Abstract
Physical activity has numerous health benefits for people with physical disabilities. Nevertheless, activity levels are often below recommended levels. To promote physical activity among children and adolescents who use a wheelchair as their primary source of mobility, this systematic review explores the physical activity patterns of this group. A systematic search of PubMed, Sports Medicine & Education Index, Web of Science, and SPORTDiscus was performed, included articles were synthesized in terms of duration, intensity, and settings in which physical activity occurred, as well as the physical activity measurement methods. Nine articles were included. The mean overall physical activity level across the included studies was 98 minutes per day (range: 78–115 minutes per day). Two articles analysed the duration of physical activity at different intensities (very light physical activity, light physical activity (LPA), moderate to vigorous physical activity (MVPA) and intensities near to maximum). Within the included articles, both subjective and objective measurement methods were used. Due to the small number of articles, combined with small sample sizes, there is not enough evidence to answer the research questions sufficiently. Nevertheless, the review provides an overview of actual research and clearly shows that the physical activity values are insufficiently researched. There is a need for further research on the scope, types and settings of physical activity in the target group.
Keywords: Physical disability, Sports, Physical exercise, Youth
Introduction
Physical activity (PA) “involves people moving, acting and performing in different contexts and settings” [1] and is associated with numerous health benefits for all people [2–4]. In particular, PA improves health, balance, muscle strength, and endurance, counteracts diseases, such as osteoporosis; and increases functional independence, social integration, and life satisfaction [5–7]. Furthermore, PA has important implications for the prevention of obesity, high blood pressure, low fitness levels, and negative clinical outcomes [8, 9]. Engaging in PA and in active lifestyles during childhood and adolescence is crucial, as habits established during this phase frequently persist into adulthood [10].
For children and adolescents with physical disabilities (PD), which the International Classification of Functioning, Disability, and Health defined as impairments, activity limitations, and participation restrictions [11, 12], participating in regular PA is particularly important but challenging: The World Health Organization (WHO) developed PA guidelines for people with disabilities in 2020 [13]. As indicated by these guidelines children and adolescents with PD who are between 5 and 19 years old should perform at least an average of 60 min per day of moderate-to-vigorous-physical-activity (MVPA), especially aerobic activity. Furthermore, muscle and bone strengthening should be incorporated at least three days per week [13, 14]. Additionally, Choi et al. [15] and Sol et al. [16] revealed the positive impact of practice-based interventions on the PA levels of children and adolescents with PD. Consequently, PA is of enormous importance for children and adolescents with PD [17, 18].
Despite this, Bloemen et al. [19] and Sit et al. [20] found that the daily lives of children and adolescents with PD were characterized by high levels of physical inactivity. For example, children and adolescents with PD like Spina Bifida or cerebral palsy are significantly less physically active than their peers without PD [21, 22]. As disabilities can affect mental, physical, and/or developmental impairments [23], children and adolescents with PD face specific barriers: Several reviews have provided an overview of empirical research on PA among youth with PD and identified barriers to PA, such as a lack of appropriate PA programs and insufficient family support [24–26].
As a sub-group of children and adolescents with PD, children and adolescents who use a wheelchair as their primary source of mobility and mode of transport (CAUW) experience various wheelchair-related PA limitations [27]. Like children and adolescents with PD, they often perform less than the aforementioned 60 min of MVPA per day [22, 28]. CAUW face several barriers to participation in leisure and sports activities such as accessibility of playgrounds and sport facilities as well as seasonal effects [16, 29]. Further there are several challenges related to integrating PA into their daily routine due to a lack of suitable opportunities [30].
CAUW’s insufficient PA levels are reflected in their health status. Several studies have shown that wheelchair users have higher body mass index, body fat percentage, and cholesterol levels as well as higher blood glucose concentrations than able bodied individuals [31, 32]. Wheelchair users are also at a higher risk of developing upper extremity overuse injuries, peripheral nerve entrapment, and pressure sores that affect the sacrum and ischial tuberosities [33]. However, PA and sports can help to prevent such injuries [33].
To promote PA in daily life among CAUW, it is important to understand their PA patterns and habits, including how, how often, and where they engage in PA [13], as well as the proportion of CAUW who comply with the WHO PA recommendations. However, to the best of our knowledge, no studies have focused on the PA patterns of CAUW exclusively. To address this gap, the present review aimed to synthesize studies on the PA patterns of CAUW to understand PA duration, intensity levels, types, and contexts [34] and summarize the methods used to measure PA.
Methods
This systematic review was performed and is reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [35].
Eligibility criteria
Articles that met the inclusion criteria were included in the present review. Articles that met one or more of the exclusion criteria were excluded. The criteria are listed in Table 1.
Table 1.
Inclusion and exclusion criteria
| Inclusion Criteria | Exclusion Criteria | |
|---|---|---|
| Measurement Method | Objective or subjective measurement of PA | |
| Outcome | PA type, contexts, duration, and patterns | Outcome(s) related to sedentary behavior |
| Population |
• CAUW aged 5–19 years old • Mean age of 5–19 years old • Studies that analyzed participants in the age group from 5 to 19 were also included if this age group was part of a bigger study population |
• Participants with non-physical disabilities (e.g., hearing, intellectual, visual impairments) • Participants under 5 years old or over 19 years old |
| Publication Type | Peer-reviewed journal articles |
• Grey literature • Conference abstracts, books, and theses • Publications without peer review |
| Languages | English, German | • other languages than German or English |
| Publication Date | 2009 to 2022 | Before 2009 |
This review included studies that used different measurement methods to capture a variability of dimensions and aspects of PA in CAUW. Objective measurement methods provide more accurate information regarding the amount and intensity of PA performed by children and adolescents, while subjective measurement methods elicit more background information such as barriers or contributing factors on PA [36, 37].
Further, this review also included interventional and non-interventional studies. The baseline data of the interventional studies offered insights into PA behavior that helped address the objectives of the review.
To ensure the quality of the included studies, only peer-reviewed articles were included in the review. To guarantee the timeliness of the studies, articles from 2009 to 2022 were included because the United Nation Convention on the Rights of Persons with Disabilities came into force and was passed in many countries from 2009 after [38]. Since then, society has been more committed to removing barriers for people with disabilities [39], and it has become easier to participate PA.
Search strategy
On December 8, 2022, we searched the following electronic databases: PubMed, SPORTDiscus, Sports Medicine & Education Index and Web of Science. Regarding our search strategy, we used a combination of terms related to children and adolescents, PA and wheelchair: ((child* OR adolescen* OR “young people*” OR boys OR girls OR student* OR pupil* OR youth*) AND (“physical activ*” OR sport* OR “physical exercis*” OR “physical inactiv*” OR “physically active” OR “physical fitness” OR “physical condition”) AND (“wheelchair*” OR “walking independen*” OR “walking disab*” OR “walking impairment*” OR “physically restrict*” OR “physically disab*” OR “spina bifida” OR “cerebral palsy” OR “motor impair*” OR “physical impair*” OR “muscular dystrop*” OR “parapleg*” OR “quadripleg*” OR “spinal cord injur*”)).
