Abstract
Umbilical hernias are common in patients with cirrhosis of the liver and ascites; however, spontaneous rupture of the hernia is a rare complication. Flood Syndrome occurs very rarely in cirrhotic patients with massive ascites and refers to the spontaneous rupture of an umbilical hernia followed by leakage of ascites fluid. A literature search shows that patients have been managed both operatively and nonoperatively for this condition. We report a case of a 56-year-old man with a history of alcohol-related liver cirrhosis and massive ascites refractory to medical therapy with sudden and spontaneous perforation of his hernia leading to drainage of ascitic fluid from the abdomen. We performed a transjugular intrahepatic portosystematic shunt to relieve portal pressure and subsequent intraabdominal pressure. The patient had resolution of symptoms and the ascitic fluid outflow was resolved.
Keywords: flood syndrome, tips, ascites, umbilical hernia, cirrhosis
CASE REPORT
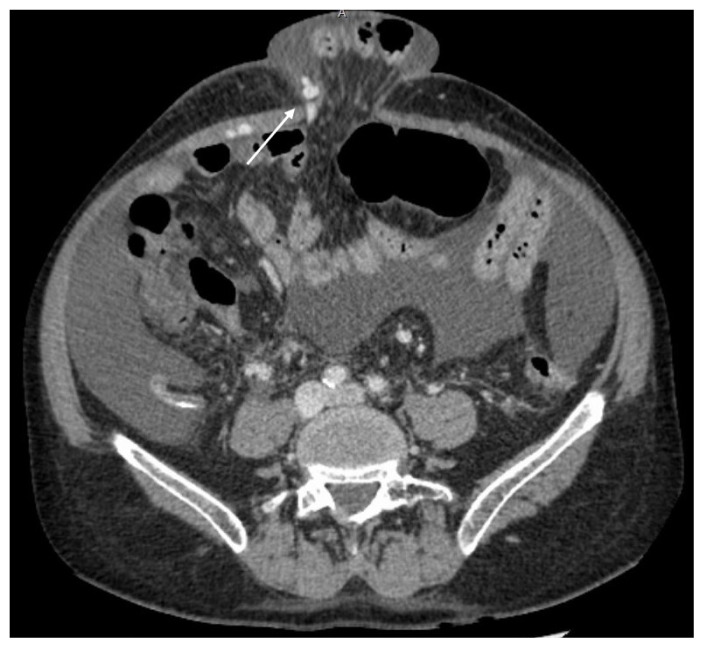
A 56-year-old caucasian man with liver cirrhosis of alcoholic etiology came to the emergency room derived from the hepatology consultation after detecting a creatinine control test of 1.62 mg / dl, sodium 125 mEq / L and finding in the physical examination an ulceration of the umbilical hernia with leakage of ascites fluid through it (Figure 1). The patient’s condition was CHILD B-7, MELD-Na 16, with signs of portal hypertension (Figure 2) and a history of II / IV esophageal varices, without previous bleeding. At the emergency department he had a blood pressure of 91/47 mmHg, a heart rate of 65 bpm, a temperature of 36.6°C and an O2 saturation of 98% baseline. Hemoglobin levels were 8 gr/dl, hematocrit 24.9%, MVC 91.5 fL, leukocytes 7600/mL (neutrophils 4700/mL), albumin 2.7 g / dL, creatinine 1.62 mg/dL, ALT 25 U/L, AST 36 U/L, GGT 119 U/L, ALP 276 U/L, total bilirubin 0.8 mg/dL, normal coagulation and ascites fluid culture and blood cultures were negative.
Figure 1.
56-year-old man with Flood Syndrome.
FINDINGS: Photograph of an ulcerated umbilical hernia (arrow heads).
Figure 2.
56-year-old man with Flood Syndrome.
FINDINGS: Axial contrast enhanced CT of the abdomen in portal phase. Umbilical hernia with exit of intestinal loops and ascitic fluid. Cirrhosis and repermeabilization of the umbilical vein (white arrow) as signs of portal hypertension.
TECHNIQUE: Axial CT, 190 mAs, 120 kV, 1mm slice thickness, 100 ml Omnipaque® 300.
