ABSTRACT
We report that carbapenem resistance developed in an extensively drug-resistant Salmonella enterica serovar Agona strain during antimicrobial therapy and in an AmpC β-lactamase-producing S. Infantis strain. Whole-genome sequence analysis indicated that carbapenem resistance in the S. Agona strain was associated with the insertion of a 160-kb IS15DI composite transposon in ompC_378, which encodes a porin consisting of 378 amino acids, along with a 397-bp deletion in the ompD. The transposon harbored 12 resistance genes including bla CTX-M-55 and an efflux pump regulatory gene, ramAp. Carbapenem resistance in the bla CMY-2-carrying S. Infantis strain was linked to the insertion of a 22,905-bp segment located 10 bp upstream of the ompC_378 coding sequence, as well as a 254-bp deletion in ompD. Our findings indicate that the loss of both ompC_378 and ompD is necessary for carbapenem resistance in extended-spectrum β-lactamase and AmpC β-lactamase-producing Salmonella strains.
IMPORTANCE
Carbapenem resistance arising from the loss of porins is commonly observed in extended-spectrum β-lactamase (ESBL) and AmpC β-lactamase-producing strains of certain Enterobacteriaceae genera, including Klebsiella pneumoniae, Escherichia coli, and Pseudomonas aeruginosa. However, this resistance mechanism is rarely reported in the Salmonella genus. To address this knowledge gap, our study offers genetic evidence demonstrating that the loss of two specific porins (OmpC_378 and OmpD) is crucial for the development of carbapenem resistance in Salmonella ESBL and AmpC β-lactamase-producing strains. Furthermore, our findings reveal that most Salmonella serovars carry seven porin parathologs, with OmpC_378 and OmpD being the key porins involved in the development of carbapenem resistance in Salmonella strains.
KEYWORDS: Salmonellosis, non-typhoidal salmonella (NTS), antimicrobial resistance, extensively drug-resistant (XDR), carbapenem resistance, whole-genome sequencing, transposon
INTRODUCTION
Salmonella is a major cause of gastroenteritis worldwide. Non-typhoidal Salmonella (NTS) was estimated to cause 93.8 million gastroenteritis globally and 155,000 deaths in 2006 (1). While NTS usually causes self-limiting gastroenteritis, invasive NTS infections often result in significant mortality rates. In 2017, NTS was estimated to cause 535,000 invasive infections and 77,500 deaths worldwide (2). Previously, chloramphenicol, amoxicillin (ampicillin), and cotrimoxazole (trimethoprim/sulfamethoxazole) were the primary drugs used to treat invasive salmonellosis. However, due to the prevalence of resistance to these first-line drugs, extended-spectrum cephalosporins (e.g., ceftriaxone) and fluoroquinolones (e.g., ciprofloxacin) have been recommended as alternative treatment options (3). Unfortunately, the extensive use of second-line antimicrobials has led to the emergence of resistance to the extended-spectrum cephalosporins and fluoroquinolones in NTS strains, posing a concerning challenge in the medical management of infections (3). Carbapenems and azithromycin are now considered a last-resort treatment option for invasive Salmonella infections caused by multidrug and extensively drug-resistant strains (3, 4).
Although carbapenem resistance remains rare in NTS, isolates displaying such resistance have been identified in humans, companion animals, livestock, wild animals, and food (5). The resistance primarily develops through the acquisition of carbapenemase genes or porin loss combined with the production of AmpC-type β-lactamase or extended-spectrum β-lactamase (ESBL) (5). While the development of carbapenem resistance during therapy has been observed in various bacterial infections (6 – 9), its occurrence in Salmonella has been rarely reported (10, 11).
In this study, we present a case of carbapenem resistance developed in S. enterica serovar Agona during therapy, as well as the resistance in an S. Infantis strain. We performed whole-genome sequence analysis to decipher the genetic characteristics and the mechanism of carbapenem resistance in the two resistant strains.
RESULTS
Genetic characteristics of S. Agona strains
Two Salmonella isolates R21.2429 and R21.2430 recovered from a patient during therapy were identified to be serovar Agona by PFGE pattern comparison (12) and in silico whole-genome sequence-based typing (SISTR). They were determined to be ST13 and harbored 14 resistance genes: aac(3)-IId, aac(6′)-Iaa, aadA22, aph(3′)-Ia, arr-2, bla CTX-M-55, bla TEM-1B, dfrA14, floR, fosA7, lnu(F), qnrS13, sul3, and tet(A), an efflux pump regulatory gene, ramAp, and T57S mutation in parC. No plasmids were found in the two isolates.
The sizes of the chromosomes in S. Agona R21.2429 and R21.2430 were determined to be 5,023,197 bp and 5,020,666 bp, respectively. Except for aac(6′)-Iaa and fosA7, the 12 other resistance genes and ramAp were found within a 140,640-bp genomic island. This genomic island was flanked by two IS15DI elements, forming an IS15DI composite transposon that was inserted in an ompC, named ompC_378, a gene encoding a porin consisting of 378 amino acids. IS15DI belongs to the IS6 family and differs from IS26 by 3 bp (13). The IS15DI composite transposon shared a large part of the sequence with a plasmid named pR18.0877_278k (GenBank accession CP037959.1). This plasmid, having IncHI2-IncHI2A replicons and a size of 278 kb, was initially identified in an XDR S. Goldcoast strain (14). pR18.0877_278k harbored 15 resistance genes and a ramAp, all located within a 160,060-bp DNA segment flanked by two IS640 elements, forming an IS640 composite transposon.
