these children continued to have some glottal stop use although they were used less at T1. In addition, three more children used glottal stops at T1 who had not used them at T0. This data suggests that glottal stops were emerging to mark prevocalic, or more often, postvocalic syllables and then declined as oral consonants were added.
Figure 2.
Percent of compensatory substitutions used for pre- and post-intervention for EMT + PE (black bars) and BAU (grey bars). The data for the low-rate children in each group are presented in the left panel and the high-rate children in the right panel.
Discussion
The purpose of this study was to analyse the speech outcomes of children with CP ± L who received an early intervention (EMT + PE) compared with a group of children who were in a BAU comparison group. Overall, there were no significant effects of the intervention on PCC or consonant inventory for the two groups. However, secondary analysis suggests that the children in the EMT + PE group who had higher-rates of word use at pre-intervention (greater than 7–10 WPM) showed more change in their consonant inventories, speech accuracy, and compensatory articulation use from pre- to post-intervention than children in the EMT+PE low-rate group and both the high and low- rate BAU comparison groups.
Predictors of response to treatment
We explored predictors of response to treatment in several different ways, including regression, correlation, and descriptive analysis. The first research question examined the predictive power of pre-intervention treatment outcome, language, and age for post-intervention speech outcomes. The only significant predictor for the regressions was pre-intervention speech performance; however, the small sample size, variability in pre-intervention performance, and possible multicollinearity may have masked important information about predictors of post-intervention outcomes. The second research question correlated pre-intervention language, speech, rate, and vocabulary variables with post-intervention PCC and consonant inventories. The correlational analysis identified several pre-intervention child characteristics that could provide guidance for the application of EMT + PE to young children with CP ± L to maximise speech outcomes. The third research question addressed a descriptive analysis of change in place and manner of articulation following the intervention. The descriptive analysis provided further evidence that speaking rate at pre-intervention was related to who benefitted from EMT + PE intervention.
Speaking rate (WPM), NDWs, and overall vocabulary size showed moderate to large effect sizes as predictors of consonant inventory and speech accuracy following intervention. Studies have shown that consonant inventory and PPC (particularly for high-pressure consonants) for children from 18 to 20 months of age is correlated with later speech outcomes (Chapman et al., 2003). It appears that these same variables are still correlated to intervention outcomes for young children. Of particular interest was the importance of rate before intervention as a predictor of speech outcome. Children who made the largest gains in speech production spoke at a rate of at least 7–10 WPM, had at least 20 total words in the PCX, had 50 words reported by parents on the MCDI, and were 23–33 months of age. These findings suggest that children who do not yet meet these rate and vocabulary size criteria might benefit more from EMT only, focussing on increasing the rate and diversity of spoken language before introducing the speech recasting component. Alternatively, including the PE component did not appear to inhibit speech production. The optimal sequencing of intervention components in naturalistic interventions for this population is an important area for future research.
Children in the EMT + PE group who had a higher rate of words spoken per minute during the PCX showed a greater change in speech sound production from pre- to post-intervention compared to children in the EMT+PE group who had lower WPM and all children in the comparison group. The children in this study responded to the EMT + PE intervention differentially based on pre-intervention WPM used in the parent–child interaction sample (high rate vs. low rate). The low-rate children performed generally the same pre- and post- intervention. Both groups gained consonant inventory and accuracy but to a lesser degree than the high-rate children.
The rate at which children use words in conversation is a critical factor affecting children’s opportunities to learn from adult responses and feedback. The dosage of an early naturalistic speech-language intervention depends to a certain extent on the frequency and quality of the opportunities to respond to child utterances with meaningful input that presents expanded language models and provides corrective feedback for speech production. Frey et al. (2018) examined the rate of caregivers’ responses to intelligible and unintelligible speech from young children with and without CP ± L. Although all caregivers were highly responsive, they found significant differences in child intelligibility and rate of spoken language (as measured by WPM) between toddlers with and without CP ± L. More specifically, children with CP ± L produced 50 words less and received 90 words less of adult input than noncleft children in a 10-min sample of caregiver–child interaction (because children with CP ± L provided fewer opportunities for caregivers to respond). Over time, reduced frequency of meaningful, semantic input from the adult communicative partner may provide children with CP ± L fewer opportunities to learn new language compared to noncleft children (Frey et al., 2018). Rate of word production is particularly important when providing feedback for speech production. In this study, it likely that the children who gained the most in speech production were those high-rate talkers who received phonological feedback and models of correct production via the recasting component of the EMT + PE intervention. For lowrate talkers, it may be more beneficial to focus first on increasing the rate of and diversity of spoken words before focussing on speech production. It may be important to build a language and communication foundation to support the use of naturalistic strategies that promote speech production, such as speech recasting.
