Franklin Delano Roosevelt: a case study Much information is available regarding the medical care of Franklin Delano Roosevelt(FDR).1,2
Figure 1 shows FDR's blood pressures duringhis presidency. In 1935, FDR's pressure was at the upper end of thenormal range but rose significantly over 9 years. By March 1945, FDRbecame ill, and Howard Bruenn, a cardiologist, was asked to examinethe president. Bruenn heard rales during physical examination. A chestx-ray film showed pulmonary edema and an enlarged cardiacsilhouette.
Electrocardiography (ECG) gave evidence of leftventricular (LV) hypertrophy, and urinalysis showed proteinuria. FDRwas manifesting several cardiovascular consequences of untreatedhypertension; LV hypertrophy, congestive heart failure (CHF), andrenal insufficiency.
Bruenn initiated digitalis therapy, alow-salt diet, a reduction in FDR's substantial alcohol and cigaretteuse, and bed rest. Within a week, FDR no longer evidenced CHF. InAugust 1944, he had chest pain while giving a campaign speech on anaval ship. In the captain's quarters, he complained of severe,crushing pain for 15 minutes. ECG and white blood cell count showedthat he was not having a myocardial infarction (MI) but angina,another possible hypertensive complication. In radio addresses at thetime of the Yalta Conference, FDR was audibly wheezing and unable tocomplete sentences. His blood pressure at the time approached 250/150mm Hg. Historians believe Stalin took advantage of a debilitatedpresident, actions that determined the fate of eastern Europe.
In April 1945, while seated for a portrait in his Georgia vacationhome, FDR fell unconscious. Bruenn estimated FDR's blood pressure tobe 350/195 mm Hg. The president died within the hour of anotherpossible hypertensive complication, intracerebral hemorrhage.
Figure 1.
Systolic and diastolic blood pressures of Franklin DelanoRoosevelt between 1931 and his death on April 12, 1945 (data fromFerrell1 andBruenn2)
METHODS
Studies were identified by searching MEDLINE within yearparameters of 1970 and 2001 using the terms angiotensin-convertingenzyme inhibitor, angiotensin-receptor blocker, andangiotensin-receptor antagonist and bibliographies ofincluded studies. Controlled trials, case reports, and reviews werereferenced.
DEVELOPMENT OF ANTIHYPERTENSIVE THERAPY
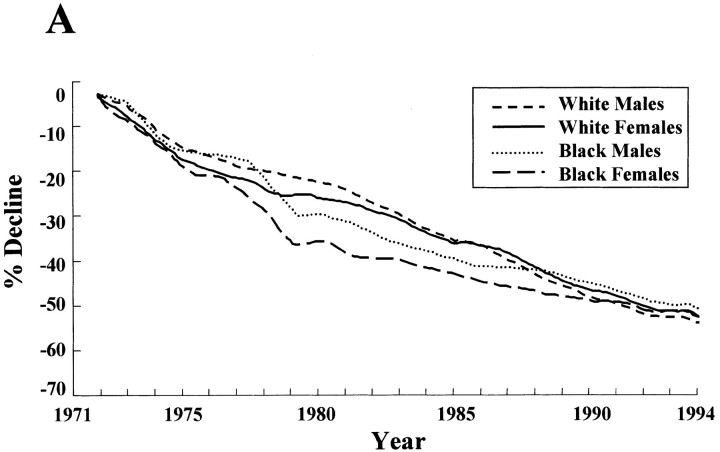
Unfortunately for FDR, the first, relatively tolerableanti-hypertensive agents, β-blockers and diuretic agents, did notbecame available until the 1950s. Since then, 28 trials havedemonstrated reduction of cardiovascular morbidity and mortality withantihypertensive therapy. In 1971, the National Heart, Lung, and BloodInstitute initiated the National High Blood Pressure Education Programto increase physician and patient awareness about treatinghypertension. Mortality rates due to coronary heart disease and strokehave steadily decreased in the past 25 years, coincident withincreased treatment of hypertension (figure 2A,2B). Since 1991 these curves have leveledoff, and stroke deaths are on the rise. The National Health andNutrition Examination Survey found a decrease in awareness andtreatment of hypertension between 1991 and 1995.3,4
Figure 2A.
