Abstract
Background:
Increased posterior tibial slope (PTS) and decreased patellar height (PH) after medial opening wedge high tibial osteotomy (MOWHTO) have been repeatedly reported in the literature. However, this has been disputed in more recent biomechanical studies.
Hypothesis:
No change in PTS or PH would result after MOWHTO with the freehand technique, regardless of the degree of the coronal plane correction.
Study Design:
Case series.
Methods:
A total of 62 patients who underwent MOWHTO between 2018 and 2020 were included. Surgery was performed using a dedicated step-by-step protocol to reduce the risk of unintentional slope changes. All patients were evaluated preoperatively and at a 2-year follow-up with the Knee injury and Osteoarthritis Outcome Score and the University of California, Los Angeles physical activity scale. Pre- and postoperative radiographic lower limb alignment parameters—including hip-knee-ankle angle (HKA), medial proximal tibial angle (MPTA), mechanical lateral distal femoral angle, proximal posterior tibial angle (PPTA), joint line convergence angle, and joint line obliquity—were measured on full-length lower limb radiographs. PH measurements assessed on lateral and anteroposterior knee radiographs included the Caton-Deschamps, Insall-Salvati, and Schröter indices.
Results:
A significant change was observed in the coronal plane alignment, with an increase in the MPTA from 84.38° to 90.39° (P < .001) and a consequent increase in the HKA from 172.19° to 180.15° (P < .001). No significant changes were observed in the PTS, as evidenced by a postoperative PPTA of 80.6° versus a preoperative value of 80.4° (P = .2). No significant changes were detected in the mean PH on all 3 indices used—pre- versus postoperative Caton-Deschamps, Insall-Salvati, and Schröter indices measured 0.95 versus 0.93 (P = .2), 1.03 versus 1.03 (P = .5), and 1.56 versus 1.54 (P = .3), respectively.
Conclusion:
In this study, MOWHTO did not result in significant changes in the PTS or PH when accurate preoperative planning and precise intraoperative freehand technique were adopted..
Keywords: opening wedge high tibial osteotomy, patellar height, patellar height measurements, posterior tibial slope
Over the past 2 decades, high tibial osteotomy (HTO) has been revived as a successful knee preservation surgery with a high survival rate.22,26,36,47 There is a higher preference for medial opening wedge HTO (MOWHTO) over lateral closing wedge HTO (LCWHTO) because of the higher complication rate and the technical difficulties in cases of conversion to total knee replacement with LCWHTO.8,14,21,28,42,54,56,61,62 The main reported reason for challenging surgical exposure in total knee replacement after HTO is decreased patellar height (PH) secondary to patellar tendon shortening after MOWHTO.13,29,46,56,58,63 In addition, decreased PH can negatively alter patellofemoral joint biomechanics.
The primary objective of HTO is to correct the coronal plane malalignment. 64 However, multiple clinical and biomechanical studies have reported unintentional alterations in the sagittal plane7,8,15,17,33,34,37,43 as well as in the PH.2,3,8,15,17,33,34,63 An increase in the posterior tibial slope (PTS) after MOWHTO has been reported, which may be related to the geometry of the proximal tibia,16,45 larger corrections, anterior plate placement, 52 intraoperative techniques, and plate design. 49
Changes in the PTS can have significant effects on knee stability and kinematics by affecting the tibiofemoral contact pressure, tibial translation, tibial shear forces, and other articular meniscal and ligamentous structures.4,5,19,20,31,50,51,57 Biomechanical cadaveric studies have demonstrated that the PTS can be maintained by optimizing intraoperative techniques. 53 Nonetheless, no clinical studies have confirmed these findings.
In this study, we aimed to demonstrate clinically that the PTS and PH can be maintained after MOWHTO with accurate preoperative planning and meticulous intraoperative techniques, regardless of the degree of coronal plane correction.
Methods
After receiving institutional review board approval for the study protocol, we retrospectively reviewed all patients who underwent knee osteotomy for correction of varus malalignment by the same senior surgeon (M.O.) between 2018 and 2020 and who had at least 2 years of follow-up data. The inclusion criteria for the study were isolated MOWHTO, age range of 18 to 65 years, Ahlbäck osteoarthritis grade <4 for the medial tibiofemoral compartments, and no previous surgery except arthroscopic meniscus repair or meniscectomy. Excluded patients were those who had femoral osteotomies, double-level osteotomies, multiplanar osteotomies, MOWHTO with planned sagittal plane correction, patients with associated intra-articular procedures, and patients with incomplete clinical or radiological information. A total of 301 patients who had knee osteotomies were reviewed. Of these, 239 patients were excluded, and 62 patients included in our study (Figure 1).
Figure 1.
Flowchart of patients’ exclusion and inclusion criteria. ACLR, anterior cruciate ligament; MOWHTO, medial opening wedge high tibial osteotomy; OATS, osteoarticular transfer system.
Preoperative Planning
On the full-length lower limb radiograph, the following preoperative lower limb alignment parameters were measured: the hip-knee-ankle angle (HKA), the medial proximal tibial angle (MPTA), the mechanical lateral distal femoral angle (mLDFA), the joint line convergence angle (JLCA), and joint line obliquity (JLO). A correction to the anatomic values of the MPTA, mLDFA, and JLCA was targeted. The weightbearing line was planned to pass through a point 50% to 55% from the medial tibial plateau. The correction angle was calculated using the method of Miniaci et al 38 for tibial osteotomies.
