Abstract
Importance:
Seasonal changes in blood pressure (BP) are associated with increased cardiovascular events and mortality during the winter months. Previous BP seasonality studies have been limited to single regions or not explored patterns in processes linked to care for people with hypertension that may accompany this seasonality. We characterized seasonal variation in population-based BP control measures using the national PCORnet® Blood Pressure Control Laboratory Surveillance System (BP Track) and evaluated the association between outdoor temperature and BP control variation.
Design:
We used repeated cross-sectional queries of electronic health record (EHR) data from 26 health systems across nine US geographic regions representing 21 states that participated in BP Track. Four BP control and BP-related process metrics summarized for quarterly series of 12-month measurement periods from January 2017 through March 2020 were used in the analysis. Aggregate weighted results were presented by calendar quarters (Quarters 1 – Quarter 4) and year. Weighted generalized linear models with repeated measures were used to investigate changes in BP control metrics across seasons (measured as calendar quarters), and to quantify the association between outdoor temperature and BP metrics. Average outdoor temperature and precipitation data by state were obtained from the National Oceanic and Atmospheric Administration (NOAA).
Participants:
Adults who had at least one ambulatory visit during a 12-month measurement period at the health system, and a hypertension diagnosis during the first six months of the measurement period or at any time prior.
Main Outcome Variables:
BP control, and three BP-related process metrics: BP improvement, medication intensification, average SBP reduction after medication intensification
Results:
Among the 1,667,149 people with hypertension diagnosis included in this study for the most recent measurement period (April 2019-March 2020), the majority were over 65 years of age (53.8%), female (51.3%), White non-Hispanic (75.8%), and had stage 1 or stage 2 hypertension (62.9%). Across all regions, BP Control and BP-related process metrics were highest in the warmer seasons (Quarters 2 and 3) and lowest in the colder seasons (Quarters 1 and 4). Quarter 2 had the highest percentage of people with improved BP (31.95±0.90%) and the highest average SBP reduction after medication intensification (16±0.23mmHg average reduction). Quarter 3 had the highest percentage of people with BP controlled (62.25±2.55%) and the lowest percentage of visits with medication intensification (9.73±0.60%). Results were largely consistent in models adjusting for age, sex, race, ethnicity and comorbidities. Average outdoor temperature was associated with BP control metrics in unadjusted models, but associations were attenuated following adjustment for age, sex, race, ethnicity, health system type (academic, non-academic, federally qualified health center [FQHC]), health system location population (urban, suburban, rural) and precipitation.
Conclusions:
In this large, national, EHR-based study, BP control and BP-related process metrics improved during warmer seasons compared with colder seasons, but outdoor temperature was not associated with performance following adjustment for potential confounders.
INTRODUCTION
Cardiovascular disease (CVD) continues to be the leading cause of death in the US and worldwide.1,2 Rates of CVD events and mortality increase in colder months, a finding that has been replicated in multiple countries.3,4 A potential contributor to this increased CVD risk is the rise in both systolic and diastolic mean BPs that occurs during winter months compared to summer months. This seasonal phenomenon has been reported in numerous countries with diverse climate conditions and across hypertensive, normotensive, treated and untreated populations.[5–13] Seasonal changes may be associated with larger BP variations than those induced by BP reduction therapy in certain settings.13 At a population level, these seasonal changes have important clinical implications for the estimated 720 million adults with uncontrolled hypertension worldwide,14 and for other groups at elevated CVD event risk.14,15,16
Management of seasonal BP changes has been addressed in several recent international treatment guidelines, including the European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability Recommendations15 and the International Society of Hypertension’s 2020 Global Hypertension Practice Guidelines.16 The recommendations include confirmation of seasonal BP changes by taking repeated measurements with home or ambulatory BP monitoring, and consideration of possible down-titration for BP levels below the recommended goal, particularly when symptoms suggest over-treatment. In the US, a small number of BP seasonality studies have been conducted, but are limited to specific populations or small regions of the country.[17–20] To date, there are no studies that explore BP seasonal variation for adults with hypertension across the US, nor any studies that investigate seasonal fluctuation in BP control metrics, such as BP control or antihypertension medication intensification. Therefore, we aimed to estimate the magnitude of the seasonal variation in population-based BP control measures in the US, and the extent to which outdoor temperature explains this variation using data from the PCORnet® Blood Pressure Control Laboratory Surveillance System (BP Track), a national BP surveillance system.21,22
METHODS
BP Track is a US-based surveillance system that leverages PCORnet®, the National Patient-Centered Clinical Research Network, for standardized electronic health record (EHR) data, and provides infrastructure for longitudinal tracking of BP control and BP-related process metrics.21,22 Participating health systems map their EHR data to a research-ready format that conforms to the PCORnet® Common Data Model (CDM), allowing for standardized querying of data in a distributed environment for research and surveillance purposes. Data quality is maintained through quarterly data curation efforts and quality checks. BP Track queries run in semi-annual waves against the PCORnet® CDM and calculate the BP control outcome and process metrics in a quarterly series of 12-month measurement periods from January 2017 to the most recent complete quarter data available. Query results from each health system are combined and compared for data quality assessment and outlier detection. The BP Track data used in this analysis was from the fifth wave, which included measurement periods beginning at each calendar quarter from January 2017 to March 2020, totaling 10 measurement periods for 26 participating health systems, as depicted in Supplementary Figure S1 in Appendix I. Calendar quarters are defined as Quarter 1 (January-March), Quarter 2 (April-June), Quarter 3 (July-September) and Quarter 4 (October-December). The contiguous US is divided into nine geographic regions of adjoining states with historically consistent climates.23 BP Track data was mapped to these nine regions based on the states where health systems are located, then linked to climate data and assembled into an analytic dataset. A map of the regions and their corresponding states is provided in Supplementary Figure S2.
Study Population
We included patients from 26 participating health systems in 21 states. Eligible patients were 18 to 85 years of age, had at least one ambulatory visit during the 12-month measurement period at the health system, and had an outpatient encounter with hypertension diagnosis (based on International Classification of Diseases, Ninth and Tenth Revision [ICD-9, ICD-10] codes described in Appendix II) during the first six months of the measurement period or at any time prior to the measurement period. Patients who were pregnant, had hospice services, end-stage renal disease, dialysis, renal transplant, received care based on an institutional special needs plan or were residing in a long-term care facility during the measurement period were excluded from analysis.22 Detailed information on eligibility inclusion and exclusion criteria is provided in Appendix II.
