Abstract
Objective To determine the incidence and severity of acute side effects from the use of polyvalent antivenin in victims of rattlesnake bites. Design We retrospectively reviewed the records of all patients who presented with rattlesnake bites to a university teaching hospital during an 11-year period. From patient medical records, we extracted demographic data, clinical measurements, and outcomes during emergency department evaluation and subsequent hospitalization. Data regarding serum sickness were not collected. Outcome measures Primary outcome variables were the occurrence of immediate hypersensitivity reaction to antivenin, the type of reaction, permanent disability at hospital discharge, and mortality. Results We identified a total of 73 patients with rattlesnake bites during the study period. Bite envenomation was graded as nonenvenomated, 7 patients (10%); mild, 23 patients (32%); moderate, 32 patients (44%); and severe, 11 patients (15%). We identified 65 patients who received antivenin. Antivenin doses ranged from 1 to 30 vials per patient (mean, 12.0 ± 6.0), for a total of 777 vials. In 43 patients (66%), 10 or more vials of antivenin were given. The mean number of vials of antivenin given to each snakebite grade were as follows: mild, 8.4 (±4.0); moderate, 11.8 (±5.7); and severe, 18.7 (±6.3). No deaths, amputations, or permanent disability from snakebite occurred in the patients receiving antivenin. Acute side effects of antivenin—occurring within the first 6 hours after administration—were seen in 12 patients (18%; 95% confidence interval, 10%-30%). Acute side effects consisted solely of urticaria in all but 1 patient (2%; 95% confidence interval, 0%-8%). This patient had a history of previous antivenin reaction and required a short course of intravenous epinephrine for blood pressure support. No other complications occurred. Conclusion The administration of polyvalent Crotalidae antivenin is safe. Acute hypersensitivity, when it occurs, consists solely in most cases of urticaria. Serious side effects are uncommon.
Polyvalent crotalid antivenin is currently considered the standard of care for the treatment of moderate to severe crotalid envenomation in the United States. This antivenin is a horse serum derivative containing neutralizing IgG immunoglobulin for the venom of 4 snake species: Crotalus atrox, Crotalus adamanteus, Crotalus terrificus, and Bothrops atrox. Two of these species, C atrox and C adamanteus, are North American snakes, and the other 2, C terrificus and B atrox, are South American. Because of venom similarities among species, this preparation is considered to be effective for the treatment of envenomation caused by all 15 species of rattlesnake found in North America and certain snake species indigenous to South America. Like other equine source preparations, antivenin is reported to be highly allergenic, with acute reactions reported in more than 20% of patients.1,2,3,4 The efficacy of polyvalent antivenin has been demonstrated in animal studies, but there is still controversy regarding its appropriate use in humans.5,6,7,8,9 Many authors have published antivenin dosing regimens for the treatment of crotalid envenomation.3,10,11 Nevertheless, many physicians delay giving treatment, or they give too small a dose of antivenin because of the fear of dangerous side effects.
In this study, we conducted a retrospective medical record review to investigate the incidence of acute side effects, morbidity, and mortality of all patients receiving antivenin for rattlesnake envenomation at our institution over an 11-year period.
METHODS
The medical records of all patients sustaining rattlesnake bites and evaluated at a major urban university medical center between January 1988 and December 1998 were retrospectively reviewed. Study patients were identified by a discharge diagnosis of snakebite or reptile bite. Cases of bites by obviously nonvenomous snake species were excluded. Each medical record was then reviewed by 1 of 2 independent reviewers (S R O, T S S) with the use of a structured data collection instrument. Data collected included demographic information on the victims, clinical presentation, treatment, outcome, and complications. Nursing notes as well as physicians's notes were reviewed. In cases where no mention of an adverse reaction was found in the hospital record, it was assumed that none occurred. Snakebite grades (nonenvenomated, mild, moderate, and severe) were assigned to each case by the reviewers based on prespecified clinical criteria.3,10 Nonenvenomated (dry) bites were defined by the presence of fang marks without a local or systemic reaction. Mild envenomation was defined as local swelling and pain without systemic reaction. Moderate envenomation was defined as extensive local effect with minimal systemic effects or mild local effects with marked systemic signs and symptoms. Patients with mild laboratory abnormalities were included in this category. Severe envenomation was defined as extensive local effect, systemic signs and symptoms, and marked laboratory abnormalities.10 Primary outcome variables were the occurrence of an immediate hypersensitivity reaction to antivenin, the type of reaction, permanent disability at hospital discharge, or mortality. Data regarding serum sickness was not obtained because too few patients were available for long-term follow-up to reliably identify this complication.