The proximal posterior tibial angle (PPTA)—used as an indication of the PTS—was measured on a standard lateral knee radiograph as the angle between the tibial longitudinal axis and posterior inclination of the tibial plateau. As previously described,32,33,44 the circle 3-point method was used to define the longitudinal axis of the tibia. Two circles were digitally drawn in the center of the tibial diaphysis at 90 and 150 mm distal to the joint line. The perimeter of both circles reaches the anterior and posterior borders of the tibial shaft. A line connecting the centers of the 2 circles defined the longitudinal axis of the tibia (Figure 2).
Figure 2.

Measurement of the PPTA with the circle 3-point method. (A) Preoperative planning and PPTA measured at 82°. (B) Postoperative MOWHTO and PPTA measured at 81.7°. MOWHTO, medial opening wedge high tibial osteotomy; PPTA, proximal posterior tibial angle.
The preoperative PH was measured on the lateral radiographs using 2 different indices referenced to the proximal tibia—Caton-Deschamps 9 and Insall-Salvati. 25 A third PH measure was assessed on the anteroposterior knee radiographs using the Schröter index referenced to the distal femur 24 (Figure 3).
Figure 3.
Indices for patellar height measurement. (A) Caton-Deschamps index = A/B, where A is the distance from the anterior angle of the tibial plateau to the most inferior point of the patellar articular surface, and B is the length of the patellar articular surface. (B) Insall-Salvati index = A/B, where A is patellar tendon length, which is the distance from the inferior pole of the patella to its insertion on the tibia, and B is the patellar length, which is the greatest pole-to-pole length. (C) Schröter index = A/B, where A is the distance between 2 vertical lines tangent to the femoral epicondyles, and B is the distance between the 2 horizontally orientated lines—1 at the base of the patella and the tangent at the femoral condyles.
Surgical Technique
The senior surgeon performs >50 osteotomies per year. Most of the patients underwent diagnostic knee arthroscopy before osteotomy to assess the condition of the articular surface and meniscus, followed by debridement or repair if needed. The surgical technique followed the double window step-by-step strategy described by Kley et al 30 A: medial approach to the proximal tibia was performed. Exposure for biplane supra-tubercle osteotomy was planned. A double soft tissue window was created sparing the posterior oblique ligament (POL)—1 window to allow posterior retraction of the pes anserinus and the second for insertion of the periosteal elevator to dissect the soft tissues of the posterior tibial cortex, which was later replaced by the posterior tissue retractor. Under fluoroscopic control, the osteotomy (biplanar) cuts were performed, making sure that the horizontal cut was superior to the tibiofibular joint level and the sagittal cut was directed cranially. Then, a metal ruler or chisel confirmed the complete osteotomy of the posterior tibial cortex by palpating it against the posterior tissue retractor.
The following intraoperative measures were adopted to maintain the tibial slope 55 :
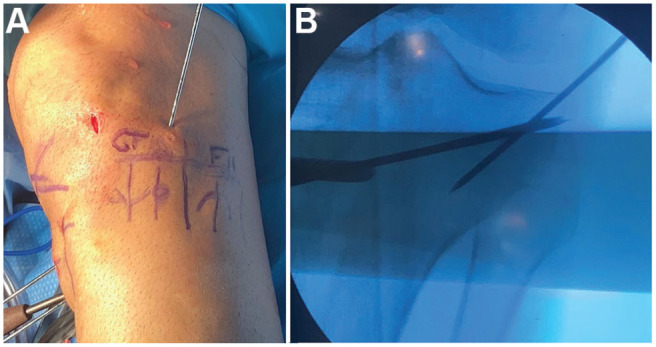
Intraoperative imaging was performed with the knee in slight flexion to align the x-ray beam with the PTS or by angling the x-ray beam to be aligned with the PTS. The view was considered satisfactory once the tibial plateau appeared as a single line on the fluoroscopy view. The osteotomy plane was defined by 2 perfectly superimposed K-wires, which indicated that the wires were parallel to the PTS (Figure 4).
An anterolateral hinge was created using a K-wire to avoid saw progression to the lateral part of the knee. This anterolateral hinge allowed posterior opening while stabilizing the anterior part of the tibia, thus preventing a high anterior-to-posterior opening that could result in increased PTS (Figure 5).
The saw blade was held parallel to the 2 wires and the PTS. The saw blade was defined as perfectly parallel to the K-wires and the PTS when it appeared by the thinnest appearance on the fluoroscopy images. Sawing was distal to the wires to avoid drifting of the cutting plane.
A complete posterolateral cortical osteotomy was performed to create a sagittally oriented hinge. This is checked after the cut with a metal ruler or a chisel, palpating the posterior tissue retractor throughout the osteotomy gap to confirm that the posterior tibial cortex has been completely osteotomized.
Using an osteotomy spreader, the osteotomy gap was opened posteriorly to avoid a high anterior-to-posterior gap ratio with the consequent increase in the PTS and decreased the PH (Figure 6).
The allograft wedge was fashioned in a triangular shape with the apex to be positioned anterior. This was to maintain lower anterior gap opening compared with posterior gap opening (Figure 6).
The wedge was inserted as posterior as possible, if possible, even posterior to the POL in the posterior protective window.
An anterior-to-posterior gap check was performed; the anterior gap should be equal or less than the posterior gap (Figure 6).
The medial collateral ligament (MCL) fibers were palpated during the opening process. If the MCL fibers were tight, pie crusting of the superficial MCL was performed.
Figure 4.
Fluoroscopy views of a right knee. (A) Lateral view showing that the x-ray beam is not parallel to the PTS. (B) Corresponding anteroposterior images showing that the tibial plateau appears as double lines and the 2 K-wires are parallel. (C) Lateral view showing the x-ray beam is parallel to the PTS. (D) Corresponding anteroposterior view showing the tibial plateau appears as a single line and 2 perfectly superimposed K-wires as an indication of being parallel to the proximal PTS. PTS, posterior tibial slope.