Three filters were used according to our inclusion criteria to refine the results and obtain the final reference sample for screening. First, the publication date, followed by the publication type was filtered to include journal articles (PubMed: “journal article,” SPORTDiscus: “academic journal,” Sports Medicine & Education Index: “science articles,” and Web of Science: “article”). Third, the publication language was filtered.
Study selection
After removing all duplicates, two independent reviewers (S.S. and a trained student assistant) enacted a three-step study selection process: (1) title screening, (2) abstract screening, and (3) full-text screening. During each step, all articles that could not be conclusively excluded were kept for further screening in the next step. The researchers were blinded to each other’s decisions. Disagreements regarding final inclusion were resolved through discussions with a third researcher (A.K.R.)
In accordance with recommendations of Briscoe et al. [40] for systematic reviews, we screened the reference lists and citations of the final included articles to identify additional relevant studies. The references were imported into Endnote X9, a reference management software [41].
Data extraction
The following data were extracted from each article: authors; country; study design; sample characteristics (number of participants, age, gender); study aim/purpose; PA type; PA duration; PA context (e.g., schooldays, weekend days, experimental design, organized sports, daily pattern); and measurement method, instrument, and duration. The data were extracted by one researcher and checked by another (S.S. and a trained student assistant). Disagreements were settled by a third researcher (A.K.R.). Missing data were requested from the study investigators.
Quality assessment
Two independent reviewers (S.S. and a trained student assistant) rated the quality of the included studies using the Standard Quality Assessment Criteria for Evaluating Primary Research developed by Kmet et al. [42]. Agreement between the raters was measured using the Pearson correlation coefficient. Disagreements were resolved through discussion with a third researcher (A.K.R.).
The QualSyst scoring system by Kmet, Cook [42] assesses quantitative and qualitative research using 14 and 10 items, respectively, that address study design, participant selection methods, random allocation procedures, blinding, outcome measures, sample size, estimation of variance, confounding, reporting of results, and the evidence used to make the conclusion. Each item is scored based on the degree to which it is met (yes = 2, partial = 1, no = 0). If an item is not applicable to a particular study, it is coded with N/A and excluded from the score calculation.
The following equation is applied to estimate the total score for quantitative studies:
The maximum score that can be obtained for the 14-item evaluation of quantitative studies is 28. The maximum score that can be obtained for the 10-item evaluation of qualitative studies is 20. The risk of bias is evaluated with a summary score (range: 0–1); higher scores indicate better methodological quality.
Synthesis of the results
Since we expected the studies included in this systematic review to employ a diverse range of research characteristics (e.g., study design, intervention characteristics, contexts, measurements, participant characteristics, and outcome measures), we performed a narrative synthesis of the studies instead of using a meta-analysis to integrate and summarize the studies. Summary tables were created to describe the characteristics of the studies and visualize statistical indicators on the PA duration and type. The studies were grouped according to PA intensity, duration, type, and context and measurement method. PA patterns were analyzed for different categories, which seemed to be helpful in answering the research question.
Results
Flow chart
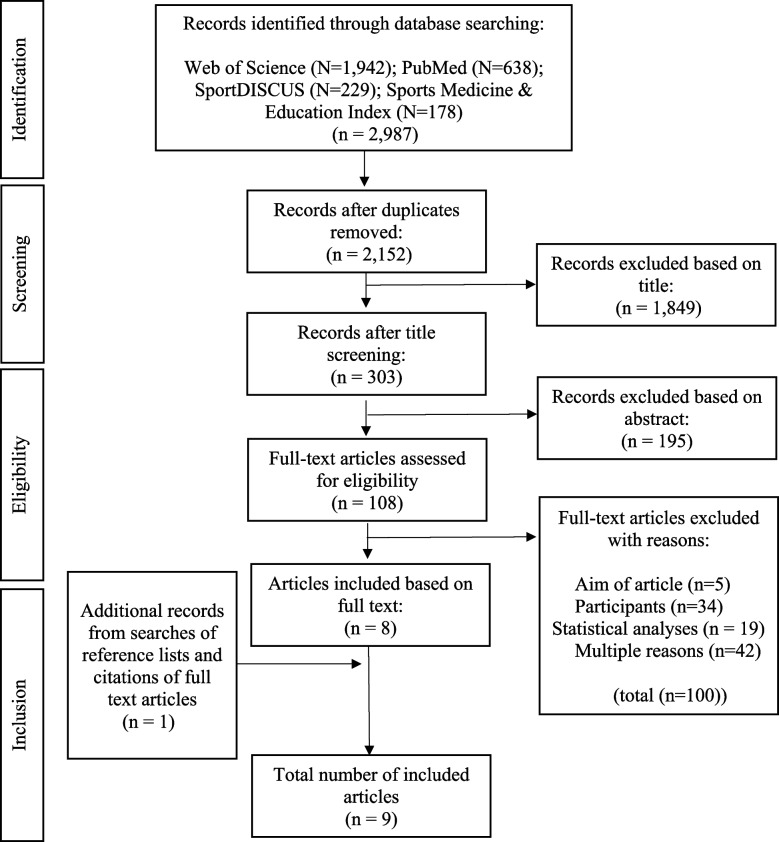
After removing 835 duplicates, title screening was performed on 2,152 potentially relevant articles. Next, abstract screening was performed on 303 articles. Then, full-text screening was performed on 108 articles, and 100 were excluded based on the study aims, statistical analysis, participants, and other reasons. The main reason for exclusion during the full-text screening was the lack of a separate analysis of CAUW. For example, the majority of studies evaluated during that step did not distinguish between wheelchairs and other walking aids.
One study was included based on snowball screening. Therefore, nine articles were included in this systematic review (Fig. 1).
Fig. 1.
Flow chart
Study characteristics
Table 2 summarizes the characteristics and results of the included studies. Key data, such as authors, country, year of publication, study design, and study aim, were extracted from each article. The sample sizes ranged from 1 [2] to 53 participants [43], with a mean of 20. One article [2] was published in 2010; the rest were published in or after 2017. The let’s ride study was reported in two articles: Bloemen et al. [43] focused on PA duration and intensity in daily life, while Bloemen et al. [19] analyzed the relationships between PA, age, and gender.
Table 2.