Percentage decline inage-adjusted mortality rates for coronary heart disease (A) and strokeby sex and race (B): United States, 1972-1994 (from the NationalHeart, Lung, Blood Institute; Vital Statistics of the United States,National Center for Health Statistics)
Figure 2B.
Percentage decline in age-adjusted mortality rates for coronaryheart disease (A) and stroke by sex and race (B): United States,1972-1994 (from the National Heart, Lung, Blood Institute; VitalStatistics of the United States, National Center for HealthStatistics)
Figure 3 shows the pathophysiologicmechanisms of blood pressure regulation andhypertension.5 Blood pressure is the product ofcardiac output and peripheral vascular resistance. If eitherincreases, blood pressure rises. β-Blocker and diuretic agentswork by lowering cardiac output. Diuretics decrease intravascularfluid volume and cardiac preload; β-blockers depress cardiacinotropy and chronotropy. Although they are effective in treatinghypertension and reducing mortality and morbidity, side effects limitpatients' compliance with their use.
Figure 3.
Determinants of blood pressure (hypertension) in thecardiovascular system based on Poiseuille's law (1842) (adapted fromKaplan5)
Newer drugs inhibited actionsof the central or peripheral sympathetic nervous system on bloodpressure; these drugs are the adrenergic inhibitors (clonidine andreserpine) and α1-adrenergic-receptor blockers(prazosin). Although these drugs are effective, significant sideeffects relegated them to second-line therapy.
More recent drugdevelopment has focused on decreasing peripheral vascular resistance(figure 3). Calciumchannel blockers, which inhibit calcium uptake into the vascularsmooth muscle cells, are effective antihypertensive drugs with betterside effect profiles than previously developed drugs.
ANGIOTENSIN-CONVERTING ENZYME INHIBITORS
Renin-angiotensin system
Angiotensin-convertingenzyme (ACE) converts inactive angiotensin I to the activeoctapeptide, angiotensin II (figure4). Angiotensin II binds to the receptors throughout thebody, which affect blood pressure (figure 5). ACE, also known as kininase II,not only blocks conversion of angiotensin I to angiotensin II but alsoinhibits the breakdown of various kinins, including bradykinin andsubstance P. Until recently, it was presumed that adverse effects ofangiotensin-converting enzyme inhibitors (ACEIs) were caused primarilyby increased bradykinin and substance P. Data now suggest that many ofthe benefits of ACEIs may be partially acting throughbradykinin.6,7,8,9
Figure 4.
The renin-angiotensin system
Figure 5.
Angiotensin II-receptor binding affecting blood pressure (adaptedfrom Kaplan5)
Angiotensin II
Angiotensin II binds to receptorsthroughout the body, acutely increasing blood pressure (figure 5). Angiotensin II alsohas long-term effects that are potentially detrimental to thecardiovascular system. Angiotensin II-mediated stimulation of growthfactors and proto-oncogene activators within the kidney, thevasculature, and the heart result in renovascular, peripheralvascular, and myocardial hypertrophy.10 Therefore, attacking therenin-angiotensin system should control not only hypertension but alsomany of its sequelae.
Brazilian pit viper
ACEIs were discovered when scientists were studying the venom ofthe Brazilian pit viper, Bothrops jararacussu. Peptides inthe venom increased bradykinin, a substance thought to shock theviper's prey. The investigators discovered that these same peptidesreduced angiotensin II levels. Four of the 5 binding ligands of thefirst oral ACEI developed (captopril) are similar to binding ligandsof the venom peptide.11
ACEIs are effective intreating high blood pressure, especially in white and young patients(patients with “high-renin” hypertension). Many patientswith newly diagnosed hypertension have concomitant medical issues thatmust be considered when choosing first-line hypertensivetherapy. ACEIs play an important role as first-line therapy in many ofthese patients. As set forth in the treatment algorithm of the 6thJoint National Committee on the Detection, Evaluation, and Treatmentof Hypertension, ACEIs are first-line therapy in diabetic patients whohave proteinuria, CHF, and have had an MI.4
Renaldisease
Adding ACEIs to usual therapy in patients with type 1diabetes mellitus who have proteinuria reduced the progression ofproteinuria by 40% and lowered the combined end points of death,transplantation, or dialysis by 50%.12 Data in patients with type 2diabetes and those without diabetes suggest that ACEIs should beconsidered first-line therapy in any patient with hypertension andproteinuria. The renoprotective effects of ACEIs may be due to theirunique ability to lower intraglomerular capillary pressure, inaddition to the blood pressure.