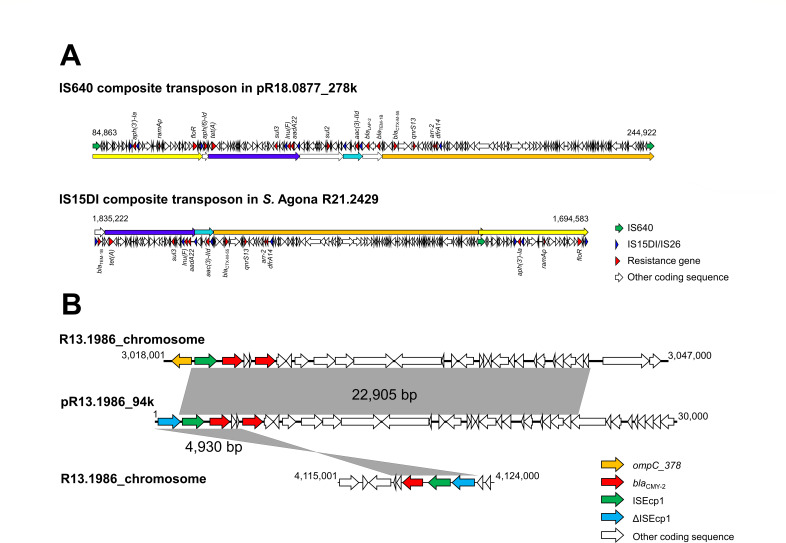
The IS15DI composite transposon found in the two S. Agona isolates exhibited significant similarity to the IS640 composite transposon (Fig. 1A). However, the IS640 composite transposon contained three DNA segments housing a total of four resistance genes (aph (6)-Id, bla TEM-1B, bla LAP-2, and sul2), which were absent in the IS15DI composite transposon. Conversely, a 3,021-bp DNA segment of the IS15DI transposon, containing bla TEM-1B, was not present in the IS640 composite transposon. Both transposons shared 12 common resistance genes and a ramAp. In terms of chromosomal variations, R21.2429 contained an additional IS640-like element (2,130 bp) and a 4-bp tandem repeat resulting from the transposition of the insertion sequence. On the other hand, R21.2430 had a 397-bp deletion in ompD.
Fig 1.
(A) Schematic map of IS640 composite transposon in plasmid pR18.0877_278k (GenBank accession no. CP037959.1) and IS15DI composite transposon in the chromosome of S. Agona R21.2429 (accession no. CP090929.1); (B) ISEcp1- bla CMY-2-harboring segments in the chromosome and plasmid pR13.1986_94k of S. Infantis strain R13.1986 (accession no. CP129384.1 and CP129386.1).
Genetic characteristics of carbapenem-resistant S. Infantis R13.1986
The S. Infantis strain was identified to be ST32. It had a chromosome size of 4,7112,862 bp and contained six plasmids: pR13.1986_108k (belonging to the IncFII incompatibility group, 108,036 bp in size), pR13.1986_94k (IncI1-I(α), 94,398 bp), pR13.1986_58k (IncL, 58,960 bp), pR13.1986_50k (IncFIC, 50,239 bp), pR13.1986_4k (Col440II, 4,779 bp), and pR13.1986_3k (ColRNAI-like, 3,205 bp). The strain carried five copies of bla CMY-2, with three copies located in the chromosome and two copies present in pR13.1986_94k. Our genomic sequence analysis identified a 22,905-bp segment that contained an ISEcp1 and two copies of bla CMY-2 and was inserted 10 bp upstream of the coding sequence of ompC_378. This 22,905 bp segment was also present in pR13.1986_94 k (Fig. 1B). In addition, another 4,930 bp segment carrying an ISEcp1, a defective ISEcp1, and a bla CMY-2, was found inserted elsewhere in the chromosome (Fig. 1B). The transposition of these bla CMY-2-carrying segments is likely mediated by ISEcp1 through a one-ended transposition process in that only a single IS element is involved (15). As a result of ISEcp1-mediated transposition, a 5-bp direct repeat was generated at the insertion sites. Furthermore, our sequence analysis also found a 254-bp deletion within ompD.
Antimicrobial susceptibility
Compared to the pan-susceptible S. Agona strain R17.4368, both XDR S. Agona strains (R21.2429 and R21.2430) showed resistance or reduced susceptibility to 14 antimicrobials, as listed in Table 1. The resistance to ampicillin, cefotaxime, ceftazidime, ceftriaxone, cefepime, chloramphenicol, gentamicin, sulfamethoxazole, trimethoprim, and tetracycline was attributed to the acquired resistance genes carried by the two strains (Table 1). The resistance to azithromycin, nalidixic acid, and tigecycline was likely contributed by ramAp through activating the expression of multidrug efflux pumps such as AcrAB-TolC (16). The resistance to ciprofloxacin was due to qnrS13 and ramAp, as Qnr genes alone typically confer only low-level resistance to fluoroquinolones in Enterobacteriaceae (17). The ciprofloxacin resistance was not linked to ParC T57S substitution, as this substitution is known not to play a role in ciprofloxacin resistance in Salmonella (18). In comparison to R17.4368, R21.2429 showed reduced susceptibility to ampicillin/sulbactam and cefoperazone/sulbactam, which could be associated with ramAp, as the β-lactamase inhibitors in these combinations could serve as substrates for multidrug efflux pumps activated by RamAp (19).
TABLE 1.