Overview of the study characteristics and results
| Author (year); Country | Study Design | Aim | Participants | PA | Measurement | Original results presented in article | |||
|---|---|---|---|---|---|---|---|---|---|
| N; Age (years; M±SD); gender | Indicator | Units; Context | Results* | Type; Instrument | total duration of wear time in h | ||||
| Bloemen et al. (2019); Netherlands [19] |
Observational Let's ride study |
1. To describe time spent sedentary and physically active of wheelchair-using youth with SB and compare this with typically developing peers; 2. To describe the intensity of daily PA and the compliance to guidelines of PA; 3. To describe the intensity of different types of activities during daily life. |
32; 13.7 (3.2); 20 boys, 14 girls |
PA | min/ 24 hours; Schoolday | 130 | Objective; Vitamove, Actiheart | 13.2 | 9% of 13.2 hours of wear time |
| PA | min/ 24 hours; weekend | 58 | 10.9 | 4% of 10.9 hours of wear time | |||||
| Wheeling | min/ 24 hours; schoolday | 101 | Objective; Vitamove, Actiheart | 13.2 | 7% of 13.2 hours of wear time | ||||
| Wheeling | min/ 24 hours; weekend | 43 | 10.9 | 3% of 10.9 hours of wear time | |||||
| Walking | min/ 24 hours; schoolday | 0 | 13.2 | 0% of 13.2 hours of wear time | |||||
| Walking | min/ 24 hours; weekend | 0 | 10.9 | 0% of 10.9 hours of wear time | |||||
| Running | min/ 24 hours; schoolday | 0 | 13.2 | 0% of 13.2 hours of wear time | |||||
| Running | min/ 24 hours; weekend | 0 | 10.9 | 0% of 10.9 hours of wear time | |||||
| (Hand)-biking | min/ 24 hours; schoolday | 0 | 13.2 | 0% of 13.2 hours of wear time | |||||
| (Hand)-biking | min/ 24 hours; weekend | 0 | 10.9 | 0% of 10.9 hours of wear time | |||||
| Non-cycling movement | min/ 24 hours; schoolday | 0 | 13.2 | 0% of 13.2 hours of wear time | |||||
| Non-cycling movement | min/ 24 hours; weekend | 0 | 10.9 | 0% of 10.9 hours of wear time | |||||
| Very Light PA (0-30%) | min/ 24 hours; schoolday | 1088 | Objective; Vitamove, Actiheart | 12.7 | 575 min of 761 min wear time | ||||
| min/ 24 hours; weekend | 1146 | 10.5 | 500 min of 628 min wear time | ||||||
| LPA (30-40%) | min/ 24 hours; schoolday | 208 | 12.7 | 110 min of 761 min wear time | |||||
| min/ 24 hours; weekend | 128 | 10.5 | 56 min of 628 min wear time | ||||||
| MPA (40-60%) | min/ 24 hours; schoolday | 104 | 12.7 | 55 min of 761 min wear time | |||||
| min/ 24 hours; weekend | 46 | 10.5 | 20 min of 628 min wear time | ||||||
| VPA (60-90%) | min/ 24 hours; schoolday | 19 | 12.7 | 10min of 761 min wear time | |||||
| min/ 24 hours; weekend | 2 | 10.5 | 1min of 628 min wear time | ||||||
| Near to max. (>90%) | min/ 24 hours; schoolday | 0 | 12.7 | 0min of 761 min wear time | |||||
| min/ 24 hours; weekend | 0 | 10.5 | 0min of 628 min wear time | ||||||
| Very Light PA; 0-30 % | Experimental design | lying, sitting, non-cycling | Objective; Vitamove, Actiheart | n.a | n.a. | ||||
| LPA; 30-40% | Experimental design | Standing, wheeling, (hand)biking | n.a | n.a. | |||||
| MPA; 40-60% | Experimental design | Walking | n.a | n.a. | |||||
| Bloemen et al. (2020); Netherlands [43] |
Exploratory Let's ride study |
To analyse the associations between PA and VO2peak, age, sex and Hoffer classification in young wheelchair-users with SB. |
34; 13.7 (3.2); 20 boys, 14 girls |
PA | min/ 24 hours; schoolday | 128 | Objective; Vitamove | 58 | 8.9% of 2.4 days wear time |
| min/ 24 hours; weekend | 58 | 4% of 2.4 days wear time | |||||||
|
36; 13.5 (3.6); 21 boys, 15 girls |
MVPA | min/ 24 hours; schoolday | 130 | Actiheart | 65 | 9% of 2.7 days wear time | |||
| min/ 24 hours; weekend | 58 | 4% of 2.7 days wear time | |||||||
|
59; n.a.; boys |
PA | min/ 24 hours; schoolday | 115 | Vita Move, Hoffer classification | 58 | 8% of 2.4 days wear time | |||
| min/ 24 hours; weekend | 58 | 4% of 2.4 days wear time | |||||||
| Girls | PA | min/ 24 hours; schoolday | 173 | 2% of 2.4 days wear time | |||||
| min/ 24 hours; weekend | 86 | 6% of 2.4 days wear time | |||||||
|
64; n.a.; Boys |
MVPA | min/ 24 hours; schoolday | 144 | Actiheart; Hoffer classification | 65 | 10% of 2.7 days wear time | |||
| min/ 24 hours; weekend | 58 | 4% of 2.7 days wear time | |||||||
| Girls | MVPA | min/ 24 hours; schoolday | 101 | 7% of 2.7 days wear time | |||||
| min/ 24 hours; weekend | 72 | 5% of 2.7 days wear time | |||||||
|
n.a.; n.a.; n.a. |
PA | n.a.; schoolday | PA decreases with increasing age of (-0.369) | Vita Move, Spearmans rank correlation (PA & Age) | n.a. | n.a. | |||
|
n.a.; n.a.; n.a. |
n.a.; weekend | PA decreases with increasing age of (-0.286) | |||||||
|
n.a.; n.a.; n.a. |
MVPA | n.a.; schoolday | MVPA decreases with increasing age of (-0.311) | Actiheart, Spearmans rank correlation (PA & Age) | n.a. | n.a | |||
|
n.a.; n.a.; n.a. |
n.a.; weekend | MVPA decreases with increasing age of (-0.512) | |||||||
| Buffart et al. (2010); Netherlands [2] | Intervention | To present the design and procedures of the ALSP intervention. |
1; 17; Boy |
energy expanditure |
kJ/kg/day; experimental design |
43 | Subjective; Questionnaire: PASIPD | n.a. | n.a. |
| Kanagasabai et al. (2018); New Zealand [44] | Interview | To develop a deeper understanding of the leisure participation experiences of children with movement impairments to be better able to inform families, therapists and community service providers about ways to improve engagement in leisure activities of children with movement impairments for their overall development and well-being. |
9; 8.4; 7 boys, 2 girls |
Organized sports | Type of sports (amount of all participants) |
Archery (1) climbing (1) Rugby (1) |
Subjective; Interview | n.a. | n.a. |
| Lauruschkus et al. (2017); Sweden [45] | Intervention |
To explore how parents of children experience their child’s participation in physical activities and to identify facilitators and barriers for being physically active. |
25 parents of 16 children (8-11 years); n.a.; 10 male, 15 female |
PA |
n.a.; n.a. |
More passiv on school, more active at home | Subjective; Interview | n.a. | n.a. |
| Sol et al. (2019); Netherlands [46] | Mixed-method | To develop a questionnaire to assess confidence in wheelchair mobility in Dutch youth (WheelConMobility Dutch Youth). |
8; 12 (8-17); 5 boys, 3 girls |
Organized Sports | Number of participant in sport | 6 | Objective; Questionnaire | n.a. | n.a. |
| Sol et al. (2022); Netherlands [16] | Intervention | To evaluate the effects of a combination of wheelchair mobility skills training and exercise training on physical activity (PA), WMS, confidence in wheelchair mobility, and physical fitness. |
35; 12.8 (3.1); n.a. |
PA | min/ 24 hours; schoolday, weekend | 94 | Objective; Activ8 activity monitor | 8 | 6,5% of 8 hours wear time / day |
| van der Geest et al. (2020); Netherlands [47] | Cross-sectional | To evaluate the validity of home measurements of upper extremity accelerometry. |
2; n.a.; boys |
Organized Sport | min/ 24 hours; n.a. | 60 | Subjective; PA diary | 12.5 | 60min Sports at school |
| 60min Physiotherapy | |||||||||
| PA | min/ 24 hours; n.a. | 120 | Subjective; PA diary | 120min Playiing WII with friends | |||||
| Walker et al. (2020); USA [48] | Photovoice | To examine barriers and facilitators to physical activity in rural youth with CP from the perspectives of children and parents and to elicit in-depth responses. |
7 childen; (14.1 - 21); 4 boys, 3 girls |
Organized sport |
n.a.; n.a. |
Subjective; Interview | n.a. | n.a. | |
|
8 parents; n.a.; 8 female |
Organized sport | Type of sports (amount of all participants) |
Climbing (1) Basketball (1) |
n.a. | n.a. | n.a. | |||
*Note: Values are calculated based on the raw data.