Figure 5.
(A) Anterolateral oblique view of a left knee with the hinge wire inserted. (B) Anteroposterior fluoroscopy view of the knee showing the hinge wire and the 2 K-wires in the osteotomy plane.
Figure 6.
Side view of the medial aspect of a left knee and upper tibia. (A) A small metallic wedge (4 mm) is used to maintain the osteotomy gap opened anteriorly. (B) An osteotomy spreader is opening the gap posteriorly, while the gap is maintained with the metallic wedge anteriorly. (C) Side view of the medial knee and upper tibia showing the allograft wedge is positioned to create a smaller gap anterior than posterior. (D and E) Osteotomy gap with the allograft wedge inserted. (D) The planned osteotomy opening at the posterior tibia (10 mm). (E) Smaller retrotubercular anterior gap (5 mm).
Postoperatively, patients were allowed a full range of motion and full weightbearing as tolerated, supported by crutches. Thromboprophylaxis by low molecular weightbearing was prescribed for 3 weeks.
Postoperative Radiographic and Clinical Assessment
Patient characteristics, operative side, Ahlbäck grade, and degree of patellofemoral degeneration were extracted from the patient database. Osteotomy precision, PTS, and PH modifications were assessed 1 year postoperatively using long-leg weightbearing radiographs with the patella centered. Preoperative and final follow-up functional scores—including Knee Injury and Osteoarthritis Outcome (KOOS) subscores (Pain, Symptoms, Activities of Daily Living, Sports and Recreation, and Quality of Living) and the University of California, Los Angeles (UCLA) physical activity score—were extracted from the patient database.
Statistical Analysis
Descriptive statistics are presented as means ± standard deviations or absolute values. Statistical analysis was performed using SPSS 12.0 (IBM). The paired Student t tests were used for all pre- and postoperative comparisons.
The mean difference (Δ) between preoperative and 1-year follow-up morphological parameters was calculated. Variables included lower limb alignment parameters (HKA, mLDFA, MPTA, JLCA, JLO, and PPTA) and PH measurement parameters (Caton Deschamps, Insall-Salvati, and Schröter indices). The absolute difference was assessed to avoid bias related to standard mean calculation (Δabsolute). Pearson correlation analysis assessed the relationship between PH measurements and the degree of coronal correction. In addition, the mean difference between preoperative and final follow-up (minimum 2-year follow-up) KOOS scores was calculated. Statistical significance for all comparisons was set at P < .05.
All radiological measurements were performed twice by 2 independent readers (M.O., C.J.) with a minimum 15-day interval between measurements. The intraclass correlation coefficient demonstrated good intraobserver (0.78) and interobserver (0.74) reproducibility.
A post hoc sample size analysis exhibited that our series allowed the comparison of lower-limb morphological parameters and PH measurements with a statistical power >90%.
Results
A total of 62 patients (n = 62 knees) were included in the study (50 men and 12 women; mean age at surgery, 42.06 ± 12.26 years). The mean follow-up time was 3 ± 2 years. The patellofemoral status was not assessed in 30 (48.39%) patients because of the unavailability of skyline view radiographs. The background characteristics of the study patients are reported in Table 1.
Table 1.
Background Characteristics and Radiographic Osteoarthritis Grades of the Patients (N = 62) a
| Variable | Value |
|---|---|
| Age, y | 42.06 ± 12.26 |
| BMI, kg/m2 | 24.66 ± 3.44 |
| Sex, male/female | 50/12 |
| Side affected, right/left | 30/32 |
| Femorotibial Ahlbäck OA grade | |
| Grade 0 | 2 |
| Grade 1 | 17 |
| Grade 2 | 24 |
| Grade 3 | 19 |
| Grade 4 | 0 |
| Patellofemoral degeneration | |
| No degeneration | 20 |
| Medial facet | 4 |
| Lateral facet | 4 |
| Both facets | 4 |
| Not assessed b | 30 |
Data are reported as mean ± SD or No. of patients. BMI, body mass index; OA, osteoarthritis.
No skyline view radiograph available.
Pre- and postoperative radiographic measurements, along with the Δ and Δabsolute values, are reported in Table 2. There were significant changes in the coronal plane alignment, with the MPTA changing from preoperative 84.38°± 4.5° to postoperative 90.39 °± 3.1° and the HKA changing from preoperative 172.19°± 3.6° to postoperative 180.15°± 2.2°(P < .0001 for both measures). Pearson correlation analysis demonstrated no association between changes in PH parameters measurements and the degree of coronal correction; hence, no subgroup analysis was performed for larger corrections.
Table 2.
Comparison of Preoperative and 1-Year Postoperative Radiographic Measurements a
| Measurement | Preoperative | 1-Year Postoperative | Δabsolute | P |
|---|---|---|---|---|
| HKA, deg | 172.19 ± 3.6 | 180.15 ± 2.2 | 7.96 ± 1.5 | <.0001 |
| mLDFA, deg | 89.1 ± 2.7 | 89.3 ± 2.6 | 0.2 ± 0.47 | |
| MPTA, deg | 84.38 ± 4.5 | 90.39 ± 3.1 | 6.04 ± 0.6 | <.0001 |
| JLCA | 1.79 ± 1.5 | 1.19 ± 1.1 | 0.5 ± 0.2 | .0156 |
| JLO | 2.93 ± 2 | 3.63 ± 4.4 | 1 ± 0.7 | .2 |
| PPTA | 80.4 ± 3.4 | 80.6 ± 3.20 | 1.4 ± 1.5 | .2 |
| Patellar height | ||||
| Caton Deschamps index | 0.95 ± 0.2 | 0.93 ± 0.2 | 0.2 ± 0.2 | .2 |
| Insall Salvati index | 1.03 ± 0.1 | 1.03 ± 0.1 | 0.1 ± 0.2 | .5 |
| Schröter Index | 1.56 ± 0.2 | 1.54 ± 0.2 | 0.2 ± 0.3 | .3 |
Data are reported as mean ± SD. Bold P values indicate a statistically significant difference between preoperative and final postoperative values (P < .05). HKA, hip-knee-ankle angle; JLCA, joint line convergence angle; JLO, joint line obliquity; mLDFA, mechanical lateral distal femoral angle; MPTA, medial proximal tibial angle; PPTA, proximal posterior tibial angle.