After withdrawing diuretic treatment, starting treatment with albumin and performing evacuating paracentesis together with water restriction, the laboratory parameters improved, with normalization of renal function and recovery of natraemia. During admission, the Surgery Service was consulted, which rejected the surgical treatment of the hernia due to the patient’s comorbidities. Along with the Hepatology section, the placement of a transjugular intrahepatic portosystematic shunt (TIPS) is proposed to improve ascites and avoid surgery. It was decided to perform a TIPS because the patient had longstanding refractory ascites that did not improve despite optimization of treatment. The patient had no contraindications for TIPS placement. The accepted contraindications for TIPS placement appear in (Table 3).
Table 3.
Accepted contraindications to TIPS [14]
| Significant pulmonary hypertension |
| Heart failure or severe cardiac valvular insufficiency |
| Rapidly progressive live failure |
| Severe or uncontrolled hepatic encephalopathy |
| Uncontrolled systemic infection or sepsis |
| Unrelieved biliary obstruction |
| Polycystic liver disease |
| Extensive primary or metastatic hepatic malignancy |
We performed a TIPS to relieve portal pressure and subsequent intraabdominal pressure. TIPS decreases the pressure in the splanchnic system and, with it, the generation of ascites by diverting blood flow from the portal vein to the systemic circulation through the suprahepatic veins (frequently the left suprahepatic vein).
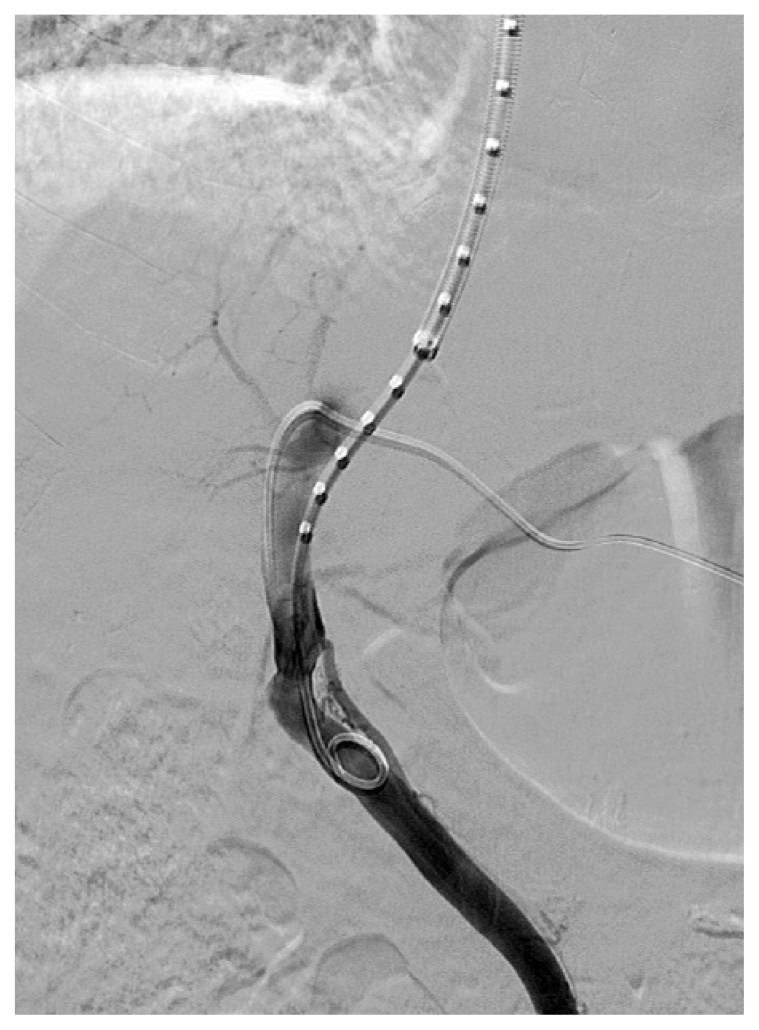
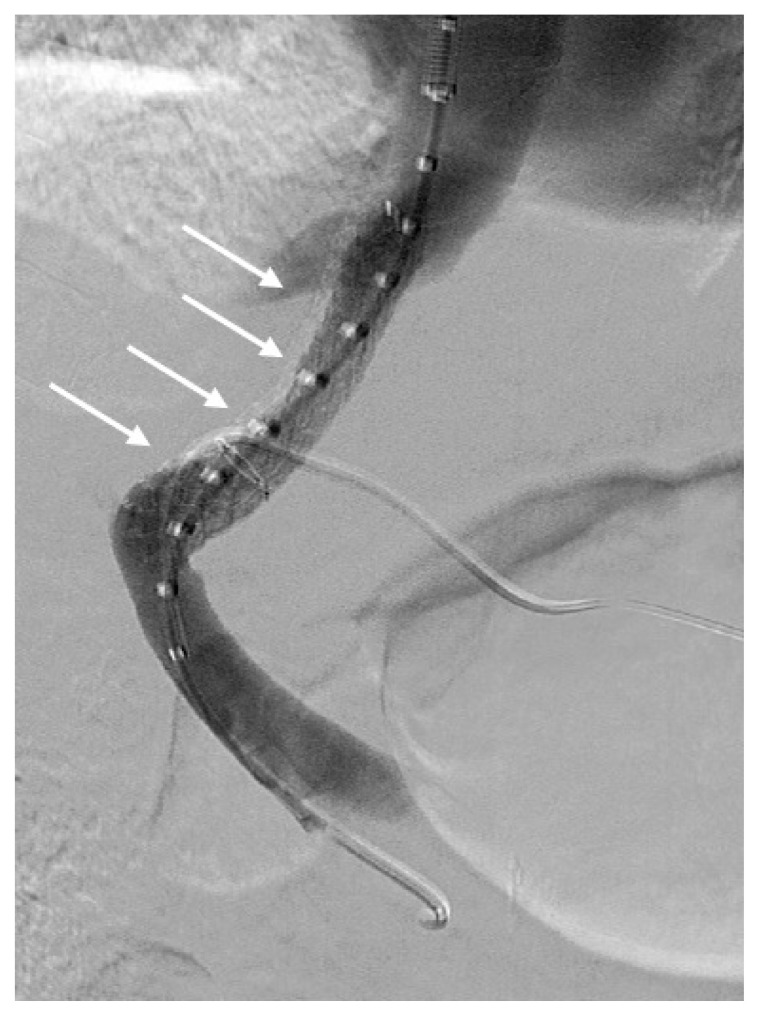
With ultrasound and scope control, we placed a catheter in the main portal percutaneously for image control. Using a right internal jugular puncture, we catheterized the left suprahepatic vein, obtaining access to the left portal vein from here (Figure 3). Initial porto-systemic gradient was 18 mmHg. We dilated the tract with an 8 mm balloon and placed a 5 + 2 cm Viahtorr® partially covered stent-graft that was well positioned, with subsequent dilation of the stent to 8 mm. In the final control, adequate flow derivation is observed through the TIPS and absence of filling of the esophageal varices (Figure 4). Final porto-systemic gradient was 6 mmHg. No immediate complications occurred.
