A key tenet of primary care is that continuity of care is central to the patient-physician relationship. Long revered but seldom studied, continuity of care has in the past been spared the rigorous evaluation now demanded by an evidence-conscious marketplace. But there is growing evidence that having consistent contact with a physician or other health professional is good medicine.
In the best and most recent interventional study of continuity of care, Wasson et al found that increased continuity was associated with a decreased risk of hospitalization and shorter stays.1 This study was limited to elderly veterans, so the findings cannot be generalized to other groups. However, observational studies have found that continuity of care is associated with decreased emergency department (ED) use and hospitalization in both children and adults2,3,4 and with timely administration of vaccinations.5
Building causal arguments based on observational data is perilous. Nevertheless, the associations found between continuity of care and decreased hospitalizations fulfill many of the criteria used to determine causality. First is the strength of the association. Continuity of care is associated with as much as a 50% reduction in ED use and hospitalization. Second, some studies have found apparent “dose-response” relationships between decreasing continuity of care and increasing risk of ED use and hospitalization. Third, there is consistency of findings across different settings and with different patient groups. Fourth, the appropriate temporal relationship has been found between the exposure and the outcomes—the continuity of care was antecedent to ED visitation or hospitalization. Finally, there is “clinical plausibility” to the findings.
Why are these findings plausible? Compliance with medications is affected by how well patients know their prescribing physicians.6 For some conditions, such as asthma, compliance with medication regimens could well protect against ED use or hospitalization. In support of this, we have found that children with asthma had a higher risk of hospitalization associated with lower continuity than was the case for all children combined.4 Greater continuity of care is also associated with physicians' improved awareness of children's psychosocial problems.7 This knowledge may enable providers to identify which patients can be safely managed at home or even by telephone, thereby avoiding visits to an ED and possibly even hospitalizations. Having a relationship with a physician might increase parents' or patients' interest in seeing that particular physician when they are not urgently ill, rather than attending the ED. In other words, patients may opt to wait 12 hours for a known provider rather than visit the ED at night to see an unknown one. In fact, the efficacy of “gatekeeping” may be considerably enhanced in situations when patients and providers know each other well. Finally, ED physicians have been shown to be more likely to admit patients to the hospital when follow-up is uncertain, as may be the case when continuity of care is poor.
There are good reasons why continuity of care has occupied a central role in the patient-physician relationship. Unfortunately, many current changes in health care delivery may threaten it. The larger size of physician groups, the increasing use of physician extenders, and the shifting allegiances of health plans with physicians all may hamper patients' or providers' attempts to establish and maintain consistent contact. Now more than ever, the value of continuity of care must be recognized.
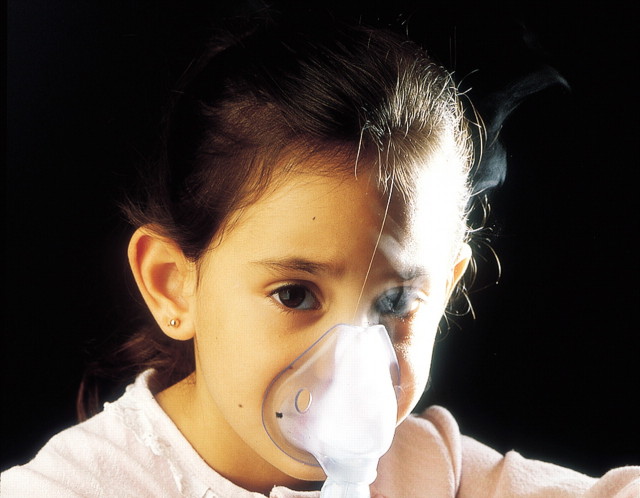
Figure 1.
Continued care will improve her compliance with asthma treatment [Oscar Burriel/SPL]
Competing interests: None declared
References
- 1.Wasson JH, Sauvigne AE, Mogielnicki RP, et al. Continuity of outpatient medical care in elderly men: a randomized trial. JAMA 1984;252: 2413-2417. [PubMed] [Google Scholar]
- 2.Gill JM, Mainous AG III. The role of provider continuity in preventing hospitalizations. Arch Fam Med 1998;7: 352-357. [DOI] [PubMed] [Google Scholar]
- 3.Gill JM, Mainous AG III, Nsereko M. The effect of continuity of care on emergency department use. Arch Fam Med 2000;9: 333-338. [DOI] [PubMed] [Google Scholar]
- 4.Christakis DA, Mell L, Koepsell TD, Zimmerman FJ, Connell FA. Association of lower continuity of care with greater risk of emergency department use and hospitalization in children. Pediatrics 2001;107: 524-529. [DOI] [PubMed] [Google Scholar]
- 5.Christakis DA, Mell L, Wright JA, Davis R, Connell FA. The association between greater continuity of care and timely measles-mumps-rubella vaccination. Am J Public Health 2000;90: 962-965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Charney E, Bynum R, Eldredge D, et al. How well do patients take oral penicillin? a collaborative study in private practice. Pediatrics 1967;40: 188-195. [PubMed] [Google Scholar]
- 7.Kelleher KJ, Childs GE, Wasserman RC, McInerny TK, Nutting PA, Gardner WP. Insurance status and recognition of psychosocial problems: a report from the Pediatric Research in Office Settings and the Ambulatory Sentinel Practice Networks. Arch Pediatr Adolesc Med 1997;151: 1109-1115. [DOI] [PubMed] [Google Scholar]