Antimicrobial susceptibility and resistance determinants in Salmonella strains
| Antimicrobial | Susceptibility (MIC, mg/L) b | Resistance in S. Agona strains linked to: | ||||
|---|---|---|---|---|---|---|
| S. Agona R17.4368 | S. Agona R21.2429 | S. Agona R21.2430 | S. Infantis R13.1986 | Resistance gene | ΔompCD c | |
| Azithromycin | S (16) | R (64) | R (64) | S (16) | ramAp | No |
| Ampicillin | S (2) | R (>64) | R (>64) | R (>64) | bla TEM-1B, bla CTX-M-55 | ND |
| Ampicillin/sulbactam a | S (≤2) | I (16) | R (>16) | R (>16) | ramAp | Yes |
| Cefoperazone/sulbactam a | S (≤8) | S (16) | R (>32) | R (>32) | ramAp | Yes |
| Cefotaxime | S (≤0.25) | R (>4) | R (>4) | R (>4) | bla CTX-M-55 | ND |
| Ceftazidime | S (0.5) | R (>8) | R (>8) | R (>8) | bla CTX-M-55 | ND |
| Ceftriaxone a | S (≤0.25) | R (>32) | R (>32) | R (>32) | bla CTX-M-55 | ND |
| Cefepime a | S (≤0.12) | R (16) | R (>16) | R (16) | bla CTX-M-55 | Yes |
| Flomoxef a | S (≤2) | S (≤2) | I (32) | R (>32) | Yes | |
| Ertapenem a | S (≤0.12) | S (≤0.12) | R (>4) | R (>4) | Yes | |
| Imipenem a | S (≤0.25) | S (≤0.25) | S (≤0.25) | R (8) | No | |
| Meropenem | S (0.06) | S (0.06) | I (2) | R (8) | Yes | |
| Colistin | S (2) | S (≤1) | S (≤1) | S (1) | No | |
| Nalidixic acid | S (8) | R (32) | R (32) | S (8) | ramAp | No |
| Ciprofloxacin | S (0.03) | R (2) | R (4) | S (0.06) | qnrS13, ramAp | Yes |
| Gentamicin | S (1) | R (>32) | R (>32) | S (1) | aac (3)-IId | ND |
| Chloramphenicol | I (16) | R (>128) | R (>128) | I (16) | floR, ramAp | ND |
| Sulfamethoxazole | S (128) | R (>1,024) | R (>1,024) | S (16) | sul3, ramAp | ND |
| Trimethoprim | S (0.5) | R (>32) | R (>32) | S (0.25) | dfrA14, ramAp | ND |
| Tetracycline | S (4) | R (>64) | R (>64) | S (4) | tet(A), ramAp | ND |
| Tigecycline | S (0.5) | R (4) | R (4) | S (0.5) | ramAp | No |
MIC was measured using the VITEK 2 system.
S, susceptible; I, intermediate; R, resistance.
ND, not determined; No, no observable effect on susceptibility; Yes, elevated resistance.
When compared to R21.2429, R21.2430 exhibited higher minimum inhibitory concentrations (MICs) for seven antimicrobials, including ampicillin/sulbactam, cefoperazone/sulbactam, cefepime, flomoxef, ertapenem, meropenem, and ciprofloxacin. Genomic sequence analysis of the two isolates revealed that R21.2430 had an additional 397 bp deletion in ompD. The defects in ompC_378 and ompD were associated with elevated MICs for the seven antimicrobials but did not significantly affect susceptibility to imipenem, colistin, nalidixic acid, and tigecycline (Table 1). Regarding the three carbapenems, the deficiency of OmpC_378 and OmpD in S. Agona R21.2430 had a greater impact on resistance to ertapenem compared to meropenem, but it had no observable effect on susceptibility to imipenem. However, in the bla CMY-2-carrying S. Infantis R13.1986, the deficiency of OmpC_378 and OmpD had a significant effect on resistance to ertapenem, meropenem, and imipenem (Table 1). In addition, S. Infantis R13.1986 displayed resistance to all β-lactam drugs and two β-lactamase inhibitor/β-lactam combinations tested, which was primarily attributed to the carriage of bla CMY-2, an AmpC β-lactamase gene.
Porins associated with carbapenem resistance
The OmpD sequence from S. Agona R21.2429 shared 56% to 100% sequence identity with seven porins in each of the strains S. Agona R21.0464, S. Infantis R21.0914, and S. Typhimurium R18.0292. These porin sequences differed from each other by 0 to 170 amino acids and were annotated to be OmpC, OmpD, OmpF, OmpS1, OmpS2, and phosphoporin PhoE (Fig. 2). Among the seven porin genes identified in each strain, three were assigned to ompC and one to ompD. Notably, ompD and an ompC, which encodes a porin of 378 amino acids (denoted as ompC_378), were all defective in the carbapenem-resistant strains S. Agona R21.2430 and S. Infantis R13.1986, as well as the previously reported S. Typhimurium S4 (10).
Fig 2.
Differences in amino acid sequences of porins found in S. Agona R21.0464 (accession no. CP093402.1), S. Infantis R21.0914 (CP121066.1), and S. Typhimurium R18.0292 (CP100739.1).
Further investigation by blasting an OmpD sequence against Salmonella genomes in the NCBI database found two distinct types or clusters of OmpD, namely OmpD_360 (consisting of 360 amino acids) and OmpD_362 (362 amino acids) (Fig. 2). The two OmpD types exhibited a distinct distribution pattern and serovar preference. Specifically, ompD_360 was identified in nearly all genomes of serovars Agona, Infantis, and Senftenberg, whereas ompD_362 was found in almost all genomes of serovars Enteritidis, Typhimurium, Newport, and Heidelberg (data not shown). However, both types were more evenly distributed in serovars Anatum and Kentucky. Notably, ompD was not identified in any S. Typhi genomes, and it was absent in approximately half of the S. Dublin and S. Reading genomes.
