Abstract
The field of medical physics has struggled with the role of research in recent years, as professional interests have dominated its growth toward clinical service. This article focuses on the subset of medical physics programs within academic medical centers and how a refocused academic mission within these centers should drive and support Discovery and Invention with Ventures and Engineering for Research Translation (DIVERT). A roadmap to a DIVERT-based scholarly research program is discussed here around the core building blocks of: (a) creativity in research and team building, (b) improved quality metrics to assess activity, (c) strategic partnerships and spinoff directions that extend capabilities, and (d) future directions driven by faculty-led initiatives. Within academia, it is the unique discoveries and inventions of faculty that lead to their recognition as scholars, and leads to financial support for their research programs and reconition of their intellectual contributions. Innovation must also be coupled to translation to demonstrate outcome successes. These ingredients are critical for research funding, and the two-decade growth in biomedical engineering research funding is an illustration of this, where technology invention has been the goal. This record can be contrasted with flat funding within radiation oncology and radiology, where a growing fraction of research is more procedure-based. However, some centers are leading the change of the definition of medical physics, by the inclusion or assimilation of researchers in fields such as biomedical engineering, machine learning, or data science, thereby widening the scope for new discoveries and inventions. New approaches to the assessment of research quality can help realize this model, revisiting the measures of success and impact. While research partnerships with large industry are productive, newer efforts that foster enterprise startups are changing how institutions see the benefits of the connection between academic innovation and affiliated startup company formation. This innovation-to-enterprise focus can help to cultivate a broader bandwidth of donor-to-investor networks. There are many predictions on future directions in medical physics, yet the actual inventive and discovery steps come from individual research faculty creativity. All success through a DIVERT model requires that faculty-led initiatives span the gap from invention to translation, with support from institutional leadership at all steps in the process. Institutional investment in faculty through endowments or clinical revenues will likely need to increase in the coming years due to the relative decreasing size of grants. Yet, radiology and radiation oncology are both high-revenue, translational fields, with the capacity to synergistically support clinical and research operations through large infrastructures that are mutually beneficial. These roadmap principles can provide a pathway for committed academic medical physics programs in scholarly leadership that will preserve medical physics as an active part of university academics.
Keywords: diagnostic, invention, imaging, linac, therapeutic, scholarship
1. INTRODUCTION
In the last few decades, there has been a notable struggle with the nuance of how research should be embedded within the field of medical physics, since it is an inherently clinically motivated profession.1 It is widely accepted that research is a part of the profession, but as with all clinical departments, each medical physics program/department struggles to balance their mission with the available resources and people. One estimate suggests that the number of medical physicists actively involved in research is less than 10% of the field.2 The percentage of AAPM members with NIH funding has continued to decrease from over 3% two decades ago to under 2% today,3 although this might be attributed to larger clinical vs research growth. A recent point/counterpoint article debated the argument about whether there is a need to explicitly include research training in CAMPEP training requirements.4 Although that debate was open-ended, there was a compelling argument that expanded research training was a necessary ingredient to a healthy program for PhD students. There is clearly less discussion about research inclusion in Master’s and Residency programs, where time limitations drive the training to didactic work and clinical apprenticeship.5 The more central questions are: How much emphasis is expected for faculty-led scholarly research within each medical physics program? When do PhD programs belong in an institution? These choices and the factors driving research programs are discussed here.
The recent consensus discussions around Medical Physics 3.0 offer some sense of a progressive balance point in the different areas necessary for future relevance, with research being a core component.6 However, it is clear that local driving factors create differences between institutions. Stated simplistically, large academic medical centers affiliated with research universities need to continue leading scholarly activity, because it is part of their institutional mission. The variations in this support often stem from the perceived tradeoff between research time and clinical time, which is an issue familiar to anyone with both academic and clinical appointments. This issue has always been hotly debated in physician subspecialties.7–9 At academic medical centers, which have a research mandate, it is resolved by the leadership helping to define their balance point.10 At nonacademic medical centers, there is less debate: these are places where clinical work takes precedence, and research is likely not supported as it is arguably not the mission of the institution. Successful research programs, usually associated with the Carnegie classification of Very High-Research Activity Universities, have major laboratory infrastructures, research support, and a commensurate expectation that these appointments lead to scholarship, successes in innovation, publication, and grant funding. Further-more, each individual faculty member’s continued academic appointment or advancement is predicated upon academic success. The faculty hiring goals and support systems are examined here.
Another major driving factor in research decision-making comes from leadership choices about how to leverage resources and think about new directions. The degree of support, motivation, and targeted hiring is driven by strategic decisions.11 Leadership positions should be clear, and their actions should be driven by trying to reach their aspirations for the program. The factors affecting these choices are discussed further here.
There are several ongoing evolutionary changes within medical physics, which will change the nature of established programs. For example, the topical areas of research within medical physics now include nontraditional skills such as computational science, data science, and biomedical engineering. Additionally, active researchers might optimally become the conduits to take academic research to commercial translation. For decades this was done via collaborations with industry, but this might increasingly be achieved through creation of new startup ventures. These changes to the definition of medical physics and the outcome measures of success need reassessment and thought about how they are holistically changing the nature of innovation, research, and donor/investment.