PA Physical activity, LPA Light physical activity, MPA Moderate physical activity, MVPA Moderate to vigorous physical activity, n.a not applicable
Data synthesis
Table 3 presents the synthesis of the PA characteristics of the included studies. The majority of included articles presented non-interventional studies (n = 6; 67%), such as observational, mixed-method, cross-sectional and exploratory designs as well as interview studies. Two studies measured PA using objective measurement method, namely, accelerometers [16, 19, 43]. One study used objective and subjective measurement methods [2]. Four studies used the following subjective measurement methods: interviews ([44], photovoice [48], subjective questionnaires [2] and PA diaries [47]. Objective measurement methods revealed higher PA values than subjective ones. Further, age structures were equally distributed across all measurement methods.
Table 3.
Data synthesis
| Number of Articles (% of all) | Number of Participants (% of all) | Main Outcome | Authors (Year) | |||
|---|---|---|---|---|---|---|
| Type of Day | Schoolday | 3 (33.3) | 120 (66.7) | Duration in min/day: mean value (mean range) | 117 (108–132) | Bloemen et al., 2019 [19], Bloemen et al., 2020 [43]; Sol et al., 2022 [16] |
| Weekend day | 3 (33.3) | 120 (66.7) | Duration in min/day: mean value (mean range) | 71 (70–79) | Bloemen et al., 2019 [19], 2020; Sol et al., 2022 [16] | |
| PA Type/ context | Overall PA | 5 (55.5) | 147 (81.7) | Duration in min/day: mean value (mean range) | 98 (78–115) | Bloemen et al., 2019 [19], Bloemen et al., 2020 [43]; Sol et al., 2022 [16]; van der Geest et al., 2020 [47] |
| Energy expenditure | 1 (11.1) | 1 (0.6) | N/A | Buffart et al., 2010 [2] | ||
| Wheeling | 1 (11.1) | 32 (17.8) | Duration in min/day: mean value (mean range) | 72 (43 –101) | Bloemen et al., 2019 [19] | |
| Organized sports | 3 (33.3) | 32 (17.8) | Type of sports | Archery, climbing, rugby, basketbal | Kanagasabai et al., 2018 [44]; Sol et al., 2019 [46]; Walker et al., 2020 [48] | |
| PA Intensity | LPA | 1 (11.1) | 32 (17.8) | Duration in min/day: mean value (mean range median) | 168 (128–208) | Bloemen et al., 2019 [19] |
| MPA | 1 (11.1) | 32 (17.8) | Duration in min/day: mean value (mean range median) | 75 (46–104) | Bloemen et al., 2019 [19] | |
| MVPA | 1 (11.1) | 53 (29.4) | Duration in min/day: mean value (mean range median) | 94 (58–144) | Bloemen et al., 2020 [44] | |
| VPA | 1 (11.1) | 32 (17.8) | Duration in min/day: mean value (mean range median) | 11 (2–19) | Bloemen et al., 2019 [19] | |
| Near to maximum | 1 (11.1) | 32 (17.8) | Duration in min/day: mean value (mean range median) | 0 (0–0) | Bloemen et al., 2019 [19] | |
PA Physical activity, LPA Light physical activity, MPA Moderate physical activity, MVPA Moderate to vigorous physical activity, VPA Vigorous physical activity, N/A Not applicable
The nine included studies examined PA components of 180 CAUW. Regarding the PA context, [16, 19, 43] revealed that CAUW moved significantly more on schooldays (average: 117 min per day) than on weekend days (average: 70 min per day) [19, 43]. examined PA based on the following intensity levels: very light PA: 0–30%, light PA (LPA): 30–40%, moderate PA (MPA): 40–60%, vigorous PA (VPA): 60–90%, and near to maximum intensities: >90%. The findings indicated that increased PA intensity led to reduced PA duration.
Further, regarding the PA durations across all intensities CAUW revealed high PA levels with a mean of 98 min per day (range: 78–115 min per day) [16, 19, 43, 47]. Daily activities such as wheeling revealed light intensities and a mean of 72 min and a range of 43 − 101 min per day [19].
Quality assessment results
Table 4 shows the methodological quality assessment results for the quantitative studies (n = 4). The QualSyst results obtained by both raters were medium to good (mean = 0.78, SD = 0.12, range 0.73–0.95). Additionally, the Pearson correlation coefficient between the raters was high (0.872; [49].
Table 4.
QualSyst results for the quantitative studies
| Studies fulfilling the criteria n | Detailed quality assessment Yes = 2; Particular = 1; No = 0; n.a. |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| No. | Item | Yes | Partial | No | N/A | Bloemen et al. (2019) [19] | Bloemen et al. (2020) [43] | Sol et al. (2019) [46] | Sol et al. (2022) [16] |
| 1 | Question /objective is sufficiently described? | 4 | 0 | 0 | 0 | 2 | 2 | 2 | 2 |
| 2 | Study design is evident and appropriate? | 3 | 1 | 0 | 0 | 1 | 2 | 2 | 2 |
| 3 | Method of subject/comparison group selection or source of information/input variables is described and appropriate? | 4 | 0 | 0 | 0 | 2 | 2 | 2 | 2 |
| 4 | Subject (and comparison group, if applicable) characteristics are sufficiently described? | 3 | 1 | 0 | 0 | 2 | 1 | 2 | 2 |
| 5 | If interventional and random allocation was possible, was it described? | 0 | 2 | 2 | 0 | 1 | n.a. | n.a. | 1 |
| 6 | If interventional and blinding of investigators was possible, was it reported? | 0 | 2 | 0 | 2 | n.a. | n.a. | n.a. | 0 |
| 7 | If interventional and blinding of subjects was possible, was it reported? | 0 | 0 | 1 | 3 | n.a. | n.a. | 0 | 0 |
| 8 | Outcome(s) and (if applicable) exposure measure(s) is/are well defined and robust to measurement/misclassification bias? Means of assessment are reported? | 2 | 2 | 0 | 0 | 2 | 2 | 1 | 1 |
| 9 | Sample size is appropriate? | 3 | 1 | 0 | 0 | 2 | 2 | 1 | 2 |
| 10 | Analytic methods are described/justified and appropriate? | 4 | 0 | 0 | 0 | 2 | 2 | 2 | 2 |
| 11 | Some estimate of variance is reported for the main results? | 1 | 2 | 1 | 0 | 1 | 2 | 1 | 1 |
| 12 | Controlled for confounding? | 0 | 0 | 2 | 2 | 0 | 0 | ||
| 13 | Results reported in sufficient detail? | 4 | 0 | 0 | 0 | 2 | 2 | 2 | 2 |
| 14 | Conclusions supported by the results? | 2 | 2 | 0 | 0 | 1 | 2 | 1 | 2 |
| Summary score (total sum / total possible sum) | 0.75 | 0.95 | 0.73 | 0.68 | |||||
Table 5 shows the methodological quality assessment results for qualitative studies (n = 5). There was a medium pearson correlation coefficient between the raters (r = 0.553, p = 0.334; [49]. Like the quantitative studies, the QualSyst results obtained by both raters for the qualitative studies were medium to good (mean = 0.76, SD = 0.07, range = 0.65–0.85).
