The physician is wrapping up the summer camp physical examination for her 10-year-old patient Jay. She has addressed his warts and his emerging myopia and given him safety counseling.
Time is up.
As Jay's mother stands up to leave, she says, “By the way, my husband has just been diagnosed with colon cancer, and his physicians say it is familial adenomatous polyposis. I heard there is a genetic test for FAP. Should Jay be tested?”
INTRODUCTION
As the revolution in molecular genetics makes its way into the clinical arena, patients are questioning their physicians about the use of complex genetic tests. In this article, we review the goals of genetic testing, discuss some of the physician-patient communication issues that are always relevant in genetic disorders, and discuss test ordering. Future articles will focus on the basics of genetic counseling, specific screening tests, ethical concerns in genetic testing, a primer on clinical genetics for the primary care provider, and practical guides to genetic issues for a variety of specific conditions.
Table 1.
| Special considerations of genetic testing |
|---|
|
GENETIC TESTING DEFINED
Genetic “tests” refers to the analysis of human DNA, RNA, chromosomes, or proteins used to detect abnormalities related to an inherited disorder.1 Tests can directly examine the DNA or RNA that make up a gene (direct testing), look at markers that are coinherited with a disease-causing gene (linkage testing), examine the protein products of genes (biochemical testing), or examine the entire chromosome (cytogenetic testing). Although these genetic tests require easily obtained blood specimens, genetic testing involves special considerations (see box).
The Internet provides an increasing volume of information that is readily disseminated. As a result, it is now becoming common for patients to request a specific drug or laboratory test from their physicians.2 However, the request may be based on only a superficial search of the Internet or on an e-mail from a friend or a support group. Often the request for a test is based on or a misunderstanding of the patient's symptoms, family condition, or other risk factors, or on a newly reported scientific discovery.
When considering genetic testing, physicians need to be aware of the difference between clinically available tests and “research only” tests. Clinical tests are performed by laboratories with federally mandated CLIA (Clinical Laboratory Improvement Amendments of 1998) certification.3 Such laboratories can charge a fee and report results for use in patient care. By contrast, laboratories that perform research testing are not required to have CLIA approval; costs are usually borne by the investigators rather than the patient, and results are not reported for use in patient care. Research laboratories may decline to perform a test if the patient does not meet the criteria of the research project. Because the speed with which test availability moves from research into clinical laboratories is unpredictable, physicians must rely on frequently updated resources for current information. One such resource is Gene Tests at www.genetests.org, which provides information on more than 450 laboratories offering testing for more than 750 inherited diseases.
Table 2.
Principles of predictive testing and carrier testing
| Principle | Clinical example |
|---|---|
| Predictive testing may be medically indicated if early diagnosis allows intervention that reduces morbidity and mortality | Early diagnosis of familial adenomatous polyposis (FAP) allows for prompt colectomy |
| Even in the absence of medical indications, predictive testing can influence life-planning decisions | Predictive testing for early onset of familial Alzheimer's disease allows planning for employment, leisure, and long-term care |
| Identifying carriers allows reproductive choices | A couple who are both carriers for sickle cell disease or for cystic fibrosis may choose prenatal testing |
| Carrier testing can improve risk assessment for members of racial and ethnic groups more likely to carry mutations for certain genetic conditions. Thus, carrier testing may then be offered to individuals who do not have a family history of the disorder | Screening for carriers of sickle cell disease (African ancestry) and Tay Sachs disease (Jewish ancestry) can identify couples at risk before the birth of an affected child |
USES OF GENETIC TESTS
Genetic tests can serve different purposes.4,5 These include
diagnostic testing
predictive testing
carrier testing
prenatal testing
preimplantation testing
newborn screening
The table listing principles of predictive testing and carrier testing provides clinical examples for each.
Diagnostic testing
Diagnostic genetic testing, like other types of diagnostic testing, is used to confirm or rule out a known or suspected genetic disorder in a symptomatic person. Although there are often other methods to make a diagnosis (eg, muscle biopsy), DNA-based testing may provide the same information at a far lower cost and often with less risk to the patient.
A 4-year-old boy, Derek, presents with progressive muscle weakness. His mother says Derek is having increasing difficulty climbing stairs and in getting up from a sitting position. Derek has an elevated serum creatine kinase concentration, and his pediatrician suspects Duchenne muscular dystrophy (DMD). In the past, a muscle biopsy would have been the test of choice to confirm the diagnosis. However, since 70% of boys with DMD have either a deletion or a duplication of the DMD gene that can be detected with a single blood test, the first step in establishing the diagnosis of DMD is drawing a blood specimen for DNA testing, at lower cost and with less risk to the patient.
Predictive testing
Predictive testing is used to clarify the genetic status of an asymptomatic family member at risk for a genetic disorder. Predictive testing always requires that the specific disease-causing mutation first be identified in an affected family member. Predictive testing is of 2 types: presymptomatic and predispositional. Huntington's disease is an example of presymptomatic testing: if the gene mutation is present in a healthy individual, symptoms are certain to occur if the person lives long enough. Even in the absence of medical interventions, predictive testing can influence life-planning decisions.