The core hypothesis of this paper is that in order to achieve success as an academic program within a research university, the programs must focus on the discovery and invention required of all successful science. In addition, new models of venture and enterprise formation can uniquely benefit medical physics. The key to the approach is that all phases are needed for success. So, this model for Discovery and Invention with Ventures and Engineering for Research Translation (DIVERT) is proposed here as a roadmap for developing academic research programs that succeed at their institution as well as internationally. The building blocks of a DIVERT research program are discussed here, which could be used as part of institutional strategic planning. These include:
Creativity and Sustaining of a research agenda
Strategic Partnerships to synergize and evolve
Quality Assessment of the outputs
Future Directions based upon aspirations and outcomes
The illustration in Fig. 1 shows the sequence of these, and each is described in the sections below.
FIG. 1.
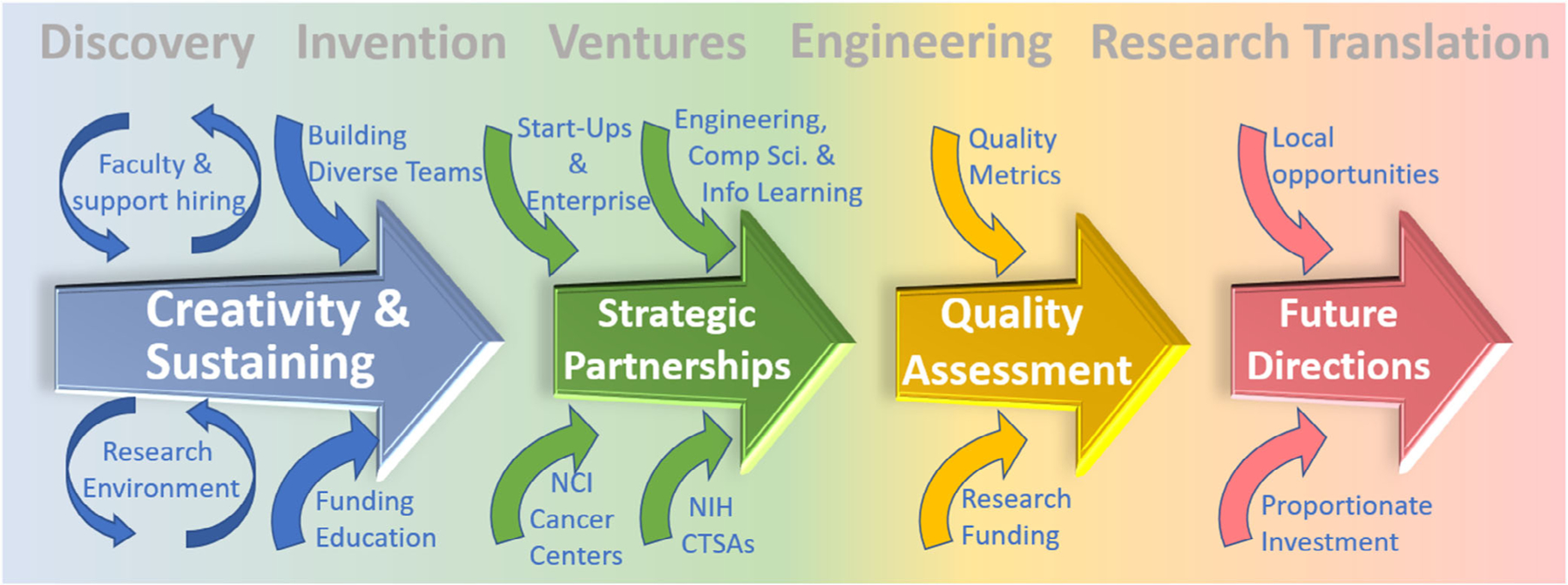
A schematic of the programmatic features of a progressive research program.
1.A. Creativity and sustaining
1.A.1. Hiring for a competitive, diverse, inventive environment
The fostering of competitive research comes both at the grassroots and leadership levels of each institution. The basic process underlying the program is that researchers are recruited faculty who exhibit an internal drive to participate in research and discover or intent things. Yet rather than rewarding them, it is common to place high burdens on their time and induce stress.12 However, the excitement to invent, discover, and design, are what drive a researcher. Successful engagement within the program requires active team-based activities as simple as journal clubs, research-based clinical rounds, and regular colloquia, as well as outreach activities that ensure national and global activity in research networks and funding. A locally engaged environment with national and international connectivity, provides the support for researchers and students who can compete successfully for funding and are leading in their field of study.13
Support for faculty hiring in clinical departments is always a point of discussion, based largely around financial support concerns. In terms of faculty hiring, the clinician-scientist type model is promoted at many larger academic medical centers for outstanding candidates, and this model could work for clinical–physicist–scientist. This model works as long as the candidates attract research funding that partially their salary support. Other programs grow their research portfolio through added research faculty slots or nontenure line research faculty that are also promoted and retained based upon grant support successes. Each of these approaches can work well if the right people are hired. However, beyond this ideal, the leadership in academic programs might ideally also participate in research to have it permeate the department.14,15 Academic medical centers hire department chairs and division leaders based upon their ability to balance all demands, including research, and so they set the tone and trends of the department.