At the final follow-up of 24 months, significant improvements were found in all KOOS subscale values and UCLA scores (P < .0001 for all). All pre- and postoperative scores for KOOS subscales are reported in Table 3. All pre- and postoperative UCLA scores are reported in Table 4.
Table 3.
Changes in KOOS Subscale Scores From Preoperative to 2 Years Postoperative a
| KOOS Subscale | Preoperative | 2-Year Postoperative | Δ [95% CI] | P |
|---|---|---|---|---|
| Pain | 54.79 ± 12.70 | 87.93 ± 13.7 | 33.14 [29.06- 37.22] | <.0001 |
| Symptoms | 47.23 ± 14.50 | 83.02 ± 15.90 | 35.79 [31.05- 40.53] | <.0001 |
| Activities of Daily Living | 54.29 ± 15.20 | 81.30 ± 18.07 | 27.01 [21.34- 32.68] | <.0001 |
| Sports and Recreation | 38.39 ± 17.78 | 81.85 ± 18.33 | 42.63 [37.48- 47.78] | <.0001 |
| Quality of Life | 39.25 ± 14.70 | 81.69 ± 18.90 | 43.39 [36.77-50.02] | <.0001 |
KOOS, Knee injury and Osteoarthritis Outcome Score. Bold P values indicate a statistically significant difference between pre- and final postoperative values (P < .05).
Table 4.
Changes in UCLA Scores From Preoperative to 2 Years Postoperative a
| Preoperative Scores | 2-Year Postoperative Scores | ||
|---|---|---|---|
| Activity Level b | No. of Patients | Activity Level b | No. of Patients |
| 2 | 5 | 2 | 2 |
| 3 | 4 | 3 | 0 |
| 4 | 13 | 4 | 2 |
| 5 | 33 | 5 | 8 |
| 6 | 6 | 6 | 14 |
| 7 | 3 | 7 | 19 |
| 8 | 3 | 8 | 16 |
| 9 | 0 | 9 | 7 |
| 10 | 1 | 10 | 0 |
The pre- to postoperative improvements in UCLA scores were statistically significant. UCLA, University of California–Los Angeles.
Activity levels as first published by Mørup-Petersen et al 41 : 1 = Wholly inactive—dependent on others; unable to leave residence. 2 = Mostly inactive—restricted to minimum activities of daily living. 3 = Sometimes participates in mild activities—eg, walking, limited housework, and limited shopping. 4 = Regularly participates in mild activities. 5 = Sometimes participates in moderate activities—such as swimming—and can do unlimited housework or shopping. 6 = Regularly participates in moderate activities. 7 = Regularly participates in active events—eg, bicycling. 8 = Regularly participates in very active events—eg, bowling or golf. 9 = Sometimes participates in impact sports—eg, jogging, tennis, skiing, acrobatics, ballet, heavy labor, or backpacking. 10 = Regularly participates in impact sports.
Throughout the follow-up period, there was no reported osteotomy revision or total knee replacement conversion. There were 2 cases of deep venous thrombosis that were managed and 1 case of superficial infection, and all were managed with medical treatment with no need for surgical intervention.
Discussion
The most important finding in our study was that there were no significant changes in the PTS and PH after MOWHTO with the meticulous freehand technique within the range of correction applied to this cohort. The corrected Mikulicz line was projected to a point of 50% to 55% from the medial tibial plateau. A more valgus target with a correction through the Fujisawa point of 62.5% may have an impact on the outcome measures and is an important caveat to be noted.
The included patients had the purest forms of MOWHTO, which were isolated procedures in which anatomic correction was planned. We believe that the effect of MOWHTO on changes in the PTS and PH would be better depicted in these pure forms of MOWHTO than in cases requiring complex concomitant procedures and intra-articular exposure. Among the excluded patients were those who had double-level knee osteotomies, which were indicated for a substantial deformity on the femoral side (mLDFA >90° as per the 2022 consensus statement of the European Society for Sports Traumatology, Knee Surgery, and Arthroscopy 11 ). In these cases, there was no consideration of the PH.
A maintained PTS after MOWHTO was demonstrated by Ruzbarsky et al 53 in a cadaveric study through executing a proper posterolateral cortical osteotomy, creating a sagittally oriented hinge and using a trapezoidal sloped plate, posterior plate positioning, and plate fixation in knee extension to compress the anterior osteotomy gap. Similarly, Blackman et al 6 in 2015 demonstrated maintained PTS and PH after MOWHTO using a newly developed instrumentation. However, they reported coronal plane undercorrection of 10.6% of the target weightbearing line ratio. Nevertheless, maintaining the PTS and PH should not be at the expense of the planned coronal correction, which is the prime target of the HTO. The negligible correlation between the coronal correction degree and changes in the PTS or the PH was further highlighted by Ozalay et al 48 in 2008, who reported significant alteration of the mechanical axis deviation by a mean of 25.5 ± 10.9 (P < .05), with varying changes of the PTS that increased in 50% of patients, decreased in 21%, and remained unchanged in 29%. The PH was maintained, with no significant correlation between the differences (P = .368).