DISCUSSION
We present the first documented case of the emergence of carbapenem resistance during antimicrobial therapy in a S. Agona infection. In addition, we investigate the resistance mechanisms in both carbapenem-resistant strains of S. Agona and S. Infantis. The S. Infant strain is the only one observed exhibiting carbapenem resistance among 25,663 clinical Salmonella isolates recovered in Taiwan from 2004 to 2021. The development of carbapenem resistance during therapy is uncommon in Salmonella species. A previous report by Armand-Lefèvre et al. described that the emergence of imipenem resistance in an S. Wien strain during antimicrobial therapy was attributed to CMY-4 β-lactamase production and porin loss (11). Another report by Su et al. demonstrated that the development of ertapenem and imipenem resistance in an ompD-deficient S. Typhimurium strain was linked to CMY-2 β-lactamase production and subsequent loss of OmpC (10). In contrast, the emergence of carbapenem resistance during therapy is relatively common in organisms such as Klebsiella pneumoniae (20, 21), Pseudomonas aeruginosa (9, 22), Escherichia coli (6, 23), and Enterobacter spp (7). In these organisms, carbapenem resistance is primarily acquired through porin loss, but less commonly via the acquisition of carbapenemase genes (6, 9). In our study, we demonstrate that the development of ertapenem resistance in an ompC-deficient S. Agona strain is linked to the presence of an ESBL gene, bla CTX-M-55, and further loss of ompD. Furthermore, carbapenem resistance in the S. Infantis strain is associated with the presence of an AmpC gene, bla CMY-2, accompanied by the loss of ompC and ompD.
Our data indicate that the S. Agona strain lacking ompC_378 and ompD expression exhibited resistance to ertapenem and reduced susceptibility to meropenem, while its susceptibility to imipenem remained unchanged (Table 1). In contrast, imipenem resistance was found in a porin-deficient S. Wien strain and a porin-deficient S. Typhimurium strain (10, 11). These variations in carbapenem resistance profiles could potentially be attributed to the presence of different classes of β-lactamases. In a study by Jacoby et al., the susceptibility in an Omp35- and Omp36-deficient K. pneumoniae strain to seven β-lactams including ertapenem, meropenem, and imipenem was investigated with various β-lactamase genes (24). The results indicated that most porin-deficient strains carrying an AmpC β-lactamase gene exhibited higher MICs for ertapenem, imipenem, and meropenem compared to those carrying an ESBL gene. Our study further demonstrates that the resistance to ertapenem, imipenem, and meropenem in S. Infantis R13.1986 was linked to the carriage of bla CMY-2 and the deficiency of ompC and ompD. Therefore, it can be inferred that Salmonella strains with defective OmpC and OmpD, while harboring an AmpC β-lactamase gene, are likely to exhibit resistance to ertapenem, imipenem, and meropenem. Conversely, porin-deficient Salmonella strains carrying an ESBL gene are likely to be resistant only to ertapenem but not imipenem.
Many studies have highlighted the diverse impacts of outer membrane porins on antimicrobials across various bacteria. A study conducted by Tsai et al. indicates that the deletion of ompK35 (comparable to ompC in Salmonella) in K. pneumoniae did not result in a significant change in the MICs of cephazolin, cephalothin, and cefoxitin. However, the deletion of ompK36 (equivalent to ompD in Salmonella) caused an increase in MICs for these three antimicrobials, shifting them from susceptible to resistant (25). The study further revealed that the simultaneous deletion of ompK35 and ompK36 had a more significant impact on antimicrobial susceptibility, resulting in 8- and 16-fold increases in the MICs of meropenem and cefepime. Another study conducted by Choi and Lee explored the effects of single, double, and triple porin deletions in E. coli, demonstrating distinct impacts on antimicrobial susceptibility. Specifically, double deletion of ompC and ompF (equivalent to ompD in Salmonella) led to elevated MICs for all the tested β-lactams, including meropenem, but not for imipenem (26). In a study on Salmonella, Chowdhury et al. reported that single deletions of ompC, ompD, or ompF did not confer protection to Salmonella against ceftazidime and meropenem (27).
Our study findings demonstrate that the ompC-defective S. Agona strain (R21.2429) did not significantly affect the MICs of ertapenem, meropenem, and imipenem. However, the ompC_378 and ompD-defective S. Agona strain (R21.2430) exhibited elevated MICs for ertapenem and meropenem, although susceptibility to imipenem remained unchanged (Table 1). In another case, Su et al. reported that ompD deficiency in a bla CMY-2-carrying S. Typhimurium strain did not result in carbapenem resistance, but resistance emerged after the further loss of OmpC_378 in the strain. Thus, these two cases indicate that the loss of both OmpC_378 and OmpD functionality in ESBL- or AmpC β-lactamases-producing strains is required for carbapenem resistance in Salmonella. Furthermore, the carbapenem-resistant S. Infantis strain characterized in our study also exhibited deficiencies in OmpC_378 and OmpD. Nevertheless, it is noteworthy that Salmonella strains producing ESBL- or AmpC β-lactamases, along with a defective ompC or ompD, may be more prone to developing carbapenem resistance during therapy.