CHF
Sixteen trials have demonstrated that ACEIs reduce morbidity andmortality in patients with depressed LV ejection fractions(LVEFs). The Cooperative North Scandinavian Enalapril Survival Study(CONSENSUS) and SOLVD-Treatment trials showed improved survival andfewer hospital admissions in patients treated withACEIs.13,14 SOLVD-Prevention demonstrateddecreased mortality and hospitalizations for patients with CHF who hadasymptomatic LV dysfunction.15 A meta-analysis of 16 CHF trialsfound a 24% survival benefit after 1 year when ACEIs were added tostandard CHF therapy.16
After an MI
Fifteen trials demonstrated that ACEIs improved survival ratesafter an MI.17,18 The benefit is seen primarily inpatients with reduced LVEFs. A meta-analysis of 14 trials of ACEI usefollowing MI found a 20% reduction after 1 year in the incidence ofsudden cardiac death.18
There'sHOPE
The Heart Outcomes Prevention Evaluation Study (HOPE)demonstrated that ACEI use significantly reduced rates of death, MI,and stroke in patients at high risk for cardiovascular disease but whodo not have evidence of LV dysfunction or CHF.19 A total of 9,500patients (32% women) aged 55 years or older with a history of coronaryartery disease, peripheral vascular disease, stroke, or diabetesmellitus and who had at least 1 other cardiac risk factor (46% hadhypertension) were randomly allocated to receive an ACEI (ramipril) orplacebo. After 4.5 years, there was a 22% reduction of risk forcardiovascular events with ACEI therapy. Interestingly, diabetesdeveloped in significantly fewer patients in the group taking theACEI. This study suggests that ACEI use has benefits beyond treatinghypertension for patients at risk for cardiovascular events. Toconfirm these findings, a similar trial with the ACEI trandolapril isunder way.
Adverse effects
A dry coughdevelops in 3% to 25% of patients who are taking an ACEI. This classeffect is due to increased bradykinin and substance P levels andsubsequent prostaglandin production, which stimulate the cough reflexin the bronchial arterial tree. Angioedema is an infrequent butpotentially life-threatening adverse effect that occurs in 0.1% to0.3% of patients receiving ACEI therapy. The incidence is higher inAfrican Americans. Angioedema usually occurs early in ACEI therapybut has been diagnosed after more than a year. Angioedema may also berelated to increased bradykinin-induced prostaglandin production,which causes histamine release.
Acute renal insufficiency andhyperkalemia can occur in elderly patients with reduced LVEFs. Thesepatients receive diuretic therapy and become intravascularlydepleted. ACE inhibition produces efferent arterial dilation that canprecipitously drop the glomerular capillary pressure. The glomerularfiltration rate falls, and creatinine and potassium levels rise. Theseadverse effects can be minimized if patients are allowed to becomeeuvolemic before the ACEI therapy is instituted. Symptomatichypotension is a possible adverse effect in patients with vasculopathywho have bilateral renal artery stenosis.
Isbradykinin good or bad?