In 2018, Akamatsu et al 1 demonstrated that the sagittal osteotomy plane does not correlate with changes in the PTS. Whereas the ratio of the anterior to the posterior opening gap and anterior posterior hinge position ratio were significantly correlated with the change in the PTS, they concluded that the PTS should be maintained as long as surgeons achieve a trapezoidal osteotomy gap and central hinge position in the sagittal view, regardless of the sagittal osteotomy plane. However, we propose that this inclination be within a reasonable range to maintain the osteotomy plane as parallel to the PTS. More recently, Chung et al 10 in 2022 demonstrated that the osteotomy inclination angle in the sagittal plane significantly affected the PTS. They reported significant changes in the PTS after osteotomies with anteriorly and posteriorly inclined osteotomy planes (P < .001), except for the cases where the sagittal osteotomy inclination angles were 5°, 0°, and −5°. We believe that an ideal osteotomy plane typically matches the proximal tibial surface, which can be facilitated by ideal wire positioning.
The craniocaudal hinge position seems to influence the PTS as well. In a cadaveric study conducted in 2018, Jo et al 27 highlighted the significant effect of the low hinge position on increasing the PTS. With a hinge positioned 1 cm inferior to a standard hinge position, the PTS significantly increased to 11.2°± 3° versus 5.6°± 2.5° increase after a standard hinge position (P < .001), despite that the ratio of the anterior to the posterior gap opening was not significantly different. In addition, they reported significantly greater MPTA when the hinge was positioned inferior compared with the standard hinge position (95.4°± 3.5° and 88°± 3.5°, respectively; P < .001). Thus, alterations in the craniocaudal hinge position would compromise the planned coronal correction. Moreover, the too low hinge position could be due to a low cutting plane. This would create a second hinge point, that is, the proximal tibiofibular joint, which would make it almost impossible to open the osteotomy gap posteriorly, making it very challenging to control the PTS and the PH.
The importance of creating a sagittal-oriented anterolateral hinge to avoid unintentional changes in the PTS or the PH has been emphasized by several authors. In their 3-dimensional surgical simulation study in 2021, Teng et al 59 demonstrated the significant effect of the axial hinge axis on increasing the medial and lateral PTS after uniplanar OWHTO. Every 10° change of the axial hinge axis with a 10° coronal valgus correction resulted in approximately 1.6° alteration of the PTS. This was demonstrated by Moon et al 40 in a 2015 clinical study when they reported a significant increase in the PTS from 7.29°± 2.56° preoperatively to 10.48°± 3.01° postoperatively (P = .001) following MOWHTO with a posterolateral positioned hinge. Also, in a cadaveric study in 2009, Wang et al 60 demonstrated that the PTS increased from 8.71°± 0.81° to 12.16°± 0.84° (P = .031) with posterolateral hinge position compared with the maintained PTS from 9.19°±1.11° to 9.78°± 1.27° (P = .029) with lateral hinge position. A proper, complete posterolateral cortical osteotomy creates an anterolateral-oriented hinge and helps achieve the correct anterior-to-posterior gap ratio.53,59,60 In our study, a clear technique to safely execute and confirm a complete posterolateral cortical osteotomy was demonstrated.
Miura et al 39 demonstrated that the PH is unchanged or moves slightly proximal to the femur after HTO. Ihle et a 24 showed no change in the PH after MOWHTO when using a femur-referenced measurement method. Alternatively, other surgical techniques would be advocated to maintain the PH, such as distal tibial tuberosity as per Gaasbeek et al, 18 who demonstrated that distal tibial tuberosity osteotomy (TTO) with HTO was effective in avoiding patella baja when compared with proximal tuberosity osteotomy with HTO. Similarly, in 2013, Longino et al 35 demonstrated that a combined distal TTO and HTO minimizes decreased PH. However, this was contradicted by Hinterwimmer et al 23 in 2011, who reported increased PH with no significant PTS changes after both proximal and distal TTOs; despite being nonsignificant, the Caton-Deschamps index increased from 0.95 to 0.97 and from 0.89 to 0.95, respectively. More recently, Ding et al 12 demonstrated that the PH is not influenced by HTO of the distal tibial tuberosity, which neither decreased nor increased. All the aforementioned studies indicate that the change in the PH is unlikely to be a consequence of the coronal correction in MOWHTO. Thus, the unintentional sagittal plane changes (PTS) result in changes in the PH. Hence, advocating for measures to control the sagittal plane while performing MOWHTO should control for changes to the PH.
Among the techniques recommended in the literature and proven to be effective are positioning parallel pins in the sagittal plane, 23 making fixations as far posteriorly as possible, completing the osteotomy posterolaterally, 60 and ensuring that the anterior osteotomy gap is approximately half the posteromedial gap. 45 Similar philosophies have been adopted in our series.
Limitations
There are some limitations to the presented study—including presenting a small series of cases, performing small degrees of corrections, and the lack of long-term evaluation. Patellar tendon stiffness in the long term may affect PH parameter measurements.
Conclusion
In this study, MOWHTO did not result in significant changes in the PTS or PH when accurate preoperative planning and precise intraoperative freehand technique were adopted.
Footnotes
Final revision submitted June 7, 2023; accepted June 20, 2023.
One or more of the authors has declared the following potential conflict of interest or source of funding: M.O. has received consulting fees from Newclip Technics, Arthrex, and Stryker. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Comité de Protection des Personnes sud Méditerranée II (ref No. 2015-10-00148).
