QUESTION: A 50-year-old woman is seen for evaluation of a facial eruption that has been present intermittently for at least 5 years. The process is located on her mid and lower face. She has used the topical corticosteroid creams diflorasone diacetate 0.05% and hydrocortisone valerate 0.2% for a prolonged period.
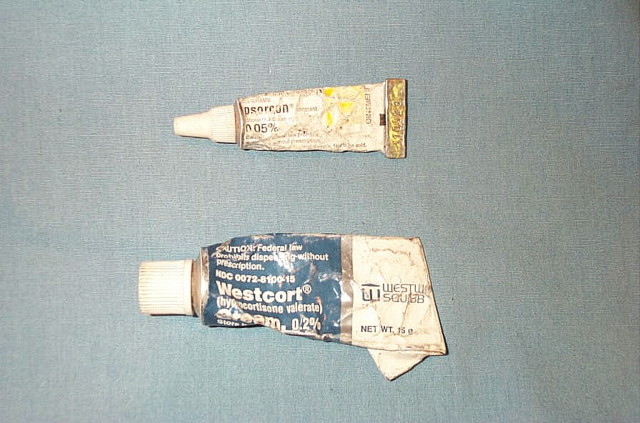
Indeed, she presents crimped empty tubes to us in hopes of refills (figure 1). These preparations provide temporary relief, but the eruption always returns.
Figure 1.
Nearly empty tubes of medium- and high-potency topical steroids presented by patient
Examination shows that she has a light complexion and marked erythema and scaling of the lower face, extending up to the cheeks. The lower lids show minor involvement (figure 2). The eruption spares the vermilion border of the lips and the lips themselves.
Figure 2.

Marked erythema and scaling of the patient's lower face
What are the diagnosis, differential diagnosis, and treatment of this condition? What role do prescription topical steroids play in this eruption?
ANSWER: This patient has steroid-induced perioral dermatitis, a condition marked by perioral or periorbital erythema and scaling with or without papules that characteristically shows a rim of sparing around the vermilion border of the lips. The process usually starts in a perioral distribution with later involvement of the chin, nasolabial folds, and occasionally the eyelids. It occurs mostly in women.
The differential diagnosis includes classic perioral dermatitis, rosacea, and acne. Perioral dermatitis can begin by itself and is seen mostly in women aged 15 to 50 years,1 although it also may rarely affect prepubertal children of both sexes.2 Perioral dermatitis can become steroid-induced perioral dermatitis after prolonged use of topical corticosteroids on the face. Steroid-induced perioral dermatitis is differentiated from common perioral dermatitis by history and clinical behavior. Patients with rosacea and acne can also develop steroid rosacea, steroid acne, or the red-face syndrome after corticosteroid abuse.3 Steroid-induced facial dermatoses tend to have more erythema, inflammation, and scaling than their noniatrogenic counterparts.
Mid- or high-potency topical corticosteroids are known to exacerbate perioral dermatitis, acne, and rosacea. They often initiate a cycle of temporary relief and increasingly severe flare-ups on attempt to stop the medicine. This has been described as an “addiction” of the skin to the steroid, requiring increasingly larger and more frequent applications of steroid creams to bring relief.4 Although temporarily reducing the inflammatory reaction, the steroid may increase the overgrowth of the bacteria through local immunosuppression.
We have observed that patients with steroid-induced perioral dermatitis often present with vigorously squeezed tubes of corticosteroids that they have used for many months to years. These patients have tried to extract as much of the precious cream as possible to counter the latest flare of the dermatitis. Thus, we term this presentation the “tortured tube” sign.
Treatment involves cessation of the topical steroid. Often this regimen initially results in moderate to severe flare-ups of the eruption. The administration of tetracycline, 500 mg by mouth twice a day, and cold tap water compresses will help to alleviate the inflammation. The lesions typically resolve after a few weeks, but occasionally may last as long as 6 months. To ensure therapeutic success, the physician must educate the patient about the course of the disease and the need to discontinue the use of topical corticosteroids.
Prevention is more important than cure. Physicians should never prescribe mid- to high-potency topical corticosteroids for facial use without clear oral and written instructions that limit the time of application to no more than 1 to 2 weeks. Even weaker corticosteroid creams have been implicated in initiating facial disorders. Refills of these medicaments should not be given over the phone. A 15-gram tube of a steroid cream may last a patient 6 to 12 months when used only on the face and is sufficient to cause cutaneous addiction with the development of uncomfortable and unsightly dermatoses.
In this case, on follow-up several months later, the patient's rash had resolved (figure 3).
Figure 3.

Resolution of the patient's rash several months after abstaining from steroid use
Competing interests: None declared
References
- 1.Habif T, ed. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 3rd ed. St Louis: Mosby; 1996.
- 2.Manders SM, Lucky AW. Perioral dermatitis in childhood. J Am Acad Dermatol 1992;27(pt 1): 688-692. [DOI] [PubMed] [Google Scholar]
- 3.Rapaport MJ, Rapaport V. Eyelid dermatitis to red face syndrome to cure: clinical experience in 100 cases. J Am Acad Dermatol 1999;41(pt 1): 435-442. [DOI] [PubMed] [Google Scholar]
- 4.Wells K, Brodell R. Topical corticosteroid “addiction”: a cause of perioral dermatitis. Postgrad Med 1993;93: 225-230. [DOI] [PubMed] [Google Scholar]