During our investigation of ompD sequences in three strains of S. Agona, S. Infantis, and S. Typhimurium, we identified seven porin genes in each genome, exhibiting more than 50% amino acid sequence identity among them. Among the seven genes, three are annotated as ompC. Subsequent analysis revealed that the ompC encoding 378 amino acids (referred to as ompC_378) was defective in all carbapenem-resistant strains S. Agona R21.2430, S. Infantis R13.1986, and the S. Typhimurium S4 that was previously described by Su et al. (10). Further investigation through blasting an OmpC_378 sequence with the Salmonella genomes in the NCBI database indicates that this gene is considerably conserved among Salmonella serovars (data not shown). In addition, we observed two distinct types of OmpD, with each displaying a distinct distribution pattern and serovar preference. For instance, OmpD_360 is present in almost all serovars Agona and Infantis, whereas OmpD_362 is carried in nearly all serovars Enteritidis and Typhimurium. It is worth noting that S. Typhi lacks the ompD gene. This raises the question of whether strains of this serovar can develop carbapenem resistance through the loss of other porins of the family. Further investigations are needed to explore the role of other porins in resistance to antimicrobials, particularly carbapenems.
The XDR S. Agona strains investigated in this study exhibit resistance to all clinically recommended antimicrobials for salmonellosis treatment, including ampicillin, chloramphenicol, cotrimoxazole, extended-spectrum cephalosporins (e.g., ceftriaxone), fluoroquinolones (e.g., ciprofloxacin), and azithromycin. In cases of XDR Salmonella, meropenem and azithromycin are considered the last-resort treatment option (4). However, meropenem alone may not effectively treat invasive Salmonella infections (28), particularly those caused by AmpC β-lactamase-producing Salmonella strains with porin deficiencies. In this case, we administered ceftazidime/avibactam, a novel cephalosporin/β-lactamase inhibitor combination agent, to treat the patient. It should be noted that, to the best of our knowledge, ceftazidime/avibactam is not currently established as the standard treatment for salmonellosis. Further investigations are necessary to determine the optimal therapy for XDR Salmonella infections, especially given the increasing prevalence of XDR Salmonella, such as S. Goldcoast, in Taiwan since 2018 (14). Through the analysis of whole-genome sequences of the isolates, we identified the resistance determinants in the XDR Salmonella strains. This information on resistance determinants can aid healthcare professionals in identifying additional alternative drugs that can effectively combat Salmonella strains.
In conclusion, our study reveals that defects in both OmpC_378 and OmpD are necessary for carbapenem resistance in Salmonella strains producing AmpC or ESBL β-lactamases. These findings shed light on the mechanisms underlying carbapenem resistance in Salmonella and have significant implications for surveillance and treatment strategies in combating antimicrobial resistance.
MATERIALS AND METHODS
The case with carbapenem-resistant S. Agona infection
An 83-year-old woman with type 2 diabetes mellitus was admitted to the Taichung Veterans General Hospital in Taiwan in 2020 due to fever, chills, and dyspnea. The patient had been in her usual state of health until 1 week before the admission. Upon admission, she was initially treated with empiric piperacillin/tazobactam. A stool culture revealed the presence of serogroup B Salmonella. The isolate, designated as R21.2429, was identified using MALDI-TOF (bioMérieux, Inc.) and BD Difco Salmonella antisera (BD, Inc.). Antimicrobial susceptibility testing of R21.2429 conducted using the VITEK 2 system indicated resistance to the third- and fourth-generation cephalosporins (ceftazidime, ceftriaxone, and cefepime), trimethoprim/sulfamethoxazole, and ciprofloxacin, while susceptibility to ertapenem and imipenem was observed. Consequently, the patient’s antimicrobial therapy was switched to ertapenem. However, after 7 days of ertapenem therapy, the patient continued to experience diarrhea, and a subsequent stool culture yielded Salmonella of serogroup B. An isolate, designated as R21.2430, was saved for further analysis. Notably, in addition to the resistance observed in R21.2429, R21.2430 developed resistance to ertapenem. Consequently, ceftazidime/avibactam therapy was initiated. After 12 days of treatment with ceftazidime/avibactam, the patient’s symptoms and signs resolved, leading to her discharge. A follow-up stool culture did not detect the presence of Salmonella.
S. Agona isolates
The serogroups of Salmonella isolates R21.2429 and R21.2430, recovered from the patient, as mentioned above, were determined using the Denka Seiken Agglutinating Sera Salmonella Antisera Sets (Denka Seiken, Japan). The serotypes were determined by comparing PFGE patterns with those in the Salmonella Fingerprint database of the Taiwan Centers for Disease Control (Taiwan CDC) (12), and later by whole-genome sequences using the tool SISTR (https://github.com/phac-nml/sistr_cmd) (29). A pan-susceptible S. Agona strain R17.4368 was included for the comparison of antimicrobial susceptibility. R17.4368 was recovered from a salmonellosis patient in Taiwan in 2017; it exhibited a PFGE pattern highly similar to those of R21.2429 and R21.2430 and contained only a resistance gene, fosA7, in the chromosome.
Carbapenem-resistant S. Infantis isolate
Carbapenem resistance was detected in Salmonella isolates obtained from various hospitals across Taiwan between 2004 and 2021, as part of the PulseNet Taiwan disease surveillance project. During this period, a total of 38,957 Salmonella isolates were collected, and antimicrobial susceptibility testing was performed on 25,663 isolates. From these isolates, only one, belonging to the serovar Infantis, displayed carbapenem resistance.
Antimicrobial susceptibility testing
Susceptibility testing was performed at the Taichung Veterans General Hospital using the VITEK 2 system (bioMérieux, Inc.) and at the Central Region Laboratory of Taiwan CDC using the Thermo Scientific Sensititre EUVSEC MIC panels to determine the MICs of ampicillin, azithromycin, cefotaxime, ceftazidime, chloramphenicol, ciprofloxacin, colistin, gentamicin, meropenem, nalidixic acid, sulfamethoxazole, tetracycline, tigecycline, and trimethoprim. The interpretation of MIC results primarily followed the CLSI breakpoints (30), with secondary reference to the EUCAST breakpoint tables (31), or the breakpoints recommended by the manufacturer of the testing panels.