It was presumed that the adverseeffects of ACEIs were primarily due to increased bradykinin and thatthe beneficial effects were due to reduced angiotensin II. However,data suggest that the mechanisms underlying ACEI effects are morecomplex. Biollaz et al20 studied the effects of enalapril insubjects with hypertension. An immediate blood pressure responseoccurred after 4 hours, and this effect was sustained through 6months. Plasma ACE activity was also reduced after 4 hours andremained low over the 6-month study. At 4 hours, there was also asignificant drop in angiotensin II levels, and levels appeared lowerat 24 hours and during the first months of therapy. However, by 5months, plasma angiotensin II levels had returned to normal. Thus,increased bradykinin may be important in the long-term blood pressureeffect of ACEIs. A recent study showed that a bradykinin-receptorantagonist significantly attenuated the ACEI blood pressureeffect. Animal studies suggest that ACEI-induced bradykinin may alsobe important in reducing morbidity and mortality in cardiomyopathy andafter an MI.6,8
ANGIOTENSIN II-RECEPTOR BLOCKERS
AngiotensinII-receptor blockers (ARBs) are equipotent to ACEIs, β-blockers,diuretic agents, and calcium channel blockers for lowering bloodpressure in a general population. Compared with placebo, ARBs havesimilar rates of adverse effects. Patients have no dry cough(bradykinin breakdown is unaffected; figure 4 and figure 6).21 Few cases of ARB-induced angioedemahave been reported. However, given that many patients have receivedARB without incurring angioedema after conversion from an ACEI, thisshould be a relative contraindication for ARB use.
Figure 6.
Mechanism of action of angiotensin II-receptor blockers (ARBs)(adapted from Weir and Dzau21). AT1 = angiotensinII-receptor type 1.
Renal disease
Pilot studies suggest thatthe progression of renal disease in patients with type 1 and type 2diabetes mellitus can be slowed with ARBs to a similar degree as seenwith ACEIs.22,23 Trials are under way in patientswith type 2 diabetes who have proteinuria to assess ARB effects onmorbidity and mortality.24,25,26
After MI
Data from studies in animals suggest that LVEFs after MI may beimproved and reperfusion arrhythmias reduced with ARB use comparedwith ACEIs.6Two trials are under way that compare the use of ARBs with that ofACEIs in patients who have had MI and who have reducedLVEFs.27,28
CHF
The study Evaluating Losartan in the Elderly (ELITE) was the firstto suggest comparable safety and efficacy between ARBs and ACEIs inpatients with CHF.29 Participants with New York HeartAssociation class II to IV heart failure (n=722; mean age, 72 years)with LVEFs of less than 40% who were not previously treated with ACEIswere randomly allocated to receive losartan potassium orcaptopril.29 The primary end point of increasedserum creatinine levels occurred in 10.5% of each group. Adverseeffects were lower with the use of losartan (44 vs 77 patients;P<0.002). The hospitalization rate for CHF was 5.7% ineach group. Mortality was lower with losartan use (4.8%) than withcaptopril (8.7%; P = 0.04), an important finding because weknow that ACEIs reduce mortality in patients with CHF.
In thelarger ELITE-II trial, patients older than 60 years with LVEFs of lessthan 40% were again randomly assigned to treatment with eitherlosartan or captopril.30 Losartan and captopril were equallyefficacious in the treatment of patients with CHF. The authorsconcluded that although ARBs have not been proved to be substitutesfor ACEIs, they may be a safe and effective alternative inACEI-intolerant patients who have CHF.
ACEI INCOMBINATION WITH ARB
The use of ACEIs improves morbidity andmortality in patients with CHF, possibly through increased bradykininlevels. Blocking angiotensin II-receptor binding with ARBs may offercomparable benefit. Would combination therapy be better than eitherdrug alone for treating CHF? In 4 pilot studies, patients with CHF onlong-term ACEI therapy were randomly allocated to receive ACEI, ARB,or combination therapy.31,32,33,34 Beneficial end points withcombination therapy included additional blood pressure lowering andimproved exercise tolerance, New York Heart Associationclassification, and LVEFs.
The Valsartan Heart Failure Trial(VAL-HeFT; presented at the American Heart Association 2000 ScientificSessions). was the first large trial to determine if there wasincremental value in adding an ARB to long-term ACEI therapy inpatients with CHF. Patients with New York Heart Association class IIto IV CHF who had LVEFs of less than 40% were randomly allocated toreceive valsartan or placebo (n=5,010; 93% receiving long-term ACEItherapy). There was a small (13%) reduction in the primary end pointof combined mortality, sudden cardiac death, CHF hospitalization, orneed for intravenous CHF medical therapy (P<0.01). Thiswas primarily due to a 27% reduction in CHF hospitalizations, with nosignificant effect on mortality. Positive secondary end pointsincluded improvement in LVEFs and quality of life.