BP Control Metrics
BP Track data includes BP control and BP-related process measures to track processes linked to improving care for patients with hypertension based on recommendations in current guidelines.22,24,25 Full technical specification for all metrics are described elsewhere.22 Our study used BP control and three related process metrics for this analysis, and detailed definitions are provided in Appendix II. In brief, the metrics are defined as follows:
BP control, defined as the percentage of people with hypertension whose BP measurement at the most recent ambulatory visit within the 12-month measurement period was <140/<90 mmHg (National Quality Forum 0018),22,26
Improvement in blood pressure, defined as the percentage of people with hypertension and either a reduction of 10 mmHg in systolic blood pressure (SBP) or achievement of SBP<140 mmHg during the most recent visit occurred in the last quarter of the measurement period among people with an SBP not controlled in the previous three quarters,22,27
Medication intensification, the percentage of visits with an added new class of antihypertensive medication following a visit with uncontrolled BP that occurred during the last quarter of the measurement period,22 and
Average SBP reduction after medication intensification, defined as the SBP change observed between a visit with medication intensification occurred in the last quarter of the measurement period and a subsequent visit within that same quarter.22
In a sensitivity analysis, BP control was defined as the percentage of people with a hypertension diagnosis whose most recent BP measurement at an ambulatory visit was <130/<80 mmHg, according to the 2017 Hypertension Clinical Practice Guidelines.24,25 Each metric was calculated for each of the 26 health systems across 10 measurement periods, by demographic groups of age, sex, race and ethnicity. Metric definitions are based on the most recent visit or a visit that occurred during the last three months of a measurement period. Therefore, all metrics were indexed to the last quarter of their corresponding measurement periods, as illustrated in Supplementary Figure S1.
Climate Data
Temperature and precipitation data were derived from the National Oceanic and Atmospheric Administration’s (NOAA) National Centers for Environmental Information. State-level monthly temperature and precipitation averages are computed by averaging the daily maximum and minimum temperatures, and daily total rainfall and melted frozen precipitation in hundredth-s of inches, respectively, reported by climate stations within each state.28 This monthly data was obtained for years 2017 to 2020, and a 3-month average temperature and precipitation values for each quarter-year were calculated for each state. States were classified into nine climate geographic regions, as shown in the map provided in Supplementary Figure S2, and linked to the BP Track data by state, region and quarter-year.
Statistical Analysis
Descriptive summaries of the participating health systems and contributing patients were produced, and weighted quarterly averages for each BP metric were calculated across all participating health systems.
A weighted generalized linear model with repeated measures was used to investigate the variation within each BP metric across seasons (represented by calendar quarters). Weights were based on the number of observations contributed by each health system for all metrics except for the average SBP reduction after medication intensification, where 1/standard error for each health system was used. Health systems serve similar populations over time, and therefore measurements within each health system were included as the repeated measure using an autoregressive correlation structure. Evidence indicates SBPs and DBPs are lower in summer months and higher in winter,[9,12,29,30] and therefore Quarter 2 (April-June) was expected to have intermediate BP Control levels compared to other quarters and was used as the reference period, providing a reasonable baseline for exploring the relative increases and decreases to BP metrics. Model-based means, estimated differences (95% CI) by quarter and the overall p-values were presented for each metric. Both unadjusted and adjusted model results were provided, where adjustment variables include age, sex, race, ethnicity, prevalence of diabetes, coronary artery disease, heart failure and average outdoor climate temperature.
A second weighted generalized linear model with repeated measures was used to quantify the association between temperature and BP metrics. The unadjusted model included quarterly average temperature by state. Measurements within each health system were repeated utilizing an autoregressive correlation structure. The linearity assumption was tested using natural cubic splines, and when violated, two linear piece-wise splines were created with a knot assignment based on visual examination of non-linearity at 50 degrees. The average change in metric per five-degree Fahrenheit increase in average temperature and associated p-values were estimated for each metric. The adjustment variables included region, age, sex, race, ethnicity, prevalence of diabetes, coronary artery disease, heart failure, health system type (academic, non-academic, federally qualified health center [FQHC]), health system location population (urban, suburban, rural) and state-level average climate precipitation. For non-linear associations, spline plots depicting the non-linear and potential linear relationships were presented.
We also conducted two sensitivity analyses to assess consistency of seasonal variation by BP control definition and data completeness. The first used the updated BP control definition from the 2017 Hypertension Clinical Practice Guidelines (SBP/DBP <130/<80 mmHg)24,25 as a metric in all models. The second was a complete case analysis that included 22 of the 26 health systems with complete data across nine measurement periods (Q4–2017 through Q4–2019). The 10th measurement period was removed from this analysis since a third of health systems did not have data for this period. The four health systems excluded represent four states in three regions. All analyses were performed by the Duke Clinical Research Institute (Durham, NC) using in SAS 9.4 (SAS Institute, Cary, NC, USA) and R version 4.0 (ggplot2_3.3.5, R Core Team).
RESULTS
A total of 26 health systems across 21 states and nine climate regions participated in the fifth wave of BP Track. Most (77%) are affiliated with an academic institution, all serve people in urban or suburban areas, and half also serve people in rural settings. The clinics within the health systems are located across all nine geographic regions of the country, with over half on the east coast. Health system characteristics are provided in Table 1.
Table 1.
Characteristics of participants included in the most complete measurement period, Q3–2018 to Q3–2019
| Patient Characteristics (N=1,818,041) | Distribution % | |
|---|---|---|
|
| ||
| Age | ||
| 18-44 | 8.9% | |
| 45-64 | 38.9% | |
| 65 and over | 52.2% | |
| Sex | ||
| Female | 52.1% | |
| Male | 47.9% | |
| Race/Ethnicity | ||
| White Non-Hispanic | 69.8% | |
| Black Non-Hispanic | 14.1% | |
| Asian Non-Hispanic | 2.2% | |
| Hispanic | 8.6% | |
| Other Race/Ethnicity | 5.3% | |
| Blood Pressure Stage at Baseline | ||
| Normal BP | 16.3% | |
| Elevated BP | 15.2% | |
| Stage1HTN | 32.9% | |
| Stage2HTN | 31.9% | |
| Missing1 | 3.7% | |
| Comorbidities | ||
| Diabetes | 28.0% | |
| Coronary Artery Disease | 17.3% | |
| Heart Failure | 6.4% | |
| Region | ||
| East North Central (ENC) | 24.6% | |
| Northeast (NE) | 19.4% | |
| South (S) | 17.2% | |
| Southeast (SE) | 15.6% | |
| South West (SW) | 12.6% | |
| Central (C) | 8.3% | |
| West North Central (WNC) | 1.7% | |
| West (W) | 0.4% | |
| North West (NW) | 0.2% | |
People with hypertension diagnosis who did not have both SBD and DBP measurements during the measurement period.