Despite these research hiring practices, within a thriving academic medical center, not everyone has to do everything and an explicit acceptance of diversity in the team is critical. This of course means that research support only needs to affect part of the whole medical physics unit. Teams can work well with complementary skill sets and backgrounds, and so an active department will have people who are primarily clinical, people who are primarily educational, and people who are primarily research.16 True diversity supports a fully inclusive environment on many levels where the differences are brought out to celebrate the strength of each other. The real skill is building the teams so that the efforts are viewed as synergistic and inspirational and are not viewed as competing. The larger academic medical centers have a scale advantage of pooled indirect funds, and clinical/departmental funding to hire their own internal support people, including IT specialists, data analysts, assistant researchers, computational machine learning experts, and regulatory/trial support. Balancing people in hybrid positions so they are a split percentage in clinical and research roles can be useful to both residents and faculty after residency, and can help promote a diverse workforce. While all these features provide a good team environment, the core part of all major academic programs is the hiring of faculty who can become a leader in their field. They must be recruited based upon their creative vision and supplied with proportionate resources to succeed at bringing in strong research teams, and have dedicated research time.17 Without strategic and sustained research-focused hiring, there is diminishing potential for a leading research program, and open searches without predefined areas of focus can help bring in a wider set of researchers who can bring new ideas and diversity to the program.
1.A.2. Supporting continuous research
The process of bootstrapping inventive or discovery-based research is to build a department’s research activity using existing resources and to sustain and grow it iteratively. Each department and leadership must find their own emphasis here, weighted by the institution’s goals and priorities and their experiences. However, even within research intensive universities there are large variations between departments and divisions occur on issues of support for research activity vs education and clinical service. The core issue is usually that there is a real cost to research, in staff time, physical space and other resources. One study indicated that startup costs and support require a 40% input for every dollar of research funding gained.18 Given that most research funding largely supports salaries, this might suggest that this investment is not a net positive revenue. Each institution must choose to invest in it, or not, based upon their goals. One of the more compelling questions is: Can an institution find a halfway point between investing in research and not? There is not much data on this, although it could be argued that a marginal research program simply takes away support from other more superior programs within a university. At competitive universities, resources typically grow toward successful research programs, and in poor financial times the resources are often strategically cut from weaker academic programs. As with clinical programs, the success is measured by the outputs, and if the productivity or quality are not high, then support will likely diminish or shift to areas of higher productivity.
While institutional investment can be matched by income from grants and contracts, it is a bootstrapping exercise where there is likely no significant income or profit to the institution,18 only a continuous cycle of grants, contracts, hiring and spending near a breakeven level. Bootstrapping processes must be sustained to keep productivity and incentivization high, and with productivity comes the benefits of an economy of scale, where research resources can be jointly supported, and some revenues might be seen. The benefits of a large-scale operation come with a self-fulfilling prophecy to attract better researchers and research grants based upon the reputation of the existing system. The best of these synergistic programs takes decades and generations to build and is deeply based on invention of tools and techniques or basic discovery of fundamental insight in the world knowledge base. Conversely the atrophy of a well-developed department can also occur without constantly finding the right balance of financial support, resources, incentives, and investigator replenishment. A symptom of a department with this decreased potential for research is when the research is focused on iterative procedures or use of commercial devices exclusively.
1.A.3. Funding education synergistically with research
Support for education is a problem that is sometimes solved by scaling up, and several centers have done this by using tuition support from their CAMPEP accredited master’s program to fund teaching and PhD programs. While this works, it has inherent limits when extended to all PhD granting academic institutions, because of limits to the number of employment opportunities available to Master’s graduates. The CAMPEP data indicate limited residency match success for Master’s graduates (50 of 73 placed, 68.5%, in 2018 with a decreasing trend), while increasing preference appears to be for acceptance of PhD graduates (43 of 45 placed for 95.6% in 2018).19 So, programs that are funded by Master’s student tuition cannot scale to larger numbers of institutions20 without those graduates obtaining jobs outside of clinical medical physics.
Another approach to funding comes from direct research grant support. Approximately 75% of PhD students in physical science or engineering within universities are funded for tuition and stipend support from research. This mechanism has a second layer of benefit of having the grants be the acid test of whether the research experience of the students is provided by peer-reviewed grant funding.21 While it can be argued that grant support is hard to come by, the converse argument is that its existence is a quality indicator of a research program with national vetting. So, a program that funds its doctoral support at least partially via grants synergizes their education and research, by the competitive peer-reviewed vetting of the funding quality.
At times, education is taken as a surrogate for research, whereas really both are needed, and this can double the perceived drain on clinical time. Providing a strong education must be viewed as part of a strong research program, but of course neither are sufficient, and so the balance of supporting both is necessary.
1.A.4. CAMPEP certification constraints
A broken link was created by the CAMPEP ABR accreditation process of PhD programs, whereby medical physics graduates now go directly into clinical residencies, rarely entering post-doctoral training. Conversely, postdoctoral trainees without CAMPEP accredited training are blocked from clinical residencies.22 This educational paradigm has created a creativity roadblock in mid-level academic medical centers, balkanizing the medical physics training into an onramp for clinical service via residency. This has been articulated in many commentaries already,3,20,22,23 and is very similar to the issues existing with residency placement in physician-research training. To resolve this, some centers have created CAMPEP accredited certificate programs for postdoctoral trainees. These programs allow creative growth of the field by drawing from PhD researchers outside of medical physics, bringing in expertise in areas such as machine learning, data science, applied physics, or engineering.