The specific speech performance outcomes for the children in the high-rate EMT + PE group included greater gains in consonants with alveolar, labial, and dental placements than observed for the children in the high-rate comparison group. Alveolar place of articulation has been described as problematic for young children with CP ± L (Klinto et al., 2014). Thus, this exploratory evidence of gains on acquisition of consonants with alveolar place of articulation is a potentially important outcome of the intervention. The target sounds in the EMT + PE intervention contained predominantly stop and fricative consonants; however, six of the eight target stop or fricative consonants had labial and alveolar placements. In addition to place of articulation gains, the children in the high-rate EMT + PE group made gains greater than the comparison group for speech accuracy, particularly in the stop and fricative manners of articulation. These two manners of articulation require production of high oral air pressure necessitating adequate velopharyngeal function. Children in the comparison group showed better growth in affricates; however, few children in either the EMT + PE or the comparison groups used affricates. Overall, the data suggest improvements in speech accuracy and increases in number of consonants following EMT + PE; however, changes in speech accuracy were not necessarily linear. In other words, children added or substituted new nontarget sounds before they acquired the targeted sound production. This pattern reflects the early stage of phonological acquisition in which children are adding and eliminating phonological processes (Sosa & Stoel-Gammon, 2012).
Limitations and future research
Sample size was a limitation of this study. A larger clinical trial with multiple sites is needed to address the dosage and timing of strategies in the intervention. In addition, pre-intervention PCC influenced the treatment response and, therefore, future studies should use random assignment to groups stratified by PCC level to minimise the effect of speech disorder severity. In addition, we used a new phonological assessment measure (PEEPS) because there are few standardised measures available for this age range. PEEPS has a small normative sample and limited validity and reliability data.
In addition, it is likely that active coaching of parents to implement the intervention would also improve outcomes by increasing the dosage of the intervention in contexts where children are motivated to talk with familiar communication partners (Roberts & Kaiser, 2011). Although this study did not train parents as intervention agents, the parents in the intervention group did have the opportunity to observe the intervention with their child and the clinician. Passive observation of intervention may have an impact on parent interaction with their child; however, parental behaviours were not measured in this study. However, a combined clinician plus parent model, similar to Roberts and Kaiser (2011), Roberts, Kaiser, Wolfe, Bryant, & Spidalieri (2014), might provide greater benefits for the child and support parents in interacting with their children.
Supplementary Material
Funding
This work was supportd by National Institute on Deafness and Other Communication Disorders [1R21DCOO9654].
Footnotes
Supplementary material
Supplemental data for this article is available online at at http://dx.doi.org/10.1080/17549507.2019.1702719
References
- Bayley N. (2006). Bayley scales of infant development-III. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Camarata S. (2010). Naturalistic intervention for speech intelligibility and speech accuracy. In Williams L, McLeod S, McCauley R. (Eds.). Interventions for speech sound disorders in children. Baltimore, MD: Brookes Publishing. [Google Scholar]
- Chapman KL, Hardin-Jones M, & Halter KA (2003). The relationship between early speech and later speech and language performance for children with cleft lip and palate. Clinical Linguistics & Phonetics, 17, 173–197. doi: 10.1080/0269920021000047864 [DOI] [PubMed] [Google Scholar]
- Chapman KL, Hardin-Jones M, Schulte J, & Halter K. (2001). Vocal development of 9- month-old babies with cleft palate. Journal of Speech, Language, and Hearing Research, 44, 1268–1283. doi: 10.1044/1092-4388(2001/099) [DOI] [PubMed] [Google Scholar]
- Fenson L, Marchman VA, Thal DJ, Dale PS, Reznick JS, & Bates E. (2007). MacArthur-Bates Communicative Development Inventories: User’s guide and technical manual (2nd edition). Baltimore, MD: Brookes. [Google Scholar]
- Frey JR, Kaiser AP, & Scherer NJ (2018). The influences of child intelligibility and rate on caregivers’ responses to their toddlers with and without cleft palate. The Cleft PalateCraniofacial Journal, 55, 276–286. doi: 10.1177/105566561 [DOI] [PubMed] [Google Scholar]
- Ha S. (2015). Effectiveness of a parent-implemented intervention program for young children with cleft palate. International Journal of Pediatric Otorhinolaryngology, 79, 707–715. doi: 10.1016/j.ijporl.2015.02.023 [DOI] [PubMed] [Google Scholar]
- Jones M. (1988). Etiology of facial clefts: Prospective evaluation of 428 patients. Cleft Palate Journal, 25, 16–20. [PubMed] [Google Scholar]
- Kaiser AP, & Hampton LH (2017). Enhanced milieu teaching. In McCauley R, Fey M. & Gilliam R. (Eds.), Treatment of Language Disorders in Children (2nd ed.). Baltimore, MD: Brookes. [Google Scholar]