Population baseline characteristics were similar across different measurement periods, albeit the number of eligible patients varied. Among the 1,667,149 people with hypertension diagnosis included in this study for the most recent measurement period (Q1–2019 through Q1–2020), the majority were over 65 years of age (53.8%), female (51.3%), White non-Hispanic (75.8%), and had stage 1 or stage 2 hypertension (62.9%). Nearly one-third (27.3%) had a diagnosis of diabetes, 18.2% of coronary artery disease, and 6.8% of heart failure. Baseline characteristics for the most recent measurement period are provided in Table 2.
Table 2.
Model-based means and estimated differences in BP control and BP-related process metrics across quarters, Q4-2017 – Q1-2020
| Quarter 1 | Quarter21 | Quarter 3 | Quarter 4 | Overall | |||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| BP Metric | Mean (SD) | Δ Estimate (95% CI) |
Mean (SD) | Δ Estimate (95% CI) |
Mean (SD) | Δ Estimate (95% CI) |
Mean (SD) | Δ Estimate (95% CI) |
P-Value |
|
| |||||||||
| % BP Control (<140/<90 mmHg) | |||||||||
| Unadjusted model2 | 60.71 (2.59) | −1.07 (−1.27, −0.87) | 61.79 (2.57) | 0 (Ref) | 62.25 (2.55) | 0.46 (0.21, 0.72) | 61.51 (2.57) | −0.27 (−0.72, 0.18) | <.001 |
| Adjusted model | 55.72 (2.40) | −3.88 (−13.42, 5.65) | 59.61 (3.89) | 0 (Ref) | 61.62 (5.43) | 2.02 (−1.41, 5.45) | 58.38 (1.88) | −1.23 (−8.38, 5.93) | 0.010 |
| % Improvement in BP | |||||||||
| Unadjusted model2 | 29.22 (1.01) | −2.73 (−3.52, −1.93) | 31.95 (0.90) | 0 (Ref) | 29.88 (0.79) | −2.07 (−2.49, −1.65) | 28.93 (0.75) | −3.01 (−3.60, −2.43) | <.001 |
| Adjusted model | 24.61 (1.61) | −2.41 (−5.89, 1.07) | 27.02 (1.78) | 0 (Ref) | 24.72 (2.28) | −2.29 (−3.94, −0.65) | 24.34 (1.40) | −2.67 (−5.28, −0.07) | <.001 |
| % Medication Intensification | |||||||||
| Unadjusted model2 | 10.52 (0.54) | 0.25 (−0.03, 0.53) | 10.27 (0.59) | 0 (Ref) | 9.73 (0.60) | −0.54 (−0.73, −0.35) | 10.23 (0.58) | −0.04 (−0.34, 0.26) | 0.005 |
| Adjusted model | 14.29 (1.65) | 1.50 (−1.65, 4.64) | 12.79 (1.59) | 0 (Ref) | 12.05 (1.89) | −0.74 (−1.73, 0.25) | 13.92 (1.60) | 1.12 (−1.45, 3.70) | 0.240 |
| Average SBP Reduction after Med Intensification (mmHg) | |||||||||
| Unadjusted model2 | 15 (0.22) | −0.73 (−1.01, −0.44) | 16 (0.23) | 0 (Ref) | 15 (0.28) | −0.89 (−1.19, −0.58) | 14 (0.25) | −1.46 (−1.76, −1.16) | <.001 |
| Adjusted model | 10 (0.38) | −1.82 (−2.71, −0.94) | 12 (0.37) | 0 (Ref) | 12 (0.57) | −0.17 (−0.73, 0.38) | 10 (0.37) | −2.40 (−3.15, −1.65) | <.001 |
Quarter 2 was used as reference to estimate differences between quarters
Unadjusted model: Quarter Year only
Adjusted model: Unadjusted model+Race/Ethnicity+Sex+Age+Diabetes+HF+CAD+Average Temperature
Figure 1 displays the distribution of weighted averages for each BP control metric by region across all quarter-years. Box plots demonstrating the overall seasonal variation by quarters are provided in Figure 2. Model-based means and estimated BP metric differences across quarters are provided in Table 3. Overall, across all regions, performance was highest in the spring/summer quarters (2 and 3) and lowest in the fall/winter quarters (1 and 4). Unadjusted results (adjustment for year only) showed Quarter 3 had with the highest percentage of people with BP controlled (62.25±2.55%) and the lowest percentage of visits with medication intensification (9.73±0.60%). Quarter 2 had the highest percentage of people with improved BP (31.95±0.90%) and the highest average SBP reduction after medication intensification (16±0.23 mmHg average reduction). Conversely, the lowest percentages of people with BP controlled were observed in Quarter 1 (60.71±2.59%), which also showed the highest percentage of medication intensification (10.52±0.54%). The lowest percentage of people with improved BP (28.93±0.75%) and the lowest average SBP reduction after medication intensification (14±0.25 mmHg average reduction) were observed in Quarter 4. All BP metrics followed a similar trend in models adjusting for age, sex, race, ethnicity and comorbidities. Results were also largely consistent when including average outdoor temperature in the adjusted models (Table 3).
Figure 1.