Genetic analysis
Bacterial isolates were subjected to PFGE analysis using the PulseNet protocol (32) and whole-genome sequencing. For whole-genome sequencing, both short sequence reads and long sequence reads were generated using the Illumina Miseq System (Illumina, Inc.) and the Oxford Nanopore MinION sequencing platform (Oxford Nanopore Technologies, Inc.), respectively. The reads generated from the Illumina Miseq System were assembled using the SPAdes assembler (33). The assembled contigs were then subjected to predict the sequence types, plasmid types, antimicrobial resistance genes, and resistance-relevant mutations in housekeeping genes using the tools available on the Center for Genomic Epidemiology website (https://www.genomicepidemiology.org/). The sequence reads obtained from the Illumina Miseq System and the Oxford Nanopore MinION sequencing platform were combined and assembled using the Unicycler assembler (34) to obtain complete genomic sequences.
Identification of porins involved in carbapenem resistance
The OmpD sequence from S. Agona R21.2429 (accession number UJA67627.1) was used as a reference to search for similar porin sequences in the genomes of S. Agona R21.0464 (CP093402.1), S. Infantis R21.0914 (CP121066.1), and S. Typhimurium R18.0292 (CP100739.1) using the TBLASTN algorithm. Porin genes with a minimum amino acid sequence identity of 50% were further analyzed. Multiple porin sequence alignment was performed using the Clustal Omega tool, a distance matrix of the aligned sequences was generated using snp-dists (https://github.com/tseemann/snp-dists) to quantify the genetic differences among the porin sequences, and a dendrogram was constructed based on the calculated distances using the SciPy (https://scipy.org/) to show clustering patterns. Porins potentially involved in carbapenem resistance were identified by examining the porin genes in the carbapenem-resistant strains S. Agona R21.2430 and S. Infantis R13.1986, along with a previously reported S. Typhimurium strain (10).
ACKNOWLEDGMENTS
This study was funded by the Taichung Veterans General Hospital (grant numbers TCVGH-1113901C and TCVGH-1113901D) and the Ministry of Health and Welfare, Taiwan (grant number MOHW111-CDC-C-315-123108).
Contributor Information
Po-Yu Liu, Email: liupoyu@gmail.com.
Chien-Shun Chiou, Email: nipmcsc@cdc.gov.tw.
Matthew J. Culyba, University of Pittsburgh, Pittsburgh, Pennsylvania, USA
DATA AVAILABILITY
The complete genomic sequences of S. Agona strain R21.2429 and S. Agona strain R21.2430 were deposited in the GenBank database under the accession numbers CP090929 and CP090930, respectively. The complete sequences of the chromosome and six plasmids of S. Infantis strain R13.1986 can be accessed under the accession numbers CP129384-CP129390. The WGS reads for S. Agona R17.4368 can be found in the SRA database under the accession number SRR7458855.
REFERENCES
- 1. Majowicz SE, Musto J, Scallan E, Angulo FJ, Kirk M, O’Brien SJ, Jones TF, Fazil A, Hoekstra RMInternational Collaboration on Enteric Disease “Burden of Illness” Studies . 2010. The global burden of nontyphoidal Salmonella gastroenteritis. CLIN INFECT DIS 50:882–889. doi: 10.1086/650733 [DOI] [PubMed] [Google Scholar]
- 2. Stanaway JD, Parisi A, Sarkar K, Blacker BF, Reiner RC, Hay SI, Nixon MR, Dolecek C, James SL, Mokdad AH, Abebe G, Ahmadian E, Alahdab F, Alemnew BTT, Alipour V, Allah Bakeshei F, Animut MD, Ansari F, Arabloo J, Asfaw ET, Bagherzadeh M, Bassat Q, Belayneh YMM, Carvalho F, Daryani A, Demeke FM, Demis ABB, Dubey M, Duken EE, Dunachie SJ, Eftekhari A, Fernandes E, Fouladi Fard R, Gedefaw GA, Geta B, Gibney KB, Hasanzadeh A, Hoang CL, Kasaeian A, Khater A, Kidanemariam ZT, Lakew AM, Malekzadeh R, Melese A, Mengistu DT, Mestrovic T, Miazgowski B, Mohammad KA, Mohammadian M, Mohammadian-Hafshejani A, Nguyen CT, Nguyen LH, Nguyen SH, Nirayo YL, Olagunju AT, Olagunju TO, Pourjafar H, Qorbani M, Rabiee M, Rabiee N, Rafay A, Rezapour A, Samy AM, Sepanlou SG, Shaikh MA, Sharif M, Shigematsu M, Tessema B, Tran BX, Ullah I, Yimer EM, Zaidi Z, Murray CJL, Crump JA. 2019. The global burden of non-typhoidal Salmonella invasive disease: a systematic analysis for the Global Burden of Disease study 2017. The Lancet Infectious Diseases 19:1312–1324. doi: 10.1016/S1473-3099(19)30418-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Crump JA, Sjölund-Karlsson M, Gordon MA, Parry CM. 2015. Epidemiology, clinical presentation, laboratory diagnosis, antimicrobial resistance, and antimicrobial management of invasive Salmonella infections. Clin Microbiol Rev 28:901–937. doi: 10.1128/CMR.00002-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hughes MJ, Birhane MG, Dorough L, Reynolds JL, Caidi H, Tagg KA, Snyder CM, Yu