Figure 3.
56-year-old man with Flood Syndrome.
FINDINGS: catheter introduced by jugular access reaching the main portal vein.
TECHNIQUE: anteroposterior angiography with 20ml of Visipaque® 320.
Figure 4.
56-year-old man with Flood Syndrome.
FINDINGS: final control after dilatation. Adequate flow derivation is observed through the TIPS (white arrows).
TECHNIQUE: anteroposterior angiography with 20ml of Visipaque® 320.
The patient remained hospitalized for five more days without the appearance of complications. During admission, an abdominal ultrasound was performed that confirmed the presence of TIPS patency, with a correct position, a velocity range between 160–220 cm / sec and patency of suprahepatic and portal veins.
The TIPS decreased the congestive pressure in the intestinal veins reducing production of ascites in a very important way. The patient received umbilical hernia cures every week for a month and had resolution of symptoms. Six weeks after TIPS placement the patient was seen again by the surgery team to have an umbilical hernia repair without needing a surgical intervention. In ultrasound control 3 and 6 months after TIPS placement, the TIPS was permeable, with velocities within the normal range.
DISCUSSION
INTRODUCTION
Flood syndrome was first reported in 1961 by Frank B. Flood and refers to the spontaneous rupture of an umbilical hernia followed by leakage of ascites fluid [3]. This disease normally occurs in cirrhotic patients with longstanding refractory ascites. The real incidence of Flood Syndrome has not been published. As commented later, this pathology can trigger important complications, even death in a high percentage of patients if untreated. There are multiple treatments for this pathology, the most important being the reduction of ascitic fluid [4,5] (Tables 1,2).