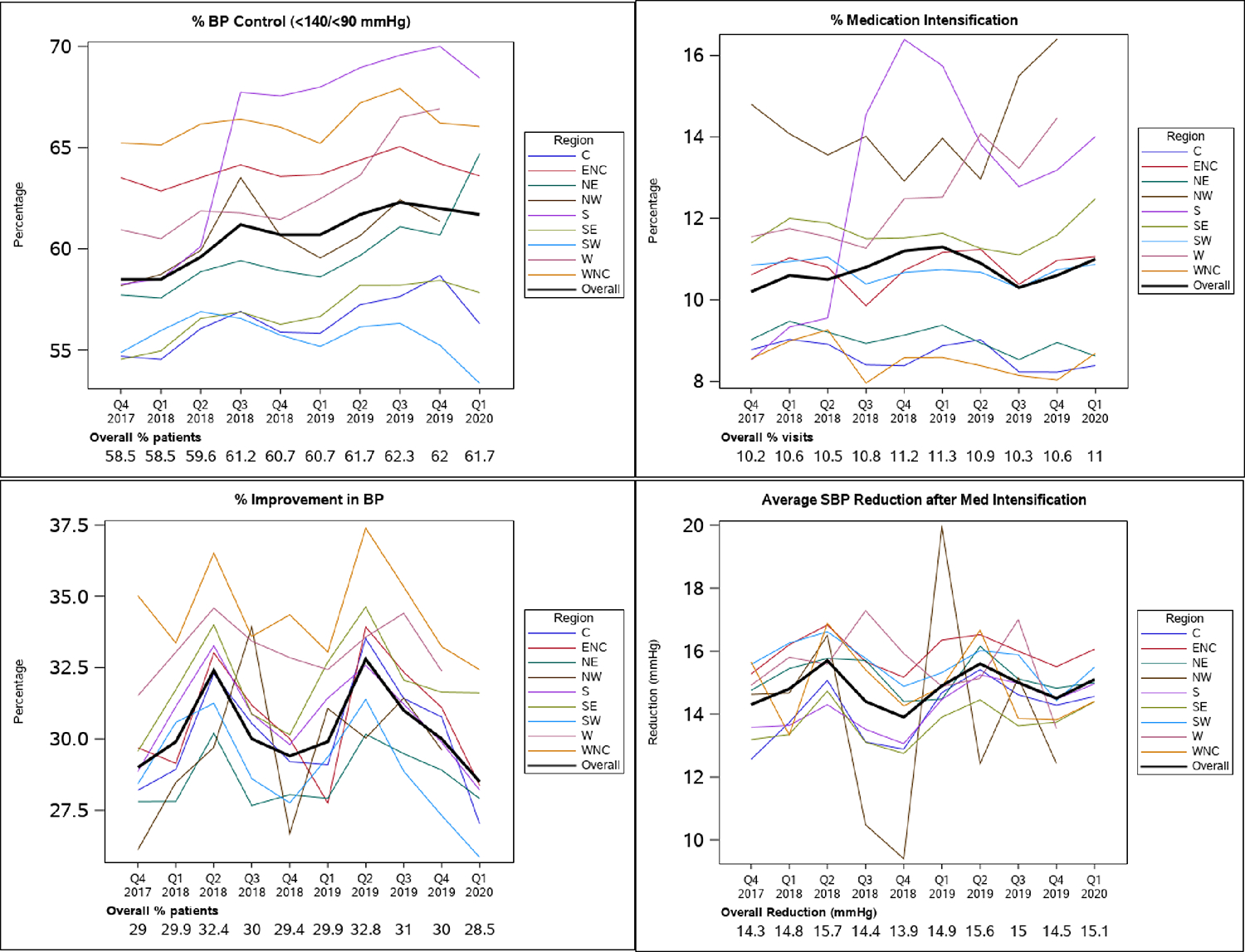
Weighted BP control and BP-related process metrics over time by region, Q4-2017 – Q1-2020
Figure 2.