AT, Altman SM, Boyle MM, Thomas D, Robbins AE, Waechter HA, Cody I, Mintz ED, Gutelius B, Langley G, Francois Watkins LK. 2021. Extensively drug-resistant typhoid fever in the United States. Open Forum Infect Dis 8:fab572. doi: 10.1093/ofid/ofab572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fernández J, Guerra B, Rodicio MR. 2018. Resistance to carbapenems in non-typhoidal Salmonella enterica serovars from humans, animals and food. Vet Sci 5:40. doi: 10.3390/vetsci5020040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hong T, Moland ES, Abdalhamid B, Hanson ND, Wang J, Sloan C, Fabian D, Farajallah A, Levine J, Thomson KS. 2005. Escherichia coli: development of carbapenem resistance during therapy. Clin Infect Dis 40:e84–6. doi: 10.1086/429822 [DOI] [PubMed] [Google Scholar]
- 7. Chen YG, Zhang Y, Yu YS, Qu TT, Wei ZQ, Shen P, Li LJ. 2008. . In vivo development of carbapenem resistance in clinical isolates of Enterobacter aerogenes producing multiple beta-lactamases. Int J Antimicrob Agents 32:302–307. doi: 10.1016/j.ijantimicag.2008.02.014 [DOI] [PubMed] [Google Scholar]
- 8. Elliott E, Brink AJ, van Greune J, Els Z, Woodford N, Turton J, Warner M, Livermore DM. 2006. In vivo development of ertapenem resistance in a patient with pneumonia caused by Klebsiella pneumoniae with an extended-spectrum -lactamase. Clin Infect Dis 42:e95–8. doi: 10.1086/503264 [DOI] [PubMed] [Google Scholar]
- 9. Solé M, Fàbrega A, Cobos-Trigueros N, Zamorano L, Ferrer-Navarro M, Ballesté-Delpierre C, Reustle A, Castro P, Nicolás JM, Oliver A, Martínez JA, Vila J. 2015. In vivo evolution of resistance of Pseudomonas aeruginosa strains isolated from patients admitted to an intensive care unit: mechanisms of resistance and antimicrobial exposure. J Antimicrob Chemother 70:3004–3013. doi: 10.1093/jac/dkv228 [DOI] [PubMed] [Google Scholar]
- 10. Su LH, Wu TL, Chiu CH. 2012. Development of carbapenem resistance during therapy for non-typhoid Salmonella infection. Clin Microbiol Infect 18:E91–4. doi: 10.1111/j.1469-0691.2012.03767.x [DOI] [PubMed] [Google Scholar]
- 11. Armand-Lefèvre L, Leflon-Guibout V, Bredin J, Barguellil F, Amor A, Pagès JM, Nicolas-Chanoine M-H. 2003. Imipenem resistance in Salmonella enterica serovar Wien related to porin loss and CMY-4 beta-lactamase production. Antimicrob Agents Chemother 47:1165–1168. doi: 10.1128/AAC.47.3.1165-1168.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chiou CS, Torpdahl M, Liao YS, Liao CH, Tsao CS, Liang SY, Wang YW, Kuo JC, Liu YY. 2015. Usefulness of pulsed-field gel electrophoresis profiles for the determination of Salmonella serovars. Int J Food Microbiol 214:1–3. doi: 10.1016/j.ijfoodmicro.2015.07.016 [DOI] [PubMed] [Google Scholar]
- 13. Wyrsch ER, Reid CJ, DeMaere MZ, Liu MY, Chapman TA, Roy Chowdhury P, Djordjevic SP. 2019. Complete sequences of multiple-drug resistant InCHI2 ST3 plasmids in Escherichia coli of porcine origin in Australia. Front Sustain Food Syst 3:18. doi: 10.3389/fsufs.2019.00018 [DOI] [Google Scholar]
- 14. Liao Y-S, Chen B-H, Hong Y-P, Teng R-H, Wang Y-W, Liang S-Y, Liu Y-Y, Tu Y-H, Chen Y-S, Chang J-H, Tsao C-S, Chiou C-S. 2019. Emergence of multidrug-resistant Salmonella enterica serovar goldcoast strains in Taiwan and international spread of the ST358 clone. Antimicrob Agents Chemother 63:e01122-19. doi: 10.1128/AAC.01122-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Poirel L, Lartigue MF, Decousser JW, Nordmann P. 2005. ISEcp1B-mediated transposition of blaCTX-M in Escherichia coli. Antimicrob Agents Chemother 49:447–450. doi: 10.1128/AAC.49.1.447-450.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hong Y-P, Wang Y-W, Chen B-H, Song H-Y, Chiou C-S, Chen Y-T. 2022. RamAp is an efflux pump regulator carried by an IncHI2 plasmid. Antimicrob Agents Chemother 66:e0115221. doi: 10.1128/AAC.01152-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Strahilevitz J, Jacoby GA, Hooper DC, Robicsek A. 2009. Plasmid-mediated quinolone resistance: a multifaceted threat. Clin Microbiol Rev 22:664–689. doi: 10.1128/CMR.00016-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chang M-X, Zhang J-F, Sun Y-H, Li R-S, Lin X-L, Yang L, Webber MA, Jiang H-X. 2021. Contribution of different mechanisms to ciprofloxacin resistance in Salmonella spp. Front Microbiol 12:663731. doi: 10.3389/fmicb.2021.663731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Li XZ, Zhang L, Srikumar R, Poole K. 1998. Beta-lactamase inhibitors are substrates for the multidrug efflux pumps of Pseudomonas aeruginosa. Antimicrob Agents Chemother 42:399–403. doi: 10.1128/AAC.42.2.399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cuzon G, Naas T, Guibert M, Nordmann P. 2010. In vivo selection of imipenem-resistant Klebsiella pneumoniae producing extended-spectrum beta-lactamase CTX-M-15 and plasmid-encoded DHA-1 cephalosporinase. Int J Antimicrob Agents 35:265–268. doi: 10.1016/j.ijantimicag.2009.10.021 [DOI] [PubMed] [Google Scholar]