Table 1.
Summary table of Flood Syndrome
| SUMMARY TABLE: | |
|---|---|
| Etiology | Longstanding ascites. Favored by atrophy of the abdominal wall secondary to poor nutritional status. |
| Incidence | The prevalence of umbilical hernias in cirrhotics is around 20%. Spontaneous hernia rupture is very rare, and no specific incidence has been described. |
| Gender ratio | It is directly related to cirrhosis, which is twice as common in men as in women. |
| Age predilection | Like cirrhosis, it occurs more frequently in patients older than 50 years. |
| Risk factors | Ascites from any cause, most frequently from alcoholic cirrhosis. |
| Treatment | Not well defined. The main objective is to reduce ascites, with drugs, paracentesis, TIPS placement, etc. In patients with a good baseline status, herniorrhaphy can be performed. Liver transplantation can also be performed. |
| Prognosis | The mortality rate is between 30–50% and can reach 60–80% if untreated. |
| Findings on imaging | Significant amount of ascites. Tension umbilical hernia with ascites inside, frequently with associated inflammatory changes. There may be intestinal loops, greater omentum, or abdominal organs within the hernia. |
| Complications | Small bowel evisceration, bowel incarceration, cellulitis, peritonitis, sepsis, and hypotension caused by massive outflow of ascites. |
Table 2.
Differential diagnosis table for Flood Syndrome
| DIFFERENTIAL TABLE: | |||
|---|---|---|---|
| US | CT | MRI | |
| Flood Syndrome | Significant ascites. Hyperechogenicity of subcutaneous fat in the umbilical hernia. Outflow of ascites with Valsalva maneuvers. Increased Doppler flow in the subcutaneous cellular tissue of the hernia. | Significant ascites. Distended umbilical hernia, with ascites inside. Stranding of the subcutaneous tissue of the hernia, with hyperenhancement. | Significant ascites. Distended umbilical hernia, with ascites inside. Signal hyperintensity on T2 sequences in the subcutaneous cellular tissue of the hernia, frequently with hyperenhancement. |
| Uncomplicated umbilical hernia | Umbilical hernia with fat inside. Normal echogenicity of the subcutaneous tissue and contents of the hernia. No pain on examination. | Umbilical hernia with fat inside from greater omentum or mesentery. No associated inflammatory changes. | Umbilical hernia with fat inside from greater omentum or mesentery. No associated inflammatory changes. |
| Complicated umbilical hernia | Hyperechogenicity of subcutaneous tissue or abdominal fat within the hernia. May present with a dilated bowel loop withing the hernia that shows increased/absent Doppler flow. | Thickening of the subcutaneous tissue of the umbilical hernia, with inflammatory changes in its content. It may present a distended intestinal loop inside, with hyper enhancement or no enhancement. | Umbilical hernia with thickening of the subcutaneous cell tissue or hyperintensity on T2 sequences in its content. It can have a distended intestinal loop inside with hyperenhancement or no enhancement, frequently with diffusion restriction. |
| Rupture of umbilical hernias from other causes | In incarcerated umbilical hernias, hyperechogenicity of subcutaneous cell tissue and abdominal fat, with dilated intestinal loops inside that shows no Doppler flow. In traumatic ruptures with Valsalva maneuvers there is leakage of intra-abdominal fat or intestinal loops. | In incarcerated and perforated umbilical hernias, inflammatory changes in the subcutaneous tissue and abdominal fat, with dilated bowel loops, frequently with no enhancement. In traumatic ruptures, a solution of cutaneous continuity with leakage of fat or intestinal loops. | In incarcerated and perforated umbilical hernias, hyperintensity on T2 signal in subcutaneous tissue and abdominal fat, with dilated intestinal loops that frequently show lack of enhancement and restricted diffusion. In traumatic ruptures, a solution of cutaneous continuity with leakage of fat or intestinal loops, which usually show normal signal intensity. |
Etiology, clinical presentation & risk factors
Umbilical hernias are 6–14% of all abdominal wall hernias in adults. In cirrhotic patients the prevalence of umbilical hernias is around 20% [4,6], being its risk 10 times higher than in the overall population [7], with spontaneous rupture of the hernia occurring very rarely. The incidence of cirrhosis is twice as high in men as in women and it is more common in patients older than 50 years. The etiology of hernias is usually multifactorial, mainly secondary to increased intra-abdominal pressure due to ascites and atrophy of the abdominal wall muscles secondary to poor nutritional status [4]. Ascites in cirrhotic patients causes an expansion of the abdominal wall generating a risk of spontaneous rupture of the hernia, which can cause cellulitis, peritonitis, sepsis, incarceration of loops and hypotension secondary to massive outflow of ascites [4,8]. There are clues that suggest the rupture of the umbilical hernia such as changes in color, ulceration or necrosis on the surface of the skin [4]. The mortality rate for untreated complicated hernias in cirrhotic patients ranges from 60–80% [9]. In US, MRI and CT we must differentiate between Flood Syndrome, uncomplicated umbilical hernias, complicated umbilical hernias and ruptured umbilical hernias due to other causes, the keys for their differentiation appear in the differential table.