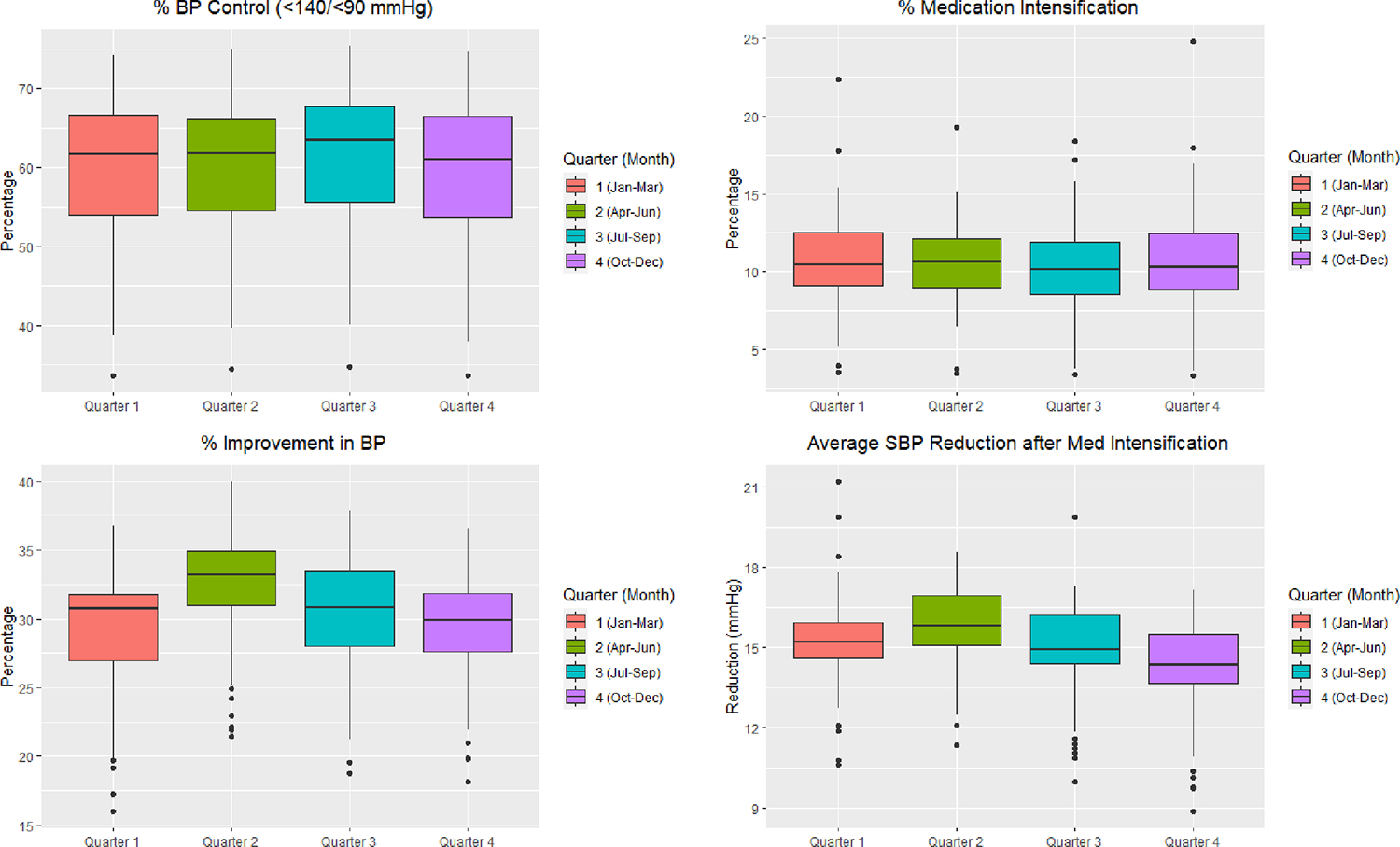
Distributions of overall BP control and BP-related process metrics by Quarter1
1 Metric distributions are based on raw values from data.
Relationships between average outdoor temperature and BP metrics are displayed in Figure 3. The association between temperature and BP control disappeared following adjustment for demographic, comorbidities, health system type (academic, non-academic, federally qualified health center [FQHC]), health system location population (urban, suburban, rural) and climate precipitation (Supplementary Table S1). In adjusted models, we observed a negative association between temperature and medication intensification (−0.16 (95% CI: −0.28, −0.04) per 5 degrees Fahrenheit increase in average temperature. Figure 3 also depicts the observed non-linear relationship between average temperature and percent of people with improved BP, with a positive association for temperatures below 50 degrees Fahrenheit (0.48 (95% CI: 0.24, 0.71)) and a negative association for temperatures above 50 degrees (−0.30 (95% CI: −0.53, −0.07)). No association was observed between the average SBP reduction after medication intensification metric and temperature (Figure 3 and Supplementary Table S1).
Figure 3.
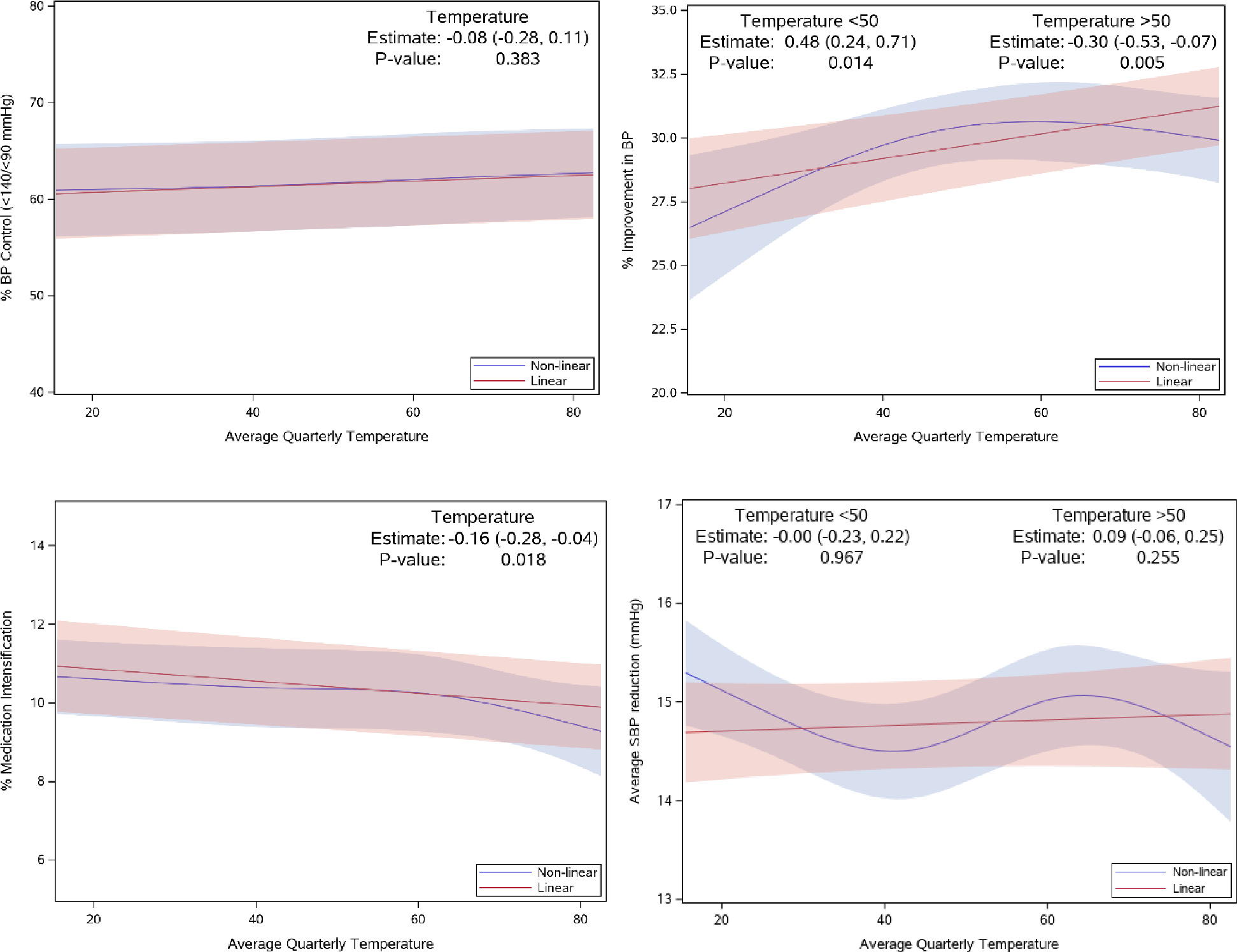
Spline plots for BP control and BP-related process metrics depicting linear and non-linear relationships with average quarterly outdoor temperature1
1 Estimates and p-values are from adjusted models.
BP Metric result=Averagetemperature+Region+Year+Race/Ethnicity+Sex+Age+Diabetes+Precipitation+Health System Factors+HF+CAD
In sensitivity analyses, we observed similar results to those using our original definition of BP control (Supplementary Table S2, S3, Figure S3). Seasonal trends were similar, with the lowest percentage shown in Quarter 1 and highest in Quarter 3. Analyses of relationship between average temperature and the secondary BP control metric also produced similar results (Supplementary Table S3). Additionally, estimates from the complete case analysis were consistent for all primary BP control and related metrics with overall added precision (Supplementary Table S4).