Huntington's disease is an autosomal dominant neurologic disorder with onset typically in the fifth decade. Early signs are often memory loss and personality changes with progression to involuntary movement disorder, dementia, and death.
Charlie, a 29-year-old man, has recently learned that his father, who died when Charlie was 3 years old, had Huntington's disease. Charlie learns from his physician that he has a 50% chance of developing Huntington's disease and that no treatment exists for this disorder. Charlie seeks additional help with decision making because he and his fiancée have planned to have children, but now he is uncertain because his life may be shortened. He's also wondering whether his career as a custom watchmaker is the best choice. After a lengthy discussion with a genetic counselor, Charlie and his fiancée agree that he should have presymptomatic genetic testing to see if he will develop Huntington's disease. They feel they cannot make informed decisions about their future without this information.
Testing of the BRCA1 gene for breast cancer susceptibility is an example of predispositional testing; the finding of a particular gene mutation provides a probability that breast cancer will occur. Predispositional testing differs from predictive testing in that a positive test result does not indicate a 100% risk of developing the condition (eg, breast cancer). Furthermore, testing 1 gene for predisposition to a common disorder does not test for all factors, and a negative test result does not alter the background population-based risk to develop the condition. Furthermore, the risks assigned to positive results may be inflated because the initial studies upon which they are based involve high-risk families in which other unidentified factors may be contributing to risk.
Before using predictive testing, it is appropriate for the patient and physicians to discuss whether early diagnosis will result in medical interventions to reduce morbidity or mortality or whether testing is to enable personal decision making. Patients need to provide their full informed consent, including a careful understanding of the benefits and risks of knowing the results of testing. In addition to pretest counseling by a genetics professional, follow-up may be required, especially by professionals with special expertise (eg, in mental health or genetics).
Given the newness of the field of medical genetics, many ethical and practice standards are yet to be worked out. For example, the American College of Medical Genetics (ACMG) and National Society of Genetic Counselors (NSGC) recommend against testing asymptomatic children at risk for adult-onset disease when no reasonable medical intervention is available.6,7 Nonetheless, it could be argued that parents or other family members may have compelling reasons to know whether a specific gene mutation is present in a child at risk.
Carrier testing
Carrier testing is used to identify individuals who have a gene mutation for a disorder inherited in an autosomal recessive or X-linked recessive manner. Usually the carrier does not have symptoms of the disease itself but seeks the information to make informed reproductive choices. Although the issues differ significantly from predictive testing, pretest and posttest counseling are equally important given that results can have social and personal implications. Depending on the genetic condition, reproductive options that may need to be discussed with carriers include pregnancy without prenatal testing, pregnancy with prenatal testing, preimplantation diagnosis, pregnancy by egg or sperm donation, parenting by adoption, or remaining childless.
Maria is a 25-year-old woman of Italian ancestry who is referred to a genetics clinic because of a family history of β-thalassemia, an autosomal recessive disorder. When Maria fails to keep her first appointment, her genetic counselor contacts her by phone. Maria admits that she did not keep her appointment because she is ashamed that “defective genes” run in her family, but she agrees to discuss her concerns further. During her follow-up appointment, Maria tells the genetic counselor that she has always assumed she is a carrier. She has heard that carriers of β-thalassemia develop jaundice and facial disfigurement as they get older. She has also been concerned that she would not be able to get health or life insurance if it were known that she was a carrier. Her genetic counselor acknowledges her concerns and explains that carriers of β-thalassemia do not have related health problems and, therefore, should have no difficulty obtaining insurance.
Maria also comes to understand the risk to the children of carriers and that she may, in fact, not be a carrier. She feels more informed and reassured and decides to go ahead with carrier testing.
Prenatal testing
Prenatal testing is used to identify the genetic status of a pregnancy at risk for a genetic disorder. Risk factors for certain genetic conditions include advanced maternal age, family history, ethnicity, or an abnormal prenatal sonogram. Current prenatal testing options include maternal serum screening and the invasive procedures of amniocentesis and chorionic villus sampling, which are widely available, and the more highly specialized techniques of placental biopsy and periumbilical blood sampling. Invasive prenatal testing has risk to the fetus, highlighting the importance of informed consent and formal genetic counseling. Prenatal testing for treatable genetic conditions and for adult-onset genetic conditions is controversial, requiring careful discussion of the advantages and disadvantages. (See upcoming articles in Gene Scene that address ethics and genetic counseling).
Preimplantation testing
Preimplantation testing is used to select early embryos for implantation that have been conceived by in vitro fertilization. Testing determines whether the embryos are free of a particular genetic condition and provides an alternative to prenatal diagnosis and termination of pregnancy. Such testing is performed only at specialized centers and is limited to a small number of disorders. The costs of preimplantation testing are high and are not usually covered by health insurance.