At the study institution, antivenin is administered aggressively for the treatment of rattlesnake envenomation. Antivenin is given immediately in the emergency department for all moderate to severe envenomations. Therapy is continued until symptoms are arrested or reversed. Surgical consultation is obtained rarely and only after antivenom therapy is felt by the clinician to be failing. Because this study was retrospective and, therefore, uncontrolled, some practice variation was inevitable. However, these basic principles were generally followed.
This study was performed with approval from the University of California Davis Medical Center investigational review board.
STATISTICAL ANALYSIS
All statistical analyses were performed using statistical software (Stata Statistical Software, version 5.0. Stata Corp, College Station, TX). Continuous variables are displayed as mean±1 SD, and 95% confidence intervals (CIs) are calculated where appropriate.
The medical records of 8 study patients were reviewed by both abstractors to test inter-rater reliability. κ values were computed to assess inter-rater agreement in the recording of multiple key data points.
RESULTS
Patient population
A total of 78 patients with discharge diagnoses of snakebite or reptile bite were identified during the study period. The medical records of 76 patients were available for review. Three records were excluded because bites were inflicted by obviously nonvenomous reptiles. These consisted of 2 boa constrictor bites and an iguana bite. Seventy-three patients were subsequently included in the study.
The northern Pacific rattlesnake (Crotalus viridis oreganus) is the only venomous snake indigenous to the area surrounding the study site. Of the snakebite cases reviewed, all except 4 occurred in wild snakes. In the 4 cases of captive snake envenomation, all were known by the victims to be rattlesnakes. Two of these snakes were described as “Pacific” rattlesnakes, and 2 were not identified in the hospital record.
Of the 73 patients identified with venomous snakebites during the study period, 59 (81%) were male, and 14 were female (19%). Ages ranged from 16 months to 68 years (mean, 21 years; median, 18 years). Thirty-three subjects were younger than 15 years, and 10 were younger than 5 years. Patients presented to the emergency department between 10 minutes and 48 hours after being bitten. Sixty-seven patients (92%) presented within 3 hours of snakebite.
Clinical characteristics
Seven patients (10%) presented with nonenvenomating (dry) bites, 23 (32%) with mild envenomation, 32 (44%) with moderate envenomations, and 11 (15%) with severe envenomations. Of the 66 patients sustaining envenomations, 64 (97%) received antivenin therapy. One patient with a dry bite also received 3 vials of antivenin, giving a total of 65 patients who received antivenin treatment. A total of 777 vials of antivenin were given to these 65 patients, ranging from 1 to 30 vials per patient (mean, 12±6). Patients with mild envenomation received 192 vials (mean, 8.4±4.0; median, 8), those with moderate envenomations received 376 vials (mean, 11.8±5.7; median, 10), and those with severe envenomations received 206 vials (mean, 18.7±6.3; median, 20) (table).