Table 5.
QualSyst results for the qualitative studies
| Studies fulfilling the criteria n | Detailed quality assessment Yes = 2; Particular = 1; No = 0; n.a. |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. | Item | Yes | Partial | No | Buffart et al., (2010) [2] | Kanagasabai et al., 2018 [44] | Lauruschkus et al., 2017 [45] | van der Geest et al., (2020) [47] | Walker et al., (2020) [48] | |
| 1 | Question / objective clearly described? | 5 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 2 | Design evident and appropriate to answer study question? | 4 | 1 | 0 | 2 | 2 | 2 | 1 | 2 | |
| 3 | Context for the study is clear? | 5 | 0 | 0 | 2 | 2 | 2 | 2 | 2 | |
| 4 | Connection to a theoretical framework / wider body of knowledge? | 3 | 2 | 0 | 2 | 2 | 1 | 1 | 2 | |
| 5 | Sampling strategy described, relevant and justified? | 3 | 2 | 0 | 1 | 2 | 1 | 2 | 2 | |
| 6 | Data collection methods clearly described and systematic? | 3 | 2 | 0 | 1 | 2 | 1 | 2 | 2 | |
| 7 | Data analysis clearly described, complete and systematic? | 4 | 1 | 0 | 1 | 2 | 2 | 2 | 2 | |
| 8 | Use of verification procedure(s) to establish credibility of the study? | 0 | 0 | 5 | 0 | 0 | 0 | 0 | 0 | |
| 9 | Conclusions supported by the results? | 3 | 1 | 1 | 1 | 2 | 2 | 2 | 0 | |
| 10 | Reflexivity of the account? | 2 | 3 | 0 | 1 | 1 | 2 | 1 | 2 | |
| Summary score (total sum / total possible sum) | 0.65 | 0.85 | 0.75 | 0.75 | 0.8 | |||||
Discussion
The objective of the present systematic review was to synthesize peer-reviewed studies on the PA patterns of CAUW to understand PA duration, intensity levels, types, and contexts and summarize the methods used to measure PA. Nine articles that investigated PA among CAUW were included in the review. A detailed analysis of the study characteristics, including study design; participant characteristics; PA context, duration, and type; and measurement instrument and duration, was conducted. Furthermore, various PA characteristics were summarized to provide insights into the habitual PA of CAUW.
Actuality of articles
The majority of the articles were published between 2017 and 2022 (n = 8). This observation is in line with the increase in the number of studies conducted on the broader topic of PA among children with disabilities over the last decade [50, 51]. Within society, there is a growing attention for inclusion and the dismantling of barriers for people with disabilities [52]. The number of articles could be due to the increasing importance and awareness of inclusion in society.
Number of articles
Nonetheless, the small number of articles included in this review is indicative of a pressing need for further research on PA among CAUW. Moreover, due to the small number of articles (n = 9) and the small sample sizes (rangeN = 1–53 participants), the results of the present review cannot be considered reliable [53]. Nevertheless, the review provides an overview of actual research and clearly shows that the PA values of CAUWs are insufficiently researched. Several studies included wheelchair users in samples of children and adolescents with disabilities but did not analyze their PA separately [54, 55], perhaps due to difficulties related to recruiting CAUW only. Due to the various PA-related barriers and needs of CAUW, it is necessary to report meaningful results separately for this group [27, 56].
Levels of PA
Nevertheless, some findings of the review should be discussed. For example, the review indicated that PA intensity impacts PA duration. Bloemen et al. [43] identified a mean of 94 min of MVPA per day. Four studies revealed a mean of 98 min (range: 78–115) of overall PA across all intensities per day [16, 19, 43, 45, 47]. Bloemen et al. [19] identified a mean of 72 min of habitual PA (range: 43–101), such as wheeling, per day and showed that the WHO-recommended level of 60 min of MVPA [13] was met.
Data synthesis
To compare the results of the included articles, the data were converted into minutes per day (24 h). This approach may have resulted in a methodological weakness because time factors, such as sleeping, could not be taken into account, leading to PA levels that might have been too high. To address this issue, we included the original study results in Table 1. Furthermore, the data obtained from accelerometers were estimates. Since they often do not meet the gold standard for free-living PA measurements, they should not be interpreted as accurate PA values [57].
Measurement duration
Meanwhile, most participants in Bloemen et al. [19] study took part in sports one to three times per week. If at least one of these activities was within the short measurement period of up to three days, that could explain the high PA levels and MVPA results. To avoid such issues and put snapshots of PA into perspective, Montoye, et al. [58] recommended that objective measurement periods should have an average duration of at least one week with a wear time of 10 h per day.
Measurement methods
Regarding measurement methods, the advantages, disadvantages, and methodological features of the instruments affected how they were used in the included studies. For example, Sol et al. [16], Bloemen et al. [19, 43] used accelerometers to capture PA duration and intensity, while Kanagasabi et al. [44] and Lauruschkus et al. [45] employed interviews to focus on PA type. Accelerometers more accurately capture quantitative aspects of PA, such as duration, frequency, and intensity. In contrast, interviews more accurately capture qualitative aspects of PA, such as type, and have limited validity with regard to duration and intensity [59]. Nonetheless, given the limited data available on PA among CAUW, future research should focus on the quantitative and qualitative aspects of PA. For example, a comprehensive overview of PA among CAUW could be obtained through a mixed-method approach, such as an ecological momentary assessment methodology in which accelerometers and survey methods are used simultaneously [60].
PA and health
The studies included in the present review did not offer clear findings on the relationship between PA and health. Since, as previously mentioned, children and adolescents should engage in at least a moderate level of PA to achieve health benefits [61], overall PA is not a very meaningful indicator because it does not address intensity or context. Furthermore, wheeling, which has been classified as LPA, has little effect on health [19]. Moreover, the lack of data on PA intensity and type in most of the included studies hindered the examination of the results in a health context [62].
Regarding the PA context, Sol et al. [16] and Bloemen et al. [19, 43] found higher PA levels on schooldays than on weekend days. Siegmund et al. [63, 64] found the same result in studies of children and adolescents who did not use wheelchairs. Regarding PA type, Doorley et al. [65] and Kjønniksen et al. [66] revealed that school sports and active travel to school (e.g. by bike or by walking) could increase participants’ PA levels on schooldays. Consequently, future studies should explore the promotion of PA on weekend days, such as weekend sports activities at sports clubs.