References
- 1. Akamatsu Y, Kobayashi H, Tsuji M, et al. Should sagittal osteotomy line be parallel to tibial posterior slope in high tibial osteotomy? BMC Musculoskelet Disord. 2018;19(1):338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Amzallag J, Pujol N, Maqdes A, et al. Patellar height modification after high tibial osteotomy by either medial opening-wedge or lateral closing-wedge osteotomies. Knee Surg Sports Traumatol Arthrosc. 2013;21(1):255-259. [DOI] [PubMed] [Google Scholar]
- 3. Backstein D, Meisami B, Gross AE. Patella baja after the modified Coventry-Maquet high tibial osteotomy. J Knee Surg. 2003;16(4):203-208. [PubMed] [Google Scholar]
- 4. Bernhardson AS, Aman ZS, DePhillipo NN, et al. Tibial slope and its effect on graft force in posterior cruciate ligament reconstructions. Am J Sports Med. 2019;47(5):1168-1174. [DOI] [PubMed] [Google Scholar]
- 5. Bernhardson AS, Aman ZS, Dornan GJ, et al. Tibial slope and its effect on force in anterior cruciate ligament grafts: anterior cruciate ligament force increases linearly as posterior tibial slope increases. Am J Sports Med. 2019;47(2):296-302. [DOI] [PubMed] [Google Scholar]
- 6. Blackman AJ, Krych AJ, Engasser WM, Levy BA, Stuart MJ. Does proximal tibial osteotomy with a novel osteotomy system obtain coronal plane correction without affecting tibial slope and patellar height? Knee Surg Sports Traumatol Arthrosc. 2015;23(12):3487-3493. [DOI] [PubMed] [Google Scholar]
- 7. Bombaci H, Canbora K, Onur G, Görgeç M. The effect of open wedge osteotomy on the posterior tibial slope. [Article in Turkish]. Acta Orthop Traumatol Turc. 2005;39(5):404-410. [PubMed] [Google Scholar]
- 8. Brouwer RW, Bierma-Zeinstra SMA, van Koeveringe AJ, Verhaar J a. N. Patellar height and the inclination of the tibial plateau after high tibial osteotomy. The open versus the closed-wedge technique. J Bone Joint Surg Br. 2005;87(9):1227-1232. [DOI] [PubMed] [Google Scholar]
- 9. Caton J, Deschamps G, Chambat P, Lerat JL, Dejour H. [Patella infera. Apropos of 128 cases]. Rev Chir Orthop Reparatrice Appar Mot. 1982;68(5):317-325. [PubMed] [Google Scholar]
- 10. Chung JH, Choi CH, Kim S-H, et al. Effect of the sagittal osteotomy inclination angle on the posterior tibial slope change in high tibial osteotomy: three-dimensional simulation study. Sci Rep. 2022;12(1):19254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dawson MJ, Ollivier M, Menetrey J, Beaufils P. Osteotomy around the painful degenerative varus knee: a 2022 ESSKA formal consensus. Knee Surg Sports Traumatol Arthrosc. 2023;31(8):3041-3043. [DOI] [PubMed] [Google Scholar]
- 12. Ding T, Tan Y, Tian X, et al. Patellar height after high tibial osteotomy of the distal tibial tuberosity: a retrospective study of age stratification. Comput Math Methods Med. 2022;2022:7193902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dohin B, Migaud H, Gougeon F, Duquennoy A. Effect of a valgization osteotomy with external wedge removal on patellar height and femoro-patellar arthritis. [Article in French]. Acta Orthop Belg. 1993;59(1):69-75. [PubMed] [Google Scholar]
- 14. Duivenvoorden T, Brouwer RW, Baan A, et al. Comparison of closing-wedge and opening-wedge high tibial osteotomy for medial compartment osteoarthritis of the knee: a randomized controlled trial with a six-year follow-up. J Bone Joint Surg Am. 2014;96(17):1425-1432. [DOI] [PubMed] [Google Scholar]
- 15. El-Azab H, Glabgly P, Paul J, Imhoff AB, Hinterwimmer S. Patellar height and posterior tibial slope after open- and closed-wedge high tibial osteotomy: a radiological study on 100 patients. Am J Sports Med. 2010;38(2):323-329. [DOI] [PubMed] [Google Scholar]
- 16. El-Azab H, Halawa A, Anetzberger H, Imhoff AB, Hinterwimmer S. The effect of closed- and open-wedge high tibial osteotomy on tibial slope: a retrospective radiological review of 120 cases. J Bone Joint Surg Br. 2008;90(9):1193-1197. [DOI] [PubMed] [Google Scholar]
- 17. Elmalı N, Esenkaya I, Can M, Karakaplan M. Monoplanar versus biplanar medial open-wedge proximal tibial osteotomy for varus gonarthrosis: a comparison of clinical and radiological outcomes. Knee Surg Sports Traumatol Arthrosc. 2013;21(12):2689-2695. [DOI] [PubMed] [Google Scholar]
- 18. Gaasbeek RDA, Sonneveld H, van Heerwaarden RJ, Jacobs WCH, Wymenga AB. Distal tuberosity osteotomy in open wedge high tibial osteotomy can prevent patella infera: a new technique. Knee. 2004;11(6):457-461. [DOI] [PubMed] [Google Scholar]
- 19. Giffin JR, Stabile KJ, Zantop T, et al. Importance of tibial slope for stability of the posterior cruciate ligament deficient knee. Am J Sports Med. 2007;35(9):1443-1449. [DOI] [PubMed] [Google Scholar]
- 20. Giffin JR, Vogrin TM, Zantop T, Woo SLY, Harner CD. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med. 2004;32(2):376-382. [DOI] [PubMed] [Google Scholar]