Twelve patients (18%; 95% CI, 10%-30%) had immediate reactions among patients treated with antivenin. Most reactions were mild and consisted of urticarial rash. Eight patients were treated with diphenhydramine, with or without concomitant steroids. One patient (2%; 95% CI, 0%-8%) had hypotension and required a short course of epinephrine infusion. This patient had a history of hypersensitivity to snakebite antivenin. No hypotension or other serious complication occurred in any other patient receiving antivenin. Two patients were given epinephrine infusion at the onset of urticaria, but neither had hypotension or airway compromise. Both of these patients received more antivenin after the initiation of epinephrine. Nine patients (75%) were continued on antivenin therapy after treatment for their hypersensitivity reactions.
Table 1.
Snakebites by grade and antivenom administration
| Bite grade | Patients, no. (%) | Mean (SD) vials of antivenin | Acute reaction, no. (%) |
|---|---|---|---|
| Dry | 7 (10) | 0.7 (±1.9) | 0 |
| Mild | 23 (32) | 8.4 (±4.0) | 2 (9) |
| Moderate | 32 (44) | 11.8 (±5.7) | 8 (25) |
| Severe | 11 (15) | 18.7 (±6.3) | 2 (18) |
| Total | 73 | 10.7 (±6.8) | 12 (18.5) |
Of the 12 patients who exhibited immediate hypersensitivity following intravenous antivenin administration, 6 (50%) had documented skin testing. The other 6 patients had no skin test recorded. Of the patients who underwent skin testing, 4 (67%) had no reaction, and 2 (33%) reacted but were still treated with antivenin. In total, 45 study patients had documented skin testing. Five (11%) of these patients had positive reactions to skin testing, but only 1 had antivenin therapy withheld based on a positive result.
There were no deaths, amputations, or permanent disability in the patients receiving antivenin at hospital discharge. Three patients underwent acute surgical intervention related to treatment of their snakebites. One patient developed compartment syndrome after a right ankle bite and required right leg and foot fasciotomies. This patient received 13 vials of antivenin and had recorded compartment pressures greater than 50 mm Hg before operative intervention. The second patient underwent surgical debridement of necrotic tissue from a finger wound. A third patient required surgical intervention to treat a first-aid-induced wound infection. This patient developed flexor tenosynovitis of the left hand after incision and application of aggressive mouth suction to his wound. Two additional patients had debridement of bullae at the bedside.
Agreement between reviewers
Inter-rater agreement for multiple key data points was excellent. The κ was greater than 0.75 for all comparisons (P<0.01).
DISCUSSION
Acute allergic reactions to antivenin therapy are uncommon and usually consist of urticaria. They rarely result in severe systemic symptoms. Of the 12 patients in this study who experienced acute reactions to antivenom, all but 1 consisted solely of urticaria. These reactions were easily treated with antihistamines and, in some instances, steroids. Nine of these patients continued antivenin therapy after treatment. Only 1 patient developed hypotension that required a short course of epinephrine. No permanent disability or death resulted from the use of antivenin.
Since its development and licensing in 1953, Wyeth polyvalent Crotalidae antivenin has remained the standard treatment of moderate to severe crotalid envenomation in the United States. The antivenin is a crude mixture of venom-neutralizing IgG immunoglobulin and several serum proteins derived from horses previously inoculated with venom from 4 species of pit viper. Side effects to antivenin are likely due to the horse serum derivation and are classified as type I hypersensitivity (anaphylaxis, anaphylactoid, or urticaria) or type III hypersensitivity (serum sickness).