Alternatively, a few pathways for CAMPEP PhD graduates have been created in split residency and research instructorships where they continue research while doing the residency, or others add on extra years of research onto the residency experience. This has the drawback of a lengthened training period at modest salary but has the benefit of placing the junior scientist on a higher potential academic track at the outset. This is much like a clinical residency or fellowship that allows research, providing a direct path to assistant professor positions. These programs depend on outstanding candidates and outstanding research institutional support to succeed. When done well, these can create the most competitive research in the field.
The problem of clinical residency is that the trainee is out of research for 2 yr and so can be limited by not having competitive research ideas. There are a number of clinical mentored training programs for this, such as the K23 award at the NIH which is considered a key stepping stone to advancing an academic medical career.24 Following the clinician-scientist model of most major academic centers would fit those clinical medical physicists. Perhaps creation of funded trainee programs for clinical/research medical physics faculty could be achieved.
1.B. Strategic partnerships
1.B.1. Comprehensive cancer centers as a partner & resource
The role of research and education in medicine is paramount. The US healthcare system has the most advanced technology available to it because of centuries of investment in research at leading medical centers. The NIH supports large infrastructure investments at these medical centers through competitive funding such as the Clinical Translational Science Awards Program (CTSA)25 or the Comprehensive Cancer Centers (CCCs).26 The National Cancer Institute vets and supports 51 CCCs in the country, and each must be defined as having expertise in three research areas including laboratory, clinical, and behavioral and population-based research. Each are expected to initiate and conduct early phase innovative clinical trials, conduct activities in outreach and education, and foster advances in healthcare technology, radiation oncology and radiology as part of them. The financial benefits of being part of these programs are critical for both the extramural funding and intrainstitutional support. Medical physics programs need to have active participation in their CCC or CTSA as a way of synergizing with the clinic research resources. There are many examples of successful programs where the principles of medical physics research advance the mission of the CCC through innovative technology introduction to the clinic, clinical trials on advanced hardware/software platforms, and even development of low-cost technology as an outreach to facilitate clinical medicine in low resource or rural settings. Notably, beyond institutions that are home to a CCC, these centers have a mandate for outreach, and satellite or regionally local institutions can establish partnerships with them. Taken as a whole, the CCC and CTSA paradigms are the ideal template for how to integrate clinical duties with research and education support. The field of medical physics is inherently linked into the CCCs mandate.
1.B.2. Academic-department partnerships — engineering, machine learning, information systems
The observation above about BME leads to a broader issue: How could an institution better synergize research by blending programs or finding partnerships across the institution, or between institutions? As stated, BME is a natural partner with medical physics and this could be better developed in many major universities, as recognized nearly 20 yr ago.27 This is perhaps the key strategic question for leadership in medical physics, because these partnerships lead to broader research programs, better bootstrapping of resources and finances, and provide a direct network of colleagues for scientific engagement without additional cost to the program. Partner programs where academic students integrate with clinical teams via student-based research projects can be highly synergistic. Another area for partnership comes from the growing need for computer science skills28 in automation and artificial intelligence through machine learning algorithms. Indeed, this single area of academics will likely have the largest impact on radiotherapy in the coming years, and those departments that embrace this research are already benefitting from being on the leading edge of this enormous growth curve.28–31 Partnership with or assimilation of these programs will undoubtedly be a growing trend in medical physics.31–33 Similar parallels might be drawn with data science, genetics, and applied physics, where partnerships or internal growth are driven by local strengths and synergies. In comparison, the applied nature of medical physics might not match well with some traditional basic science departments such as physics, mathematics, or computer science. Partnerships with graduate-only or research-only institutions can be a cost-free way to develop major research networks and growth in research programs.
1.B.3. Academic-industry partnerships
Radiotherapy and diagnostic radiology are fields dominated by large companies advancing highly integrated systems. Collaboration with industry in this space can be negotiated at the institutional level for major partnerships or by more limited individual investigator initiatives. The benefits of this leading to cutting edge technology and advancing high level diagnostic or therapy procedures is well documented, and is an integral part of modern medicine.34 Additionally, individual investigator partnerships with industry are commonly done in well-defined synergistic relationships to advance a technology. A number of NIH funding mechanisms have been created to foster these,35 such as the ongoing Industry-Academic Partnerships Program. The partnership to translate an idea or a tool matches the measures of success discussed previously, where a researcher can ensure that their ideas translate by prototyping it with a company that has the expertise and resources to advance it. One of the only practical, short-term pathways to translate a new technology into medicine is to have it advanced by a company.36,37
1.B.4. Academic-startup partnerships
Perhaps the most important partners can come from within the department by taking on new roles, when small scale academic-to-industry startup companies are formed by a handful of people with the goal of making a fundamentally new tool. Technology or tools invented at the institution are advanced along with building the company itself.38 In a thriving research environment, incubation and birth of startup companies is a key indicator of healthy transformative research.13 Many large academic institutions overtly support new homegrown startups to mature intellectual property by people who are the most vested in its success.39 Smaller medical centers are less likely to allow company incubation or tolerate faculty leaves for startup initiation, unlike larger academic centers. Many institutions realize now that this approach also spurs the creation of a wider donor/investor base around the institution itself. This can support new ventures and also help perpetuate a culture of investment and donor activity side by side.39 Alternatively, the small business granting programs SBIR and STTR both provide easier access to research and development funds than traditional grants for individual investigators. These can provide the conduit for younger researchers to test out new venture creation as an alternative to traditional academic research. Scientists can avail of entrepreneurial training opportunities, which are growing on most university campuses. Medical physics needs to be a part of this expanding opportunity and should specifically think of ways to foster and encourage innovation and entrepreneurship as an adjunct path to clinical physics. Perhaps the most beneficial part of this focus for medical physics is that it helps build enthusiasm for transformative research vs more iterative research models. This step of the DIVERT model is now becoming critical, because it not only helps focus on inventions that can translate but it can also help sustain the research activity of the program through extramural contact with researchers in the startups, as well as investment-based enterprise funding that is synergistic with the institutional donor base.