Treatment
The treatment of this pathology is complicated and is not defined, so it must be evaluated in each patient individually, being the most important measure the reduction of ascites, although optimal management of Flood syndrome has not been established. Ascites has as conventional treatment the use of diuretics, water restriction, albumin administration, evacuating paracentesis or the placement of pigtail catheters [5], but this treatment is often insufficient. Because cirrhotic patients are at increased risk of adverse effects after surgical interventions, the treatment of umbilical hernias, especially perforated hernias, with herniorrhaphy is controversial.
Transjugular intrahepatic portosystematic shunt (TIPS) has been shown to be a better option for cirrhotic patients with complicated umbilical hernias [4]. TIPS placement is the most widely used optimal method [10,11]. TIPS decreases the porto-systemic gradient, managing to resolve the clinical consequences derived from portal hypertension. In most cases, what is expected is that the ascites improves or resolves and the umbilical hernia perforation ends up closing without the need for surgery.
There are several accepted contraindications for TIPS that appear in (Table 3). Possible complications derived from the TIPS placement procedure are shown in (Table 4).
Table 4.
Potential complications of TIPS procedure [14].
| Complications | Classification |
|---|---|
| Minor | Fever, haemobilia |
| Major | Haemoperitoneum, biliary peritonitis, hepatic infarction, trauma to hepatic artery or branches, renal failure, liver failure, TIPS infection (TIPSitis) |
| Death |
There are other effective treatments such as the placement of a peritoneal-jugular shunt, partial splenic embolization [9], treatment with fibrin glue injection [12] and in patients with good baseline status (based on MELD), herniorrhaphy [13], since mortality is 6–20% when hernias are treated by surgery [9]. In patients treated by surgery, the most frequent complications are the presence of wound infection / dehiscence, leakage of ascites fluid, liver failure and recurrence of the hernia [12]. Liver transplantation may be another option, being able to perform the transplant and hernia repair in the same intervention [7].
TEACHING POINT
Flood syndrome is a life-threatening complication whose main treatment is based on reducing ascites, and interventional procedures such as placement of abdominal drainage catheters or TIPS catheters may be necessary in refractory cases.
QUESTIONS
1. Regarding the treatment of Flood Syndrome
Treatment is well established and does not depend on the type of patient.
The main objective of treatment is to reduce ascites. Applies.
Evacuation paracentesis and pigtail catheter placement are not recommended.
Placing a TIPS is not an option.
Performing a liver transplant is not indicated.
Explanation:
The treatment of Flood Syndrome is poorly defined and must be adapted to each patient. [The treatment of this pathology is complicated and is not defined…].
Applies. The main objective is to reduce ascites to achieve closure of the umbilical hernia. [The treatment of this pathology is complicated and is not defined, so it must be evaluated in each patient individually, being the most important measure the reduction of ascites].
Evacuation paracentesis and placement of pigtail catheters are good measures to reduce ascites. [Ascites has as conventional treatment the use of diuretics, water restriction, evacuating paracentesis or the placement of pigtail catheters…].
The placement of a TIPS is a good option to reduce ascites. [The placement of TIPS is the most widely used optimal method…].
Performing a liver transplant is a good option in certain patients. [Liver transplantation may be another option…].
2. Flood Syndrome is
Rupture of an umbilical hernia from a penetrating wound.
The presence of refractory ascites despite TIPS placement.
Spontaneous rupture of an umbilical hernia due to the presence of abundant ascites. Applies.