Although the actual incidence of side effects is unknown, in 1 review of 26 patients receiving antivenin, type I hypersensitivity occurred in 6 (23%), and type III hypersensitivity occurred in 13 patients (50%). Of the 6 patients who had type I hypersensitivity, 3 (12%) developed severe systemic manifestations. This study also suggested that the incidence of serum sickness was related to dose, occurring in 5 of 6 (83%) of patients given more than 8 vials of antivenin.1 The findings of that study, together with case reports of severe reactions to antivenin, have understandably led to a fear of polyvalent antivenin therapy and a reluctance by clinicians to administer this potentially beneficial treatment.1,12
Although our study lacks the power to definitively evaluate the use of skin test screening for acute reactions to antivenin, our data suggest that this test is highly unreliable in predicting acute side effects. This is in agreement with prior studies that have demonstrated false-positive rates as high as 40%.1,2,13 None of the patients who underwent documented skin testing in our study was harmed by the test, and some high-risk patients may have been identified. In only 1 patient was antivenin withheld based on a positive skin test result. Therefore, it is difficult to recommend against skin testing as described in the package insert. Clinicians should, however, be aware of the inherent unreliability of this test. Despite being packaged together, the vial of horse serum provided for skin testing and the vial of antivenin are not prepared from the same horse and do not contain the same concentrations of horse proteins.10 This may explain the unreliability of this test. Some experts recommend using diluted reconstituted antivenin for skin testing.10
The main limitations of our study are related to its retrospective nature. Recording bias is an important possible limitation. Acute complications to antivenin administration may have occurred that were not recorded in the hospital record. During our data collection, if no mention of acute side effects was made in the medical record, it was assumed that no reaction occurred. We have assumed that any serious, acute reaction to antivenin would have been recorded in the hospital medical record.
Because snakebite patients were seen by many different clinicians over an 11-year period, some variation in clinical practice was inevitable. For example, the amount of antivenin given based on envenomation severity and the treatments given for acute antivenin reactions were highly variable. One patient with an apparent nonvenomous bite was also given 3 vials of antivenin before the onset of symptoms. Most likely this antivenin was given inadvertently or by an inexperienced clinician. This variation in clinical practice makes it difficult to draw conclusions regarding the efficacy of antivenin or the management of acute antivenin reactions. However, assessment of the frequency of acute reactions and safety of antivenin were still possible.
Referral bias is another possible limitation to our study. Because this study was performed at a large academic medical center, the study population may not mirror patient populations encountered at most community emergency departments. In many community hospitals, highly severe envenomation and acute reaction to antivenin therapy are accepted indications for transfer. Therefore, this referral bias would, if anything, tend to increase the severity of envenomations and the number of allergic reactions in our study population.
Polyvalent crotalid antivenin remains the treatment of choice for moderate to severe rattlesnake envenomation. In this retrospective study, a large number of patients were treated with few apparent side effects. Acute allergic reactions were generally mild and consisted usually of urticaria alone. Severe systemic side effects were rare. Until newer products with even fewer side effects are widely available, polyvalent antivenin should be used for the treatment of moderate to severe rattlesnake envenomation without fear of dangerous side effects.14,15,16
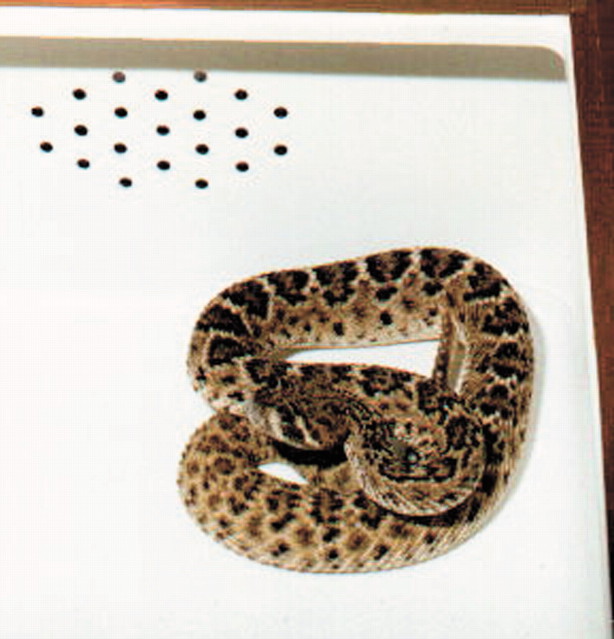
Figure 1.
Crotalus atrox: use of polyvalent antivenin after its bite is safe and effective
Acknowledgments
James Holmes and Nathan Kuppermann helped in the data analysis and in the writing of the manuscript.