To obtain valid insights into health-related PA among CAUW, future studies should collect data from a larger number of participants over a longer time period. Therefore, the difference of PA in various weekdays should be noted to exclude snapshots of the overall PA (e.g. when CAUW have club training once a week and this is when the PA was measured). Furthermore, PA intensity should be considered in relation to PA duration and type. In addition, future research should examine whether CAUW meet PA WHO recommendations and examine the factors that affect their ability to meet the WHO recommendations.
Type of research
Qualitative studies of PA types and contexts, such as organized sports and energy expenditure, are less suitable for obtaining reliable data on PA intensity and frequency per week than objective measurement methods [44, 45, 47, 48]. For example, it was unclear whether participants engaged in organized sports more than once a week or if the data merely reflected a snapshot of a single day. Future studies should examine PA types that have not yet been considered, such as active travel. To answer the present review’s research question concerning PA among CAUW, it is necessary to identify different factors and consider PA type and duration together.
Practical implications
Existing barriers such as accessibility of built environments as well as difficult possibilities to participate in sport groups influence PA-levels of CAUW [45, 48]. Therefore, in order to increase PA-levels, it is of enormous importance to identify and reduce existing barriers. Further research should also focus on barriers and facilitators regarding PA in CAUW.
Strengths and limitations
The main strength of the present review was the inclusion of studies that objectively and subjectively measured PA, enabling the examination of a variety of PA patterns and variables (e.g., frequency, intensity, time, type). Furthermore, the systematic literature search employed several electronic databases and a comprehensive list of search strings. In addition, the reference lists of all included articles were manually checked to obtain other relevant studies. The search strategy was broad enough to identify relevant studies, including ones that did not make overall PA analysis their main objective. Unlike reviews in the broader PD research field [24, 67], the present review only included studies that exclusively focused on CAUW to clearly connect PA patterns to wheelchair use. Research on multiple impairments cannot guarantee that the observed behavior is not due to a secondary impairment.
Regarding limitations, the variety of study designs made it difficult to compare and synthesize the results of the included studies. To address this issue, the results were converted into minutes per day (24 h). However, PA levels might have been too high because time factors, such as sleeping, could not be taken into account. In addition, only nine studies with small sample sizes were included in this review due to the lack of sufficient studies in the field. The review’s findings cannot be generalized or considered representative due to this small number of studies and sample sizes.
Conclusion
This systematic review yielded inconclusive results regarding PA among CAUW. The nine included articles examined PA components related to a total of 180 CAUW. The data synthesis revealed connections between PA intensity, duration, type, and context. The classification of wheeling as an LPA can be useful for further research. There is a need for high-quality studies of PA among CAUW with larger sample sizes as well as studies of different daily PA contexts.
Based on the present review, no valid conclusions can be made. To gain a deeper understanding of the PA patterns and needs of CAUW and the barriers they face, a combination of quantitative and qualitative measures could be used to simultaneously collect valid data on PA domains, such as duration, intensity, type, and context.
Acknowledgements
Not applicable.
Authors' contributions
Conceptualization: S. Seemüller, F. Beck, A. K. Reimers; Methodology: S. Seemüller, F. Beck, A. K. Reimers; Formal analysis: S. Seemüller, F. Beck; Preparing tables and figures: S. Seemüller; Writing (original draft): S. Seemüller; Writing (reviewing and editing): S. Seemüller, F. Beck, A. K. Reimers; Supervision: A. K. Reimers.
Funding
Open Access funding enabled and organized by Projekt DEAL. We acknowledge financial support by Deutsche Forschungsgemeinschaft and Friedrich-Alexander-Universität Erlangen-Nürnberg within the funding programme "Open Access Publication Funding". This research was not supported by any grants from funding agencies in the public, commercial, or not-for-profit sectors.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Piggin J. What is physical activity? A holistic definition for teachers, researchers and policy makers. Front Sports Act Living. 2020;2:72. doi: 10.3389/fspor.2020.00072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Buffart LM, van den Berg-Emons RJ, van Mechelen W, van Meeteren J, van der Slot W, Stam HJ, et al. Promoting physical activity in an adolescent and a young adult with physical disabilities. Disabil Health J. 2010;3(2):86–92. [DOI] [PubMed]
- 3.Lee CJ, Sanders RH, Payton CJ. Changes in force production and stroke parameters of trained able-bodied and unilateral arm-amputee female swimmers during a 30 s tethered front-crawl swim. J Sports Sci. 2014;32(18):1704–11. [DOI] [PubMed]
- 4.Janssen I, LeBlanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act. 2010;7(1):40. doi: 10.1186/1479-5868-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heath GN, Fentem PH. 8 physical activity among persons with disabilities—A public health perspective. Exerc Sport Sci Rev. 1997;25(1):195–234. [PubMed] [Google Scholar]
- 6.Durstine JL, Painter P, Franklin BA, Morgan D, Pitetti KH, Roberts SO. Physical activity for the chronically Ill and disabled. Sports Med. 2000;30(3):207–219. doi: 10.2165/00007256-200030030-00005. [DOI] [PubMed] [Google Scholar]
- 7.Urbanski PK, Kim Y, Conners RT, Nadolska A, Tasiemski T. Life satisfaction in persons with spinal cord injury across the seasons. Spinal Cord. 2021;59(2):193–200. doi: 10.1038/s41393-020-0532-5. [DOI] [PubMed] [Google Scholar]
- 8.Martin JJ. Benefits and barriers to physical activity for individuals with disabilities: a social-relational model of disability perspective. Disabil Rehabil. 2013;35(24):2030–2037. doi: 10.3109/09638288.2013.802377. [DOI] [PubMed] [Google Scholar]
- 9.Warburton DE, Nicol CW, Bredin SSJC. Health benefits of physical activity: the evidence. Can Med Assoc J. 2006;174(6):801–809. doi: 10.1503/cmaj.051351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zick CD, Smith KR, Brown BB, Fan JX, Kowaleski-Jones L. Physical activity during the transition from adolescence to adulthood. J Phys Act Health. 2007;4(2):125–137. doi: 10.1123/jpah.4.2.125. [DOI] [PubMed] [Google Scholar]
- 11.WHO. International Classification of Functioning, disability, and Health: Children & Youth Version: ICF-CY: World Health Organization; 2007.