CONCLUSIONS
ACEIs remain first-line therapy inpatients with hypertension and concurrent CHF, proteinuria, or whohave had an MI, because their use lowers morbidity and mortality ineach of these types of patients. For patients who cannot tolerateACEIs, ARBs may offer an alternative, especially in patients with CHF,for whom more data with ARBs are available. Future trials will confirmwhether adding ARB to the medical regimen of these patients alreadytaking an ACEI will add significant incremental value. Which class ofdrugs will be first-line therapy in the future? If pending studiesshow that ARBs are as good, if not better, than ACEI therapy withfewer side effects, ARBs may replace ACEIs in the treatment of thesepatients.
Franklin Delano Roosevelt suffered manycardiovascular consequences of untreated hypertension. During the lastyear of his presidency, while guiding the United States through WorldWar II, FDR was plagued with CHF, renal disease, and angina and diedof a cerebrovascular event. It is obvious that he would have benefitedon many levels from a medication that attacked the renin-angiotensinsystem.
Summary points
Angiotensin-converting enzyme inhibitors (ACEIs) are first-line therapy in patients with hypertension and concurrent congestive heart failure or proteinuria or who have had myocardial infarction; they reduce morbidity and mortality in each of these patients
Angiotensin II-receptor blockers (ARBs) are equipotent to ACEIs, β-blockers, diuretics, and calcium channel blockers for lowering blood pressure in a general population
ARBs have excellent adverse effect profiles comparable to placebo
In patients who cannot tolerate ACEIs, ARBs may offer an alternative, especially in patients with congestive heart failure where morbidity and mortality data with the use of ARBs are available
Future trials will confirm whether adding an ARB to the medical regimen of patients with congestive heart failure who are already taking an ACEI will add significant incremental value
Figure 2.
Roosevelt in November 1944. Five months later, he would die ofhypertensive complications
AP
Figure 3.
This man is having his blood pressure checked by a nurseat a distance using a digital monitor
Paul Vathis/AP
Competing interests: V F has received honoraria for talks on hypertensive therapy for several pharmaceutical companies, including BMS, Novartis, Merck, Astra Merck, and Pfizer
Authors: Timothy Bishop is a cardiology fellow at University of New Mexico Health Sciences Center, Albuquerque. Vincent Figueredo is director of echocardiography and cardiovascular clinical research at the Heart and Vascular Center at Lovelace Clinic and associate director of the Center for Preventive Cardiovascular Medicine at University of New Mexico Health Sciences Center.
References
- 1.Ferrell RH. TheDying President: Franklin D Roosevelt,1944-1945. Columbia, MO: University of Missouri Press;1998.
- 2.Bruenn H. Clinical notes onthe illness and death of President Franklin DRoosevelt. Ann Intern Med 1970;72:579-591. [DOI] [PubMed] [Google Scholar]
- 3.Burt VL, Culter JA, Higgins M,et al. Trends in the prevalence, awareness, treatment, and control ofhypertension in the adult US population: data from the healthexamination surveys, 1960 to 1991.Hypertension 1995;26:60-69 [erratum published inHypertension 1996;27:1192]. [DOI] [PubMed] [Google Scholar]
- 4.The sixth report of the JointNational Committee on prevention, detection, evaluation, and treatmentof high blood pressure. Arch Intern Med 1997;157:2413-2446 [erratum published in ArchIntern Med 1998;158:573]. [DOI] [PubMed] [Google Scholar]
- 5.Kaplan NM. ClinicalHypertension. 6th ed. Baltimore: Williams & Wilkins;1994.