- Kaiser AP, & Roberts MY (2013). Parent-implemented enhanced milieu teaching with preschool children with intellectual disabilities. Journal of Speech, Language, and Hearing Research, 56, 295–309. doi: 10.1044/1092-4388(2012/11-0231) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser AP, Scherer NJ, Frey JR, & Roberts MY (2017). The effects of EMT+PE on the speech and language skills of young children with cleft palate: A pilot study. American Journal of Speech-Language Pathology, 26, 806–818. doi: 10.1044/16-0008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klinto K, Salameh E, Olsson M, Flynn T, Svensson H, & Lohmander A. (2014). Phonology in Swedish-speaking three-year-olds born with cleft lip and palate and the relationship with consonant production at 18 months. International Journal of Language and Communicative Disorders, 49, 240–254. doi: 10.1111/1460-6984.12068 [DOI] [PubMed] [Google Scholar]
- Lawrence MA (2016). ez: Easy analysis and visualization of factorial experiments. R package version 4.4–0. Retrieved from https://CRAN.R-project.org/package=ez [Google Scholar]
- Miller J, & Chapman R. (2009). Systematic analysis of language transcripts. Madison, WI: University of Wisconsin. [Google Scholar]
- Pamplona MC, Ysunza A, & Ramirez P. (2004). Naturalistic intervention in cleft palate children. International Journal of Pediatric Otorhinolaryngology, 68, 75–81. doi: 10.1016/j.ijporl.2003.09.007 [DOI] [PubMed] [Google Scholar]
- Peredo T, Zelaya M, & Kaiser AP (2017). Teaching lowincome Spanish-speaking caregivers to implement EMT en Español with their young children with language impairments: A pilot study. American Journal of Speech-Language Pathology, 27, 136–153. doi: 10.1044/2017_AJSLP-16-0228 [DOI] [PubMed] [Google Scholar]
- Peterson-Falzone SJ, Hardin-Jones MA, & Karnell MP (2001). Cleft palate speech (3rd ed.). St. Louis, MO: Mosby. [Google Scholar]
- R Core Team (2018). R: A language and environment for statistical computing. Vienna, Austria: R SurFoundation for Statistical Computing. Retrieved from https://www.R-project.org [Google Scholar]
- Roberts M, & Kaiser AP (2011). The effectiveness of parentimplemented language interventions: A meta-analysis. American Journal of Speech-Language Pathology, 20, 180–199. doi: 10.1044/1058-0360(2011/10-0055) [DOI] [PubMed] [Google Scholar]
- Roberts M, Kaiser A, Wolfe C, Bryant J, & Spidalieri A. (2014). Effects of Teach-Model-Coach-Review instructional approach on caregiver use of language support strategies and expressive language support. American Journal of SpeechLanguage Pathology, 57, 1851–1869. doi: 10.1044/2014_JSLHR-L-13-0113 [DOI] [PubMed] [Google Scholar]
- Scherer NJ (1999). The speech and language status of toddlers with cleft lip and/or palate following early vocabulary intervention. American Journal of Speech-Language Pathology, 8, 81–93. doi: 10.1044/1058-0360.0801.81 [DOI] [Google Scholar]
- Scherer NJ, Boyce S, & Martin G. (2013). Pre-linguistic children with cleft palate: Growth of gesture, vocalization and word use. International Journal of Speech-Language Pathology, 15, 586–592. doi: 10.3109/17549507.2013.794475 [DOI] [PubMed] [Google Scholar]
- Scherer NJ, D’Antonio LL, & McGahey H. (2008). Early intervention for children with cleft palate. Cleft PalateCraniofacial Journal, 45, 18–31. doi: 10.1597/06-085.1 [DOI] [PubMed] [Google Scholar]
- Scherer N, & Kaiser AP (2010). Enhanced milieu teaching with phonological emphasis: Application for children with CLP in treatment of sound disorders in children. In Williams A, McLeod S, & McCauley R. (Eds.), Interventions for speech sound disorders in children. Baltimore, MD: Brookes. [Google Scholar]
- Scherer NJ, Williams AL, Kaiser A, Roberts M, Frey J, & Stoel-Gammon C. (2012, June), Efficacy of an early speech intervention for children with cleft palate. Paper presented at the International Clinical Linguistics and Phonetics Conference, Cork, Ireland. [Google Scholar]
- Scherer NJ, Williams LA, & Proctor-Williams K. (2008). Early and later vocalization skills in children with and without cleft palate. International Journal of Pediatric Otorhinolaryngology, 72, 827–840. doi: 10.1016/j.ijporl.2008.02.010 [DOI] [PubMed] [Google Scholar]
- Scherer NJ, Williams AL, Stoel-Gammon C, & Kaiser A. (2012). Assessment of single word production for children under three years of age: Comparison of children with and without cleft palate. International Journal of Otolaryngology, Cleft –VPI Special Issue, 2012. Article ID 724214. doi: 10.1155/2012/724214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sosa A, & Stoel-Gammon C. (2012). Lexical and phonological effects in early words production. Journal of Speech, Language, and Hearing Research, 55, 596–608. doi: 10.1044/1092-4388(2011/10-0113) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoel-Gammon C, & Williams LA (2013). Early phonological development: Creating an assessment test. Clinical Linguistics and Phonetics, 27, 278–286. doi: 10.3109/02699206.2013.766764 [DOI] [PubMed] [Google Scholar]
- Wickham H. (2016). ggplot2: Elegant graphics for data analysis. New York: Springer-Verlag. [Google Scholar]
- Zimmerman IR, Steiner VG, & Pond RE (2002). Preschool language scale. Fourth Edition (PLS-4). San Antonio, TX: The Psychological Corporation. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.