1.C. Quality assessment methods
1.C.1. Research funding — comparing biomedical engineering to medical physics
Research funding is one indicator of quality, yet it is only one aspect of success. Clearly, it is commonly used as a practical measure by institutions, where the finances may drive local enthusiasm. As shown in Fig. 2, the number of grants funded in Radiation studies (Diagnostic/Oncology are bundled together in the NIH Reporter) show a fluctuating, but largely steady support at about 1.2% of the NIH budget. By itself, this is a good indicator, but when contrasted with fields that are expanding, such as Biomedical Engineering (BME), it is interesting to note that in this same 20 yr period, BME has grown from 0.6% to 1.6% and arguably competes significantly with the field of medical physics. This competition was recognized as early as 2004,27 but research in BME is now on an apparently uninhibited growth trajectory,40 while research in medical physics is continuing to decline in relative numbers.3 Some of the more interdisciplinary programs in the country have blended or partnered BME and MP programs to provide synergy and broaden their research programs. This also helps scale the program up to a size that benefits from the larger pool of resources and activity.
FIG. 2.
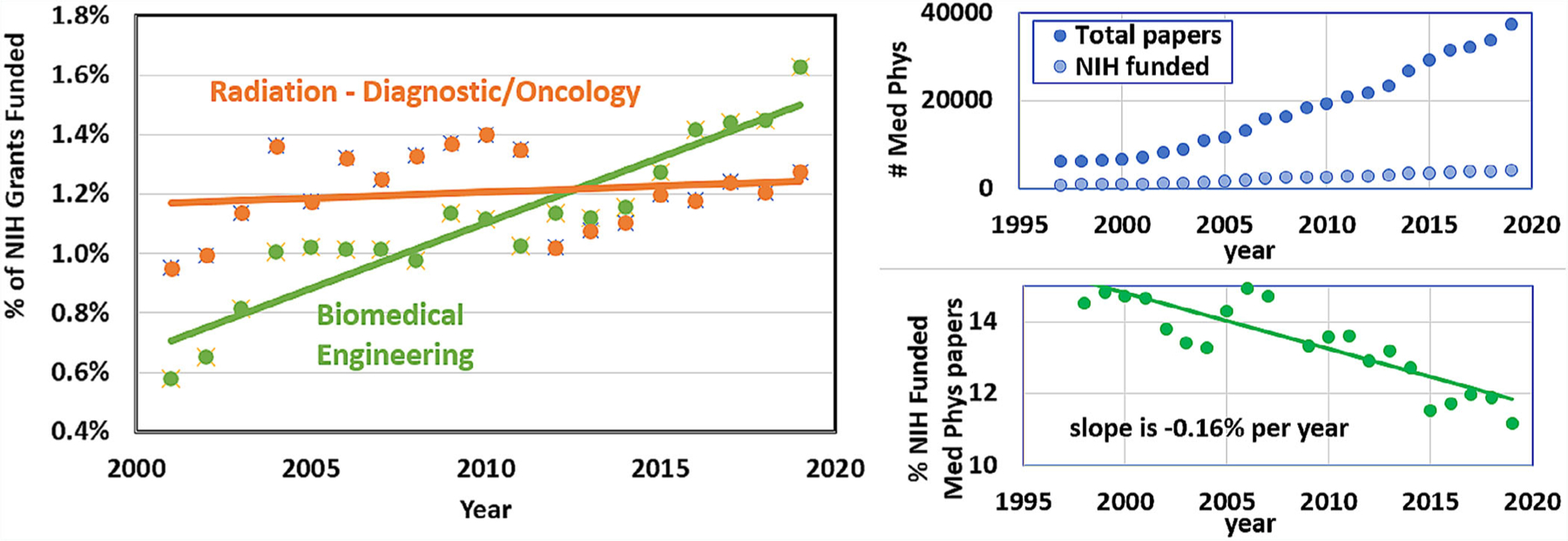
The percentage of funded grants from the National Institutes of Health (source: NIH Reporter) showing trends over 20 yr for Radiation-Diagnostic/Oncology departments and Biomedical Engineering departments. In (b) the total of all papers in the subject of medical physics is shown at right, with and those that are NIH funded. Below the fraction that are NIH funded has shown to decrease from near 15% to below 9% to date.