- 12.Aubert S, Barnes JD, Demchenko I, Hawthorne M, Abdeta C, Abi Nader P, et al. Global matrix 4.0 physical activity report card grades for children and adolescents: results and analyses from 57 countries. J Phys Act Health. 2022;19(11):700–28. [DOI] [PubMed]
- 13.Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451. doi: 10.1136/bjsports-2020-102955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carty C, van der Ploeg HP, Biddle SJH, Bull F, Willumsen J, Lee L, et al. The first global physical activity and sedentary behavior guidelines for people living with disability. J Phys Act Health. 2021;18(1):86–93. doi: 10.1123/jpah.2020-0629. [DOI] [PubMed] [Google Scholar]
- 15.Choi JY, Rha D-w, Park ES. Change in pulmonary function after incentive spirometer exercise in children with spastic cerebral palsy: a randomized controlled study. Yonsei Med J. 2016;57(3):769–75. [DOI] [PMC free article] [PubMed]
- 16.Sol ME, Verschuren O, Horemans H, Westers P, Visser-Meily JMA, De Groot JF. The effects of wheelchair mobility skills and exercise training on physical activity, fitness, skills and confidence in youth using a manual wheelchair. Disabil Rehabil. 2022;44(16):4398–4407. doi: 10.1080/09638288.2021.1907456. [DOI] [PubMed] [Google Scholar]
- 17.Carbone PS, Smith PJ, Lewis C, LeBlanc C. Promoting the participation of children and adolescents with disabilities in sports, recreation, and physical activity. Pediatrics. 2021;148(6):e2021054664. doi: 10.1542/peds.2021-054664. [DOI] [PubMed] [Google Scholar]
- 18.Rimmer JA, Rowland JL. Physical activity for youth with disabilities: a critical need in an underserved population. Dev Neurorehabi. 2008;11(2):141. doi: 10.1080/17518420701688649. [DOI] [PubMed] [Google Scholar]
- 19.Bloemen MAT, van den Berg-Emons RJG, Tuijt M, Nooijen CFJ, Takken T, Backx FJG, et al. Physical activity in wheelchair-using youth with spina bifida: an observational study. J Neuroeng Rehabil. 2019;16:9. doi: 10.1186/s12984-018-0464-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sit C, Aubert S, Carty C, Silva DAS, López-Gil JF, Asunta P, et al. Promoting physical activity among children and adolescents with disabilities: the translation of policy to practice internationally. J Phys Act Health. 2022;19(11):758–768. doi: 10.1123/jpah.2022-0351. [DOI] [PubMed] [Google Scholar]
- 21.Maher CA, Williams MT, Olds T, Lane AE. Physical and sedentary activity in adolescents with cerebral palsy. Dev Med Child Neurol. 2007;49(6):450–457. doi: 10.1111/j.1469-8749.2007.00450.x. [DOI] [PubMed] [Google Scholar]
- 22.Schoenmakers M, de Groot J, Gorter JW, Hillaert J, Helders P, Takken T. Muscle strength, aerobic capacity and physical activity in independent ambulating children with lumbosacral spina bifida. Disabil Rehabil. 2009;31(4):259–266. doi: 10.1080/09638280801923235. [DOI] [PubMed] [Google Scholar]
- 23.Antonak F, Livneh R. Measurement of attitudes towards persons with disabilities. Disabil Rehabil. 2000;22(5):211–224. doi: 10.1080/096382800296782. [DOI] [PubMed] [Google Scholar]
- 24.Bloemen M, Van Wely L, Mollema J, Dallmeijer A, de Groot J. Evidence for increasing physical activity in children with physical disabilities: a systematic review. Dev Med Child Neurol. 2017;59(10):1004–1010. doi: 10.1111/dmcn.13422. [DOI] [PubMed] [Google Scholar]
- 25.Li R, Sit CHP, Yu JJ, Duan JZJ, Fan TCM, McKenzie TL, et al. Correlates of physical activity in children and adolescents with physical disabilities: a systematic review. Prev Med. 2016;89:184–193. doi: 10.1016/j.ypmed.2016.05.029. [DOI] [PubMed] [Google Scholar]
- 26.Shields N, Synnot AJ, Barr M. Perceived barriers and facilitators to physical activity for children with disability: a systematic review. Br J Sports Med. 2012;46(14):989–997. doi: 10.1136/bjsports-2011-090236. [DOI] [PubMed] [Google Scholar]
- 27.Dolbow DR, Figoni SF. Accommodation of wheelchair-reliant individuals by community fitness facilities. Spinal Cord. 2015;53(7):515–519. doi: 10.1038/sc.2015.26. [DOI] [PubMed] [Google Scholar]
- 28.Bare A, Vankoski SJ, Dias L, Danduran M, Boas S. Independent ambulators with high sacral myelomeningocele: the relation between walking kinematics and energy consumption. Dev Med Child Neurol. 2001;43(1):16–21. doi: 10.1017/s0012162201000032. [DOI] [PubMed] [Google Scholar]
- 29.Bloemen MA, Verschuren O, van Mechelen C, Borst HE, de Leeuw AJ, van der Hoef M, et al. Personal and environmental factors to consider when aiming to improve participation in physical activity in children with Spina Bifida: a qualitative study. BMC Neurol. 2015;15:11. doi: 10.1186/s12883-015-0265-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Verschuren O, Wiart L, Hermans D, Ketelaar M. Identification of facilitators and barriers to physical activity in children and adolescents with cerebral palsy. J Pediatr. 2012;161(3):488–494. doi: 10.1016/j.jpeds.2012.02.042. [DOI] [PubMed] [Google Scholar]
- 31.Crytzer TM, Dicianno BE, Kapoor R. Physical activity, exercise, and health-related measures of fitness in adults with spina bifida: a review of the literature. PM & R: the journal of injury, function, and rehabilitation. 2013;5(12):1051–62. [DOI] [PubMed]
- 32.Hammill H, Swanepoel M, Ellapen T, Strydom G. The health benefits and constraints of exercise therapy for wheelchair users: a clinical commentary. Afr J Disabil. 2017;6(1):1–8. doi: 10.4102/ajod.v6i0.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Carbone PS, Smith PJ, Lewis C, LeBlanc C, Children D Council. Council Sports Med F Promoting the participation of children and adolescents with disabilities in sports, recreation, and physical activity. Pediatrics. 2021;148(6):e2021054664. doi: 10.1542/peds.2021-054664. [DOI] [PubMed] [Google Scholar]
- 34.Nigg CR, Fuchs R, Gerber M, Jekauc D, Koch T, Krell-Roesch J, et al. Assessing physical activity through questionnaires – A consensus of best practices and future directions. Psychol Sport Exerc. 2020;50:101715. [DOI] [PMC free article] [PubMed]
- 35.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):89. doi: 10.1186/s13643-021-01626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Muckler FA, Seven SA. Selecting performance measures: objective versus subjective measurement. Hum Factors. 1992;34(4):441–455. doi: 10.1177/001872089203400406. [DOI] [Google Scholar]
- 37.Gupta S, Adam E, McDade TJP. Objective versus subjective measures of health: Systematic differences, determinants and biases. 2010:18.
- 38.Klemm K. Inklusion in Deutschland. 2015.
- 39.Hirschberg M. Behinderung: Neues Verständnis nach der Behindertenrechtskonvention. 2011.
- 40.Briscoe S, Bethel A, Rogers M. Conduct and reporting of citation searching in cochrane systematic reviews: a cross-sectional study. Res Synth Methods. 2020;11(2):169–180. doi: 10.1002/jrsm.1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Endnote. Analytics Clarivate. Clarivate Analytics2023.
- 42.Kmet LM, Cook LS, Lee RC. Standard quality assessment criteria for evaluating primary research papers from a variety of fields. Alberta Heritage Foundation for Medical Research (AHFMR); 2004.