- 6.Weidenbach R, Schulz R, GresP, Behrends M, Post H, Heusch G. Enhanced reduction of myocardialinfarct size by combined ACE inhibition and AT(1)-receptorantagonism. Br J Pharmacol 2000;131:138-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Taal MW, BrennerBM. Renoprotective benefits of RAS inhibition: from ACEI toangiotensin II antagonists. Kidney Int 2000;57:1803-1817. [DOI] [PubMed] [Google Scholar]
- 8.Liu YH, Yang XP, Mehta D,Bulagannawar M, Scicli GM, Carretero OA. Role of kinins in chronicheart failure and in the therapeutic effect of ACE inhibitors inkininogen-deficient rats. Am J Physiol Heart CircPhysiol 2000;278:H507-H514. [DOI] [PubMed] [Google Scholar]
- 9.Gainer JV, Morrow JD, LovelandA, King DJ, Brown NJ. Effect of bradykinin-receptor blockade on theresponse to angiotensin-converting-enzyme inhibitor in normotensiveand hypertensive subjects. N Engl J Med 1998;339:1285-1292. [DOI] [PubMed] [Google Scholar]
- 10.Sander GE, McKinnie JJ,Greenberg SS, Giles TD. Angiotensin-converting enzyme inhibitors andangiotensin II receptor antagonists in the treatment of heart failurecaused by left ventricular systolic dysfunction. ProgCardiovasc Dis 1999;41:265-300. [DOI] [PubMed] [Google Scholar]
- 11.Ferreira LA, Henriques OB,Lebrun I, et al. Biologically active peptides from Bothropsjararacussu venom. Agents Actions Suppl 1992;36:209-214. [PubMed] [Google Scholar]
- 12.Lewis EJ, Hunsicker LG, BainRP, Rohde RD. The effect of angiotensin-converting-enzyme inhibitionon diabetic nephropathy: the Collaborative Study Group. NEngl J Med 1993;329:1456-1462 [erratum published in N Engl JMed 1994;330:152]. [DOI] [PubMed] [Google Scholar]
- 13.The CONSENSUS Trial StudyGroup. Effects of enalapril on mortality in severe congestive heartfailure: results of the Cooperative North Scandinavian EnalaprilSurvival Study (CONSENSUS). N Engl J Med 1987;316:1429-1435. [DOI] [PubMed] [Google Scholar]
- 14.The SOLVDInvestigators. Effect of enalapril on survival in patients withreduced left ventricular ejection fractions and congestive heartfailure. N Engl J Med 1991;325:293-302. [DOI] [PubMed] [Google Scholar]
- 15.Yusuf S, Pepine CJ, GarcesC, et al. Effect of enalapril on myocardial infarction and unstableangina in patients with low ejectionfractions. Lancet 1992;340:1173-1178. [DOI] [PubMed] [Google Scholar]
- 16.Massie BM. 15 years ofheart-failure trials: what have we learned?Lancet 1998;352(suppl 1):S129-S133. [DOI] [PubMed] [Google Scholar]
- 17.Flather MD, Yusuf S, KoberL, et al. Long-term ACE-inhibitor therapy in patients with heartfailure or left-ventricular dysfunction: a systematic overview of datafrom individual patients. ACE-Inhibitor Myocardial InfarctionCollaborative Group. Lancet 2000;355:1575-1581. [DOI] [PubMed] [Google Scholar]
- 18.Domanski MJ, Exner DV,Borkowf CB, Geller NL, Rosenberg Y, Pfeffer MA. Effect of angiotensinconverting enzyme inhibition on sudden cardiac death in patientsfollowing acute myocardial infarction: a meta-analysis of randomizedclinical trials. J Am Coll Cardiol 1999;33:598-604. [DOI] [PubMed] [Google Scholar]
- 19.Yusuf S, Sleight P, Pogue J,Bosch J, Davies R, Dagenais G. Effects of anangiotensin-converting-enzyme inhibitor, ramipril, on cardiovascularevents in high-risk patients: the Heart Outcomes Prevention EvaluationStudy Investigators. N Engl J Med 2000;342:145-153 [errata published in N Engl JMed 2000;342:748, 1376].10639539 [Google Scholar]
- 20.Biollaz J, Brunner HR,Gavras I, Waeber B, Gavras H. Antihypertensive therapy with MK 421:angiotensin II-renin relationships to evaluate efficacy of convertingenzyme blockade. J Cardiovasc Pharmacol 1982;4:966-972. [PubMed] [Google Scholar]