DISCUSSION
We evaluated seasonal variation in BP control and BP-related process metrics using standardized EHR data from a national BP surveillance system. Our study’s main finding was that BP control and related metrics improved during warmer seasons and worsen during colder seasons. Improvement in BP reaches a high in Quarter 2 (April-June), when the highest SBP reductions are also observed with or without medication intensification. The percentage of people with BP controlled to <140/<90 mmHg increased from Quarter 2 to Quarter 3 (July-September), then decreased, reaching the lowest percentage in Quarter 1 (January-March), when the highest percentage of visits with medication intensification was also observed. Results were largely consistent in models adjusting for age, sex, race, ethnicity and comorbidities. State average outdoor temperature was associated with BP control in unadjusted models, but associations were attenuated following adjustment for age, sex, race, ethnicity, comorbidities, health system factors and precipitation, and did not explain the seasonal variability.
The largest average decreases in BP measurements occurred in the months of April through June, while more people reached BP control in July through September. This observed lag in trend across BP metrics may be due to the different amplitudes in BP improvement across seasons. In unadjusted models, the estimated average SBP reduction after medication intensification was higher in Quarter 2 (16±0.23mmHg average reduction) than in Quarter 3 (15±0.28mmHg average reduction). Moreover, the 2020 International Society of Hypertension Global Hypertension Practice Guideline indicates the average BP decline in the summer is 5/3 mmHg (systolic/diastolic),16 which does not meet our threshold of BP improvement of 10 mmHg reduction in SBP. Additionally, a study conducted in the US that investigated the relationship between outdoor temperature and BP among older men found that cumulative exposure to decreasing outdoor and perceived temperatures can increase BP,19 which may also explain the lowest BP improvement observed in the months of October through December while the lowest number of people with BP controlled occurred in the months of January through March. When adjusted for temperature, seasonal variation for percent of visits with medication intensification was no longer statistically significant, and substantial imprecision was introduced to all estimates (Supplementary Table S1). This is expected given the strong association between different seasons and changes in the outdoor average temperatures.
Prior studies have found outdoor temperature to be a primary driver of BP seasonality.[17–19,31] In our analysis of outdoor climate temperature and BP metrics, we observed small associations in unadjusted models, which were attenuated following adjustment for confounders. The large majority of prior studies reporting strong associations between outdoor temperature and BP seasonal variation were confined to short-term exposure and measurements (e.g. 24-hr, 7-day),[17,19,20,31] which were not available in our data. The observed weak association in our analysis may also represent other seasonal determinants besides outdoor climate temperature that contribute to the seasonal BP control metric variation and its magnitude. In addition to temperature and precipitation, seasonality is markedly characterized by other environmental factors such as change in daytime length and hours of sunlight, particularly in non-equatorial regions. A recent study found exposure to higher solar UV radiation to be associated with lower SBP, and that it independently contributes to the BP seasonal variation.32 Various studies have reported overall increased springtime and summertime physical activity due to yard work, exercise and longer time spent in other physical activities, which favorably influences BP levels.33,34 Additionally, energy intake generally increases in wintertime, which unfavorably impacts BP.35,36 Some studies suggested that home heating and reduced exposure to cold climate may be particularly effective in avoiding BP rise.36,37 Another study found the effects of seasonality and personal-level environmental temperature to be two independent predictors on ambulatory BP monitoring, where air temperature affects daytime SBP, and seasonality (measured in daylight hours) affects nighttime SBP.31 Thus, interfering factors that may explain the seasonal fluctuations observed in our study include change in daylight exposure, levels of physical activity, behavior, body weight, cigarette smoking, dietary intake and living environments.[31–39] A notable finding in our study is the U-shaped relationship between climate temperature and the percent of people with improved BP, indicating extreme low and high levels in temperatures decrease the number of people with BP improvement. This mirrors the U-shaped relationship often found in temperature and cardiovascular events, where extreme high and low levels increases risk.38
Our finding that BP fluctuation occurs in people with hypertension across the US and impacts the trend of hypertension management process metrics is consistent with international management guidelines, which incorporate seasonality considerations into care recommendations. The European Society of Hypertension working group recommends consideration of tapering of antihypertensive medications in hot weather when BP is below the recommended target.15 A recent review suggests early adjustment of antihypertensive medications before winter and summer months would suppress the excessive seasonal BP variations.8 These seasonal adjustments may be an important treatment target for prevention of cardiovascular events and mortality, particularly the excess occurred during the winter months.40 Additionally, a seasonality component in BP control must be considered in the interpretation of study findings, as results from evaluating interventions that do not account for BP seasonality may not provide an accurate measure of the intervention effects.41 Finally, our findings have implications on longitudinal quality monitoring of population health and population-based interventions for hypertension management, providing evidence of the need for a more periodic surveillance of BP control than one- or two-year cycles of survey data.
We recognize some important limitations in our study. First, the health systems included in our analysis overrepresent academic medical centers that serve mostly urban and suburban populations. Therefore, results are not representative of non-academic health systems or the general population with hypertension. Moreover, urban and suburban communities are more likely to have accessibility to indoor temperature control, potentially preventing BP from rising as much during the colder months8,9 and underestimating the magnitude of the seasonal variation in the results. Second, medication intensification follows a seasonal pattern, which likely contributes to the fluctuation of the average SBP reduction after medication intensification metric in addition to the true effects of seasons in SBP changes. Third, BP Track data does not collect patient-level information so no adjustments can be made on patient characteristics other than age, sex, race, ethnicity and prevalence in comorbidity (diagnosis of diabetes, coronary artery disease and heart failure) at the health system level. For example, other seasonal factors such as weight, dietary or behavior changes cannot be included in our models. Fourth, the climate data in the study are monthly temperature and precipitation values averaged over three months for each quarter, and the qualifying BP measurements for each metric could have occurred any time within the quarter. Consequently, the climate data are not perfect measures of the outdoor temperature and precipitation to which people were exposed, and such data limitations considerably influence the associations between temperature and metrics reported in this study. Finally, the magnitude of changes we observed in population-based seasonal BP control metrics was modest. Actual changes may be greater than the results reported in this study, as BP variation has been found to be less pronounced for ambulatory than home measurements.29
CONCLUSIONS
In this large, national, EHR-based study, BP control and BP-related process metrics improved during warmer seasons compared with colder seasons, but average outdoor temperature was not associated with performance following adjustment for potential confounders. Future work to evaluate the impact of seasonal changes in BP management on clinical outcomes is needed.