The incarceration of an inguinal hernia in post-surgical patients.
Long-standing hydronephrosis secondary to urothelioma in the lower urinary tract.
Explanation:
It is the rupture of an umbilical hernia, not due to a penetrating wound but due to massive ascites. [Flood Syndrome occurs very rarely in cirrhotic patients with massive ascites and refers to the spontaneous rupture of an umbilical hernia followed by leakage of ascites fluid].
Flood Syndrome occurs in patients with refractory ascites and TIPS can be one of its treatments. [Flood Syndrome occurs very rarely in cirrhotic patients with massive ascites and refers to the spontaneous rupture of an umbilical hernia followed by leakage of ascites fluid], [The placement of TIPS is the most widely used optimal method…]
Applies. [Flood Syndrome occurs very rarely in cirrhotic patients with massive ascites and refers to the spontaneous rupture of an umbilical hernia followed by leakage of ascites fluid].
Flood syndrome occurs in patients with long-standing ascites, it refers to the spontaneous rupture of an umbilical hernia and does not necessarily occur in post-surgical patients. [Flood Syndrome occurs very rarely in cirrhotic patients with massive ascites and refers to the spontaneous rupture of an umbilical hernia followed by leakage of ascites fluid].
Flood Syndrome is not related to the urinary tract. [Flood Syndrome occurs very rarely in cirrhotic patients with massive ascites and refers to the spontaneous rupture of an umbilical hernia followed by leakage of ascites fluid].
3. In the treatment of Flood Syndrome
Surgical treatment of the hernia should not be performed
Blood albumin levels should be decreased.
Partial embolization of the spleen is not a reasonable option.
The treatment is well defined.
The placement of a TIPS is a good treatment option. Applies.
Explanation:
The treatment of umbilical hernia with herniorrhaphy is controversial, but it is performed on some occasions. [Treatment of umbilical hernias by herniorrhaphy, especially perforated hernias, is controversial…].
The goal in these patients with massive ascites is to increase albumin levels. [Ascites has as conventional treatment the use of diuretics, water restriction, albumin administration…].
Partial embolization of the spleen is an option in certain patients. […there are other effective treatments such as the placement of a peritoneal-jugular shunt, partial splenic embolization…].
The treatment of these patients is complex and poorly defined. [The treatment of this pathology is complicated and is not defined…].
Applies. The placement of TIPS is a good treatment option, since it allows to reduce the amount of ascites in patients who do not improve with less invasive treatments. [The placement of TIPS is the most widely used optimal method…]
4. Flood Syndrome occurs in
Patients with long-standing ascites and spontaneous bacterial peritonitis.
Patients with cirrhosis without ascites.
Patients with massive ascites. Applies.
Patients with incarcerated inguinal hernias.
Patients with femoral hernias complicated by massive ascites.
Explanation:
Flood syndrome occurs in patients with ascites, but it is not related to spontaneous bacterial peritonitis. [Flood Syndrome occurs very rarely in cirrhotic patients with massive ascites…].
Flood syndrome occurs in patients with cirrhosis and long-standing ascites. [Flood Syndrome occurs very rarely in cirrhotic patients with massive ascites…].
Applies. [Flood Syndrome occurs very rarely in cirrhotic patients with massive ascites…].
Flood Syndrome occurs in patients with ruptured umbilical hernias. [Flood Syndrome… refers to the spontaneous rupture of an umbilical].
Flood Syndrome occurs in patients with massive ascites and ruptured umbilical hernias. [Flood Syndrome occurs very rarely in cirrhotic patients with massive ascites and refers to the spontaneous rupture of an umbilical hernia followed by leakage of ascites fluid].
5. In patients with Flood Syndrome it is not indicated
To administer diuretic treatment.
To administer albumin.
To perform evacuating paracentesis.
To increase water intake. Applies.
To perform a surgical repair of the umbilical hernia.
Explanation:
For the treatment of ascites, the administration of diuretics is indicated. [Ascites has as conventional treatment the use of diuretics, water restriction…].
For the treatment of ascites, the administration of albumin is indicated. [Ascites has as conventional treatment the use of diuretics, water restriction, albumin administration…].
Evacuation paracentesis is indicated to reduce ascites. [Ascites has as conventional treatment the use of diuretics, water restriction, albumin administration, evacuating paracentesis…].