- 21. Haddad FS, Bentley G. Total knee arthroplasty after high tibial osteotomy: a medium-term review. J Arthroplasty. 2000;15(5):597-603. [DOI] [PubMed] [Google Scholar]
- 22. He M, Zhong X, Li Z, Shen K, Zeng W. Progress in the treatment of knee osteoarthritis with high tibial osteotomy: a systematic review. Syst Rev. 2021;10(1):56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hinterwimmer S, Beitzel K, Paul J, et al. Control of posterior tibial slope and patellar height in open-wedge valgus high tibial osteotomy. Am J Sports Med. 2011;39(4):851-856. [DOI] [PubMed] [Google Scholar]
- 24. Ihle C, Ahrend M, Grünwald L, et al. No change in patellar height following open wedge high tibial osteotomy using a novel femur-referenced measurement method. Knee. 2017;24(5):1118-1128. [DOI] [PubMed] [Google Scholar]
- 25. Insall J, Salvati E. Patella position in the normal knee joint. Radiology. 1971;101(1):101-104. [DOI] [PubMed] [Google Scholar]
- 26. Jin C, Song E-K, Santoso A, et al. Survival and risk factor analysis of medial open wedge high tibial osteotomy for unicompartment knee osteoarthritis. Arthroscopy. 2020;36(2):535-543. [DOI] [PubMed] [Google Scholar]
- 27. Jo H-S, Park J-S, Byun J-H, et al. The effects of different hinge positions on posterior tibial slope in medial open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2018;26(6):1851-1858. [DOI] [PubMed] [Google Scholar]
- 28. Kaper BP, Bourne RB, Rorabeck CH, Macdonald SJ. Patellar infera after high tibial osteotomy. J Arthroplasty. 2001;16(2):168-173. [DOI] [PubMed] [Google Scholar]
- 29. Kesmezacar H, Erginer R, Ogut T, et al. Evaluation of patellar height and measurement methods after valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2005;13(7):539-544. [DOI] [PubMed] [Google Scholar]
- 30. Kley K, Bin Abd Razak HR, Khakha RS, et al. Soft-tissue management and neurovascular protection during opening-wedge high tibial osteotomy. Arthrosc Tech. 2021;10(2):e419-e422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kolbe R, Schmidt-Hebbel A, Forkel P, et al. Steep lateral tibial slope and lateral-to-medial slope asymmetry are risk factors for concomitant posterolateral meniscus root tears in anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc. 2019;27(8):2585-2591. [DOI] [PubMed] [Google Scholar]
- 32. Krause M, Drenck TC, Korthaus A, et al. Patella height is not altered by descending medial open-wedge high tibial osteotomy (HTO) compared to ascending HTO. Knee Surg Sports Traumatol Arthrosc. 2018;26(6):1859-1866. [DOI] [PubMed] [Google Scholar]
- 33. LaPrade RF, Oro FB, Ziegler CG, Wijdicks CA, Walsh MP. Patellar height and tibial slope after opening-wedge proximal tibial osteotomy: a prospective study. Am J Sports Med. 2010;38(1):160-170. [DOI] [PubMed] [Google Scholar]
- 34. Laprade RF, Spiridonov SI, Nystrom LM, Jansson KS. Prospective outcomes of young and middle-aged adults with medial compartment osteoarthritis treated with a proximal tibial opening wedge osteotomy. Arthroscopy. 2012;28(3):354-364. [DOI] [PubMed] [Google Scholar]
- 35. Longino PD, Birmingham TB, Schultz WJ, Moyer RF, Giffin JR. Combined tibial tubercle osteotomy with medial opening wedge high tibial osteotomy minimizes changes in patellar height: a prospective cohort study with historical controls. Am J Sports Med. 2013;41(12):2849-2857. [DOI] [PubMed] [Google Scholar]
- 36. Lorbergs AL, Birmingham TB, Primeau CA, et al. Improved methods to measure outcomes after high tibial osteotomy. Clin Sports Med. 2019;38(3):317-329. [DOI] [PubMed] [Google Scholar]
- 37. Marti CB, Gautier E, Wachtl SW, Jakob RP. Accuracy of frontal and sagittal plane correction in open-wedge high tibial osteotomy. Arthroscopy. 2004;20(4):366-372. [DOI] [PubMed] [Google Scholar]
- 38. Miniaci A, Ballmer FT, Ballmer PM, Jakob RP. Proximal tibial osteotomy. A new fixation device. Clin Orthop Relat Res. 1989;(246):250-259. [PubMed] [Google Scholar]
- 39. Miura H, Kawamura H, Nagamine R, Urabe K, Iwamoto Y. Is patellar height really lower after high tibial osteotomy? Fukuoka Igaku Zasshi. 1997;88(6):261-266. [PubMed] [Google Scholar]
- 40. Moon SW, Park SH, Lee BH, et al. The effect of hinge position on posterior tibial slope in medial open-wedge high tibial osteotomy. Arthroscopy. 2015;31(6):1128-1133. [DOI] [PubMed] [Google Scholar]
- 41. Mørup-Petersen A, Skou ST, Holm CE, et al. Measurement properties of UCLA Activity Scale for hip and knee arthroplasty patients and translation and cultural adaptation into Danish. Acta Orthop. 2021;92(6):681-688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Murray R, Winkler PW, Shaikh HS, Musahl V. High tibial osteotomy for varus deformity of the knee. J Am Acad Orthop Surg Glob Res Rev. 2021;5(7):e21.00141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Naudie DDR, Amendola A, Fowler PJ. Opening wedge high tibial osteotomy for symptomatic hyperextension-varus thrust. Am J Sports Med. 2004;32(1):60-70. [DOI] [PubMed] [Google Scholar]