Newborn screening
Screening shortly after birth for inborn errors of metabolism and hearing loss offers the opportunity to begin treatment or intervention for serious disorders as soon as possible. Many newborn screening programs are legally mandated, although legislation varies by state.8,9 The tests themselves are not diagnostic but, rather, identify neonates who are candidates for further evaluation.
INFORMATION RESOURCES
Physicians must rely on frequently updated, easily accessed resources for current information on the specific use of genetic testing. One such resource is GeneClinics at www.geneclinics.org, which has about 100 disease profiles relating genetic testing to diagnosis, management, and genetic counseling of specific diseases.
The physician and Jay's mother consult GeneClinics and learn that evaluating Jay further for this autosomal dominant disorder is warranted. Testing Jay for the APC gene mutation associated with familial adenomatous polyposis will be appropriate if his father has an identifiable mutation; laboratories performing this testing can be identified through GeneTests. The mother and the physician are both aware now that further surveillance of Jay for intestinal polyps will be indicated if Jay tests positive for his father's APC mutation or if molecular genetic testing in his father is uninformative.
CONCLUSION
Although testing is available for hundreds of inherited diseases, molecular genetic testing is still in its infancy and promises to become a larger part of primary care practice. Physicians must be familiar with the appropriate uses of genetic testing for their patients and with current information resources that will allow them to convey reliable information.
For each patient with an inherited disease, the practitioner must be able to define his or her role and that of the genetics professional by becoming familiar with the elements of a genetic consultation. Next month we will look at the genetic consultation and focus on the physician-patient relationship and the potential roles of the primary care provider in this dynamic.
Summary points
Genetic testing is the analysis of DNA, RNA, chromosomes, or proteins to detect abnormalities related to an inherited disorder
Such testing is relevant to medical management when used for diagnosis, early treatment through predictive testing, and newborn screening
It is also relevant to personal decision making when used for prenatal diagnosis, carrier testing, and predictive testing of an untreatable disorder
Testing requires informed consent, careful discussion of test interpretation, and follow-up services
Clinical availability of genetic testing changes rapidly, necessitating reliance on frequently updated information resources.
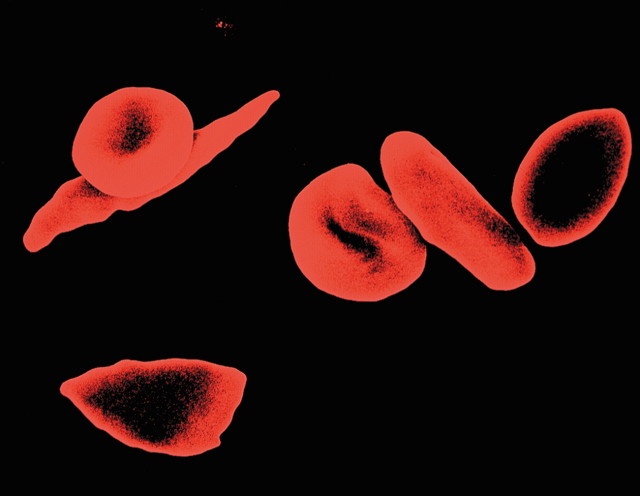
Figure 1.
Sickle cell carriers may choose prenatal testing
Murti/SPL
Competing interests: The authors are affiliated with Gene Tests and GeneClinics, organizations mentioned in this article.
References
- 1.Holtzman NA, Watson MS, eds. Promoting Safe and Effective Genetic Testing in the United States. Final Report of the Task Force on Genetic Testing. Baltimore: Johns Hopkins University Press; 1998. [PubMed]
- 2.Jadad AR. Promoting partnerships: challenges for the Internet age. BMJ 1999;319: 761-764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clinical Laboratory Improvement Amendments of 1998 Regulation #HFCA-2239F. Reference 63 FR 26722. Available at: http://www.phppo.cdc.gov/dls/clia/chronol.asp. Accessed March 6, 2001.
- 4.Pagon RA. Genetic diagnosis and counseling. In: Dale DC, Federman DD, eds. Scientific American Medicine. New York: Scientific American; 2001: VIII.
- 5.Fink L, Collins F. The Human Genome Project: view from the National Institutes of Health. J Am Med Womens Assoc 1997;52: 4-7. [PubMed] [Google Scholar]
- 6.American Society of Human Genetics and American College of Medical Genetics. Points to consider: ethical, legal, and psychosocial implications of genetic testing in children and adolescents. Am J Hum Genet 1995;57: 1233-1241. [PMC free article] [PubMed] [Google Scholar]
- 7.National Society of Genetic Counseling. Prenatal and childhood testing for adult onset disorders. Resolution adopted 1995. Available at: http://www.nsgc.org/about_position.asp#adultonsetdis. Accessed March 6, 2001.
- 8.National Newborn Screening and Genetics Resources Center contact information page. National Newborn Screening and Genetics Resources Center Web site. Available at http://genes-r-us.uthscsa.edu/contact/htm. Accessed March 6, 2001.
- 9.National Center for Hearing Assessment and Management (NCHAM) Web site. Available at: http://www.infanthearing.org. Accessed March 6, 2001.