Supplementary Material
REFERENCES
- 1.Centers for Disease Control and Prevention. Leading Causes of Death Reports, 2020. CDC WISQARS Online Database. Atlanta, GA: Centers for Disease Control and Prevention; 2020. Accessed January 11, 2022. [Google Scholar]
- 2.World Health Organization (WHO). The Top 10 Causes of Death. WHO’s Global Health Estimates 2020: Deaths by Cause, Age, Sex, by Country and by Region, 2000–2019. Geneva: World Health Organization. Accessed December 03, 2021. [Google Scholar]
- 3.Madaniyazi Lina, Armstrong Ben, Chung Yeonseung, Chris Fook Sheng, Xerxes Seposo, Yoonhee Kim, Aurelio Tobias, Yuming Guo, Francesco Sera, Yasushi Honda, Antonio Gasparrini, Masahiro Hashizume, the Multi-Country Multi-City (MCC) Collaborative Research Network, Seasonal variation in mortality and the role of temperature: a multi-country multi-city study, International Journal of Epidemiology, 2021. [Google Scholar]
- 4.Stewart S, Keates AK, Redfern A, McMurray JJV. Seasonal variations in cardiovascular disease. Nat Rev Cardiol. 2017 Nov;14(11):654–664. doi: 10.1038/nrcardio.2017.76. Epub 2017 May 18. [DOI] [PubMed] [Google Scholar]
- 5.Modesti PA, Rapi S, Rogolino A, Tosi B, Galanti G. Seasonal blood pressure variation: implications for cardiovascular risk stratification. Hypertens Res 2018; 41:475–482. [DOI] [PubMed] [Google Scholar]
- 6.Wang Q, Li C, Guo Y, Barnett AG, Tong S, Phung D, et al. Environmental ambient temperature and blood pressure in adults: a systematic review and meta-analysis. Sci Total Environ 2017; 575:276–286. [DOI] [PubMed] [Google Scholar]
- 7.Kollias A, Kyriakoulis KG, Stambolliu E, Ntineri A, Anagnostopoulos I, Stergiou GS. Seasonal blood pressure variation assessed by different measurement methods: systematic review and meta-analysis. J Hypertens. 2020. May;38(5):791–798. [DOI] [PubMed] [Google Scholar]
- 8.Narita K, Hoshide S, Kario K. Seasonal variation in blood pressure: current evidence and recommendations for hypertension management. Hypertens Res. 2021. Nov;44(11):1363–1372. [DOI] [PubMed] [Google Scholar]
- 9.Lewington S, Li L, Sherliker P, Guo Y, Millwood I, Bian Z, et al. Seasonal variation in blood pressure and its relationship with outdoor temperature in 10 diverse regions of China: the China Kadoorie Biobank. J Hypertens 2012; 30:1383–1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goyal A, Narang K, Ahluwalia G, Sohal PM, Singh B, Chhabra ST, Aslam N, Mohan B, Wander GS. Seasonal variation in 24 h blood pressure profile in healthy adults- A prospective observational study. J Hum Hypertens. 2019. Aug;33(8):626–633. [DOI] [PubMed] [Google Scholar]
- 11.Alperovitch A, Lacombe JM, Hanon O, Dartigues JF, Ritchie K, Ducimetière P, et al. Relationship between blood pressure and outdoor temperature in a large sample of elderly individuals: the Three-City study. Arch Int Med 2009; 169:75–80. [DOI] [PubMed] [Google Scholar]
- 12.Narita K, Hoshide S, Kanegae H, Kario K. Seasonal Variation in Masked Nocturnal Hypertension: The J-HOP Nocturnal Blood Pressure Study. Am J Hypertens. 2021. Jun 22;34(6):609–618. doi: 10.1093/ajh/hpaa193. [DOI] [PubMed] [Google Scholar]
- 13.Brennan PJ, Greenberg G, Miall WE, Thompson SG. Seasonal variation in arterial blood pressure. Br Med J Clin Res Ed) 1982; 285:919–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.NCD Risk Factor Collaboration (NCD-RisC) (2021). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. The Lancet, 398(10304), 957–980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stergiou GS, Palatini P, Modesti PA, Asayama K, Asmar R, Bilo G, de la Sierra A, Dolan E, Head G, Kario K, Kollias A, Manios E, Mihailidou AS, Myers M, Niiranen T, Ohkubo T, Protogerou A, Wang J, O’Brien E, Parati G. Seasonal variation in blood pressure: Evidence, consensus and recommendations for clinical practice. Consensus statement by the European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. J Hypertens. 2020. Jul;38(7):1235–1243 [DOI] [PubMed] [Google Scholar]
- 16.Unger Thomas, Borghi Claudio, Charchar Fadi, Khan Nadia A., Poulter Neil R., Prabhakaran Dorairaj, Ramirez Agustin, Schlaich Markus, Stergiou George S., Tomaszewski Maciej, Wainford Richard D., Williams Bryan, Schutte Aletta E.. 2020. International Society of Hypertension Global Hypertension Practice Guidelines. [DOI] [PubMed] [Google Scholar]
- 17.Kent ST, Howard G, Crosson WL, Prineas R, & McClure LA (2011). The association of remotely-sensed outdoor temperature with blood pressure levels in REGARDS: a cross-sectional study of a large, national cohort of African-American and white participants. Environmental Health, 10, 7 - 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jehn M, Appel LJ, Sacks FM, Miller ER 3rd; DASH Collaborative Research Group. The effect of ambient temperature and barometric pressure on ambulatory blood pressure variability. Am J Hypertens 2002; 15:941–945. [DOI] [PubMed] [Google Scholar]