Competing interests: None declared
References
- 1.Jurkovich GJ, Luterman A, McCullar K, Ramenofsky ML, Curreri PW. Complications of Crotalidae antivenin therapy. J Trauma 1988;28: 1032-1037. [DOI] [PubMed] [Google Scholar]
- 2.Spaite DW, Dart RC, Hurlbut JT, et al. Skin testing: implications in the management of pit viper envenomation. Ann Emerg Med 1988;17: 389. [Google Scholar]
- 3.Roberts JR, Otten EJ. Snakebites and other reptiles. In: Goldfrank LR, ed. Goldfrank's Toxicologic Emergencies. Stamford, CT: Appleton & Lange; 1998: 1603-1623.
- 4.Tanen D, Ruha A, Graeme K, Curry S. Epidemiology and hospital course of rattlesnake envenomations cared for at a tertiary referral center in central Arizona. Acad Emerg Med 2001;8: 177-182. [DOI] [PubMed] [Google Scholar]
- 5.Minton SA. Polyvalent antivenin in the treatment of experimental snake venom poisoning. Am J Trop Med Hyg 1954;3: 1077-1082. [DOI] [PubMed] [Google Scholar]
- 6.Russell FE, Ruzic N, Gonzalez H. Effectiveness of antivenin (Crotalidae) polyvalent following injection of Crotalus venom. Toxicon 1973;11: 461-464. [DOI] [PubMed] [Google Scholar]
- 7.Brubacher JR, Lachman D, Hoffman RS. Efficacy of Wyeth polyvalent antivenin used in the pretreatment of copperhead envenomation in mice. Wilderness Environ Med 1999;10: 142-145. [DOI] [PubMed] [Google Scholar]
- 8.Rosen PB, Leiva JI, Ross CP. Delayed antivenom treatment for a patient after envenomation by Crotalus atrox. Ann Emerg Med 2000;35: 86-88. [DOI] [PubMed] [Google Scholar]
- 9.Derlet RW, Silva J. Rattlesnake bites: surgical vs. medical treatment. Med Rounds 1989;2: 35-39. [Google Scholar]
- 10.Norris RL, Bush SP. North American venomous reptile bites. In: Auerbach P, ed. Wilderness Medicine: Management of Wilderness and Environmental Emergencies. St Louis; Mosby; 2001: 896-926.
- 11.Walter FG, Bilden EF, Gibly RL. Envenomations. Crit Care Clin 1999;15: 353-386. [DOI] [PubMed] [Google Scholar]
- 12.Arunanthy S, Hertzberg SR. A life-threatening anaphylactoid reaction to polyvalent snake antivenom despite pretreatment. Med J Aust 1998;169: 257-258. [DOI] [PubMed] [Google Scholar]
- 13.Malasit P, Warrell DA, Chanthavanich P, et al. Prediction, prevention, and mechanism of early (anaphylactic) antivenom reactions in victims of snake bites. BMJ 1986;292: 17-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Seifert SA, Boyer LV, Dart RC, Porter RS, Sjostrom L. Relationship of venom effects to venom antigen and antivenom serum concentrations in a patient with Crotalus atrox envenomation treated with a Fab antivenom. Ann Emerg Med 1997;30: 49-53. [DOI] [PubMed] [Google Scholar]
- 15.Clark RF, Williams SR, Nordt SP, Boyer-Hassen LV. Successful treatment of crotalid-induced neurotoxicity with a new polyspecific crotalid Fab antivenom. Ann Emerg Med 1997;30: 54-57. [DOI] [PubMed] [Google Scholar]
- 16.Dart RC, Seifert SA, Carroll L, et al. Affinity-purified, mixed monospecific crotalid antivenom ovine Fab for the treatment of crotalid venom poisoning. Ann Emerg Med 1997;30: 33-39. [DOI] [PubMed] [Google Scholar]