1.C.2. Metrics of success
A key question is: What is the best way to assess the productivity and quality of translational research to ensure that resources are balanced? This concept of measuring academic research quality is a deep area of exploration, with basic publication metrics such as impact factor, h-index, and CiteScore being common measures. Still, it is well recognized that publication metrics alone can be misguided output measures.41–45 Grant funding is commonly used as a blunt measure of peer-reviewed research quality.46 PhD student numbers are used to measure output and innovation.47 Holistic metrics focusing on product outputs and impact in the world would be ideal, if possible. One proposal, called the PQRST approach to measuring an academic’s success, was described recently.44 The acronym stands for five progressive measures of “success,” namely productivity, quality, repeatability, sharing, and translation. While productivity is easily measured by quantity of papers and grants, quality is more subtle and must include things like citation numbers of the papers, rather than impact factor of the journal. Repeated use of the work is a documented way to verify impact. Additionally, the sharing of resources or tools developed is an important step in science, and this is now mandated by several funding agencies and publishers. Finally, it seems clear that if research is truly successful there is a progression of activities that end in translation of the research to impact the world, such as production of industry product development or clinical trial translation. Implementation of these metrics can be included as part of the process of searching for and hiring new faculty, or at the milestones of evaluation such as promotions, tenure decisions, annual salary evaluations, or programmatic assessment.
1.D. Future directions
1.D.1. Future directions are driven by innovations from the faculty
There have been several workgroups, discussion panels, think tanks and review papers on research directions in medical physics, and these topics can be directly transcribed from any of these reports.6,48,49 Perhaps most importantly the investigators’ strengths and drive and the institutions’ capabilities must motivate the choice of topics. The academic faculty hiring process that requires researchers to self-identify their research program. Through the peer review process of grants and publications, they determine their path, which is influenced by institutional resources and their professional network growth. A savvy researcher has ample opportunity to shift direction to match areas of high impact. There is no substitute for competitive driven faculty who create a vision for their research, as invention and discovery are driven by them and their students. Additionally, there is always room for professional society leadership to help negotiate or lobby for the role of medical physics as an academic medical discipline, and to highlight the successes of in each part of the discovery, invention, venture, enterprise, and research translation. The DIVERT model proposed here is one way to frame the discussion and may be useful to propose the roadmap and methods for thinking about the problem. Part of the reason for proposing the model and the steps in the pathway are to clearly articulate the vision. Still, successes will be measured by both individual institutional efforts as well as professional society efforts that help Radiology and Therapeutic Radiological societies support these initiatives.
1.D.2. The luxury of research in a high-revenue field
The current state of Radiation Oncology, as in many therapeutic fields such as Surgery, continues to advance high-cost technology tools to make procedures safer and more precise. Indeed, these tools run counter to trends in most of medicine, such as family medicine, obstetrics, or gastroenterology, where less costly treatments are advocated for. Thus, medical physics is in the luxurious position of being able to innovate at both the low and high cost ends of research technology, and this should be taken advantage of. Discovery and innovation of new technologies must bring new capabilities or better safety and outcomes. The caveat to being a field with high revenue and expensive devices is that the investment in major research devices is expensive and must be maintained to be at the leading edge of the field. Research-intensive medical physics programs must be cognizant of investing in competitive devices and facilities to leverage joint clinical and research use in partnership.
1.D.3. Future funding for research and researchers at institutions
Research funding levels have not kept pace with inflation, and while there was a period where the NIH budget had doubled, inflation adjusted dollars indicate a flat funding level over the past two decades. During this time, faculty salaries in medical physics have grown. So, there is a real problem going forward that external research support for senior faculty salaries will continue to shrink. Of course, medical schools have been struggling with this issue for decades in clinician-scientist support. The solutions are not easy but can be related to using clinical revenue to support research or looking for ways to endow leading researchers. It is inevitable that funding will continue to lose pace with faculty salaries and that institutions will need to find their own ways to support faculty in research. This is a much larger issue for all the biomedical research world.
2. SUMMARY
Medical physicists have always had two roles, to support the goals of clinical medicine and to advance the technologies used in medicine. The former goal is critical but supporting the practice of medicine alone will not lead the field of research. We must also ensure that medical physics is an active field of academic scholarship, through creation of new knowledge. Medical physics leadership within academic medical centers must lead through promotion of innovation and enterprise, as proposed here within the DIVERT model. While there is an altruistic motivation of ensuring that medical physics continues to grow, there is also the practical motivation of gaining more institutions financially supporting medical physics as a scholarly field. The starting place for all scholarly science is discovery and invention-based programming, which comes directly from faculty and students who are brought in with that as their focus. The steps proposed here within the model are designed to clarify the need to DIVERT attention to the components that matter the most for successful academic leadership.
Clearly not all institutions will have the capacity or leadership structure to allow active research to happen, and this is part of the uneven playing field across the spectrum of institutions. Academic medical centers that have limited funding or limited capacity to hire innovative faculty will have problems succeeding in this pathway and likely have more decisions to make about which departments to support. Additionally, the positioning of medical physics faculty within clinical departments may not provide support for a technological research agenda. These are challenging issues that may not have ideal solutions. The steps proposed here can help to bootstrap activity that could lead toward better institutional support, but of course there are no guarantees.