- 19.Halonen JI, Zanobetti A, Sparrow D, Vokonas PS, Schwartz J. Relationship between outdoor temperature and blood pressure. Occup Environ Med. 2011;68(4):296–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dashti HS, Aslibekyan S, Scheer FA, Smith CE, Lamon-Fava S, Jacques P, et al. Clock genes explain a large proportion of phenotypic variance in systolic blood pressure and this control is not modified by environmental temperature. Am J Hypertens 2016; 29:132–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pletcher MJ, et al. The PCORnet Blood Pressure Control Laboratory: A Platform for Surveillance and Efficient Trials. Circ Cardiovasc Qual Outcomes. 2020. Mar;13(3):e006115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cooper-Dehoff RM, Fontil V, Carton T, Chamberlain AM, Todd J, O’Brien EC, Shaw KM, Smith M, Choi S, Nilles EK, Ford D, Tecson KM, Dennar PE, Ahmad F, Wu S, McClay JC, Azar K, Singh R, Modrow MF, … Pletcher MJ. (2021). Tracking blood pressure control performance and process metrics in 25 US health systems: The Pcornet blood pressure control laboratory. Journal of the American Heart Association, 10(21), [e022224]. 10.1161/JAHA.121.022224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thomas R. Karl and Walter James Koss. Regional and National Monthly, Seasonal, and Annual Temperature Weighted by Area, 1895–1983. Historical Climatology Series 4–3, 1984. National Climatic Data Center, Asheville, NC, 38 pp. [Google Scholar]
- 24.Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, et al. 2017/ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2018;138:e426–e483. https://pubmed.ncbi.nlm.nih.gov/30354655/ [DOI] [PubMed] [Google Scholar]
- 25.Casey DE, Thomas RJ, Bhalla V, Commodore-Mensah Y, Heidenreich PA, Kolte D, Muntner P, Smith SC, Spertus JA, Windle JR, et al. 2019 AHA/ACC clinical performance and quality measures for adults with high blood pressure: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. Circ Cardiovasc Qual Outcomes. 2019;12:e000057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Quality ID #236 (NQF 0018): controlling high blood pressure—national quality strategy domain: effective clinical care. Available at: www.acr.org/-/media/ACR/NOINDEX/Measures/2018_Measure_236_Registry.pdf. Accessed December 30, 2021.
- 27.eCQI. Hypertension: improvement in blood pressure. 2018. Available at: https://ecqi.healthit.gov/sites/default/files/ecqm/measures/CMS65v7.html. Accessed October 30 2020. [Google Scholar]
- 28.Physical Sciences Laboratory. Glossary of Terms. Available at: https://psl.noaa.gov/data/usclimate/glossary.html. Accessed January 20, 2022. [Google Scholar]
- 29.Sega R, Cesana G, Bombelli M, Grassi G, Stella ML, Zanchetti A, et al. Seasonal variations in home and ambulatory blood pressure in the PAMELA population. Pressione Arteriose Monitorate e Loro Associazioni. J Hypertens 1998; 16:1585–1592. [DOI] [PubMed] [Google Scholar]
- 30.Charach Gideon & Rabinovich Pavel & Weintraub Moshe. (2004). Seasonal Changes in Blood Pressure and Frequency of Related Complications in Elderly Israeli Patients with Essential Hypertension. Gerontology. 50. 315–21. 10.1159/000079130. [DOI] [PubMed] [Google Scholar]
- 31.Modesti PA, Morabito M, Massetti L, Rapi S, Orlandini S, Mancia G, et al. Seasonal blood pressure changes: an independent relationship with temperature and daylight hours. Hypertension 2013; 61:908–914. [DOI] [PubMed] [Google Scholar]
- 32.Weller RB, Wang Y, He J, Maddux FW, Usvyat L, Zhang H, Feelisch M, & Kotanko P (2020). Does Incident Solar Ultraviolet Radiation Lower Blood Pressure? Journal of the American Heart Association: Cardiovascular and Cerebrovascular Disease, 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Matthews CE, Freedson PS, Hebert JR, Stanek EJ 3rd, Merriam PA, Rosal MC, et al. Seasonal variation in household, occupational, and leisure time physical activity: longitudinal analyses from the seasonal variation of blood cholesterol study. Am J Epidemiol 2001; 153:172–183. [DOI] [PubMed] [Google Scholar]
- 34.Garriga A, Sempere-Rubio N, Molina-Prados MJ, Faubel R. Impact of Seasonality on Physical Activity: A Systematic Review. Int J Environ Res Public Health. 2021;19(1):2. Published 2021 Dec 21. doi: 10.3390/ijerph19010002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stelmach-Mardas M, Kleiser C, Uzhova I, Peñalvo JL, La Torre G, Palys W, Lojko D, Nimptsch K, Suwalska A, Linseisen J, Saulle R, Colamesta V, Boeing H. Seasonality of food groups and total energy intake: a systematic review and meta-analysis. Eur J Clin Nutr. 2016. Jun;70(6):700–8. [DOI] [PubMed] [Google Scholar]
- 36.Ma Y, Olendzki BC, Li W, Hafner AR, Chiriboga D, Hebert JR, et al. Seasonal variation in food intake, physical activity, and body weight in a predominantly overweight population. Eur J Clin Nutr 2006; 60:519–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kristal-Boneh E, Harari G, Green MS, Ribak J. Summer–winter variation in 24 h ambulatory blood pressure. Blood Press Monitor 1996; 1:87–94. [PubMed] [Google Scholar]
- 38.Brook RD, Weder AB, Rajagopalan S. ‘Environmental hypertensionology’ the effects of environmental factors on blood pressure in clinical practice and research. J Clin Hypertens (Greenwich) 2011; 13:836–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Algert CS, Roberts CL, Shand AW,Morris JM, Ford JB. Seasonal variation in pregnancy hypertension is correlated with sunlight intensity. Am J Obstet Gynecol 2010;203: e211–5. [DOI] [PubMed] [Google Scholar]
- 40.Barnett AG, Sans S, Salomaa V, Kuulasmaa K, Dobson AJ. The effect of temperature on systolic blood pressure. Blood Press Monit 2007; 12:195–203. [DOI] [PubMed] [Google Scholar]
- 41.Gepts T, Nguyen AM, Cleland C, Wu W, Pham-Singer H, Shelley D. Accounting for Blood Pressure Seasonality Alters Evaluation of Practice-Level Blood Pressure Control Intervention. Am J Hypertens. 2020. Mar 13;33(3):220–222. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