- 43.Bloemen MT, de Groot T, Kruitwagen JF, Rook C, van den Berg-Emons R, Backx RJG. Determinants of physical activity in young wheelchair-user with spina bifida. J Rehabil Med. 2020;52(10):jrm00115. [DOI] [PubMed]
- 44.Kanagasabai PS, Mulligan H, Hale LA, Mirfin-Veitch B. I do like the activities which I can do … leisure participation experiences of children with movement impairments. Disabil Rehabil. 2018;40(14):1630–1638. doi: 10.1080/09638288.2017.1303093. [DOI] [PubMed] [Google Scholar]
- 45.Lauruschkus K, Nordmark E, Hallstrom I. Parents’ experiences of participation in physical activities for children with cerebral palsy - protecting and pushing towards independence. Disabil Rehabil. 2017;39(8):771–8. [DOI] [PubMed]
- 46.Sol ME, Bloemen MAT, Verschuren O, Rushton PW, Visser-Meily JMA, de Groot JF. Wheelchair Mobility Confidence Scale for Dutch youth using a manual wheelchair. Disabil Rehabil Assist Technol. 2019;15(6):684–91. 10.1080/17483107.2019.1604832. [DOI] [PubMed]
- 47.van der Geest A, Essers JMN, Bergsma A, Jansen M, de Groot IJM. Monitoring daily physical activity of upper extremity in young and adolescent boys with Duchenne muscular dystrophy: a pilot study. Muscle Nerve. 2020;61(3):293–300. doi: 10.1002/mus.26763. [DOI] [PubMed] [Google Scholar]
- 48.Walker A, Colquitt G, Elliot S, Emter M, Li L. Using participatory action research to examine barriers and facilitators to physical activity among rural adolescents with cerebral palsy. Disabil Rehabil. 2020;42(26):3838–3849. doi: 10.1080/09638288.2019.1611952. [DOI] [PubMed] [Google Scholar]
- 49.Hootman JM, Driban JB, Sitler MR, Harris KP, Cattano NM. Reliability and validity of three quality rating instruments for systematic reviews of observational studies. Res Synth Methods. 2011;2(2):110–118. doi: 10.1002/jrsm.41. [DOI] [PubMed] [Google Scholar]
- 50.Ku B, Rhodes RE. Physical activity behaviors in parents of children with disabilities: a systematic review. Res Dev Disabil. 2020;107:103787. doi: 10.1016/j.ridd.2020.103787. [DOI] [PubMed] [Google Scholar]
- 51.Ginis KAM, van der Ploeg HP, Foster C, Lai B, McBride CB, Ng K, et al. Participation of people living with disabilities in physical activity: a global perspective. Lancet. 2021;398(10298):443–455. doi: 10.1016/S0140-6736(21)01164-8. [DOI] [PubMed] [Google Scholar]
- 52.World Health Organization. Disability inclusion in health responses to COVID-19 in the Eastern Mediterranean Region: results of a rapid assessment. 2022.
- 53.Tipton E, Hallberg K, Hedges LV, Chan W. Implications of small samples for generalization: adjustments and rules of thumb. Eval Rev. 2017;41(5):472–505. doi: 10.1177/0193841X16655665. [DOI] [PubMed] [Google Scholar]
- 54.Lavelle G, Noorkoiv M, Theis N, Korff T, Kilbride C, Baltzopoulos V, et al. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF) as a measure of physical activity (PA) in young people with cerebral palsy: a cross-sectional study. Physiotherapy. 2020;107:209–215. doi: 10.1016/j.physio.2019.08.013. [DOI] [PubMed] [Google Scholar]
- 55.Lankhorst K, Takken T, Zwinkels M, van Gaalen L, te Velde S, Backx F, et al. Sports participation, physical activity, and health-related fitness in youth with chronic diseases or physical disabilities: the health in adapted youth sports study. J Streng Cond Res. 2021;35(8):2327–2337. doi: 10.1519/JSC.0000000000003098. [DOI] [PubMed] [Google Scholar]
- 56.Turk MA, McDermott S. The COVID-19 pandemic and people with disability. Disabil Health J. 2020;13(3):100944. [DOI] [PMC free article] [PubMed]
- 57.Burchartz A, Oriwol D, Kolb S, Schmidt SCE, Wunsch K, Manz K, et al. Comparison of self-reported & device-based, measured physical activity among children in Germany. BMC Public Health. 2021;21(1):1081. doi: 10.1186/s12889-021-11114-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Montoye AHK, Moore RW, Bowles HR, Korycinski R, Pfeiffer KA. Reporting accelerometer methods in physical activity intervention studies: a systematic review and recommendations for authors. J Sports Med. 2018;52(23):1507. doi: 10.1136/bjsports-2015-095947. [DOI] [PubMed] [Google Scholar]
- 59.Pawlowski CS, Andersen HB, Troelsen J, Schipperijn J. Children’s physical activity behavior during school recess: a pilot study using GPS, accelerometer, participant observation, and go-along interview. PLoS One. 2016;11(2):e0148786. doi: 10.1371/journal.pone.0148786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Schmidt MD, Freedson PS, Chasan-Taber L. Estimating physical activity using the CSA accelerometer and a physical activity log. Med Sci Sports Exerc. 2003;35(9):1605–1611. doi: 10.1249/01.MSS.0000084421.97661.17. [DOI] [PubMed] [Google Scholar]
- 61.Miko HC, Zillmann N, Ring-Dimitriou S, Dorner TE, Titze S, Bauer RJDG. Auswirkungen von Bewegung auf die Gesundheit. 2020;82(S 03):S184–95. [DOI] [PMC free article] [PubMed]
- 62.Eime RM, Young JA, Harvey JT, Charity MJ, Payne WR. A systematic review of the psychological and social benefits of participation in sport for children and adolescents: informing development of a conceptual model of health through sport. Int J Behav Nutr Phys Act. 2013;10(1):98. doi: 10.1186/1479-5868-10-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sigmund E, De Ste Croix M, Miklánková L, Frömel K. Physical activity patterns of kindergarten children in comparison to teenagers and young adults. Eur J Public Health. 2007;17(6):646–651. doi: 10.1093/eurpub/ckm033. [DOI] [PubMed] [Google Scholar]
- 64.Sigmund E, Sigmundová D, Ansari WE. Changes in physical activity in pre-schoolers and first-grade children: longitudinal study in the Czech Republic. Child Care Health Dev. 2009;35(3):376–382. doi: 10.1111/j.1365-2214.2009.00945.x. [DOI] [PubMed] [Google Scholar]
- 65.Doorley R, Pakrashi V, Ghosh B. Quantifying the health impacts of active travel: assessment of methodologies. Transp Rev. 2015;35(5):559–82. doi: 10.1080/01441647.2015.1037378. [DOI] [Google Scholar]
- 66.Kjønniksen L, Anderssen N, Wold B. Organized youth sport as a predictor of physical activity in adulthood. Scand J Med Sci Sports. 2009;19(5):646–654. doi: 10.1111/j.1600-0838.2008.00850.x. [DOI] [PubMed] [Google Scholar]
- 67.Bradbury M, O’Brien C, Giles N, Fenton S, Neilson S, Duda JL. Sedentary behaviour in non-ambulant children and young people with physical disabilities: a systematic search and review protocol. BMJ Open. 2021;11(12):e053077. doi: 10.1136/bmjopen-2021-053077. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.