- 44. Nerhus TK, Ekeland A, Solberg G, et al. Radiological outcomes in a randomized trial comparing opening wedge and closing wedge techniques of high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2017;25(3):910-917. [DOI] [PubMed] [Google Scholar]
- 45. Noyes FR, Goebel SX, West J. Opening wedge tibial osteotomy: the 3-triangle method to correct axial alignment and tibial slope. Am J Sports Med. 2005;33(3):378-387. [DOI] [PubMed] [Google Scholar]
- 46. Okamoto R, Koshino T, Morii T. Shortening of patellar ligament and patella baja with improvement of quadriceps muscle strength after high tibial osteotomy. Bull Hosp Jt Dis. 1993;53(3):21-24. [PubMed] [Google Scholar]
- 47. Ollivier B, Berger P, Depuydt C, Vandenneucker H. Good long-term survival and patient-reported outcomes after high tibial osteotomy for medial compartment osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2021;29(11):3569-3584. [DOI] [PubMed] [Google Scholar]
- 48. Ozalay M, Ozkoc G, Circi E, et al. The correlation of correction magnitude and tibial slope changes following open wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. 2008;16(10):948-951. [DOI] [PubMed] [Google Scholar]
- 49. Ozel O, Yucel B, Mutlu S, Orman O, Mutlu H. Changes in posterior tibial slope angle in patients undergoing open-wedge high tibial osteotomy for varus gonarthrosis. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):314-318. [DOI] [PubMed] [Google Scholar]
- 50. Petrigliano FA, Suero EM, Voos JE, Pearle AD, Allen AA. The effect of proximal tibial slope on dynamic stability testing of the posterior cruciate ligament- and posterolateral corner-deficient knee. Am J Sports Med. 2012;40(6):1322-1328. [DOI] [PubMed] [Google Scholar]
- 51. Rodner CM, Adams DJ, Diaz-Doran V, et al. Medial opening wedge tibial osteotomy and the sagittal plane: the effect of increasing tibial slope on tibiofemoral contact pressure. Am J Sports Med. 2006;34(9):1431-1441. [DOI] [PubMed] [Google Scholar]
- 52. Rubino LJ, Schoderbek RJ, Golish SR, Baumfeld J, Miller MD. The effect of plate position and size on tibial slope in high tibial osteotomy: a cadaveric study. J Knee Surg. 2008;21(1):75-79. [DOI] [PubMed] [Google Scholar]
- 53. Ruzbarsky JJ, Arner JW, Dornan GJ, Provencher MT, Vidal AF. Tibial slope can be maintained during medial opening-wedge proximal tibial osteotomy with sagittally oriented hinge, posterior plate position, and knee hyperextension: a cadaveric study. Arthroscopy. 2021;37(7):2181-2188. [DOI] [PubMed] [Google Scholar]
- 54. Ruzbarsky JJ, Dare DM, Marx RG. Closing verses opening wedge high tibial osteotomy: an evidence-based review. HSS J. 2015;11(3):291-293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Sautet P, Kley K, Khakha R, Ollivier M. Minimally invasive double level osteotomy in severe knee varus: pearls and pitfalls. Arthrosc Tech. 2022;11(6):e1105-e1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Scuderi GR, Windsor RE, Insall JN. Observations on patellar height after proximal tibial osteotomy. J Bone Joint Surg Am. 1989;71(2):245-248. [PubMed] [Google Scholar]
- 57. Shelburne KB, Kim H-J, Sterett WI, Pandy MG. Effect of posterior tibial slope on knee biomechanics during functional activity. J Orthop Res. 2011;29(2):223-231. [DOI] [PubMed] [Google Scholar]
- 58. Staeheli JW, Cass JR, Morrey BF. Condylar total knee arthroplasty after failed proximal tibial osteotomy. J Bone Joint Surg Am. 1987;69(1):28-31. [PubMed] [Google Scholar]
- 59. Teng Y, Mizu-Uchi H, Xia Y, et al. Axial but not sagittal hinge axis affects posterior tibial slope in medial open-wedge high tibial osteotomy: a 3-dimensional surgical simulation study. Arthroscopy. 2021;37(7):2191-2201. [DOI] [PubMed] [Google Scholar]
- 60. Wang JH, Bae JH, Lim HC, et al. Medial open wedge high tibial osteotomy: the effect of the cortical hinge on posterior tibial slope. Am J Sports Med. 2009;37(12):2411-2418. [DOI] [PubMed] [Google Scholar]
- 61. Westrich GH, Peters LE, Haas SB, Buly RL, Windsor RE. Patella height after high tibial osteotomy with internal fixation and early motion. Clin Orthop Relat Res. 1998;354:169-174. [DOI] [PubMed] [Google Scholar]
- 62. Windsor RE, Insall JN, Vince KG. Technical considerations of total knee arthroplasty after proximal tibial osteotomy. J Bone Joint Surg Am. 1988;70(4):547-555. [PubMed] [Google Scholar]
- 63. Wright JM, Heavrin B, Begg M, Sakyrd G, Sterett W. Observations on patellar height following opening wedge proximal tibial osteotomy. Am J Knee Surg. 2001;14(3):163-173. [PubMed] [Google Scholar]
- 64. Wu L, Lin J, Jin Z, Cai X, Gao W. Comparison of clinical and radiological outcomes between opening-wedge and closing-wedge high tibial osteotomy: a comprehensive meta-analysis. PLoS One. 2017;12(2):e0171700. [DOI] [PMC free article] [PubMed] [Google Scholar]