- 21.Weir MR, Dzau VJ. Therenin-angiotensin-aldosterone system: a specific target forhypertension management. Am J Hypertens 1999;12:205S-213S. [DOI] [PubMed] [Google Scholar]
- 22.Ruilope LM, Aldigier JC,Ponticelli C, Oddou-Stock P, Botteri F, Mann JF. Safety of thecombination of valsartan and benazepril in patients with chronic renaldisease. European Group for the Investigation of Valsartan in ChronicRenal Disease. J Hypertens 2000;18:89-95. [PubMed] [Google Scholar]
- 23.Lacourciere Y, Belanger A,Godin C, et al. Long-term comparison of losartan and enalapril onkidney function in hypertensive type 2 diabetics with earlynephropathy. Kidney Int 2000;58:762-769. [DOI] [PubMed] [Google Scholar]
- 24.Andersen S, Tarnow L,Rossing P, Hansen BV, Parving HH. Renoprotective effects ofangiotensin II receptor blockade in type 1 diabetic patients withdiabetic nephropathy. Kidney Int 2000;57:601-606. [DOI] [PubMed] [Google Scholar]
- 25.Rodby RA, Rohde RD, ClarkeWR, et al. The Irbesartan Type II Diabetic Nephropathy Trial: studydesign and baseline patient characteristics. For the CollaborativeStudy Group. Nephrol Dial Transplant 2000;15:487-497. [DOI] [PubMed] [Google Scholar]
- 26.Venkata C, Ram S, FierroG. The benefits of angiotensin II receptor blockers in patients withrenal insufficiency or failure. Am J Ther 1998;5:101-105. [DOI] [PubMed] [Google Scholar]
- 27.Pfeffer MA, McMurray J,Leizorovicz A, et al. Valsartan in acute myocardial infarction trial(VALIANT): rationale and design. Am Heart J 2000;140:727-750. [DOI] [PubMed] [Google Scholar]
- 28.Dickstein K, Kjekshus J;OPTIMAAL Trial Steering Committee and Investigators. Comparison ofbaseline data, initial course, and management: losartan versuscaptopril following acute myocardial infarction (The OPTIMAALTrial). Optimal Trial in Myocardial Infarction with the AngiotensinIIAntagonist Losartan. Am J Cardiol 2001;87:766-771, A7. [DOI] [PubMed] [Google Scholar]
- 29.Pitt B, Segal R, MartinezFA, et al. Randomised trial of losartan versus captopril in patientsover 65 with heart failure (Evaluation of Losartan in the ElderlyStudy, ELITE). Lancet 1997;349:747-752. [DOI] [PubMed] [Google Scholar]
- 30.Pitt B, Poole-Wilson PA,Segal R, et al. Effect of losartan compared with captopril onmortality in patients with symptomatic heart failure: randomisedtrial—the Losartan Heart Failure Survival Study ELITEII. Lancet 2000;355:1582-1587. [DOI] [PubMed] [Google Scholar]
- 31.Baruch L, Andan IS, Judd DL,et al. Hemodynamic response to AT1 receptor blockade with Valsartan inACE inhibitor-treated patients with heart failure[Abstr]. Circulation 1996;94(suppl I):I-428. [Google Scholar]
- 32.Tocchi M, Rosiano S, AnzuiniA, et al. Angiotensin II receptor blockade combined to ACE-inhibitionimproves left ventricular dilation and exercise ejection fraction incongestive heart failure [Abstr]. J Am CollCardiol 1998;31:188A. [Google Scholar]
- 33.Hamroff G, Blaufarb I,Mancini D, et al. Angiotensin II-receptor blockade further reducesafterload safely in patients maximally treated withangiotensin-converting enzyme inhibitors for heartfailure. J Cardiovasc Pharmacol 1997;30:533-536. [DOI] [PubMed] [Google Scholar]
- 34.McKelvie RS, Yusuf S,Pericak D, et al. Comparison of candesartan, enalapril, and theircombination in congestive heart failure: randomized evaluation ofstrategies for left ventricular dysfunction (RESOLVD) pilot study. TheRESOLVD Pilot Study Investigators.Circulation 1999;100:1056-1064. [DOI] [PubMed] [Google Scholar]