The role of major professional societies such as the AAPM could be an important adjunct to the institutional steps proposed. One of the reasons for proposing the DIVERT model is to simply articulate and visually illustrate what is needed. Discussion between AAPM, RSNA, and ASRTO could be beneficial, and hopefully this vision of a roadmap can be leveraged toward the discussion. However, institutional leadership needs to take the initiatives discussed here, independent of any professional society support in order to gain local institutional success in academic scholarship. So, the major motivation for this article is to provide a roadmap that individual investigators and leaders can use to think about what is possible to bootstrap their own activity. Academic medical physics programs should lead by designing their own balance of clinical work, education, and research innovation.
ACKNOWLEDGMENTS
This work was partially funded by NCI grant P30CA023108.
Footnotes
CONFLICT OF INTEREST
The authors have no conflict to disclose relevant to this article.
REFERENCES
- 1.Orton CG, Giger ML. A brief history of the AAPM: celebrating 60 years of contributions to medical physics practice and science. Med Phys. 2018;45:497–501. [DOI] [PubMed] [Google Scholar]
- 2.Bortfeld T, Jeraj R. The physical basis and future of radiation therapy. Br J Radiol. 2011;84:485–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Whelan B, Moros EG, Fahrig R, et al. Development and testing of a database of NIH research funding of AAPM members: a report from the AAPM Working Group for the Development of a Research Database (WGDRD). Med Phys. 2017;44:1590–1601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williamson JF, Das I, White G. The current CAMPEP graduate program didactic course guidelines have insufficiently rigorous requirements for research training. Med Phys. 2020;47:5403–5407. [DOI] [PubMed] [Google Scholar]
- 5.Prisciandaro JI, Willis CE, Burmeister JW, et al. Essentials and guidelines for clinical medical physics residency training programs: executive summary of AAPM Report Number 249. J Appl Clin Med Phys. 2014;15:4763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Samei E, Pawlicki T, Bourland D, et al. Redefining and reinvigorating the role of physics in clinical medicine: a report from the AAPM Medical Physics 3.0 Ad Hoc Committee. Med Phys. 2018;45:e783–e789. [DOI] [PubMed] [Google Scholar]
- 7.Stein CM. Academic clinical research: death by a thousand clicks. Sci Transl Med. 2015;7:318fs49. [DOI] [PubMed] [Google Scholar]
- 8.Dunn AN, Walsh RM, Lipman JM, et al. Can an academic RVU model balance the clinical and research challenges in surgery? J Surg Educ. 2020;77:1473–1480. [DOI] [PubMed] [Google Scholar]
- 9.Feghali-Bostwick C, Harvey J, Hasseler C, Lee-Chavarria D, Halushka P. A team-based translational journal club: understanding the translational research highway. J Clin Transl Sci. 2019;3:291–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baroutjian A, Sutherland M, Hoff JJ, et al. The impact of hospital/university affiliation on research productivity among US-based authors in the fields of trauma, surgical critical care, acute care, and emergency general surgery. Am Surg. 2021;87:30–38. [DOI] [PubMed] [Google Scholar]
- 11.Ma OJ, Hedges JR, Newgard CD. The academic RVU: ten years developing a metric for and financially incenting academic productivity at Oregon Health & Science University. Acad Med. 2017;92:1138–1144. [DOI] [PubMed] [Google Scholar]
- 12.Dorsey ER, Van Wuyckhuyse BC, Beck CA, Passalacqua WP, Guzick DS. The economics of new faculty hires in basic science. Acad Med. 2009;84:26–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pogue BW. Grant funding needs parallel the start-up venture: an analogy for translational research success. J Biomed Opt. 2018;23:1–3. [DOI] [PubMed] [Google Scholar]
- 14.Bennis W, Biederman PW. Organizing Genius: The Secrets of Creative Collaboration. Revised ed; 2007: Addison-Wesley Publishing Company, Inc. [Google Scholar]
- 15.Singh SN, Mishra S, Kim D. Research-related burnout among faculty in higher education. Psychol Rep. 1998;83:463–473. [DOI] [PubMed] [Google Scholar]
- 16.Rosewall T, Kelly V, Higgins J, et al. The influence of programmatic change on radiation therapist research capacity-a single-center case study. J Med Imaging Radiat Sci. 2009;40:170–177. [DOI] [PubMed] [Google Scholar]
- 17.Libby AM, Ingbar DH, Nearing KA, Moss M, Albino J. Developing senior leadership for clinical and translational science. J Clin Transl Sci. 2018;2:124–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rathmell WK, Brown NJ, Kilburg RR. Transformation to academic leadership: the role of mentorship and executive coaching. Consult Psychol J. 2019;71:141–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Commission on Accreditation of Medical Physics Education Programs. Available from: http://campep.org/.