- 21. Chia JH, Su LH, Lee MH, Kuo AJ, Shih NY, Siu LK, Wu TL. 2010. Development of high-level carbapenem resistance in Klebsiella pneumoniae among patients with prolonged hospitalization and carbapenem exposure. Microb Drug Resist 16:317–325. doi: 10.1089/mdr.2009.0048 [DOI] [PubMed] [Google Scholar]
- 22. Tsai MH, Wu TL, Su LH, Lo WL, Chen CL, Liang YH, Chiu CH. 2014. Carbapenem-resistant-only Pseudomonas aeruginosa infection in patients formerly infected by carbapenem-susceptible strains. Int J Antimicrob Agents 44:541–545. doi: 10.1016/j.ijantimicag.2014.07.022 [DOI] [PubMed] [Google Scholar]
- 23. Oteo J, Delgado-Iribarren A, Vega D, Bautista V, Rodríguez MC, Velasco M, Saavedra JM, Pérez-Vázquez M, García-Cobos S, Martínez-Martínez L, Campos J. 2008. Emergence of imipenem resistance in clinical Escherichia coli during therapy. Int J Antimicrob Agents 32:534–537. doi: 10.1016/j.ijantimicag.2008.06.012 [DOI] [PubMed] [Google Scholar]
- 24. Jacoby GA, Mills DM, Chow N. 2004. Role of beta-lactamases and porins in resistance to ertapenem and other beta-lactams in Klebsiella pneumoniae. Antimicrob Agents Chemother 48:3203–3206. doi: 10.1128/AAC.48.8.3203-3206.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tsai YK, Fung CP, Lin JC, Chen JH, Chang FY, Chen TL, Siu LK. 2011. . Klebsiella pneumoniae outer membrane porins OmpK35 and OmpK36 play roles in both antimicrobial resistance and virulence. Antimicrob Agents Chemother 55:1485–1493. doi: 10.1128/AAC.01275-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Choi U, Lee CR. 2019. Distinct roles of outer membrane porins in antibiotic resistance and membrane integrity in Escherichia coli Front Microbiol 10:953. doi: 10.3389/fmicb.2019.00953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Chowdhury AR, Mukherjee D, Singh AK, Chakravortty D. 2022. Loss of outer membrane protein A (OmpA) impairs the survival of Salmonella Typhimurium by inducing membrane damage in the presence of ceftazidime and meropenem. J Antimicrob Chemother 77:3376–3389. doi: 10.1093/jac/dkac327 [DOI] [PubMed] [Google Scholar]
- 28. Liu PY, Wang KC, Hong YP, Chen BH, Shi ZY, Chiou CS. 2021. The first imported case of extensively drug-resistant Salmonella enterica serotype typhi infection in Taiwan and the antimicrobial therapy. J Microbiol Immunol Infect 54:740–744. doi: 10.1016/j.jmii.2020.03.017 [DOI] [PubMed] [Google Scholar]
- 29. Yoshida CE, Kruczkiewicz P, Laing CR, Lingohr EJ, Gannon VPJ, Nash JHE, Taboada EN. 2016. The Salmonella in Silico typing resource (SISTR): an open web-accessible tool for rapidly typing and subtyping draft Salmonella genome assemblies. PLoS One 11:e0147101. doi: 10.1371/journal.pone.0147101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. CLSI . 2020. Performance standards for antimicrobial susceptibility testing. In CLSI supplement M100. Clinical and Laboratory Standards Institute, Wayne (PA). [Google Scholar]
- 31. European Committee on Antimicrobial Susceptibility Testing . 2021. Breakpoint tables for interpretation of mics and zone diameters version 11.0. Available from: http://wwweucastorg/clinical_breakpoints/
- 32. Ribot EM, Fair MA, Gautom R, Cameron DN, Hunter SB, Swaminathan B, Barrett TJ. 2006. Standardization of pulsed-field GEL electrophoresis protocols for the subtyping of Escherichia coli O157:H7, Salmonella, and Shigella for PulseNet. Foodborne Pathog Dis 3:59–67. doi: 10.1089/fpd.2006.3.59 [DOI] [PubMed] [Google Scholar]
- 33. Bankevich A, Nurk S, Antipov D, Gurevich AA, Dvorkin M, Kulikov AS, Lesin VM, Nikolenko SI, Pham S, Prjibelski AD, Pyshkin AV, Sirotkin AV, Vyahhi N, Tesler G, Alekseyev MA, Pevzner PA. 2012. SPAdes: a new genome assembly algorithm and its applications to single-cell sequencing. J Comput Biol 19:455–477. doi: 10.1089/cmb.2012.0021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wick RR, Judd LM, Gorrie CL, Holt KE. 2017. Unicycler: resolving bacterial genome assemblies from short and long sequencing reads. PLoS Comput Biol 13:e1005595. doi: 10.1371/journal.pcbi.1005595 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The complete genomic sequences of S. Agona strain R21.2429 and S. Agona strain R21.2430 were deposited in the GenBank database under the accession numbers CP090929 and CP090930, respectively. The complete sequences of the chromosome and six plasmids of S. Infantis strain R13.1986 can be accessed under the accession numbers CP129384-CP129390. The WGS reads for S. Agona R17.4368 can be found in the SRA database under the accession number SRR7458855.