Applies. [Ascites has as conventional treatment the use of diuretics, water restriction…].
Surgical treatment of umbilical hernia in these patients is controversial, but it is performed on certain occasions. [Treatment of umbilical hernias by herniorrhaphy, especially perforated hernias, is controversial…].
ABBREVIATIONS
- TIPS
transjugular intrahepatic portosystemic shunt
- MELD
model for end-stage liver disease
- CHILD
child-pugh score
Footnotes
AUTHORS’ CONTRIBUTIONS: Pablo Peñalver Calero: wrote the article and collected the images.
Marco Leyva Vásquez-Caicedo: helped writing the article and reviewed the final manuscript.
Claudia Jimena González-Nieto: reviewed the final manuscript.
Javier Eduardo Armijo Astrain: reviewed the final manuscript.
José Vicente Méndez Montero: reviewed the final manuscript.
REFERENCES
- 1.Child CG, Turcotte JG. Surgery and portal hypertension. Major Probl Clin Surg. 1964;1:1–85. [PubMed] [Google Scholar]
- 2.Kamath PS, Wiesner RH, Malinchoc M, et al. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33(2):464–470. doi: 10.1053/jhep.2001.22172. [DOI] [PubMed] [Google Scholar]
- 3.Flood FB. Spontaneous perforation of the umbilicus in Laennec’s cirrhosis with massive ascites. N Engl J Med. 1961;264:72–74. doi: 10.1056/NEJM196101122640204. [DOI] [PubMed] [Google Scholar]
- 4.Telem DA, Schiano T, Divino CM. Complicated hernia presentation in patients with advanced cirrhosis and refractory ascites: management and outcome. Surgery. 2010;148(3):538–543. doi: 10.1016/j.surg.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 5.Nguyen ET, Tudtud-Hans LA. Flood Syndrome: Spontaneous Umbilical Hernia Rupture Leaking Ascitic Fluid-A Case Report. Perm J. 2017;21:16–152. doi: 10.7812/TPP/16-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eker HH, van Ramshorst GH, de Goede B, et al. A prospective study on elective umbilical hernia repair in patients with liver cirrhosis and ascites. Surgery. 2011;150(3):542–546. doi: 10.1016/j.surg.2011.02.026. [DOI] [PubMed] [Google Scholar]
- 7.Dokmak S, Aussilhou B, Belghiti J. Umbilical hernias and cirrhose. J Visc Surg. 2012;149(5 Suppl):e32–e39. doi: 10.1016/j.jviscsurg.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 8.Belghiti J, Durand F. Abdominal wall hernias in the setting of cirrhosis. Semin Liver Dis. 1997;17(3):219–226. doi: 10.1055/s-2007-1007199. [DOI] [PubMed] [Google Scholar]
- 9.Chikamori F, Mizobuchi K, Ueta K, et al. Flood syndrome managed by partial splenic embolization and percutaneous peritoneal drainage. Radiol Case Rep. 2020;16(1):108–112. doi: 10.1016/j.radcr.2020.10.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DeLuca IJ, Grossman ME. Flood syndrome. JAAD Case Rep. 2014;1(1):5–6. doi: 10.1016/j.jdcr.2014.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith MT, Rase B, Woods A, et al. Risk of hernia incarceration following transjugular intrahepatic portosystemic shunt placement. J Vasc Interv Radiol. 2014;25(1):58–62. doi: 10.1016/j.jvir.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 12.Sheikh MM, Siraj B, Fatima F, Ehsan H, Shahid MH. Flood Syndrome: A Rare and Fatal Complication of Umbilical Hernia in Liver Cirrhosis. Cureus. 2020;12(8):e9915. doi: 10.7759/cureus.9915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marsman HA, Heisterkamp J, Halm JA, Tilanus HW, Metselaar HJ, Kazemier G. Management in patients with liver cirrhosis and an umbilical hernia. Surgery. 2007;142(3):372–375. doi: 10.1016/j.surg.2007.05.006. [DOI] [PubMed] [Google Scholar]
- 14.Tripathi D, Stanley AJ, Hayes PC, et al. Transjugular intrahepatic portosystemic stent-shunt in the management of portal hypertension. Gut. 2020;69(7):1173–1192. doi: 10.1136/gutjnl-2019-320221. [DOI] [PMC free article] [PubMed] [Google Scholar]