- 20.Mills MD, Elson HR, Orton CG. The terminal M.S. degree is no longer appropriate for students interested in a career in clinical medical physics in the United States. Med Phys. 2011;38:1737–1739. [DOI] [PubMed] [Google Scholar]
- 21.Knight D, Kinoshita T, Choe N, Borrego M. Doctoral student funding portfolios across and within engineering, life sciences and physical sciences. Stud Grad Postdoct Educ. 2018;9:75–90. [Google Scholar]
- 22.Fullerton GD, Vanek KN, Orton CG. Point/Counterpoint: the 2014 initiative is not only unnecessary but it constitutes a threat to the future of medical physics. Med Phys. 2011;38:5267–5270. [DOI] [PubMed] [Google Scholar]
- 23.Halvorsen PH, Mills MD. The next decade for clinical medical physics. J Appl Clin Med Phys. 2014;15:5334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Culican SM, Rupp JD, Margolis TP. Retaining clinician-scientists: nature versus nurture. Invest Ophthalmol Vis Sci. 2014;55:3219–3222. [DOI] [PubMed] [Google Scholar]
- 25.Printz C NCATS advisory council recommends strategies to strengthen CTSA program. Clin Transl Sci. 2014;7:349–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.NCI-Designated Cancer Centers. Available from: https://www.cancer.gov/research/infrastructure/cancer-centers.
- 27.Kruger RL, Curran BH, Hendee WR. The growth of biomedical engineering is a major challenge to medical physics. Med Phys. 2004;31:2375–2376. [DOI] [PubMed] [Google Scholar]
- 28.Kang J, Thompson RF, Aneja S, et al. National Cancer Institute Workshop on artificial intelligence in radiation oncology: training the next generation. Pract Radiat Oncol. 2020;20:30155–30157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thompson RF, Valdes G, Fuller CD, et al. Artificial intelligence in radiation oncology: a specialty-wide disruptive transformation? Radiother Oncol. 2018;129:421–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mak RH, Endres MG, Paik JH, et al. Use of crowd innovation to develop an artificial intelligence-based solution for radiation therapy targeting. JAMA Oncol. 2019;5:654–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dercle L, Henry T, Carre A, Paragios N, Deutsch E, Robert C. Reinventing radiation therapy with machine learning and imaging bio-markers (radiomics): state-of-the-art, challenges and perspectives. Methods. 2020;19:30318–30324. [DOI] [PubMed] [Google Scholar]
- 32.Seo H, Badiei Khuzani M, Vasudevan V, et al. Machine learning techniques for biomedical image segmentation: an overview of technical aspects and introduction to state-of-art applications. Med Phys. 2020;47: e148–e167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kang J, Rancati T, Lee S, et al. Machine learning and radiogenomics: lessons learned and future directions. Front Oncol. 2018;8:228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lewin JS. Industrial-academic research relationships: departmental collaborations. Radiology. 2009;250:23–27. [DOI] [PubMed] [Google Scholar]
- 35.Clarke LP. NCI initiative: development of novel imaging technologies. Med Phys. 2000;27:1699–1701. [DOI] [PubMed] [Google Scholar]
- 36.Tolikas M, Antoniou A, Ingber DE. The Wyss institute: a new model for medical technology innovation and translation across the academic-industrial interface. Bioeng Transl Med. 2017;2:247–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Letourneur D, Joyce K, Chauvierre C, Bayon Y, Pandit A. Enabling MedTech translation in academia: redefining value proposition with updated regulations. Adv Healthc Mater. 2020;10:2001237. [DOI] [PubMed] [Google Scholar]
- 38.Manbachi A, Kreamer-Tonin K, Walch P, et al. Starting a medical technology venture as a young academic innovator or student entrepreneur. Ann Biomed Eng. 2018;46:1–13. [DOI] [PubMed] [Google Scholar]
- 39.Pisano GP. Can science be a business? Lessons from biotech. Harv Bus Rev. 2006;84:114–124. [PubMed] [Google Scholar]
- 40.Katona PG. Biomedical engineering: a field on the move. Conf Proc IEEE Eng Med Biol Soc. 2004;2004:5457. [DOI] [PubMed] [Google Scholar]
- 41.Aziz NA, Rozing MP. Profit (p)-index: the degree to which authors profit from co-authors. PLoS One. 2013;8:e59814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Koroulakis A, Rice SR, DeCesaris C, Knight N, Nichols EM. Perceptions and patterns in academic publishing: a survey of United States residents in radiation oncology. Adv Radiat Oncol. 2020;5:146–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Trapp JV. The new Scopus CiteScore formula and the Journal Impact Factor: a look at top ranking journals and middle ranking journals in the Scopus categories of General Physics and Astronomy, Materials Science, General Medicine and Social Sciences. Phys Eng Sci Med. 2020;43:739–748. [DOI] [PubMed] [Google Scholar]
- 44.Ioannidis JP, Khoury MJ. Assessing value in biomedical research: the PQRST of appraisal and reward. JAMA. 2014;312:483–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ioannidis JP, Greenland S, Hlatky MA, et al. Increasing value and reducing waste in research design, conduct, and analysis. Lancet. 2014;383:166–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Iyengar R, Wang Y, Chow J, Charney DS. An integrated approach to evaluate faculty members’ research performance. Acad Med. 2009;84:1610–1616. [DOI] [PubMed] [Google Scholar]
- 47.Wootton R A simple, generalizable method for measuring individual research productivity and its use in the long-term analysis of departmental performance, including between-country comparisons. Health Res Policy Syst. 2013;11:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cumberlin RL, Coleman CN. Research in medical physics. Int J Radiat Oncol Biol Phys. 2001;49:891–895. [DOI] [PubMed] [Google Scholar]
- 49.Mills MD. The future of medical physics in the US health-care system. J Appl Clin Med Phys. 2013;14:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]


